Paragangliomas and Anemia: Literature Review and Case Report
Abstract
1. Introduction
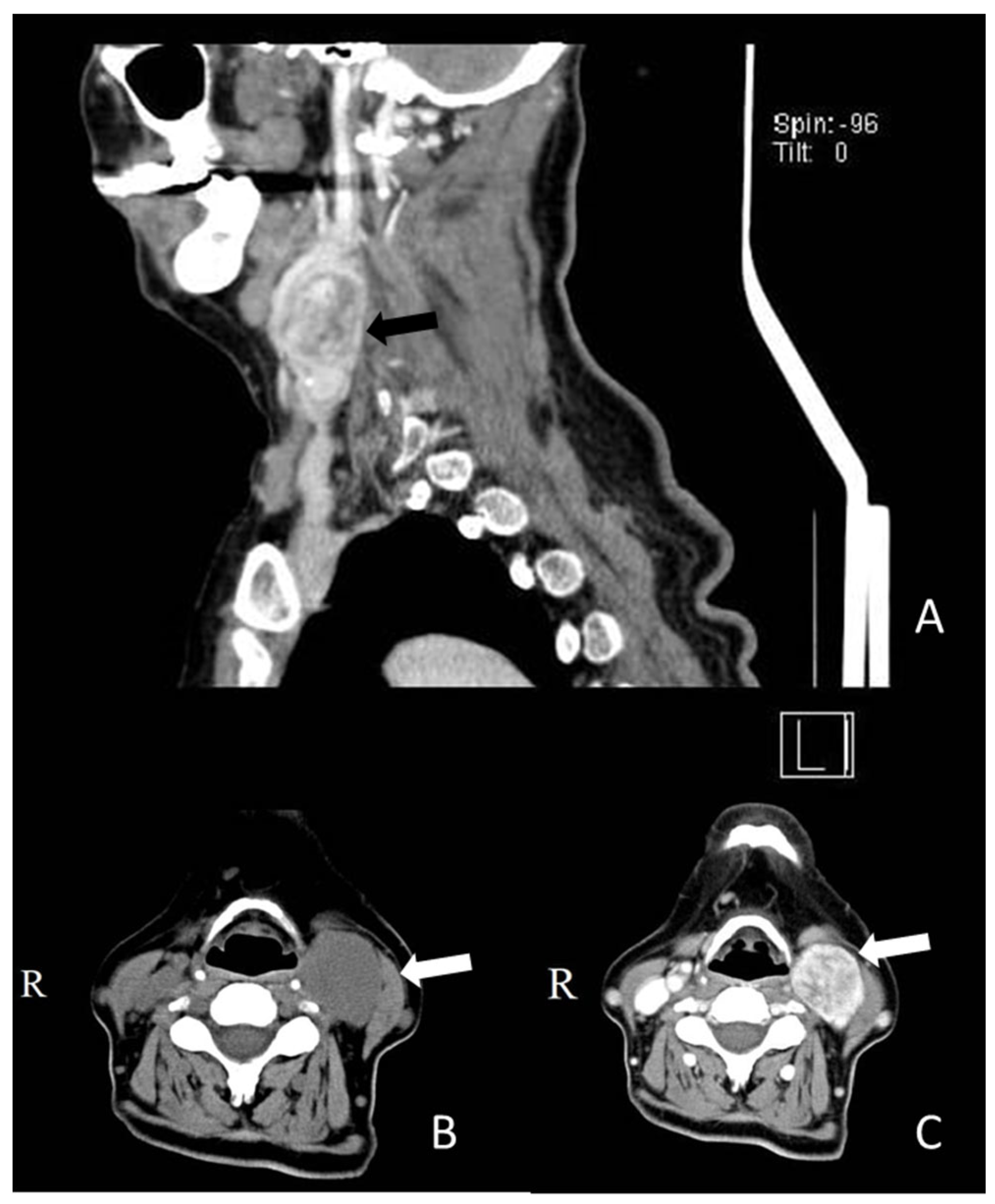
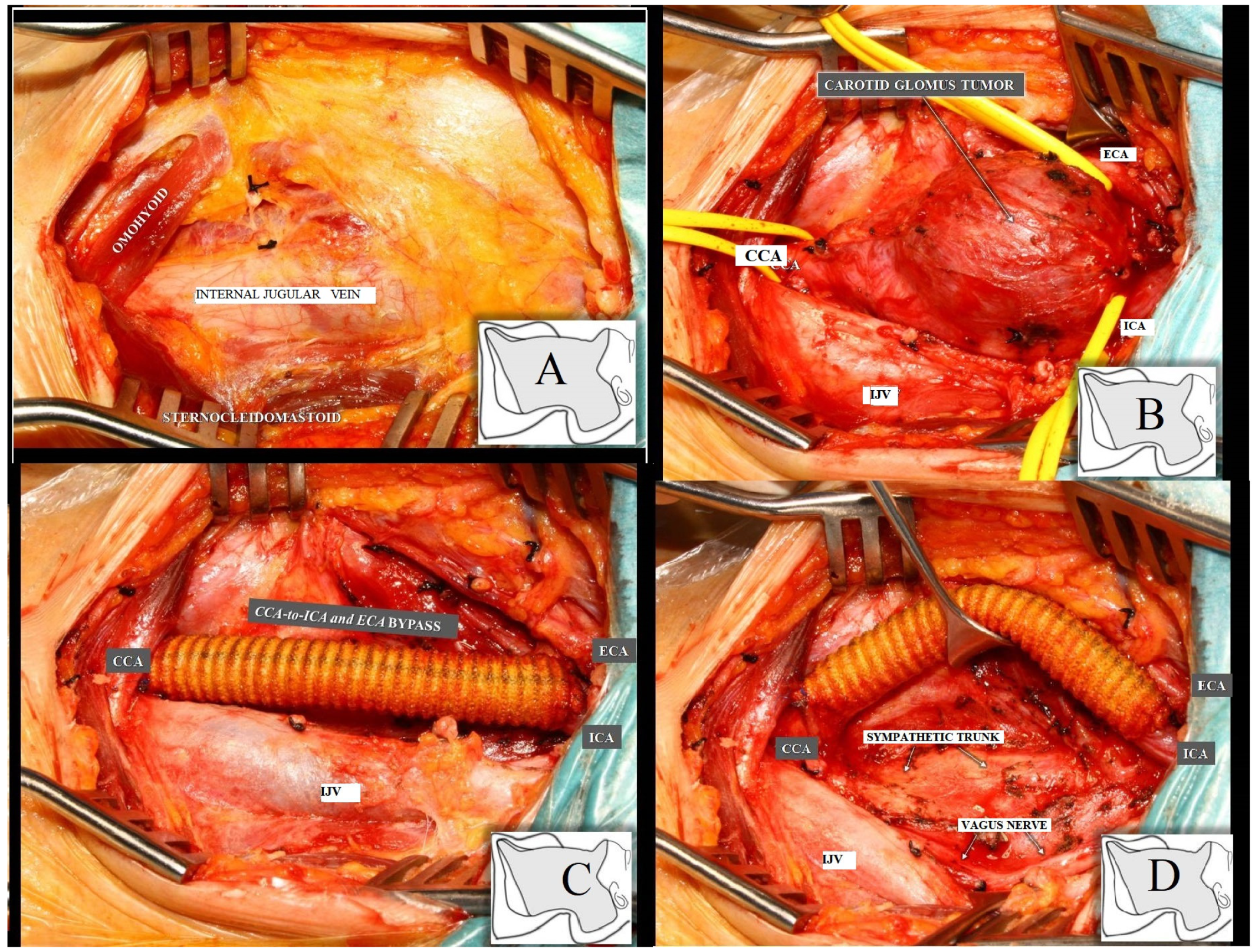
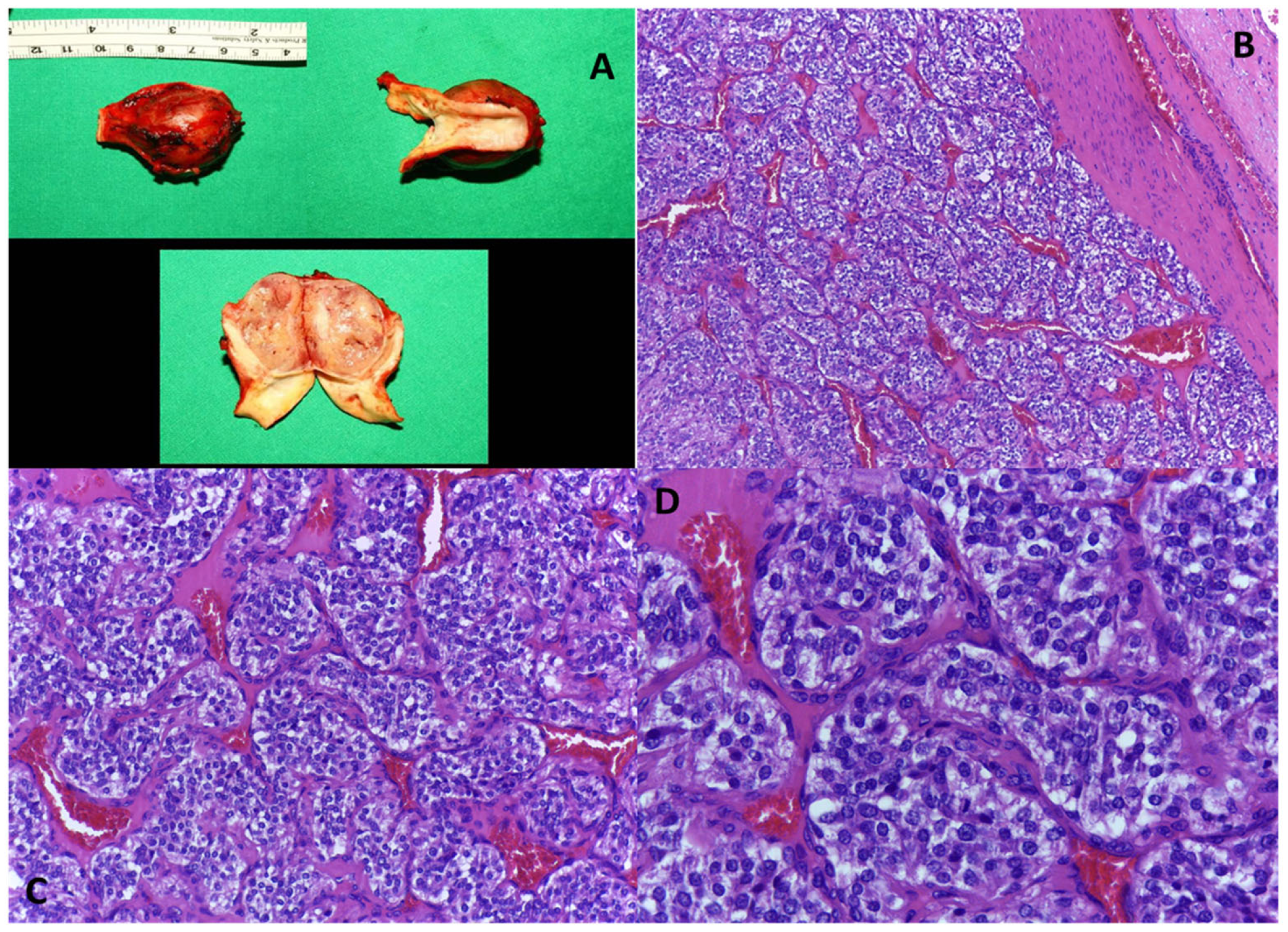
2. Case Report
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Andrei, S.; Isac, S.; Jelea, D.; Martac, C.; Stefan, M.-G.; Cotorogea-Simion, M.; Buzatu, C.G.S.; Ingustu, D.; Abdulkareem, I.; Vasilescu, C. COVID-19 Pandemic Was Associated with Lower Activity but Not Higher Perioperative Mortality in a Large Eastern European Center. Med. Sci. Monit. 2022, 28, e935809-1–e935809-13. [Google Scholar] [CrossRef] [PubMed]
- Welander, J.; Söderkvist, P.; Gimm, O. Genetics and clinical characteristics of hereditary pheochromocytomas and paragangliomas. Endocr. Relat. Cancer 2011, 18, R253–R276. [Google Scholar] [CrossRef] [PubMed]
- van Duinen, N.; Steenvoorden, D.; Kema, I.P.; Jansen, J.C.; Vriends, A.H.J.T.; Bayley, J.P.; Smit, J.W.A.; Romijn, J.A.; Corssmit, E.P.M. Increased urinary excretion of 3-methoxytyramine in patients with head and neck paragangliomas. J. Clin. Endocrinol. Metab. 2010, 95, 209–214. [Google Scholar] [CrossRef] [PubMed]
- McNicol, A.M. Update on tumours of the adrenal cortex, phaeochromocytoma and extra-adrenal paraganglioma. Histopathology 2011, 58, 155–168. [Google Scholar] [CrossRef] [PubMed]
- Erickson, D.; Kudva, Y.C.; Ebersold, M.J.; Thompson, G.B.; Grant, C.S.; van Heerden, J.A.; Young, W.F. Benign paragangliomas: Clinical presentation and treatment outcomes in 236 patients. J. Clin. Endocrinol. Metab. 2001, 86, 5210–5216. [Google Scholar] [CrossRef]
- Lee, J.A.; Duh, Q.Y. Sporadic paraganglioma. World J. Surg. 2008, 32, 683–687. [Google Scholar] [CrossRef]
- Dannenberg, H.; Dinjens, W.N.M.; Abbou, M.; Van Urk, H.; Pauw, B.K.H.; Mouwen, D.; Mooi, W.J.; de Krijger, R.R. Frequent germ-line succinate dehydrogenase subunit D gene mutations in patients with apparently sporadic parasympathetic paraganglioma. Clin. Cancer Res. 2002, 8, 2061–2066. [Google Scholar]
- Ramlawi, B.; David, E.A.; Kim, M.P.; Garcia-Morales, L.J.; Blackmon, S.H.; Rice, D.C.; Vaporciyan, A.A.; Reardon, M.J. Contemporary surgical management of cardiac paragangliomas. Ann. Thorac. Surg. 2012, 93, 1972–1976. [Google Scholar] [CrossRef]
- Brown, M.L.; Zayas, G.E.; Abel, M.D.; Young, W.F.; Schaff, H.V. Mediastinal paragangliomas: The mayo clinic experience. Ann. Thorac. Surg. 2008, 86, 946–951. [Google Scholar] [CrossRef]
- Armstrong, M.J.; Chiosea, S.I.; Carty, S.E.; Hodak, S.P.; Yip, L. Thyroid paragangliomas are locally aggressive. Thyroid 2012, 22, 88–93. [Google Scholar] [CrossRef]
- Castelblanco, E.; Gallel, P.; Ros, S.; Gatius, S.; Valls, J.; De-Cubas, A.A.; Maliszewska, A.; Yebra-Pimentel, M.T.; Menarguez, J.; Gamallo, C.; et al. Thyroid paraganglioma. Report of 3 cases and description of an immunohistochemical profile useful in the differential diagnosis with medullary thyroid carcinoma, based on complementary DNA array results. Hum. Pathol. 2012, 43, 1103–1112. [Google Scholar] [CrossRef] [PubMed]
- Simpson, L.N.; Hughes, B.D.; Karikari, I.O.; Mehta, A.I.; Hodges, T.R.; Cummings, T.J.; Bagley, C.A. Catecholamine-secreting paraganglioma of the thoracic spinal column: Report of an unusual case and review of the literature. Neurosurgery 2012, 70, E1049–E1052; discussion E1052. [Google Scholar] [CrossRef] [PubMed]
- Matsumoto, M.; Abe, K.; Baba, H.; Kinoshita, N.; Yamauchi, T.; Shiraishi, M.; Osaki, M.; Hayashi, T. Paraganglioma of the cauda equina: A report of two cases with unusual histopathological features. Clin. Neuropathol. 2012, 31, 39–43. [Google Scholar] [CrossRef] [PubMed]
- Burnichon, N.; Brière, J.J.; Libé, R.; Vescovo, L.; Rivière, J.; Tissier, F.; Jouanno, E.; Jeunemaitre, X.; Bénit, P.; Tzagoloff, A.; et al. SDHA is a tumor suppressor gene causing paraganglioma. Hum. Mol. Genet. 2010, 19, 3011–3020. [Google Scholar] [CrossRef]
- Fishbein, L.; Merrill, S.; Fraker, D.L.; Cohen, D.L.; Nathanson, K.L. Inherited mutations in pheochromocytoma and paraganglioma: Why all patients should be offered genetic testing. Ann. Surg. Oncol. 2013, 20, 1444–1450. [Google Scholar] [CrossRef]
- Boedeker, C.C.; Neumann, H.P.H.; Maier, W.; Bausch, B.; Schipper, J.; Ridder, G.J. Malignant head and neck paragangliomas in SDHB mutation carriers. Otolaryngol. Head Neck Surg. 2007, 137, 126–129. [Google Scholar] [CrossRef]
- Neumann, H.P.H.; Erlic, Z.; Boedeker, C.C.; Rybicki, L.A.; Robledo, M.; Hermsen, M.; Schiavi, F.; Falcioni, M.; Kwok, P.; Bauters, C.; et al. Clinical predictors for germline mutations in head and neck paraganglioma patients: Cost reduction strategy in genetic diagnostic process as fall-out. Cancer Res. 2009, 69, 3650–3656. [Google Scholar] [CrossRef]
- Drovdlic, C.M.; Myers, E.N.; Peters, J.A.; Baysal, B.E.; Brackmann, D.E.; Slattery, W.H.; Rubinstein, W.S. Proportion of heritable paraganglioma cases and associated clinical characteristics. Laryngoscope 2001, 111, 1822–1827. [Google Scholar] [CrossRef]
- Galan, S.R.; Kann, P.H. Genetics and molecular pathogenesis of pheochromocytoma and paraganglioma. Clin. Endocrinol. 2013, 78, 165–175. [Google Scholar] [CrossRef]
- Neumann, H.P.H.; Young, W.F.; Eng, C. Pheochromocytoma and Paraganglioma. N. Engl. J. Med. 2019, 381, 552–565. [Google Scholar] [CrossRef]
- Neumann, H.P.H.; Bausch, B.; McWhinney, S.R.; Bender, B.U.; Gimm, O.; Franke, G.; Schipper, J.; Klisch, J.; Altehoefer, C.; Zerres, K.; et al. Germ-line mutations in nonsyndromic pheochromocytoma. N. Engl. J. Med. 2002, 346, 1459–1466. [Google Scholar] [CrossRef] [PubMed]
- Al-Harthy, M.; Al-Harthy, S.; Al-Otieschan, A.; Velagapudi, S.; Alzahrani, A.S. Comparison of pheochromocytomas and abdominal and pelvic paragangliomas with head and neck paragangliomas. Endocr. Pract. 2009, 15, 194–202. [Google Scholar] [CrossRef] [PubMed]
- Eisenhofer, G.; Timmers, H.J.; Lenders, J.W.M.; Bornstein, S.R.; Tiebel, O.; Mannelli, M.; King, K.S.; Vocke, C.D.; Linehan, W.M.; Bratslavsky, G.; et al. Age at diagnosis of pheochromocytoma differs according to catecholamine phenotype and tumor location. J. Clin. Endocrinol. Metab. 2011, 96, 375–384. [Google Scholar] [CrossRef]
- O’Riordain, D.S.; Young, W.F.; Grant, C.S.; Carney, J.A.; van Heerden, J.A. Clinical spectrum and outcome of functional extraadrenal paraganglioma. World J. Surg. 1996, 20, 916–921; discussion 922. [Google Scholar] [CrossRef] [PubMed]
- Beard, C.M.; Sheps, S.G.; Kurland, L.T.; Carney, J.A.; Lie, J.T. Occurrence of pheochromocytoma in Rochester, Minnesota, 1950 through 1979. Mayo Clin. Proc. 1983, 58, 802–804. [Google Scholar]
- Chen, H.; Sippel, R.S.; O’Dorisio, M.S.; Vinik, A.I.; Lloyd, R.V.; Pacak, K. The North American Neuroendocrine Tumor Society consensus guideline for the diagnosis and management of neuroendocrine tumors: Pheochromocytoma, paraganglioma, and medullary thyroid cancer. Pancreas 2010, 39, 775–783. [Google Scholar] [CrossRef]
- McNeil, A.R.; Blok, B.H.; Koelmeyer, T.D.; Burke, M.P.; Hilton, J.M. Phaeochromocytomas discovered during coronial autopsies in Sydney, Melbourne and Auckland. Aust. N. Z. J. Med. 2000, 30, 648–652. [Google Scholar] [CrossRef]
- Sutton, M.G.; Sheps, S.G.; Lie, J.T. Prevalence of clinically unsuspected pheochromocytoma. Review of a 50-year autopsy series. Mayo Clin. Proc. 1981, 56, 354–360. [Google Scholar] [CrossRef]
- Brankovic, B.; Radisavljevic, M.; Radojkovic, M.; Stanojevic, G.; Stojanovic, M.; Nagorni, A.; Radojkovic, D.; Jeremic, L.; Nestorovic, M.; Karamarkovic, A. Nonfunctional retroperitoneal paraganglioma presenting as acute upper gastrointestinal hemorrhage. Hepatogastroenterology 2010, 57, 288–291. [Google Scholar]
- King, K.S.; Darmani, N.A.; Hughes, M.S.; Adams, K.T.; Pacak, K. Exercise-induced nausea and vomiting: Another sign and symptom of pheochromocytoma and paraganglioma. Endocrine 2010, 37, 403–407. [Google Scholar] [CrossRef][Green Version]
- Patetsios, P.; Gable, D.R.; Garrett, W.V.; Lamont, J.P.; Kuhn, J.A.; Shutze, W.P.; Kourlis, H.; Grimsley, B.; Pearl, G.J.; Smith, B.L.; et al. Management of carotid body paragangliomas and review of a 30-year experience. Ann. Vasc. Surg. 2002, 16, 331–338. [Google Scholar] [CrossRef] [PubMed]
- Mancini, L.; Roncaroli, F. Malignant paraganglioma of the posterior mediastinum with 27 years follow-up. Pathologica 1997, 89, 184–188. [Google Scholar] [PubMed]
- Mayer, R.; Fruhwirth, J.; Beham, A.; Groell, R.; Poschauko, J.; Hackl, A. Radiotherapy as adjunct to surgery for malignant carotid body paragangliomas presenting with lymph node metastases. Strahlenther. Onkol. 2000, 176, 356–360. [Google Scholar] [CrossRef] [PubMed]
- Robertson, D.I.; Cooney, T.P. Malignant carotid body paraganglioma: Light and electron microscopic study of the tumor and its metastases. Cancer 1980, 46, 2623–2633. [Google Scholar] [CrossRef] [PubMed]
- Baez, J.C.; Jagannathan, J.P.; Krajewski, K.; O’Regan, K.; Zukotynski, K.; Kulke, M.; Ramaiya, N.H. Pheochromocytoma and paraganglioma: Imaging characteristics. Cancer Imaging 2012, 12, 153–162. [Google Scholar] [CrossRef]
- Moskovic, D.J.; Smolarz, J.R.; Stanley, D.; Jimenez, C.; Williams, M.D.; Hanna, E.Y.; Kupferman, M.E. Malignant head and neck paragangliomas: Is there an optimal treatment strategy? Head Neck Oncol. 2010, 2, 23. [Google Scholar] [CrossRef]
- Madeddu, C.; Gramignano, G.; Astara, G.; Demontis, R.; Sanna, E.; Atzeni, V.; Macciò, A. Pathogenesis and Treatment Options of Cancer Related Anemia: Perspective for a Targeted Mechanism-Based Approach. Front. Physiol. 2018, 9, 1294. [Google Scholar] [CrossRef]
- Maccio, A.; Madeddu, C.; Gramignano, G.; Mulas, C.; Tanca, L.; Cherchi, M.C.; Floris, C.; Omoto, I.; Barracca, A.; Ganz, T. The role of inflammation, iron, and nutritional status in cancer-related anemia: Results of a large, prospective, observational study. Haematologica 2015, 100, 124–132. [Google Scholar] [CrossRef]
- Macciò, A.; Madeddu, C.; Massa, D.; Mudu, M.C.; Lusso, M.R.; Gramignano, G.; Serpe, R.; Melis, G.B.; Mantovani, G. Hemoglobin levels correlate with interleukin-6 levels in patients with advanced untreated epithelial ovarian cancer: Role of inflammation in cancer-related anemia. Blood 2005, 106, 362–367. [Google Scholar] [CrossRef]
- Falkensammer, C.E.; Thurnher, M.; Leonhartsberger, N.; Ramoner, R. C-reactive protein is a strong predictor for anaemia in renal cell carcinoma: Role of IL-6 in overall survival: CRP and anaemia in renal cell carcinoma. BJU Int. 2011, 107, 1893–1898. [Google Scholar] [CrossRef]
- Sweet, R.A.; Fairbairn, J.F.; Joyce, J.W.; Goellner, J.R. Chemodectoma with multiple skeletal metastasis and anemia. Minn. Med. 1976, 59, 844–848. [Google Scholar] [PubMed]
- Schwartz, M.L.; Israel, H.L. Severe anemia as a manifestation of metastatic jugular paraganglioma. Arch. Otolaryngol. 1983, 109, 269–272. [Google Scholar] [CrossRef] [PubMed]
- el Allame, L.; Belkhayat, S.; Chkoff, L.; Mechatt, F.; Chkoff, M.R.; Benchkroun, B.A.; Assem, A.; Balafrej, A.; Sebti, F.; Balafrej, S. Spontaneous hemoperitoneum complicating intraperitoneal paraganglioma. J. Chir. 1989, 126, 242–247. [Google Scholar]
- Mutabagani, K.H.; Klopfenstein, K.J.; Hogan, M.J.; Caniano, D.A. Metastatic paraganglioma and paraneoplastic-induced anemia in an adolescent: Treatment with hepatic arterial chemoembolization. J. Pediatr. Hematol. Oncol. 1999, 21, 544–547. [Google Scholar] [CrossRef] [PubMed]
- Sauseng, W.; Benesch, M.; Lackner, H.; Urban, C.; Kronberger, M.; Gadner, H.; Höllwarth, M.; Spuller, E.; Aschauer, M.; Horcher, E. Clinical, radiological, and pathological findings in four children with gastrointestinal stromal tumors of the stomach. Pediatr. Hematol. Oncol. 2007, 24, 209–219. [Google Scholar] [CrossRef]
- Uchida, D.; Ogawa, T.; Ueki, T.; Kominami, Y.; Numata, N.; Matsusita, H.; Morimoto, Y.; Nakarai, A.; Ota, S.; Nanba, S.; et al. A case of gangliocytic paraganglioma with lymphoid metastasis. Nihon Shokakibyo Gakkai Zasshi 2010, 107, 1456–1465. [Google Scholar]
- Sandmann, M.; Fähndrich, M.; Lorenzen, J.; Heike, M. Gangliocytic paraganglioma—A rare cause of an upper gastrointestinal bleeding. Z. Gastroenterol. 2010, 48, 1297–1300. [Google Scholar] [CrossRef]
- Boeriu, A.; Dobru, D.; Georgescu, R.; Mocan, S.; Boeriu, C. Gangliocytic paraganglioma: A rare cause of gastrointestinal bleeding. J. Gastrointest. Liver Dis. 2015, 24, 109–112. [Google Scholar] [CrossRef]
- Oya, S.; Yamasaki, Y.; Nakamura, T.; Morishige, S.; Yamaguchi, M.; Aoyama, K.; Seki, R.; Mouri, H.; Osaki, K.; Naito, Y.; et al. Interleukin-6-producing paraganglioma mimicking multicentric Castleman disease. Rinsho Ketsueki 2020, 61, 1605–1610. [Google Scholar] [CrossRef]
- Al Atrash, E.; Abdullah, M.F.; Pressey, J.; Mohan, S. GIST presenting as refractory iron-deficiency anaemia in paediatric patient. BMJ Case Rep. 2022, 15, e248365. [Google Scholar] [CrossRef]
- Effat, K.G.; Karam, M. Jugulotympanic paraganglioma (glomus tumour) presenting with recurrent epistaxis. J. Laryngol. Otol. 2004, 118, 153–155. [Google Scholar] [CrossRef]
- Lin, P.; Shih, H.; Chen, Y.; Chang, Y. Iron-deficiency anemia caused by duodenal paraganglioma in an adolescent. Kaohsiung J. Med. Sci. 2022, 38, 716–718. [Google Scholar] [CrossRef] [PubMed]
- Dong, Z.R.; Xia, Y.N.; Zhao, Y.Y.; Wu, R.; Liu, K.-X.; Shi, K.; Yan, L.-J.; Yao, C.-Y.; Yan, Y.-C.; Li, T.; et al. Hepatic metastatic paraganglioma 12 years after retroperitoneal paraganglioma resection: A case report. BMC Gastroenterol. 2019, 19, 142. [Google Scholar] [CrossRef]
- Williams, M.D. Paragangliomas of the Head and Neck: An Overview from Diagnosis to Genetics. Head Neck Pathol. 2017, 11, 278–287. [Google Scholar] [CrossRef] [PubMed]
- Guilmette, J.; Sadow, P.M. A Guide to Pheochromocytomas and Paragangliomas. Surg. Pathol. Clin. 2019, 12, 951–965. [Google Scholar] [CrossRef] [PubMed]
- Albsoul, N.; Alsmady, M.; Al-Aardah, M.; Altaher, R. Carotid body paraganglioma management and outcome. Eur. J. Sci. Res. 2009, 37, 567–574. [Google Scholar]
- McCrary, H.C.; Babajanian, E.; Calquin, M.; Carpenter, P.; Casazza, G.; Naumer, A.; Greenberg, S.; Kohlmann, W.; Cannon, R.; Monroe, M.M.; et al. Characterization of Malignant Head and Neck Paragangliomas at a Single Institution Across Multiple Decades. JAMA Otolaryngol. Head Neck Surg. 2019, 145, 641. [Google Scholar] [CrossRef]
- Sobol, S.M.; Dailey, J.C. Familial Multiple Cervical Paragangliomas: Report of a Kindred and Review of the Literature. Otolaryngol.-Head Neck Surg. 1990, 102, 382–390. [Google Scholar] [CrossRef]
- Sykes, J.M.; Ossoff, R.H. Paragangliomas of the Head and Neck. Otolaryngol. Clin. N. Am. 1986, 19, 755–767. [Google Scholar] [CrossRef]
- Davidovic, L.B.; Djukic, V.B.; Vasic, D.M.; Sindjelic, R.P.; Duvnjak, S.N. Diagnosis and treatment of carotid body paraganglioma: 21 years of experience at a clinical center of Serbia. World J. Surg. Oncol. 2005, 3, 10. [Google Scholar] [CrossRef]
- Lee, J.H.; Barich, F.; Karnell, L.H.; Robinson, R.A.; Zhen, W.K.; Gantz, B.J.; Hoffman, H.T. National Cancer Data Base report on malignant paragangliomas of the head and neck. Cancer 2002, 94, 730–737. [Google Scholar] [CrossRef] [PubMed]
- Fliedner, S.M.J.; Lehnert, H.; Pacak, K. Metastatic Paraganglioma. Semin. Oncol. 2010, 37, 627–637. [Google Scholar] [CrossRef] [PubMed]
- Sajid, M.S.; Hamilton, G.; Baker, D.M.; Joint Vascular Research Group. A multicenter review of carotid body tumour management. Eur. J. Vasc. Endovasc. Surg. 2007, 34, 127–130. [Google Scholar] [CrossRef]
- Makiese, O.; Chibbaro, S.; Marsella, M.; Tran Ba Huy, P.; George, B. Jugular foramen paragangliomas: Management, outcome and avoidance of complications in a series of 75 cases. Neurosurg. Rev. 2012, 35, 185–194; discussion 194. [Google Scholar] [CrossRef] [PubMed]
- Huy, P.T.B.; Kania, R.; Duet, M.; Dessard-Diana, B.; Mazeron, J.J.; Benhamed, R. Evolving concepts in the management of jugular paraganglioma: A comparison of radiotherapy and surgery in 88 cases. Skull Base 2009, 19, 83–91. [Google Scholar] [CrossRef]
- Papaspyrou, K.; Mann, W.J.; Amedee, R.G. Management of head and neck paragangliomas: Review of 120 patients. Head Neck 2009, 31, 381–387. [Google Scholar] [CrossRef]
- Makeieff, M.; Raingeard, I.; Alric, P.; Bonafe, A.; Guerrier, B.; Marty-Ane, C. Surgical management of carotid body tumors. Ann. Surg. Oncol. 2008, 15, 2180–2186. [Google Scholar] [CrossRef]
- Borba, L.A.B.; Araújo, J.C.; de Oliveira, J.G.; Filho, M.G.; Moro, M.S.; Tirapelli, L.F.; Colli, B.O. Surgical management of glomus jugulare tumors: A proposal for approach selection based on tumor relationships with the facial nerve. J. Neurosurg. 2010, 112, 88–98. [Google Scholar] [CrossRef]
- Fayad, J.N.; Keles, B.; Brackmann, D.E. Jugular foramen tumors: Clinical characteristics and treatment outcomes. Otol. Neurotol. 2010, 31, 299–305. [Google Scholar] [CrossRef]
- Glasscock, M.E. The history of glomus tumors: A personal perspective. Laryngoscope 1993, 103 Pt 2 (Suppl. S60), 3–6. [Google Scholar] [CrossRef]
- Lloyd, S.; Obholzer, R.; Tysome, J.; BSBS Consensus Group. British Skull Base Society Clinical Consensus Document on Management of Head and Neck Paragangliomas. Otolaryngol. Head Neck Surg. 2020, 163, 400–409. [Google Scholar] [CrossRef]
- Persky, M.S.; Setton, A.; Niimi, Y.; Hartman, J.; Frank, D.; Berenstein, A. Combined endovascular and surgical treatment of head and neck paragangliomas—A team approach. Head Neck 2002, 24, 423–431. [Google Scholar] [CrossRef] [PubMed]
- Foote, R.L.; Pollock, B.E.; Gorman, D.A.; Schomberg, P.J.; Stafford, S.L.; Link, M.J.; Kline, R.W.; Strome, S.E.; Kasperbauer, J.L.; Olsen, K.D. Glomus jugulare tumor: Tumor control and complications after stereotactic radiosurgery. Head Neck 2002, 24, 332–338; discussion 338–339. [Google Scholar] [CrossRef] [PubMed]
- Jansen, J.C.; van den Berg, R.; Kuiper, A.; van der Mey, A.G.; Zwinderman, A.H.; Cornelisse, C.J. Estimation of growth rate in patients with head and neck paragangliomas influences the treatment proposal. Cancer 2000, 88, 2811–2816. [Google Scholar] [CrossRef] [PubMed]
- Langerman, A.; Athavale, S.M.; Rangarajan, S.V.; Sinard, R.J.; Netterville, J.L. Natural history of cervical paragangliomas: Outcomes of observation of 43 patients. Arch. Otolaryngol. Head Neck Surg. 2012, 138, 341–345. [Google Scholar] [CrossRef] [PubMed]
- Kollert, M.; Minovi, A.A.; Draf, W.; Bockmühl, U. Cervical paragangliomas-tumor control and long-term functional results after surgery. Skull Base 2006, 16, 185–191. [Google Scholar] [CrossRef]
- Hinerman, R.W.; Amdur, R.J.; Morris, C.G.; Kirwan, J.; Mendenhall, W.M. Definitive radiotherapy in the management of paragangliomas arising in the head and neck: A 35-year experience. Head Neck 2008, 30, 1431–1438. [Google Scholar] [CrossRef]
- Zeng, G.; Zhao, J.; Ma, Y.; Huang, B. Resection of carotid body tumors and the additional choice of intraoperative shunt in complicated tumors. Ann. Vasc. Surg. 2012, 26, 511–515. [Google Scholar] [CrossRef]
- Lian, L.S.; Liu, C.W.; Guan, H.; Zheng, Y.H.; Chen, X.M.; Li, Y.J. Efficacy of surgical therapy for carotid body tumors. Chin. Med. Sci. J. 2011, 26, 241–245. [Google Scholar] [CrossRef]
- Miller, R.B.; Boon, M.S.; Atkins, J.P.; Lowry, L.D. Vagal paraganglioma: The Jefferson experience. Otolaryngol. Head Neck Surg. 2000, 122, 482–487. [Google Scholar] [CrossRef]
- Suárez, C.; Rodrigo, J.P.; Bödeker, C.C.; Llorente, J.L.; Silver, C.E.; Jansen, J.C.; Takes, R.P.; Strojan, P.; Pellitteri, P.K.; Rinaldo, A.; et al. Jugular and vagal paragangliomas: Systematic study of management with surgery and radiotherapy. Head Neck 2013, 35, 1195–1204. [Google Scholar] [CrossRef] [PubMed]
- Hallett, J.W.; Nora, J.D.; Hollier, L.H.; Cherry, K.J.; Pairolero, P.C. Trends in neurovascular complications of surgical management for carotid body and cervical paragangliomas: A fifty-year experience with 153 tumors. J. Vasc. Surg. 1988, 7, 284–291. [Google Scholar] [CrossRef] [PubMed]
- Chino, J.P.; Sampson, J.H.; Tucci, D.L.; Brizel, D.M.; Kirkpatrick, J.P. Paraganglioma of the head and neck: Long-term local control with radiotherapy. Am. J. Clin. Oncol. 2009, 32, 304–307. [Google Scholar] [CrossRef] [PubMed]
- Krych, A.J.; Foote, R.L.; Brown, P.D.; Garces, Y.I.; Link, M.J. Long-term results of irradiation for paraganglioma. Int. J. Radiat. Oncol. Biol. Phys. 2006, 65, 1063–1066. [Google Scholar] [CrossRef]
- Lightowlers, S.; Benedict, S.; Jefferies, S.J.; Jena, R.; Harris, F.; Burton, K.E.; Burnet, N.G. Excellent local control of paraganglioma in the head and neck with fractionated radiotherapy. Clin. Oncol. R Coll. Radiol. 2010, 22, 382–389. [Google Scholar] [CrossRef]
- Galland-Girodet, S.; Maire, J.P.; De-Mones, E.; Benech, J.; Bouhoreira, K.; Protat, B.; Demeaux, H.; Darrouzet, V.; Huchet, A. The role of radiation therapy in the management of head and neck paragangliomas: Impact of quality of life versus treatment response. Radiother. Oncol. 2014, 111, 463–467. [Google Scholar] [CrossRef]
- Paris, J.; Facon, F.; Thomassin, J.M.; Zanaret, M. Cervical paragangliomas: Neurovascular surgical risk and therapeutic management. Eur. Arch. Otorhinolaryngol. 2006, 263, 860–865. [Google Scholar] [CrossRef]
- Chan, W.S.; Wei, W.I.; Tse, H.F. “Malignant” baroreflex failure after surgical resection of carotid body tumor. Int. J. Cardiol. 2007, 118, e81–e82. [Google Scholar] [CrossRef]
- Maturo, S.; Brennan, J. Baroreflex failure: A rare complication of carotid paraganglioma surgery. Laryngoscope 2006, 116, 829–830. [Google Scholar] [CrossRef]
- Hamidi, O.; Young, W.F.; Iñiguez-Ariza, N.M.; Kittah, N.E.; Gruber, L.; Bancos, C.; Tamhane, S.; Bancos, I. Malignant Pheochromocytoma and Paraganglioma: 272 Patients Over 55 Years. J. Clin. Endocrinol. Metab. 2017, 102, 3296–3305. [Google Scholar] [CrossRef]
- Hu, K.; Persky, M.S. Multidisciplinary management of paragangliomas of the head and neck, Part 1. Oncology 2003, 17, 983–993. [Google Scholar] [PubMed]
- Plouin, P.F.; Chatellier, G.; Fofol, I.; Corvol, P. Tumor recurrence and hypertension persistence after successful pheochromocytoma operation. Hypertension 1997, 29, 1133–1139. [Google Scholar] [CrossRef] [PubMed]
- Favia, G.; Lumachi, F.; Polistina, F.; D’Amico, D.F. Pheochromocytoma, a rare cause of hypertension: Long-term follow-up of 55 surgically treated patients. World J. Surg. 1998, 22, 689–693; discussion 694. [Google Scholar] [CrossRef] [PubMed]
- van Heerden, J.A.; Roland, C.F.; Carney, J.A.; Sheps, S.G.; Grant, C.S. Long-term evaluation following resection of apparently benign pheochromocytoma(s)/paraganglioma(s). World J. Surg. 1990, 14, 325–329. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, S.; Ito, T.; Tomoda, J.; Higashi, T.; Yamada, G.; Tsuji, T. Malignant pheochromocytoma with hepatic metastasis diagnosed 20 years after resection of the primary adrenal lesion. Intern. Med. 1993, 32, 789–794. [Google Scholar] [CrossRef] [PubMed]
- Amar, L.; Servais, A.; Gimenez-Roqueplo, A.P.; Zinzindohoue, F.; Chatellier, G.; Plouin, P.F. Year of diagnosis, features at presentation, and risk of recurrence in patients with pheochromocytoma or secreting paraganglioma. J. Clin. Endocrinol. Metab. 2005, 90, 2110–2116. [Google Scholar] [CrossRef]
- National Comprehensive Cancer Network (NCCN). NCCN Clinical Practice Guidelines in Oncology. Available online: https://www.nccn.org/professionals/physician_gls/pdf/genetics_bop.pdf (accessed on 2 September 2023).
| CRT. No. | Gender | Age | Location of Paraganglioma | Severity of Anemia | Type of Tumor | Metastases | Associated Pathology |
|---|---|---|---|---|---|---|---|
| 1 [42] | F | - | Glomus jugulare | Severe | Malignant | Lung | - |
| 2 [43] | M | 27 | Retroperitoneal | Severe | Benign | - | Hemoperitoneum |
| 3 [44] | M | 17 | Mediastinal | Severe | Benign | - | - |
| 4 [45] | M | - | Mediastinal | Moderate | Benign | - | GIST |
| 5 [46] | F | 67 | 2nd portion of duodenum | Moderate | Malignant | Lymph nodes | - |
| 6 [47] | F | 62 | 1st portion of duodenum | Severe | Benign | - | - |
| 7 [48] | M | 38 | 1st portion of duodenum | Severe | Benign | - | - |
| 8 [49] | M | 17 | Pelvic | Moderate | Benign | - | IL-6 secreting paraganglioma mimicking multicentric Castleman disease |
| 9 [50] | F | 9 | Gastric | Severe | Benign | - | GIST |
| 10 [51] | M | - | Jugulotympanic | Severe | Malignant | Extent to nasopharynx | - |
| 11 [52] | F | 19 | 4th portion of duodenum | Severe | Malignant | Pelvic | - |
| 12 [53] | F | 39 | Hepatic | Moderate | Benign | - | - |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tănăsescu, M.-D.; Popescu, Ș.; Mincă, A.; Isac, T.; Suliman, E.; Grigorie, M.M.; Suliman, E.; Stăniloaie, D.; Timofte, D.; Ionescu, D. Paragangliomas and Anemia: Literature Review and Case Report. Medicina 2023, 59, 1925. https://doi.org/10.3390/medicina59111925
Tănăsescu M-D, Popescu Ș, Mincă A, Isac T, Suliman E, Grigorie MM, Suliman E, Stăniloaie D, Timofte D, Ionescu D. Paragangliomas and Anemia: Literature Review and Case Report. Medicina. 2023; 59(11):1925. https://doi.org/10.3390/medicina59111925
Chicago/Turabian StyleTănăsescu, Maria-Daniela, Ștefan Popescu, Alexandru Mincă, Teodora Isac, Emel Suliman, Maria Mihaela Grigorie, Emine Suliman, Daniel Stăniloaie, Delia Timofte, and Dorin Ionescu. 2023. "Paragangliomas and Anemia: Literature Review and Case Report" Medicina 59, no. 11: 1925. https://doi.org/10.3390/medicina59111925
APA StyleTănăsescu, M.-D., Popescu, Ș., Mincă, A., Isac, T., Suliman, E., Grigorie, M. M., Suliman, E., Stăniloaie, D., Timofte, D., & Ionescu, D. (2023). Paragangliomas and Anemia: Literature Review and Case Report. Medicina, 59(11), 1925. https://doi.org/10.3390/medicina59111925





