Characteristics of Age Classification into Five-Year Intervals to Explain Sarcopenia and Immune Cells in Older Adults
Abstract
:1. Introduction
2. Materials and Methods
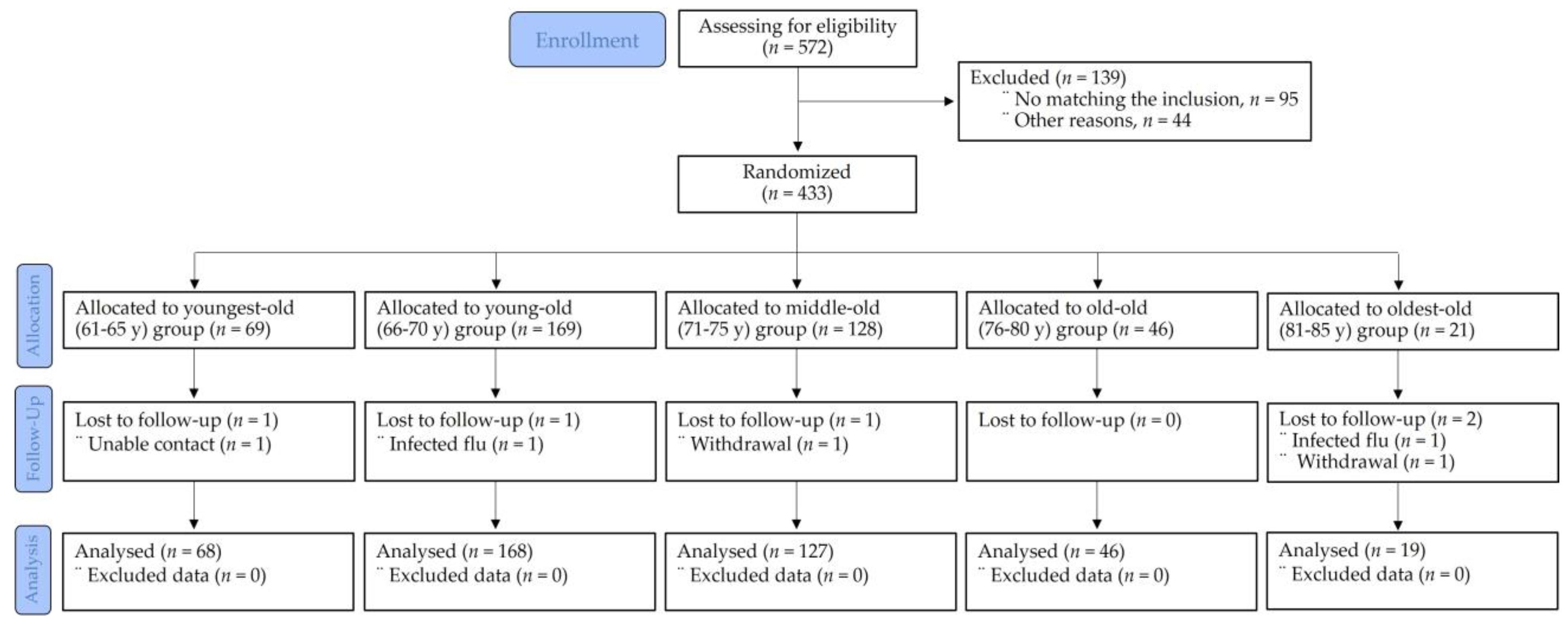
2.1. Study Design and Participants
2.2. Daily Physical Activity Measurements
2.3. Anthropometric Measurements
2.4. Sarcopenia Measures
2.5. Immunocyte Measures
2.6. Data Analyses
3. Results
3.1. Demographic, Anthropometric, and Clinical Characteristics
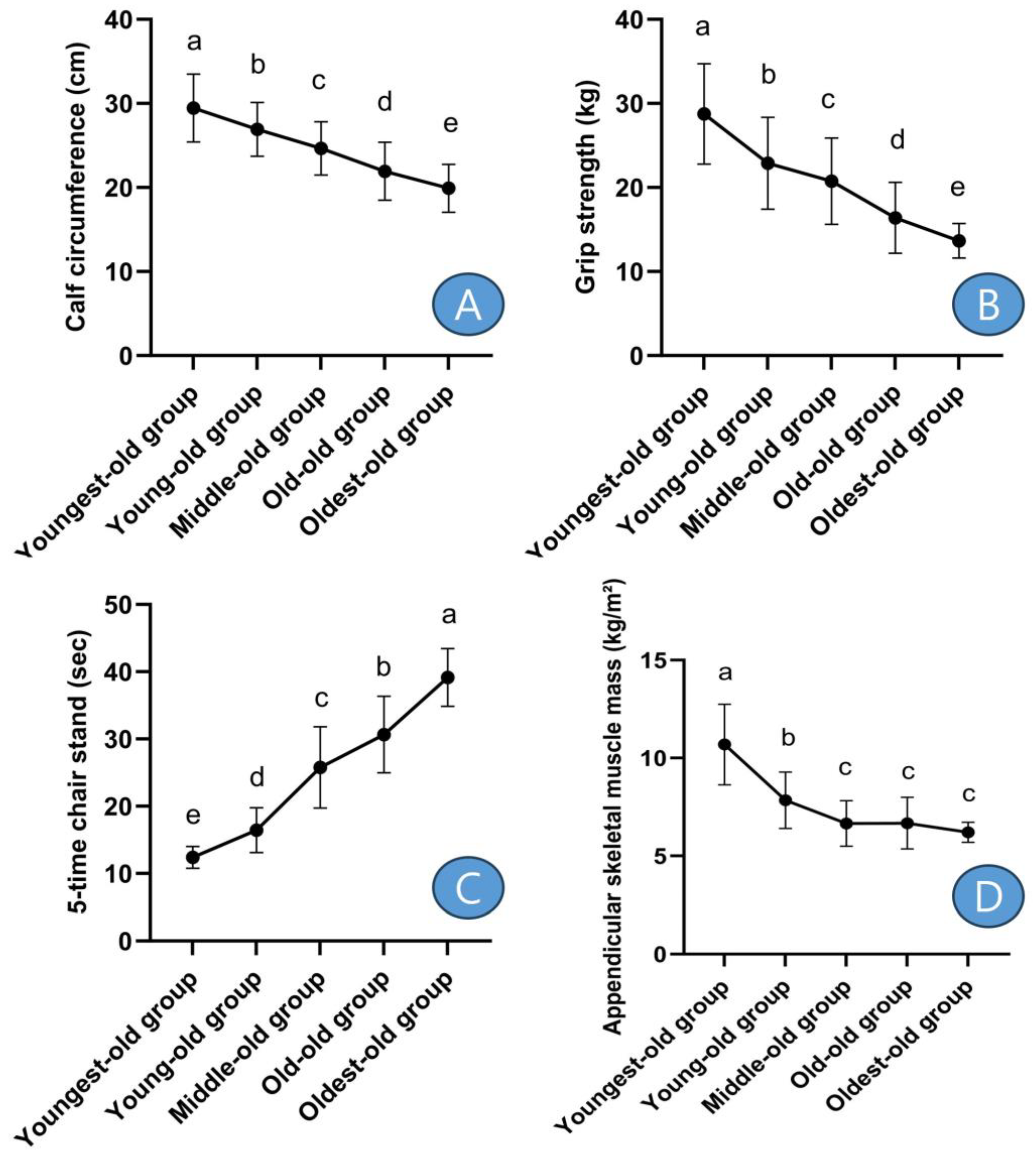
3.2. Comparative Results of Sarcopenic Factors
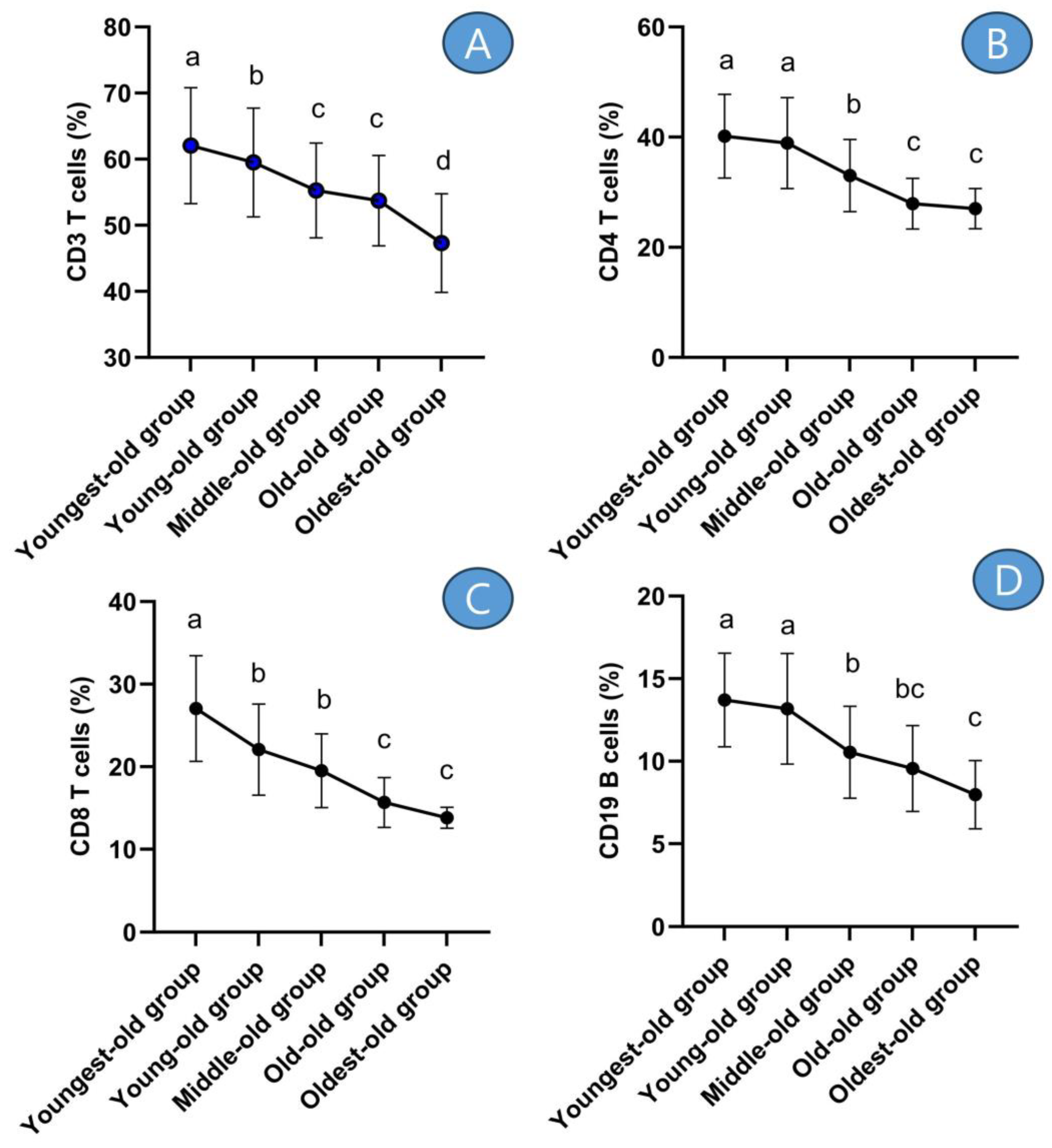
3.3. Comparative Results of Lymphocyte Subsets
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Vogelsang, E.M.; Raymo, J.M.; Liang, J.; Kobayashi, E.; Fukaya, T. Population Aging and Health Trajectories at Older Ages. J. Gerontol. B Psychol. Sci. Soc. Sci. 2019, 74, 1245–1255. [Google Scholar] [CrossRef]
- Schulz, R.; Martire, L.M. Family caregiving of persons with dementia: Prevalence, health effects, and support strategies. Am. J. Geriatr. Psychiatry 2004, 12, 240–249. [Google Scholar] [CrossRef]
- Ory, M.; Hoffman, M.K.; Hawkins, M.; Sanner, B.; Mockenhaupt, R. Challenging aging stereotypes: Strategies for creating a more active society. Am. J. Prev. Med. 2003, 25 (Suppl. S2), 164–171. [Google Scholar] [CrossRef]
- Boeckxstaens, P.; De Graaf, P. Primary care and care for older persons: Position paper of the European Forum for Primary Care. Qual. Prim. Care 2011, 19, 369–389. [Google Scholar]
- Dear, B.F.; Scott, A.J.; Fogliati, R.; Gandy, M.; Karin, E.; Dudeney, J.; Nielssen, O.; McDonald, S.; Heriseanu, A.I.; Bisby, M.A.; et al. The Chronic Conditions Course: A Randomised Controlled Trial of an Internet-Delivered Transdiagnostic Psychological Intervention for People with Chronic Health Conditions. Psychother. Psychosom. 2022, 91, 265–276. [Google Scholar] [CrossRef]
- Mijnarends, D.M.; Luiking, Y.C.; Halfens, R.J.G.; Evers, S.M.A.A.; Lenaerts, E.L.A.; Verlaan, S.; Wallace, M.; Schols, J.M.G.A.; Meijers, J.M.M. Muscle, Health and Costs: A Glance at their Relationship. J. Nutr. Health Aging 2018, 22, 766–773. [Google Scholar] [CrossRef]
- Chen, L.K.; Woo, J.; Assantachai, P.; Auyeung, T.W.; Chou, M.Y.; Iijima, K.; Jang, H.C.; Kang, L.; Kim, M.; Kim, S.; et al. Asian Working Group for Sarcopenia: 2019 consensus update on sarcopenia diagnosis and treatment. J. Am. Med. Dir. Assoc. 2020, 21, 300–307e2. [Google Scholar] [CrossRef]
- Cruz-Jentoft, A.J.; Landi, F.; Topinková, E.; Michel, J.P. Understanding sarcopenia as a geriatric syndrome. Curr. Opin. Clin. Nutr. Metab Care 2010, 13, 1–7. [Google Scholar] [CrossRef]
- Cruz-Jentoft, A.J.; Bahat, G.; Bauer, J.; Boirie, Y.; Bruyère, O.; Cederholm, T.; Cooper, C.; Landi, F.; Rolland, Y.; Sayer, A.A.; et al. Writing Group for the European Working Group on Sarcopenia in Older People 2 (EWGSOP2), and the Extended Group for EWGSOP2. Sarcopenia: Revised European consensus on definition and diagnosis. Age Ageing 2019, 48, 16–31. [Google Scholar] [CrossRef]
- Cosquéric, G.; Sebag, A.; Ducolombier, C.; Thomas, C.; Piette, F.; Weill-Engerer, S. Sarcopenia is predictive of nosocomial infection in care of the elderly. Br. J. Nutr. 2006, 96, 895–901. [Google Scholar] [CrossRef]
- Tidball, J.G.; Welc, S.S.; Wehling-Henricks, M. Immunobiology of Inherited Muscular Dystrophies. Compr. Physiol. 2018, 8, 1313–1356. [Google Scholar] [CrossRef]
- Nelke, C.; Dziewas, R.; Minnerup, J.; Meuth, S.G.; Ruck, T. Skeletal muscle as potential central link between sarcopenia and immune senescence. EBioMedicine 2019, 49, 381–388. [Google Scholar] [CrossRef]
- Thériault, M.E.; Paré, M.È.; Maltais, F.; Debigaré, R. Satellite cells senescence in limb muscle of severe patients with COPD. PLoS ONE 2012, 7, e39124. [Google Scholar] [CrossRef]
- Cheng, H.L. A simple, Easy-to-Use Spreadsheet for Automatic Scoring of the International Physical Activity Questionnaire (IPAQ) Short Form. 2016. Available online: https://www.researchgate.net/publication/310953872_A_simple_easy-touse_spreadsheet_for_automatic_scoring_of_the_International_Physical_Activity_Questionnaire_IPAQ_Short_Form (accessed on 6 June 2023).
- He, H.; Pan, L.; Wang, D.; Liu, F.; Du, J.; Pa, L.; Wang, X.; Cui, Z.; Ren, X.; Wang, H.; et al. Normative values of hand grip strength in a large unselected Chinese population: Evidence from the China National Health Survey. J. Cachexia Sarcopenia Muscle 2023, 14, 1312–1321. [Google Scholar] [CrossRef]
- Wu, X.; Li, X.; Xu, M.; Zhang, Z.; He, L.; Li, Y. Sarcopenia prevalence and associated factors among older Chinese population: Findings from the China Health and Retirement Longitudinal Study. PLoS ONE 2021, 16, e0247617. [Google Scholar] [CrossRef]
- Heo, S.J.; Park, S.K.; Jee, Y.S. Effects of phytoncide on immune cells and psychological stress of gynecological cancer survivors: Randomized controlled trials. J. Exerc. Rehabil. 2023, 19, 170–180. [Google Scholar] [CrossRef]
- Park, S.; Park, S.K.; Jee, Y.S. Moderate- to fast-walking improves immunocytes through a positive change of muscle contractility in old women: A pilot study. J. Exerc. Rehabil. 2023, 19, 45–56. [Google Scholar] [CrossRef]
- Jee, Y.S. Influences of acute and/or chronic exercise on human immunity: Third series of scientific evidence. J. Exerc. Rehabil. 2020, 16, 205–206. [Google Scholar] [CrossRef]
- Franceschi, C.; Garagnani, P.; Parini, P.; Giuliani, C.; Santoro, A. Inflammaging: A new immune-metabolic viewpoint for age-related diseases. Nat. Rev. Endocrinol. 2018, 14, 576–590. [Google Scholar] [CrossRef]
- Cohen, J. A power primer. Psychol. Bull. 1992, 112, 155–159. [Google Scholar] [CrossRef]
- Rolland, Y.; Czerwinski, S.; Van Kan, G.A.; Morley, J.E.; Cesari, M.; Onder, G.; Woo, J.; Baumgartner, R.; Pillard, F.; Boirie, Y.; et al. Sarcopenia: Its assessment, etiology, pathogenesis, consequences and future perspectives. J. Nutr. Health Aging 2008, 12, 433–450. [Google Scholar] [CrossRef] [PubMed]
- Cruz-Jentoft, A.J.; Baeyens, J.P.; Bauer, J.M.; Boirie, Y.; Cederholm, T.; Landi, F.; Martin, F.C.; Michel, J.P.; Rolland, Y.; Schneider, S.M.; et al. Sarcopenia: European consensus on definition and diagnosis: Report of the European Working Group on Sarcopenia in Older People. Age Ageing 2010, 39, 412–423. [Google Scholar] [CrossRef] [PubMed]
- Gallagher, D.; Visser, M.; De Meersman, R.E.; Sepúlveda, D.; Baumgartner, R.N.; Pierson, R.N.; Harris, T.; Heymsfield, S.B. Appendicular skeletal muscle mass: Effects of age, gender, and ethnicity. J. Appl. Physiol. 1997, 83, 229–239. [Google Scholar] [CrossRef] [PubMed]
- D’Onofrio, G.; Cseri, J. (Eds.) Frailty and Sarcopenia: Recent Evidence and New Perspectives; Books on Demand GmbH: Norderstedt, Germany, 2022. [Google Scholar]
- Weiskopf, D.; Weinberger, B.; Grubeck-Loebenstein, B. The aging of the immune system. Transpl. Int. 2009, 22, 1041–1050. [Google Scholar] [CrossRef]
- Vitlic, A.; Lord, J.M.; Phillips, A.C. Stress, ageing and their influence on functional, cellular and molecular aspects of the immune system. Age 2014, 36, 9631. [Google Scholar] [CrossRef]
- Olsson, J.; Wikby, A.; Johansson, B.; Löfgren, S.; Nilsson, B.O.; Ferguson, F.G. Age-related change in peripheral blood T-lymphocyte subpopulations and cytomegalovirus infection in the very old: The Swedish longitudinal OCTO immune study. Mech. Ageing Dev. 2000, 121, 187–201. [Google Scholar] [CrossRef]
- Freitas, G.R.R.; da Luz Fernandes, M.; Agena, F.; Jaluul, O.; Silva, S.C.; Lemos, F.B.C.; Coelho, V.; Elias, D.N.; Galante, N.Z. Aging and End Stage Renal Disease Cause A Decrease in Absolute Circulating Lymphocyte Counts with A Shift to A Memory Profile and Diverge in Treg Population. Aging Dis. 2019, 10, 49–61. [Google Scholar] [CrossRef]
- Zanni, F.; Vescovini, R.; Biasini, C.; Fagnoni, F.; Zanlari, L.; Telera, A.; Di Pede, P.; Passeri, G.; Pedrazzoni, M.; Passeri, M.; et al. Marked increase with age of type 1 cytokines within memory and effector/cytotoxic CD8+ T cells in humans: A contribution to understand the relationship between inflammation and immunosenescence. Exp. Gerontol. 2003, 38, 981–987. [Google Scholar] [CrossRef]
- Yang, W.; Hu, P. Skeletal muscle regeneration is modulated by inflammation. J. Orthop. Translat. 2018, 13, 25–32. [Google Scholar] [CrossRef]
- Gavazzi, G.; Herrmann, F.; Krause, K.H. Aging and infectious diseases in the developing world. Clin. Infect. Dis. 2004, 39, 83–91. [Google Scholar] [CrossRef]
- Griffin, W.S. Inflammation and neurodegenerative diseases. Am. J. Clin. Nutr. 2006, 83, 470S–474S. [Google Scholar] [CrossRef] [PubMed]
- Castelo-Branco, C.; Soveral, I. The immune system and aging: A review. Gynecol. Endocrinol. 2014, 30, 16–22. [Google Scholar] [CrossRef] [PubMed]
- Walsh, N.P.; Gleeson, M.; Pyne, D.B.; Nieman, D.C.; Dhabhar, F.S.; Shephard, R.J.; Oliver, S.J.; Bermon, S.; Kajeniene, A. Position statement. Part two: Maintaining immune health. Exerc. Immunol. Rev. 2011, 17, 64–103. [Google Scholar] [PubMed]

| Groups | p | η2 | |||||
|---|---|---|---|---|---|---|---|
| Youngest-Old | Young-Old | Middle-Old | Old-Old | Oldest-Old | |||
| Items | (n = 68) | (n = 168) | (n = 127) | (n = 46) | (n = 19) | ||
| Age (y) | 64.46 ± 1.11 | 67.57 ± 1.32 | 73.17 ± 1.38 | 77.61 ± 1.27 | 83.00 ± 1.53 | 0.001 | 0.933 |
| Height (cm) | 170.18 ± 4.30 | 169.32 ± 4.30 | 168.85 ± 5.00 | 167.85 ± 4.73 | 167.01 ± 4.13 | 0.003 | 0.039 |
| Body weight (kg) | 70.60 ± 6.37 | 73.84 ± 7.66 | 73.24 ± 7.96 | 73.55 ± 7.28 | 69.29 ± 8.04 | 0.009 | 0.032 |
| BMI (kg/m2) | 24.39 ± 2.23 | 25.79 ± 2.85 | 26.07 ± 3.39 | 25.84 ± 2.80 | 24.87 ± 3.06 | 0.002 | 0.038 |
| Lean mass (kg) | 48.65 ± 6.08 | 47.25 ± 5.21 | 47.20 ± 5.85 | 45.65 ± 4.36 | 41.71 ± 4.57 | 0.001 | 0.061 |
| Fat mass (kg) | 22.98 ± 3.46 | 22.60 ± 2.82 | 24.39 ± 3.32 | 26.37 ± 2.82 | 26.21 ± 3.16 | 0.001 | 0.156 |
| OV/OB | 0.44 ± 0.50 | 0.49 ± 0.50 | 0.55 ± 0.50 | 0.61 ± 0.49 | 0.63 ± 0.50 | 0.285 | 0.012 |
| DM | 0.18 ± 0.38 | 0.21 ± 0.41 | 0.18 ± 0.39 | 0.13 ± 0.34 | 0.16 ± 0.37 | 0.741 | 0.005 |
| HTN | 0.24 ± 0.43 c | 0.35 ± 0.48 b | 0.53 ± 0.50 b | 0.61 ± 0.49 a | 0.63 ± 0.50 a | 0.001 | 0.069 |
| HLD | 0.31 ± 0.47 | 0.30 ± 0.46 | 0.33 ± 0.47 | 0.22 ± 0.42 | 0.32 ± 0.48 | 0.717 | 0.005 |
| ARTH | 0.32 ± 0.47 | 0.51 ± 0.50 | 0.54 ± 0.50 | 0.54 ± 0.50 | 0.58 ± 0.51 | 0.041 | 0.023 |
| LBP | 0.26 ± 0.44 d | 0.32 ± 0.47 bc | 0.54 ± 0.50 bc | 0.61 ± 0.49 b | 0.68 ± 0.48 a | 0.001 | 0.078 |
| Groups | p | η2 | |||||
|---|---|---|---|---|---|---|---|
| Youngest-Old | Young-Old | Middle-Old | Old-Old | Oldest-Old | |||
| (n = 68) | (n = 168) | (n = 127) | (n = 46) | (n = 19) | |||
| Calf circumference (cm) | 29.44 ± 4.03 | 26.92 ± 3.18 | 24.66 ± 3.17 | 21.93 ± 3.46 | 19.90 ± 2.84 | 0.001 | 0.357 |
| Grip strength (kg) | 28.74 ± 5.97 | 22.89 ± 5.47 | 20.75 ± 5.13 | 16.39 ± 4.21 | 13.65 ± 2.05 | 0.001 | 0.348 |
| 5-time chair stand test (sec) | 12.40 ± 1.63 | 16.43 ± 3.33 | 25.77 ± 6.04 | 30.65 ± 5.68 | 39.16 ± 4.30 | 0.001 | 0.723 |
| ASM (kg/m2) | 10.69 ± 2.05 | 7.84 ± 1.44 | 6.65 ± 1.16 | 6.67 ± 1.32 | 6.20 ± 0.51 | 0.001 | 0.488 |
| Groups | p | η2 | |||||
|---|---|---|---|---|---|---|---|
| Youngest-Old | Young-Old | Middle-Old | Old-Old | Oldest-Old | |||
| (n = 68) | (n = 168) | (n = 127) | (n = 46) | (n = 19) | |||
| WBC (×103 cells/μL) | 5.99 ± 0.91 | 5.88 ± 0.71 | 5.71 ± 0.84 | 5.78 ± 0.82 | 5.80 ± 0.66 | 0.277 | 0.016 |
| NK cells (%) | 23.26 ± 4.67 | 17.92 ± 6.18 | 14.02 ± 5.12 | 10.33 ± 3.15 | 9.37 ± 3.02 | 0.001 | 0.371 |
| CD3 T cells (%) | 62.05 ± 8.76 | 59.52 ± 8.23 | 55.27 ± 7.16 | 53.74 ± 6.83 | 47.31 ± 7.46 | 0.001 | 0.170 |
| CD4 T cells (%) | 40.17 ± 7.60 | 38.94 ± 8.24 | 33.04 ± 6.56 | 27.93 ± 4.62 | 27.03 ± 3.65 | 0.001 | 0.274 |
| CD8 T cells (%) | 27.06 ± 6.41 | 22.07 ± 5.51 | 19.51 ± 4.46 | 15.68 ± 3.02 | 13.82 ± 1.28 | 0.001 | 0.328 |
| CD19 B cells (%) | 13.71 ± 2.83 | 13.18 ± 3.35 | 10.54 ± 2.78 | 9.56 ± 2.60 | 7.98 ± 2.07 | 0.001 | 0.253 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Heo, S.-J.; Jee, Y.-S. Characteristics of Age Classification into Five-Year Intervals to Explain Sarcopenia and Immune Cells in Older Adults. Medicina 2023, 59, 1700. https://doi.org/10.3390/medicina59101700
Heo S-J, Jee Y-S. Characteristics of Age Classification into Five-Year Intervals to Explain Sarcopenia and Immune Cells in Older Adults. Medicina. 2023; 59(10):1700. https://doi.org/10.3390/medicina59101700
Chicago/Turabian StyleHeo, Seung-Jae, and Yong-Seok Jee. 2023. "Characteristics of Age Classification into Five-Year Intervals to Explain Sarcopenia and Immune Cells in Older Adults" Medicina 59, no. 10: 1700. https://doi.org/10.3390/medicina59101700
APA StyleHeo, S.-J., & Jee, Y.-S. (2023). Characteristics of Age Classification into Five-Year Intervals to Explain Sarcopenia and Immune Cells in Older Adults. Medicina, 59(10), 1700. https://doi.org/10.3390/medicina59101700






