Evaluation of the Efficiency of Hand Hygiene Technique with Hydroalcoholic Solution by Image Color Summarize
Abstract
1. Introduction
2. Materials and Methods
2.1. Setting and Participants
2.2. Study Group
2.3. Demographic Characteristics
2.4. Domain: Knowledge Data
2.5. Materials
2.6. Protocol
2.6.1. Stage I
2.6.2. Stage II
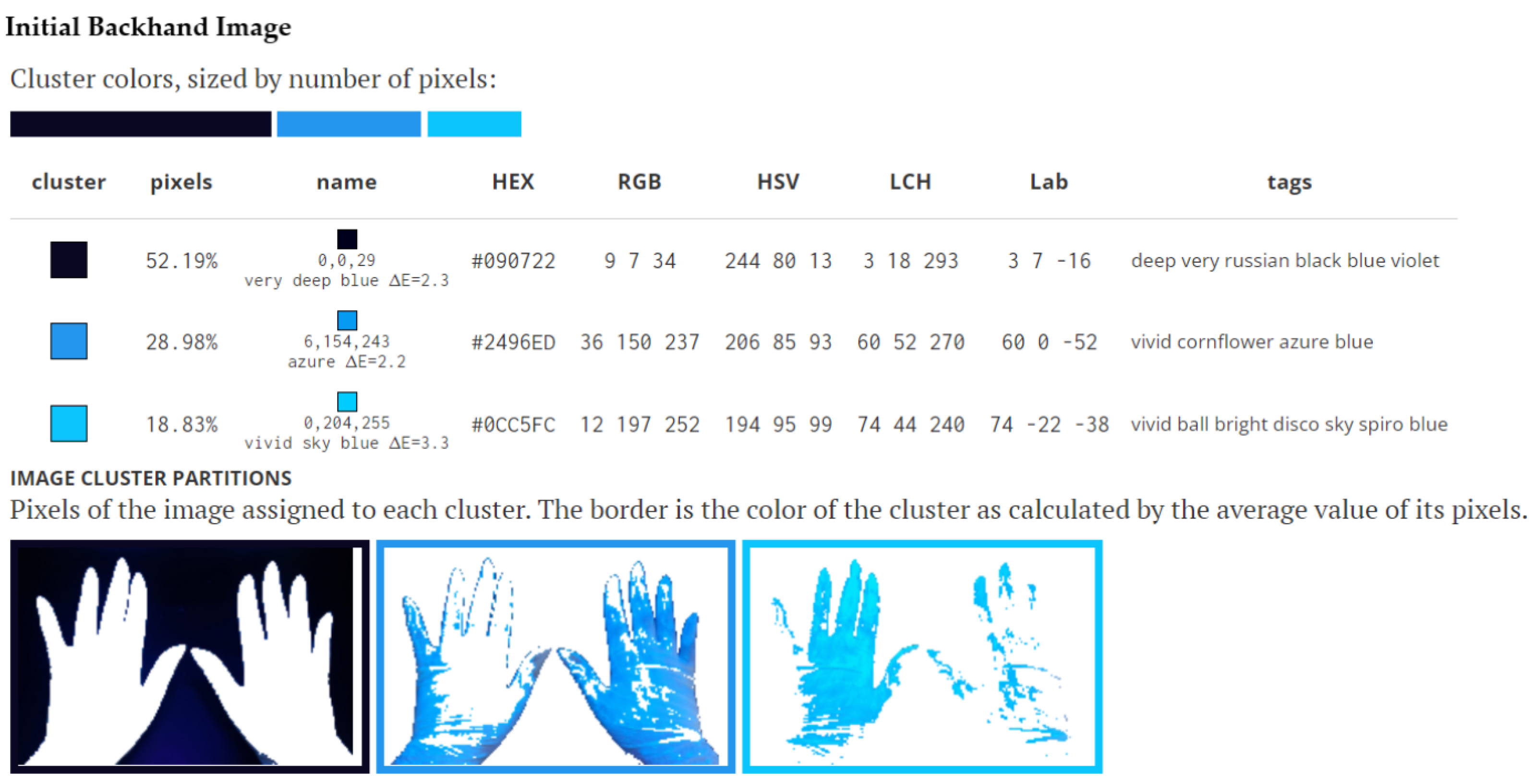
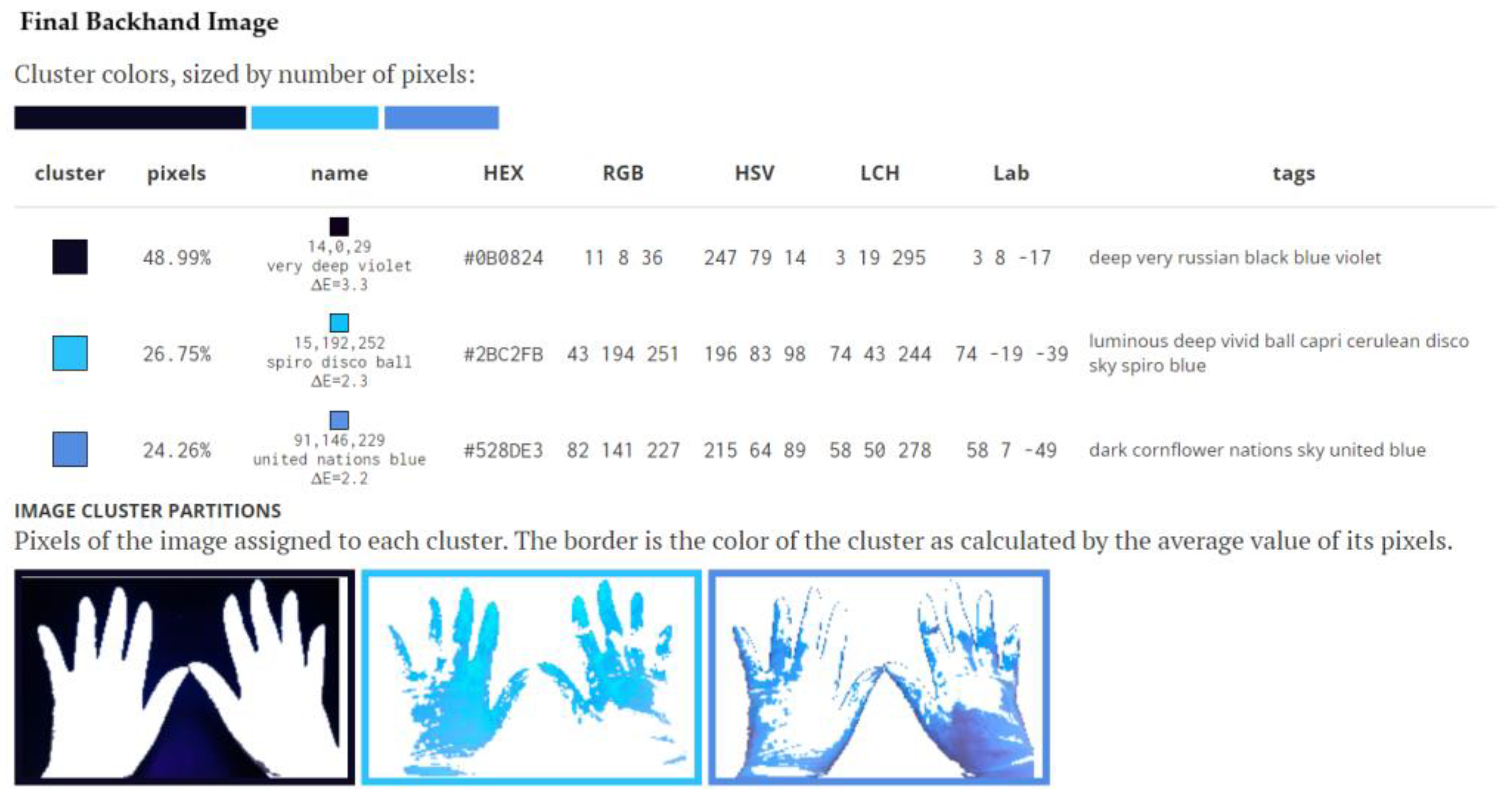
2.7. Data Collection
2.8. Statistical Data
3. Results
3.1. Demographic Data
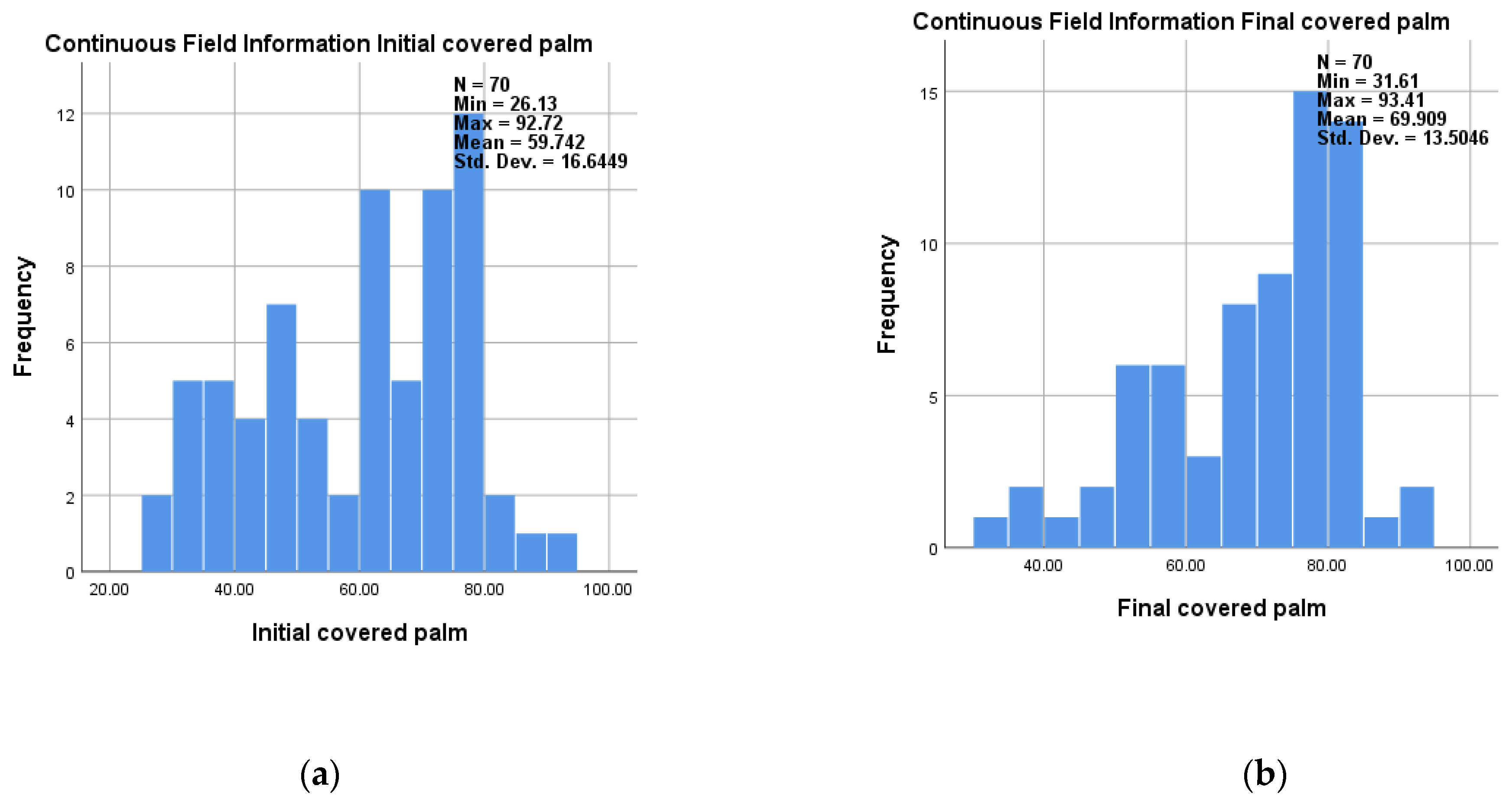
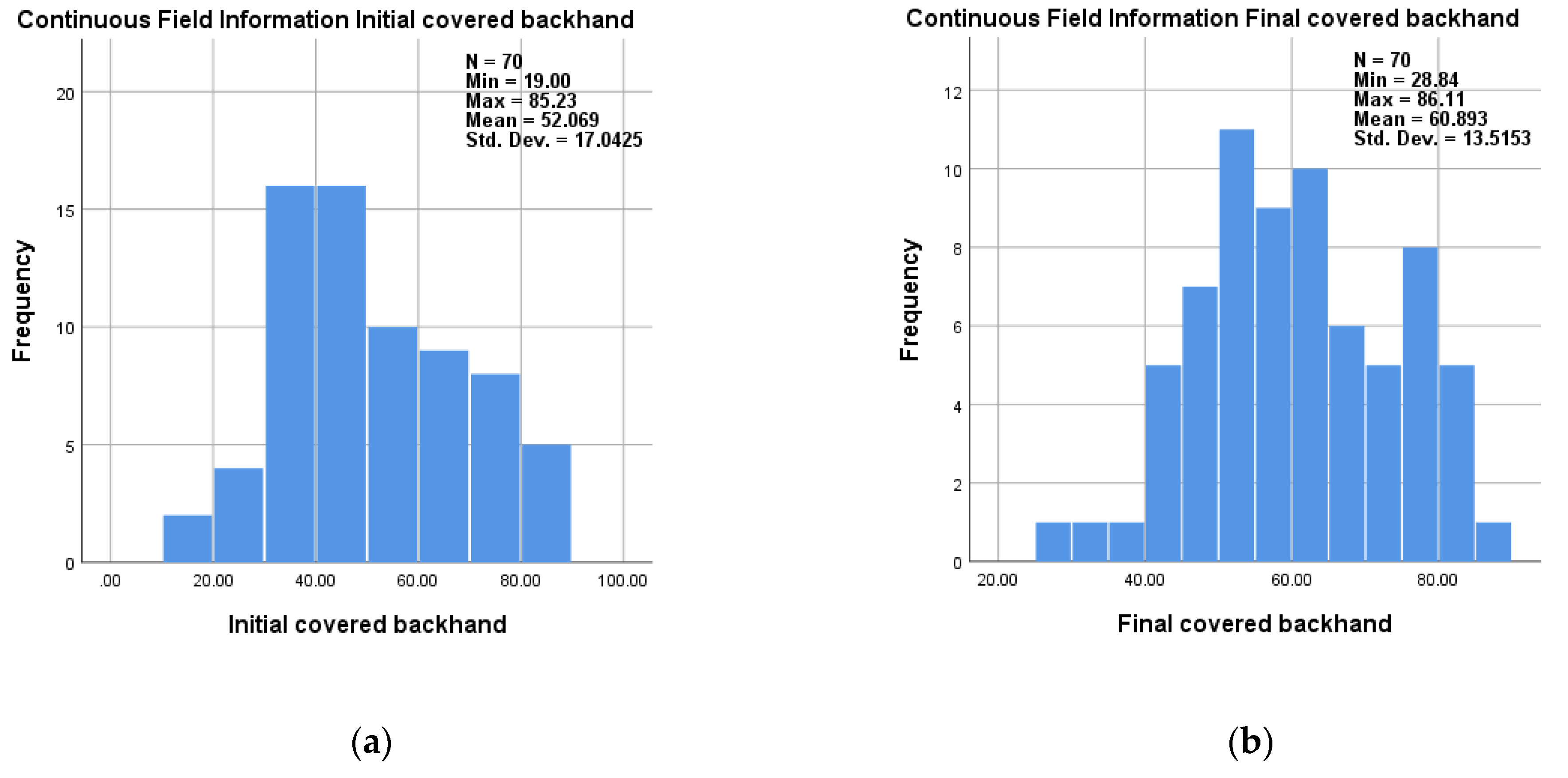
3.2. Descriptive Statistics of Analyzed Data
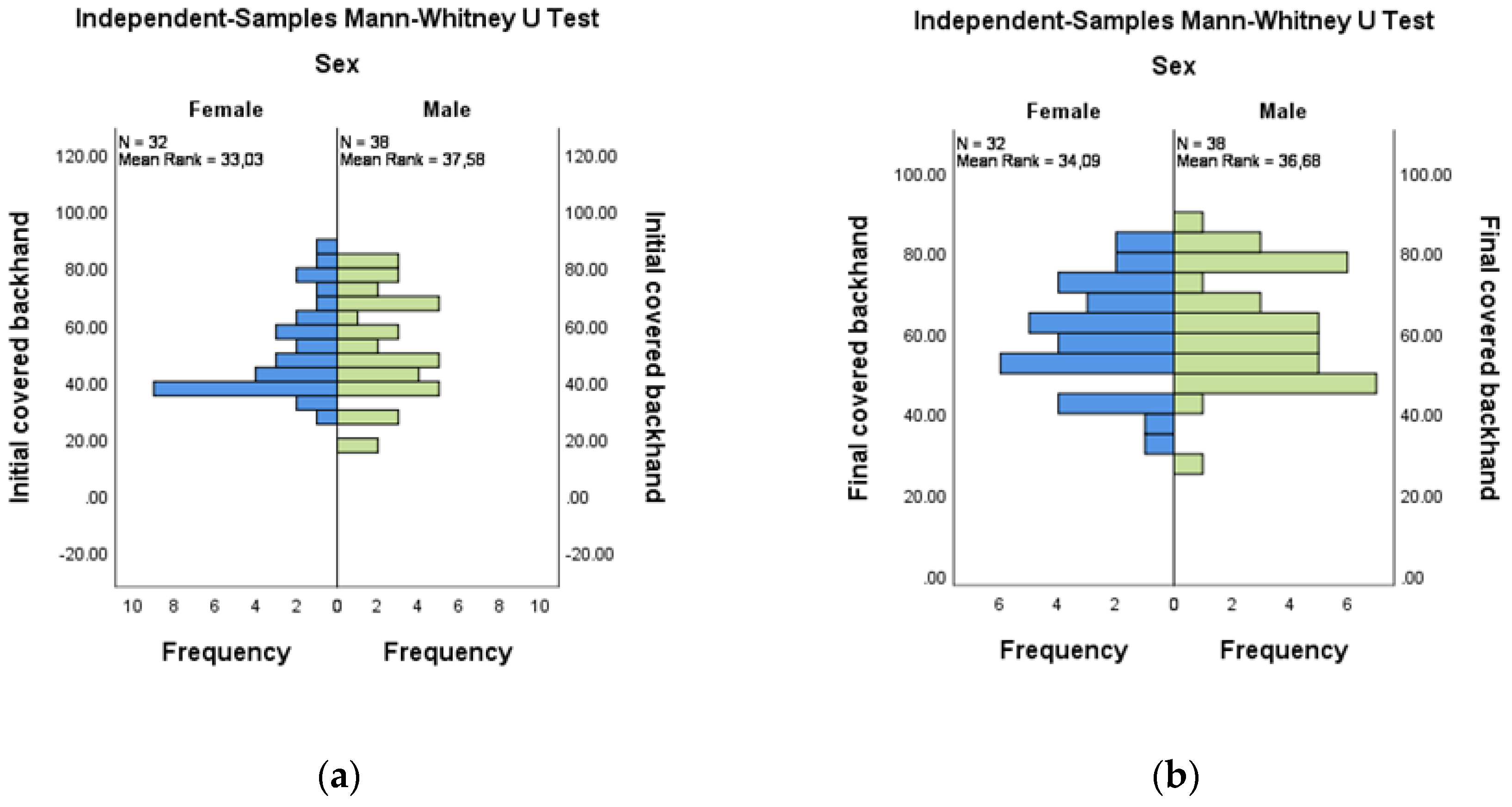
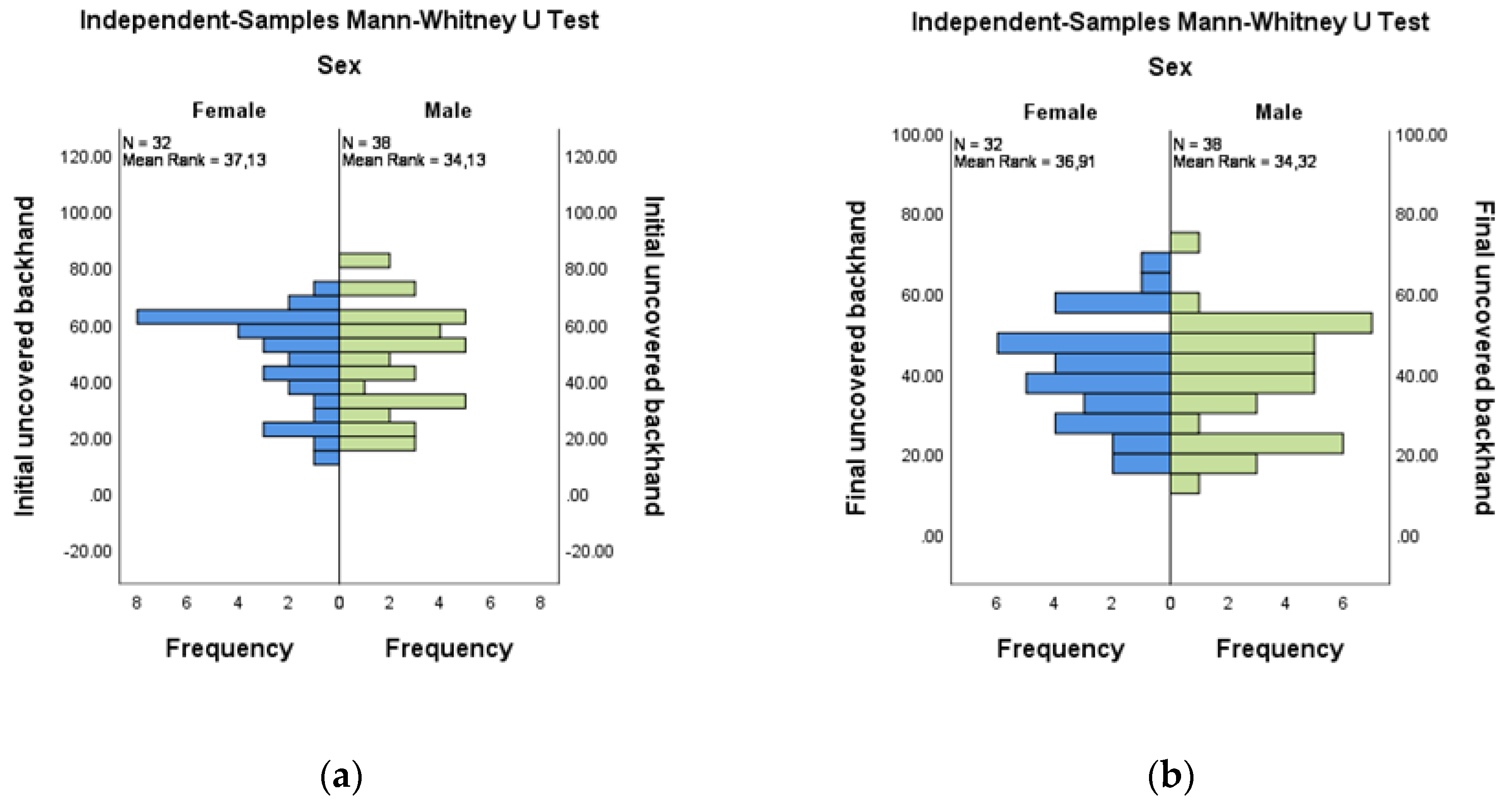
3.3. Comparative Evaluation of the Coverage Areas at the Backhands by Gender
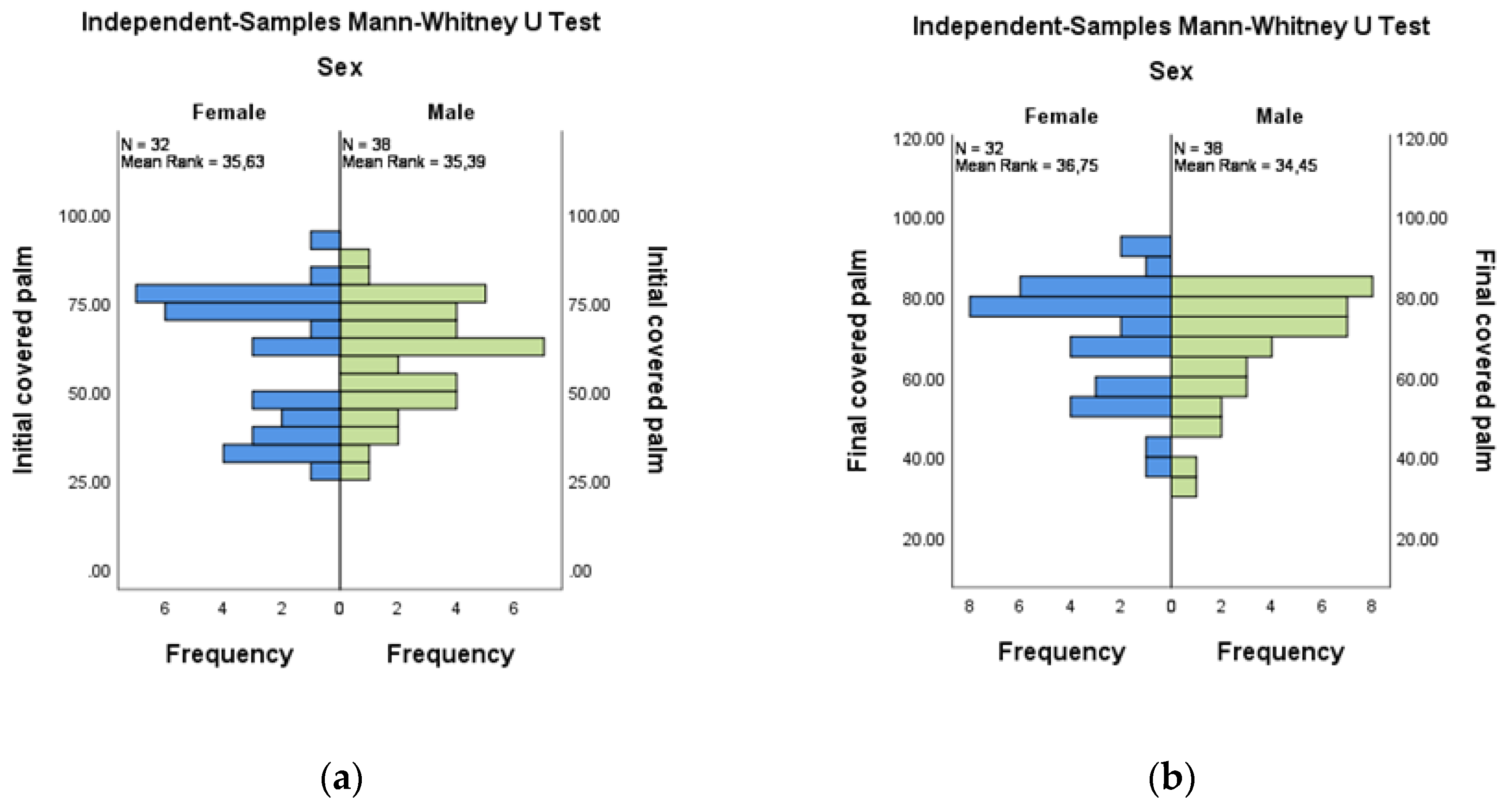
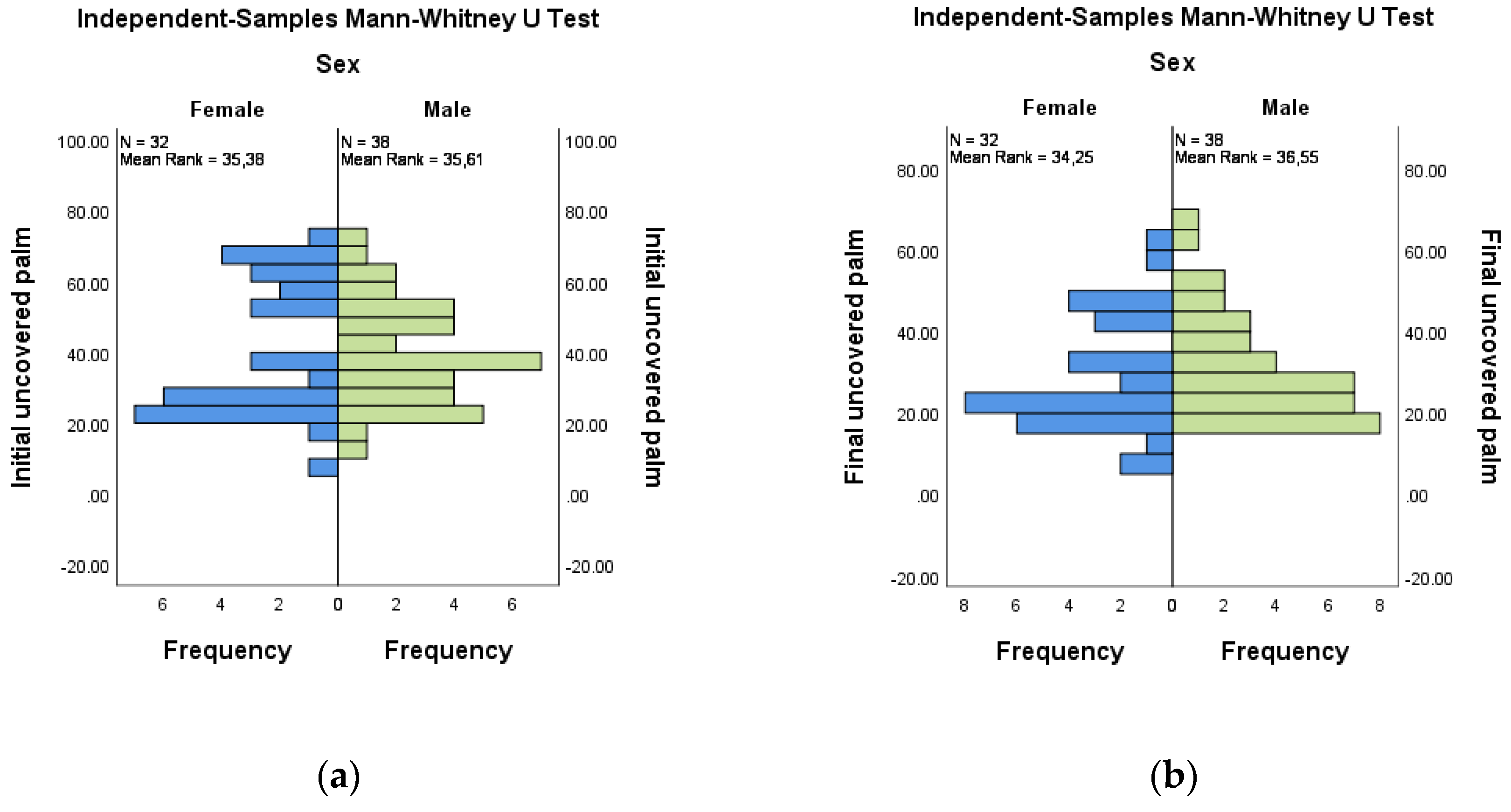
3.4. Evaluation of the Coverage Areas at the Palms
3.5. Comparative Analysis of the Studied Groups
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- WHO Guidelines on Hand Hygiene in Health Care: First Global Patient Safety Challenge Clean Care Is Safer Care; WHO-Recommended Hand Rub Formulations; World Health Organization: Geneva, Switzerland, 2009; p. 12. Available online: https://www.ncbi.nlm.nih.gov/books/NBK144054/ (accessed on 2 June 2022).
- Pittet, D.; Allegranzi, B.; Storr, J.; Donaldson, L. ‘Clean Care is Safer Care’: The Global Patient Safety Challenge 2005–2006. Int. J. Infect. Dis. 2006, 10, 419–424. [Google Scholar] [CrossRef]
- Fluent, M.T. Hand hygiene in the dental setting: Reducing the risk of infection. Compend. Contin. Educ. Dent. 2013, 34, 624–627. [Google Scholar]
- Babeluk, R.; Jutz, S.; Mertlitz, S.; Matiasek, J.; Klaus, C. Hand hygiene-evaluation of three disinfectant hand sanitizers in a community setting. PLoS ONE 2014, 9, e111969. [Google Scholar] [CrossRef]
- Kampf, G.; Kramer, A. Epidemiologic background of hand hygiene and evaluation of the most important agents for scrubs and rubs. Clin. Microbiol. Rev. 2004, 17, 863–893. [Google Scholar] [CrossRef]
- Boyce, J.; Pittet, D. Guideline for Hand Hygiene in Health-Care Settings: Recommendations of the Healthcare Infection Control Practices Advisory Committee and the HICPAC/SHEA/APIC/IDSA Hand Hygiene Task Force. Infect. Control. Hosp. Epidemiol. 2002, 23, S3–S40. [Google Scholar] [CrossRef]
- Widmer, A.F. Replace hand washing with use of a waterless alcohol hand rub? Clin. Infect. Dis. 2000, 31, 136–143. [Google Scholar] [CrossRef]
- Rotter, M.L. Arguments for alcoholic hand disinfection. J. Hosp. Infect. 2006, 48 (Suppl. A), S4–S8. [Google Scholar] [CrossRef]
- Voss, A.; Widmer, A.F. No time for handwashing!? Handwashing versus alcoholic rub: Can we afford 100% compliance? Infect. Control. Hosp. Epidemiol. 1997, 18, 205–208. [Google Scholar] [CrossRef]
- Pittet, D.; Hugonnet, S.; Harbarth, S.; Mourouga, P.; Sauvan, V.; Touveneau, S.; Perneger, T.V. Effectiveness of a hospital-wide programme to improve compliance with hand hygiene. Lancet 2000, 356, 1307–1312. [Google Scholar] [CrossRef]
- Zapka, C.; Leff, J.; Henley, J.; Tittl, J.; De Nardo, E.; Butler, M.; Griggs, R.; Fierer, N.; Edmonds-Wilson, S. Comparison of Standard Culture-Based Method to Culture-Independent Method for Evaluation of Hygiene Effects on the Hand Microbiome. mBio 2017, 8, e00093-17. [Google Scholar] [CrossRef]
- Mukherjee, P.K.; Chandra, J.; Retuerto, M.; Arters, K.A.; Consolo, M.C.; Patterson, A.; Bajaksouzian, S.; Arbogast, J.W.; Cartner, T.J.; Jacobs, M.R.; et al. Effect of alcohol-based hand rub on hand microbiome and hand skin health in hospitalized adult stem cell transplant patients: A pilot study. J. Am. Acad. Dermatol. 2018, 78, 1218–1221.e5. [Google Scholar] [CrossRef]
- Helder, O.K.; Brug, J.; Looman, C.W.; van Goudoever, J.B.; Kornelisse, R.F. The impact of an education program on hand hygiene compliance and nosocomial infection incidence in an urban neonatal intensive care unit: An intervention study with before and after comparison. Int. J. Nurs. Stud. 2010, 47, 1245–1252. [Google Scholar] [CrossRef]
- Tschudin-Sutter, S.; Sepulcri, D.; Dangel, M.; Ulrich, A.; Frei, R.; Widmer, A.F. Simplifying the World Health Organization Protocol: 3 Steps Versus 6 Steps for Performance of Hand Hygiene in a Cluster-randomized Trial. Clin. Infect. Dis. 2019, 69, 614–620. [Google Scholar] [CrossRef]
- Conway, L.; Moore, C.; Coleman, B.L.; McGeer, A. Frequency of hand hygiene opportunities in patients on a general surgery service. Am. J. Infect. Control 2020, 48, 490–495. [Google Scholar] [CrossRef]
- Stewardson, A.J.; Sax, H.; Gayet-Ageron, A.; Touveneau, S.; Longtin, Y.; Zingg, W.; Pittet, D. Enhanced performance feedback and patient participation to improve hand hygiene compliance of health-care workers in the setting of established multimodal promotion: A single-centre, cluster randomised controlled trial. Lancet Infect. Dis. 2016, 16, 1345–1355. [Google Scholar] [CrossRef]
- Albright, J.; White, B.; Pedersen, D.; Carlson, P.; Yost, L.; Littau, C. Use patterns and frequency of hand hygiene in healthcare facilities: Analysis of electronic surveillance data. Am. J. Infect. Control 2018, 46, 1104–1109. [Google Scholar] [CrossRef]
- Montoya, A.; Schildhouse, R.; Goyal, A.; Mann, J.D.; Snyder, A.; Chopra, V.; Mody, L. How often are health care personnel hands colonized with multidrug-resistant organisms? A systematic review and meta-analysis. Am. J. Infect. Control 2019, 47, 693–703. [Google Scholar] [CrossRef]
- Saveanu, C.I.; Porsega, A.; Anistoroaei, D.; Iordache, C.; Bobu, L.; Saveanu, A.E. Cross-Sectional Study to Evaluate Knowledge on Hand Hygiene in a Pandemic Context with SARS-CoV-2. Medicina 2022, 58, 304. [Google Scholar] [CrossRef] [PubMed]
- Available online: https://www.umfiasi.ro/ro/academic/programe-de-studii/licenta/Pagini/Student-Medicin%C4%83-dentar%C4%83.aspx (accessed on 24 May 2022).
- Xia, F.; Hughes, J.P.; Voldal, E.C.; Heagerty, P.J. Power and sample size calculation for stepped-wedge designs with discrete outcomes. Trials 2021, 22, 598. [Google Scholar] [CrossRef] [PubMed]
- Robinson, A.L.; Lee, H.J.; Kwon, J.; Todd, E.; Rodriguez, F.P.; Ryu, D. Adequate Hand Washing and Glove Use are Necessary To Reduce Cross-Contamination from Hands with High Bacterial Loads. J. Food Prot. 2016, 79, 304–308. [Google Scholar] [CrossRef] [PubMed]
- Martin Krzywinski Image Color Summarizer 0.76 © 2006–2022|mkweb.bcgsc.ca. Available online: http://mkweb.bcgsc.ca/color-summarizer/?analyze (accessed on 16 June 2022).
- Chinaramrungraung, C.; Yoosook, W.; Sujirarat, D.; Srisatjaluk, L.R. Bacteria decontamination after different hand hygiene procedures in dental assistants during patient care. Mahidol Dent. J. 2016, 36, 1–2. Available online: https://dt.mahidol.ac.th/th/wp-content/uploads/2017/08/Bacteria-decontamination-after-different-hand-hygiene.pdf (accessed on 16 June 2022).
- Bhatia, M.; Dehankar, D. Comparative Efficacy Of Hand Hygiene Techniques For Removing Bacteria From The Hands Of Health Care Workers With Microbiological Evaluation. Int. J. Life Sci. Pharma Res. 2017, 50, 10. Available online: https://www.ijlpr.com/admin/php/uploads/319_pdf.pdf (accessed on 17 June 2022).
- Zubair, M.; Zafar, A.; Yaqoob, A.; Javed, H.; Ejaz, H. Comparison of Different Hand Washing Techniques To Control Transmission Of Microorganisms. Pak. J. Med. Health Sci. 2017, 11, 1118–1120. Available online: https://www.pjmhsonline.com/2017/july_sep/pdf/1118.pdf (accessed on 17 June 2022).
- Holton, R.H.; Huber, M.A.; Terezhalmy, G.T. Antimicrobial efficacy of soap and water hand washing versus an alcohol-based hand cleanser. Tex. Dent. J. 2009, 126, 1175–1180. [Google Scholar]
- Khairnar, M.R.G.A.; Dalvi, T.M.; Kalghatgi, S.; Datar, U.V.; Wadgave, U.; Shah, S.; Preet, L. Comparative Efficacy of Hand Disinfection Potential of Hand Sanitizer and Liquid Soap among Dental Students: A Randomized Controlled Trial. Indian J. Crit. Care Med. 2020, 24, 336–339. [Google Scholar] [CrossRef]
- da Silveira, E.A.; Bubeck, K.A.; Batista, E.R.; Piat, P.; Laverty, S.; Beauchamp, G.; Archambault, M.; Elce, Y. Comparison of an alcohol-based hand rub and water-based chlorhexidine gluconate scrub technique for hand antisepsis prior to elective surgery in horses. Can. Vet. J. 2016, 57, 164–168. [Google Scholar]
- Bischoff, W.E.; Reynolds, T.M.; Sessler, C.N.; Edmond, M.B.; Wenzel, R.P. Handwashing compliance by health care workers: The impact of introducing an accessible, alcohol-based hand antiseptic. Arch. Intern. Med. 2000, 160, 1017–1021. [Google Scholar] [CrossRef]
- Stauffer, F.; Griess, M.; Pleininger, G.; Zhumadilova, A.; Assadian, O. Acceptability and tolerability of liquid versus gel and standard versus virucidal alcohol-based hand rub formulations among dental students. Am. J. Infect. Control 2013, 41, 1007–1011. [Google Scholar] [CrossRef]
- Mahasneh, A.M.; Alakhras, M.; Khabour, O.F.; Al-Sa’di, A.G.; Al-Mousa, D.S. Practices of Infection Control Among Dental Care Providers: A Cross Sectional Study. Clin. Cosmet. Investig. Dent. 2020, 12, 281–289. [Google Scholar] [CrossRef] [PubMed]
- Huber, M.A.; Holton, R.H.; Terezhalmy, G.T. Cost analysis of hand hygiene using antimicrobial soap and water versus an alcohol-based hand rub. J. Contemp. Dent. Pract. 2006, 7, 37–45. [Google Scholar] [CrossRef] [PubMed]
- Chow, A.; Arah, O.A.; Chan, S.P.; Poh, B.F.; Krishnan, P.; Ng, W.K.; Choudhury, S.; Chan, J.; Ang, B. Alcohol handrubbing and chlorhexidine handwashing protocols for routine hospital practice: A randomized clinical trial of protocol efficacy and time effectiveness. Am. J. Infect. Control 2012, 40, 800–805. [Google Scholar] [CrossRef] [PubMed]
- Reilly, J.S.; Price, L.; Lang, S.; Robertson, C.; Cheater, F.; Skinner, K.; Chow, A. A Pragmatic Randomized Controlled Trial of 6-Step VS 3-Step Hand Hygiene Technique in Acute Hospital Care in the United Kingdom. Infect. Control. Hosp. Epidemiol. 2016, 37, 661–666. [Google Scholar] [CrossRef] [PubMed]
- Tschudin-Sutter, S.; Rotter, M.L.; Frei, R.; Nogarth, D.; Häusermann, P.; Stranden, A.; Pittet, D.; Widmer, A.F. Simplifying the WHO ‘how to hand rub’ technique: Three steps are as effective as six-results from an experimental randomized crossover trial. Clin. Microbiol. Infect. 2017, 23, 409.e1–409.e4. [Google Scholar] [CrossRef] [PubMed]
- Park, H.Y.; Kim, S.K.; Lim, Y.J.; Kwak, S.H.; Hong, M.J.; Mun, H.M.; Park, S.Y.; Kim, H.J.; Choi, H.R.; Jeong, J.S.; et al. Assessment of the appropriateness of hand surface coverage for health care workers according to World Health Organization hand hygiene guidelines. Am. J. Infect. Control 2014, 42, 559–561. [Google Scholar] [CrossRef]
- Durso, F.T.; Parmar, S.; Heidish, R.S.; Tordoya Henckell, S.; Oncul, O.S.; Jacob, J.T. Improving the communication of hand hygiene procedures: Controlled observation, redesign, and randomized group comparisons. Infect. Control. Hosp. Epidemiol. 2021, 42, 194–202. [Google Scholar] [CrossRef]
- Thivichon-Prince, B.; Barsotti, O.; Girard, R.; Morrier, J.J. Hand hygiene practices in a dental teaching center: Measures and improve. Eur. J. Dent. 2014, 8, 481–486. [Google Scholar] [CrossRef]
- Pires, D.; Bellissimo-Rodrigues, F.; Soule, H.; Gayet-Ageron, A.; Pittet, D. Revisiting the WHO “How to Handrub” Hand Hygiene Technique: Fingertips First? Infect. Control. Hosp. Epidemiol. 2017, 38, 230–233. [Google Scholar] [CrossRef]
- Sunkesula, V.; Kundrapu, S.; Knighton, S.; Cadnum, J.L.; Donskey, C.J. A Randomized Trial to Determine the Impact of an Educational Patient Hand-Hygiene Intervention on Contamination of Hospitalized Patient’s Hands with Healthcare-Associated Pathogens. Infect. Control. Hosp. Epidemiol. 2017, 38, 595–597. [Google Scholar] [CrossRef]
- Laskar, A.M.R.D.; Bhat, P.; Pottakkat, B.; Narayan, S.; Sastry, A.S.; Sneha, R. A multimodal intervention to improve hand hygiene compliance in a tertiary care center. Am. J. Infect. Control 2018, 46, 775–780. [Google Scholar] [CrossRef]
- Johnson, P.D.; Martin, R.; Burrell, L.J.; Grabsch, E.A.; Kirsa, S.W.; O’Keeffe, J.; Mayall, B.C.; Edmonds, D.; Barr, W.; Bolger, C.; et al. Efficacy of an alcohol/chlorhexidine hand hygiene program in a hospital with high rates of nosocomial methicillin-resistant Staphylococcus aureus (MRSA) infection. Med. J. Aust. 2005, 183, 509–514. [Google Scholar] [CrossRef]
- Whitby, M.; McLaws, M.L. Handwashing in healthcare workers: Accessibility of sink location does not improve compliance. J. Hosp. Infect. 2004, 58, 247–253. [Google Scholar] [CrossRef] [PubMed]
- O’Boyle, C.A.; Henly, S.J.; Larson, E. Understanding adherence to hand hygiene recommendations: The theory of planned behavior. Am. J. Infect. Control 2001, 29, 352–360. [Google Scholar] [CrossRef] [PubMed]
- Dehghan Manshadi, S.A.; Sedaghat, M.; Mohammad Hashem, F.; Salehi, M.; Mohammadnejad, E.; Seifi, A.; Salami Khaneshan, A. Knowledge and perception of hand hygiene: A survey using WHO standardized tools in Tehran, Iran. Casp. J. Intern. Med. 2022, 13, 122–126. [Google Scholar] [CrossRef]
- Schmidtke, K.A.; Aujla, N.; Marshall, T.; Hussain, A.; Hodgkinson, G.P.; Arheart, K.L.; Birnbach, D.J.; Kudrna, L.; Vlaev, I. A Crossover Randomized Controlled Trial of Priming Interventions to Increase Hand Hygiene at Ward Entrances. Front. Public Health 2022, 9, 781359. [Google Scholar] [CrossRef] [PubMed]
- Pittet, D. The Lowbury lecture: Behaviour in infection control. J. Hosp. Infect. 2004, 58, 1–13. [Google Scholar] [CrossRef]
- Larson, E.L.; Quiros, D.; Lin, S.X. Dissemination of the CDC’s Hand Hygiene Guideline and impact on infection rates. Am. J. Infect. Control 2007, 35, 666–675. [Google Scholar] [CrossRef][Green Version]
- Irehovbude, J.; Okoye, C.A. Hand hygiene compliance: Bridging the awareness-practice gap in sub-Saharan Africa. GMS Hyg. Infect. Control 2020, 15, Doc06. [Google Scholar] [CrossRef]
- Nalule, Y.; Buxton, H.; Ir, P.; Leang, S.; Macintyre, A.; Pors, P.; Samol, C.; Dreibelbis, R. Hand hygiene during facility-based childbirth in Cambodia: A theory-driven, mixed-methods observational study. BMC Pregnancy Childbirth 2021, 21, 429. [Google Scholar] [CrossRef]
- Wall, R.T.; Datta, S.; Dexter, F.; Ghyasi, N.; Robinson, A.; Persons, D.; Boling, K.A.; McCloud, C.A.; Krisanda, E.K.; Gordon, B.M.; et al. Effectiveness and feasibility of an evidence-based intraoperative infection control program targeting improved basic measures: A post-implementation prospective case-cohort study. J. Clin. Anesth. 2022, 77, 110632. [Google Scholar] [CrossRef]
- Rezk, F.; Stenmarker, M.; Acosta, S.; Johansson, K.; Bengnér, M.; Åstrand, H.; Andersson, A.C. Healthcare professionals’ experiences of being observed regarding hygiene routines: The Hawthorne effect in vascular surgery. BMC Infect. Dis. 2021, 21, 420. [Google Scholar] [CrossRef]
- Loftus, R.W.; Dexter, F.; Goodheart, M.J.; McDonald, M.; Keech, J.; Noiseux, N.; Pugely, A.; Sharp, W.; Sharafuddin, M.; Lawrence, W.T.; et al. The Effect of Improving Basic Preventive Measures in the Perioperative Arena on Staphylococcus aureus Transmission and Surgical Site Infections: A Randomized Clinical Trial. JAMA Netw. Open 2020, 3, e201934. [Google Scholar] [CrossRef] [PubMed]
- Moralejo, D.; El Dib, R.; Prata, R.A.; Barretti, P.; Corrêa, I. Improving adherence to Standard Precautions for the control of health care-associated infections. Cochrane Database Syst. Rev. 2018, 2, CD010768. [Google Scholar] [CrossRef] [PubMed]
- Matatiele, P.; Southon, B.; Dabula, B.; Marageni, T.; Poongavanum, P.; Kgarebe, B. Assessment of quality of alcohol-based hand sanitizers used in Johannesburg area during the COVID-19 pandemic. Sci. Rep. 2022, 12, 4231. [Google Scholar] [CrossRef] [PubMed]
- Golin, A.P.; Choi, D.; Ghahary, A. Hand sanitizers: A review of ingredients, mechanisms of action, modes of delivery, and efficacy against coronaviruses. Am. J. Infect. Control 2020, 48, 1062–1067. [Google Scholar] [CrossRef] [PubMed]
- Suchomel, M.; Eggers, M.; Maier, S.; Kramer, A.; Dancer, S.J.; Pittet, D. Evaluation of World Health Organization-Recommended Hand Hygiene Formulations. Emerg. Infect. Dis. 2020, 26, 2064–2068. [Google Scholar] [CrossRef]
- Swoboda, S.M.; Earsing, K.; Strauss, K.; Lane, S.; Lipsett, P.A. Electronic monitoring and voice prompts improve hand hygiene and decrease nosocomial infections in an intermediate care unit. Crit. Care Med. 2004, 32, 358–363. [Google Scholar] [CrossRef]
- Kampf, G.; Ostermeyer, C. Influence of applied volume on efficacy of 3-minute surgical reference disinfection method prEN 12791. Appl. Environ. Microbiol. 2004, 70, 7066–7069. [Google Scholar] [CrossRef]
| Sex | |||||
|---|---|---|---|---|---|
| Frequency | Percent | Valid Percent | Cumulative Percent | ||
| Gender | Female | 32 | 45.7 | 45.7 | 45.7 |
| Male | 38 | 54.3 | 54.3 | 100 | |
| Total | 70 | 100 | 100 | ||
| Descriptive Statistics | |||||
|---|---|---|---|---|---|
| n | Minimum | Maximum | Mean | Std. Deviation | |
| I-C-B | 70 | 19 | 85.23 | 52.07 | 17.04 |
| I-NC-B | 70 | 14.77 | 81 | 47.34 | 17.17 |
| F-C-B | 70 | 28.84 | 86.11 | 60.89 | 13.51 |
| F-NC-B | 70 | 13.89 | 71.16 | 39.11 | 13.51 |
| I-C-P | 70 | 26.13 | 92.72 | 59.74 | 16.64 |
| I-NC-P | 70 | 7.28 | 73.87 | 40.26 | 16.64 |
| F-C-P | 70 | 31.61 | 93.41 | 69.91 | 13.50 |
| F-NC-P | 70 | 6.59 | 68.39 | 30.09 | 13.50 |
| Valid N (listwise) | 70 | ||||
| Pair | Mean | N | Std. Deviation | Std. Error Mean | Correlation | Sig. | |
|---|---|---|---|---|---|---|---|
| 1 | I-C-B | 52.0693 | 70 | 17.04245 | 2.03696 | 0.509 | 0.000 * |
| F-C-B | 60.8925 | 70 | 13.51530 | 1.61539 | |||
| 2 | I-NC-B | 47.3386 | 70 | 17.17381 | 2.05266 | 0.492 | 0.000 * |
| F-NC-B | 39.1075 | 70 | 13.51530 | 1.61539 | |||
| 3 | I-C-P | 59.7417 | 70 | 16.64494 | 1.98945 | 0.336 | 0.005 * |
| F-C-P | 69.9089 | 70 | 13.50459 | 1.61411 | |||
| 4 | I-NC-P | 40.2583 | 70 | 16.64494 | 1.98945 | 0.336 | 0.005 * |
| F-NC-P | 30.0911 | 70 | 13.50459 | 1.61411 |
| I-C-B | F-C-B | I-NC-B | F-NC-B | I-C-P | F-C-P | I-NC-P | F-NC-P | |
|---|---|---|---|---|---|---|---|---|
| Total N | 70 | 70 | 70 | 70 | 70 | 70 | 70 | 70 |
| Mann-Whitney U | 687.00 | 653.00 | 556.00 | 563.00 | 604.00 | 568.00 | 612.00 | 648.00 |
| Wilcoxon W | 1428.00 | 1394.00 | 1297.00 | 1304.00 | 1345.00 | 1309.00 | 1353.00 | 1389.00 |
| Test Statistic | 687.00 | 653.00 | 556.00 | 563.00 | 604.00 | 568.00 | 612.00 | 648.00 |
| Standard Error | 84.82 | 84.82 | 84.82 | 84.82 | 84.82 | 84.82 | 84.82 | 84.82 |
| Standardized Test Statistic | 0.93 | 0.53 | −0.61 | −0.53 | −0.05 | −0.47 | 0.05 | 0.47 |
| Asymptotic Sig. (2-sided test) | 0.35 | 0.60 | 0.54 | 0.60 | 0.96 | 0.64 | 0.96 | 0.64 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Saveanu, C.I.; Anistoroaei, D.; Todireasa, S.; Saveanu, A.E.; Bobu, L.I.; Bamboi, I.; Boronia, O.; Balcos, C. Evaluation of the Efficiency of Hand Hygiene Technique with Hydroalcoholic Solution by Image Color Summarize. Medicina 2022, 58, 1108. https://doi.org/10.3390/medicina58081108
Saveanu CI, Anistoroaei D, Todireasa S, Saveanu AE, Bobu LI, Bamboi I, Boronia O, Balcos C. Evaluation of the Efficiency of Hand Hygiene Technique with Hydroalcoholic Solution by Image Color Summarize. Medicina. 2022; 58(8):1108. https://doi.org/10.3390/medicina58081108
Chicago/Turabian StyleSaveanu, Catalina Iulia, Daniela Anistoroaei, Stefan Todireasa, Alexandra Ecaterina Saveanu, Livia Ionela Bobu, Irina Bamboi, Octavian Boronia, and Carina Balcos. 2022. "Evaluation of the Efficiency of Hand Hygiene Technique with Hydroalcoholic Solution by Image Color Summarize" Medicina 58, no. 8: 1108. https://doi.org/10.3390/medicina58081108
APA StyleSaveanu, C. I., Anistoroaei, D., Todireasa, S., Saveanu, A. E., Bobu, L. I., Bamboi, I., Boronia, O., & Balcos, C. (2022). Evaluation of the Efficiency of Hand Hygiene Technique with Hydroalcoholic Solution by Image Color Summarize. Medicina, 58(8), 1108. https://doi.org/10.3390/medicina58081108







