Surgical Reconstruction with Tendon Allografting Following Iatrogenic Rupture of the Plantar Fascia: A Case Report
Abstract
1. Introduction
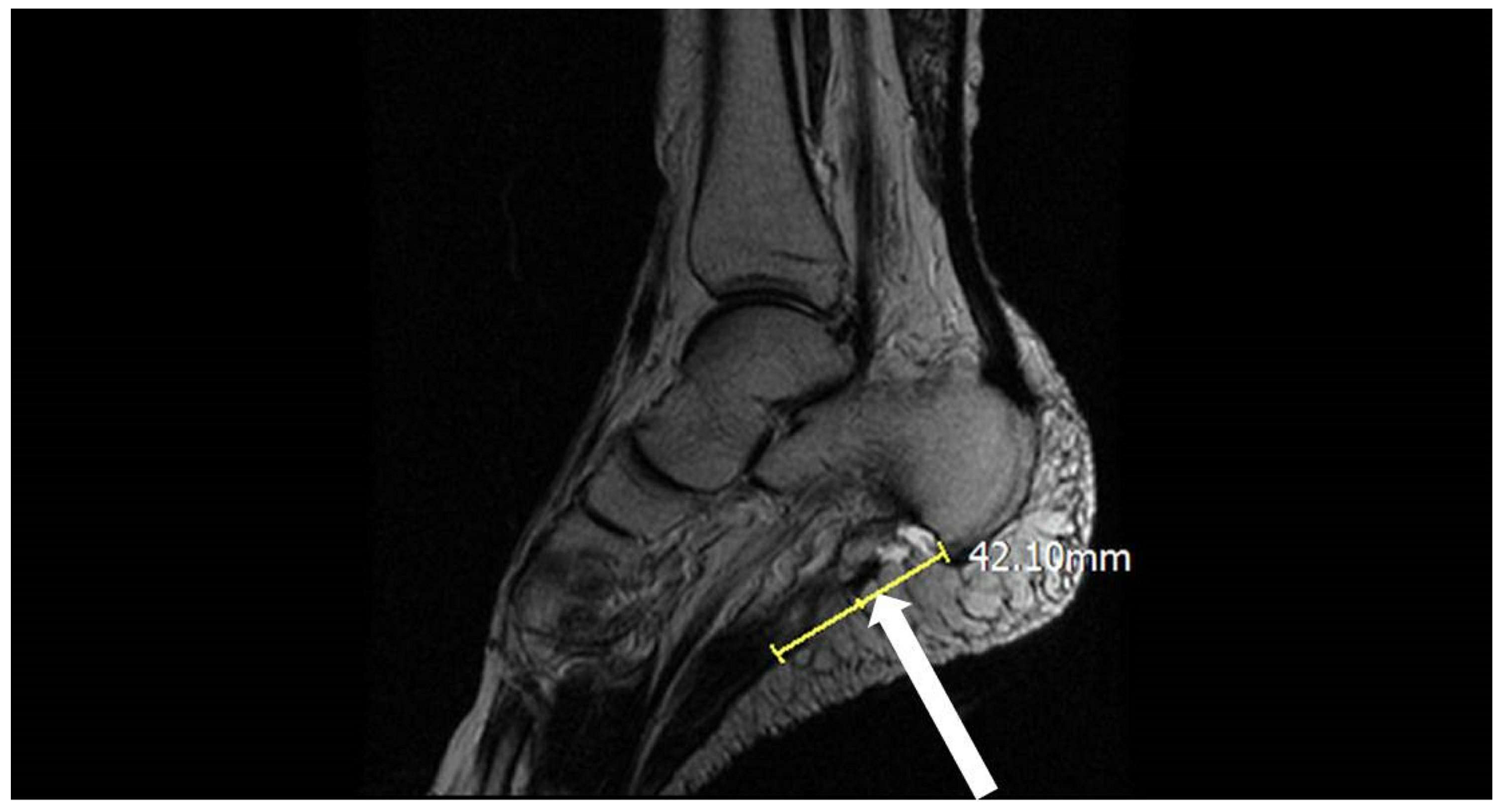
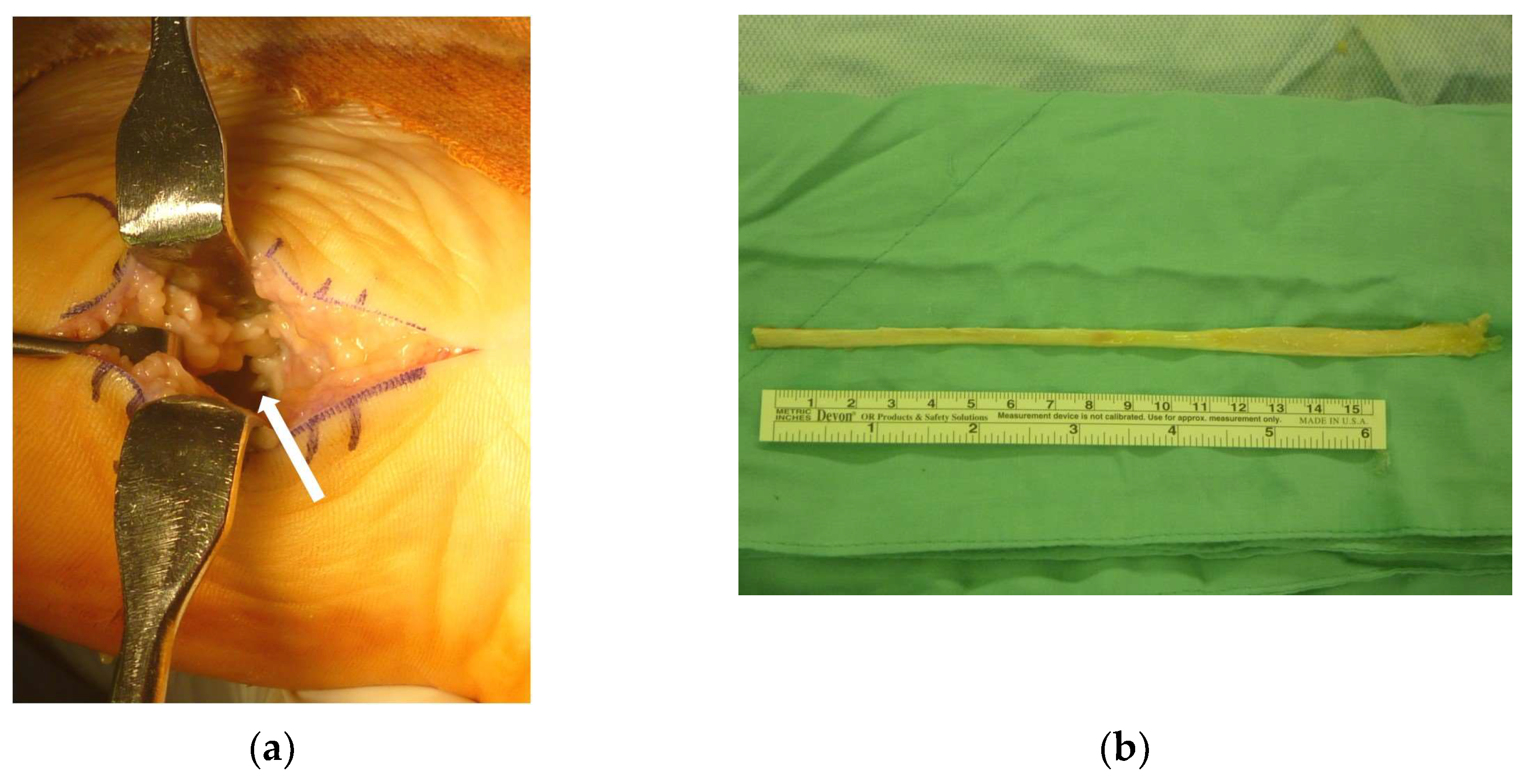
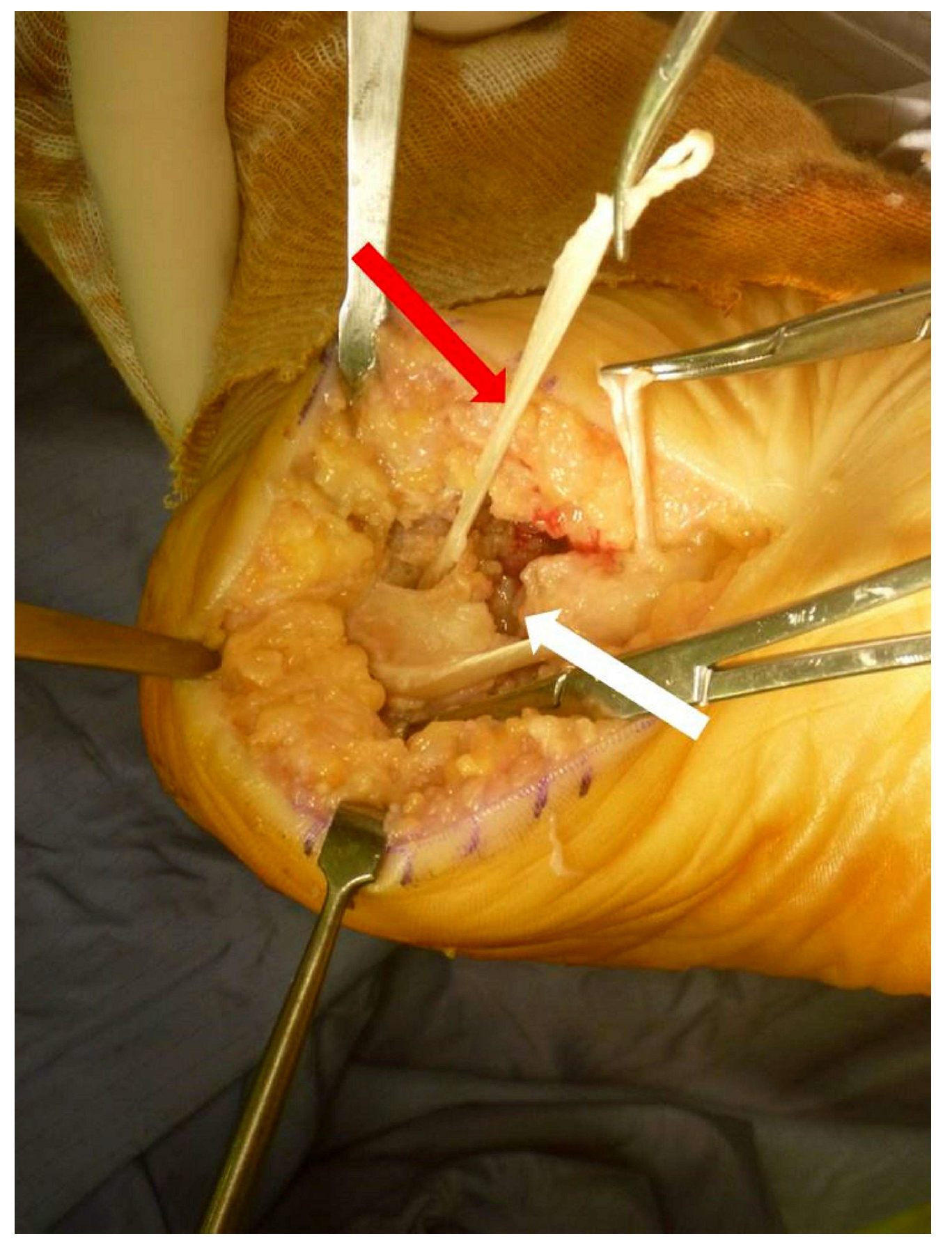
2. Case Presentation
3. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Michetti, M.L.; Jacobs, S.A. Calcaneal heel spurs: Etiology, treatment, and a new surgical approach. J. Foot Surg. 1983, 22, 234–239. [Google Scholar] [PubMed]
- Landorf, K.B.; Menz, H.B. Plantar heel pain and fasciitis. BMJ Clin. Evid. 2008, 2008, 1111. [Google Scholar]
- Monteagudo, M.; Maceira, E.; Garcia-Virto, V.; Canosa, R. Chronic plantar fasciitis: Plantar fasciotomy versus gastrocnemius recession. Int. Orthop. 2013, 37, 1845–1850. [Google Scholar] [CrossRef] [PubMed]
- Gamba, C.; Serrano-Chinchilla, P.; Ares-Vidal, J.; Solano-Lopez, A.; Gonzalez-Lucena, G.; Ginés-Cespedosa, A. Proximal medial gastrocnemius release versus open plantar fasciotomy for the surgical treatment in recalcitrant plantar fasciitis. Foot Ankle Int. 2020, 41, 267–274. [Google Scholar] [CrossRef]
- Debus, F.; Eschbach, D.; Ruchholtz, S.; Peterlein, C.D. Rupture of plantar fascia: Current standard of therapy: A systematic literature review. Foot Ankle Surg. 2020, 26, 358–362. [Google Scholar] [CrossRef] [PubMed]
- Schaarup, S.O.; Burgaard, P.; Johannsen, F.E. Surgical repair of complete plantar fascia ruptures in high-demand power athletes: An alternative treatment option. J. Foot Ankle Surg. 2020, 59, 195–200. [Google Scholar] [CrossRef] [PubMed]
- Bosworth, D.M. Repair of defects in the tendo achillis. J. Bone Jt. Surg. Am. 1956, 3, 111–114. [Google Scholar] [CrossRef]
- Lee, J.; Schuberth, J.M. Surgical Treatment of the Neglected Achilles Tendon Rupture; Achilles Tendon; Andrej, Č., Ed.; IntechOpen: London, UK, 2012; pp. 115–141. [Google Scholar]
- Wapner, K.L.; Pavlock, G.S.; Hecht, P.J.; Naselli, F.; Walther, R. Repair of chronic Achilles tendon rupture with flexor hallucis longus tendon transfer. Foot Ankle Int. 1993, 14, 443–449. [Google Scholar] [CrossRef] [PubMed]
- Kitaoka, H.B.; Alexander, I.J.; Adelaar, R.S.; Nunley, J.A.; Myerson, M.S.; Sanders, M. Clinical rating systems for the ankle-hindfoot, midfoot, hallux, and lesser toes. Foot Ankle Int. 1994, 15, 349–353. [Google Scholar] [CrossRef] [PubMed]
- Pulvertaft, R.G. Tendon grafts for flexor tendon injuries in the fingers and thumb; a study of technique and results. J. Bone Joint Surg. Br. 1956, 38-B, 175–194. [Google Scholar] [CrossRef] [PubMed]
- Fakoya, A.O.J.; Otohinoyi, D.A.; Fakoya, F.A. Correlation of some predisposing intrinsic conditions with the morphological integrity of the Achilles tendon. Ann. Afr. Med. 2018, 17, 58–63. [Google Scholar] [CrossRef] [PubMed]
- Deren, M.E.; Klinge, S.A.; Mukand, N.H.; Mukand, J.A. Tendinopathy and tendon rupture associated with statins. JBJS Rev. 2016, 4, e4. [Google Scholar] [CrossRef] [PubMed]
- Morales, D.R.; Slattery, J.; Pacurariu, A.; Pinheiro, L.; McGettigan, P.; Kurz, X. Relative and absolute risk of tendon rupture with fluoroquinolone and concomitant fluoroquinolone/corticosteroid therapy: Population-based nested case–control study. Clin. Drug Investig. 2019, 39, 205–213. [Google Scholar] [CrossRef] [PubMed]
- Servey, J.T.; Jonas, C. Plantar fascia rupture: Ultrasound to facilitate recognition. J. Am. Board Fam. Med. 2018, 31, 282–285. [Google Scholar] [CrossRef] [PubMed]
- Öztürk, G.T.; Ulaşlı, A.M. Ultrasound-guided platelet-rich plasma injection in a patient with a plantar fascia tear. J. Am. Podiatr. Med. Assoc. 2017, 107, 565–567. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.S.; Choi, Y.R.; Kim, S.W.; Lee, J.Y.; Seo, J.H.; Jeong, J.J. Risk factors affecting chronic rupture of the plantar fascia. Foot Ankle Int. 2014, 35, 258–263. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.H.; Song, E.K.; Seon, J.K.; Woo, S.H. Surgical treatment of neglected traumatic quadriceps tendon rupture with knee ankylosis. Knee Surg. Relat. Res. 2016, 28, 161–164. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Deijkers, R.L.; Bloem, R.M.; Petit, P.L.; Brand, R.; Vehmeyer, S.B.; Veen, M.R. Contamination of bone allografts: Analysis of incidence and predisposing factors. J. Bone Jt. Surg. Br. 1997, 79, 161–166. [Google Scholar] [CrossRef]
- Mroz, T.E.; Joyce, M.J.; Steinmetz, M.P.; Lieberman, I.H.; Wang, J.C. Musculoskeletal allograft risks and recalls in the United States. J. Am. Acad. Orthop. Surg. 2008, 16, 559–565. [Google Scholar] [CrossRef] [PubMed]
- Hinsenkamp, M.; Muylle, L.; Eastlund, T.; Fehily, D.; Noël, L.; Strong, D.M. Adverse reactions and events related to musculoskeletal allografts: Reviewed by the World Health Organisation Project NOTIFY. Int. Orthop. 2012, 36, 633–641. [Google Scholar] [CrossRef] [PubMed]


Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chin, C.-M.; Tang, H.-M.; Yang, K.-C.; Chen, I.-H.; Wang, C.-C. Surgical Reconstruction with Tendon Allografting Following Iatrogenic Rupture of the Plantar Fascia: A Case Report. Medicina 2022, 58, 1075. https://doi.org/10.3390/medicina58081075
Chin C-M, Tang H-M, Yang K-C, Chen I-H, Wang C-C. Surgical Reconstruction with Tendon Allografting Following Iatrogenic Rupture of the Plantar Fascia: A Case Report. Medicina. 2022; 58(8):1075. https://doi.org/10.3390/medicina58081075
Chicago/Turabian StyleChin, Chien-Ming, Huan-Ming Tang, Kai-Chiang Yang, Ing-Ho Chen, and Chen-Chie Wang. 2022. "Surgical Reconstruction with Tendon Allografting Following Iatrogenic Rupture of the Plantar Fascia: A Case Report" Medicina 58, no. 8: 1075. https://doi.org/10.3390/medicina58081075
APA StyleChin, C.-M., Tang, H.-M., Yang, K.-C., Chen, I.-H., & Wang, C.-C. (2022). Surgical Reconstruction with Tendon Allografting Following Iatrogenic Rupture of the Plantar Fascia: A Case Report. Medicina, 58(8), 1075. https://doi.org/10.3390/medicina58081075





