Basic Life Support Knowledge among Junior Medical and Dental Students, Communication Channels, and the COVID-19 Pandemic
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Online Platform
2.3. First Questionnaire
2.4. Second Questionnaire
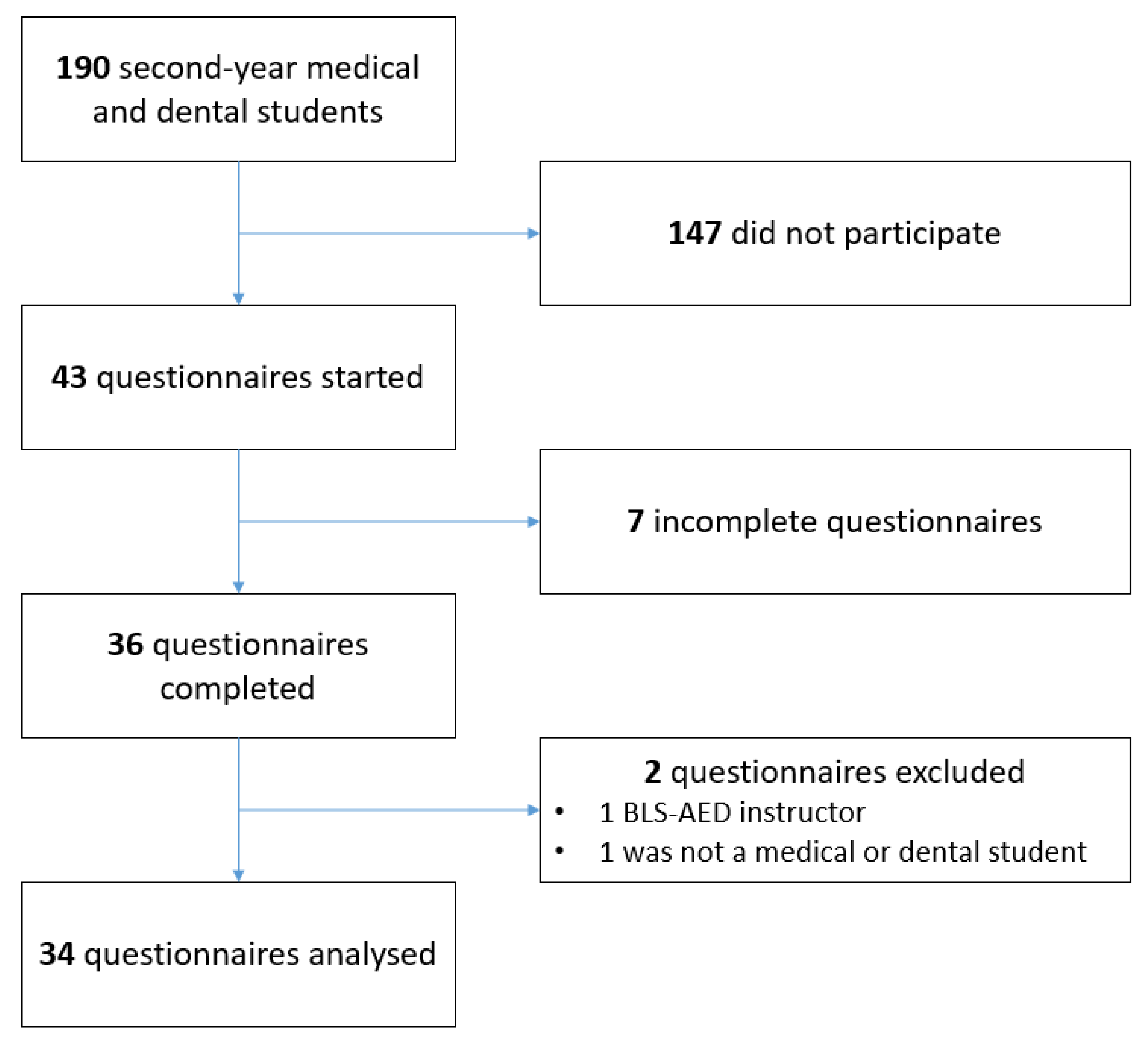
2.5. Exclusion Criteria
2.6. Outcomes
2.7. Data Curation and Statistical Analysis
3. Results
3.1. First Questionnaire
3.2. Second Questionnaire
4. Discussion
4.1. Main Considerations
4.2. Limitations
4.3. Perspectives
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Yasunaga, H.; Horiguchi, H.; Tanabe, S.; Akahane, M.; Ogawa, T.; Koike, S.; Imamura, T. Collaborative effects of bystander-initiated cardiopulmonary resuscitation and prehospital advanced cardiac life support by physicians on survival of out-of-hospital cardiac arrest: A nationwide population-based observational study. Crit. Care 2010, 14, R199. [Google Scholar] [CrossRef] [PubMed]
- Olasveengen, T.M.; Semeraro, F.; Ristagno, G.; Castren, M.; Handley, A.; Kuzovlev, A.; Monsieurs, K.G.; Raffay, V.; Smyth, M.; Soar, J.; et al. European Resuscitation Council Guidelines 2021: Basic Life Support. Resuscitation 2021, 161, 98–114. [Google Scholar] [CrossRef] [PubMed]
- Regard, S.; Rosa, D.; Suppan, M.; Giangaspero, C.; Larribau, R.; Niquille, M.; Sarasin, F.; Suppan, L. Evolution of Bystander Intention to Perform Resuscitation Since Last Training: Web-Based Survey. JMIR Form. Res. 2020, 4, e24798. [Google Scholar] [CrossRef] [PubMed]
- Xie, J.Y.-Y.; Frost, R.; Meakin, R. Not quite a doctor, but should I help? A qualitative exploration of medical students’ attitudes towards responding to medical emergencies that occur in the public domain. BMJ Open 2019, 9, e028035. [Google Scholar] [CrossRef]
- Willmore, R.D.; Veljanoski, D.; Ozdes, F.; Stephens, B.; Mooney, J.; Crumley, S.G.; Doshi, A.; Davies, P.; Badhrinarayanan, S.; Day, E.; et al. Do medical students studying in the United Kingdom have an adequate factual knowledge of basic life support? World J. Emerg. Med. 2019, 10, 75. [Google Scholar] [CrossRef]
- Baldi, E.; Contri, E.; Bailoni, A.; Rendic, K.; Turcan, V.; Donchev, N.; Nadareishvili, I.; Petrica, A.-M.; Yerolemidou, I.; Petrenko, A.; et al. Final-year medical students’ knowledge of cardiac arrest and CPR: We must do more! Int. J. Cardiol. 2019, 296, 76–80. [Google Scholar] [CrossRef]
- Sturny, L.; Regard, S.; Larribau, R.; Niquille, M.; Savoldelli, G.L.; Sarasin, F.; Schiffer, E.; Suppan, L. Differences in basic life support knowledge between junior medical students and lay people: Web-based questionnaire study. J. Med. Internet Res. 2021, 23, e25125. [Google Scholar] [CrossRef]
- Suppan, L.; Herren, T.; Taramarcaz, V.; Regard, S.; Martin-Achard, S.; Zamberg, I.; Larribau, R.; Niquille, M.; Mach, F.; Suppan, M.; et al. A Short Intervention Followed by an Interactive E-Learning Module to Motivate Medical Students to Enlist as First Responders: Protocol for a Prospective Implementation Study. JMIR Res. Protoc. 2020, 9, e24664. [Google Scholar] [CrossRef]
- Semeraro, F.; Greif, R.; Böttiger, B.W.; Burkart, R.; Cimpoesu, D.; Georgiou, M.; Yeung, J.; Lippert, F.S.; Lockey, A.; Olasveengen, T.M.; et al. European Resuscitation Council Guidelines 2021: Systems saving lives. Resuscitation 2021, 161, 80–97. [Google Scholar] [CrossRef]
- Scquizzato, T.; Pallanch, O.; Belletti, A.; Frontera, A.; Cabrini, L.; Zangrillo, A.; Landoni, G. Enhancing citizens response to out-of-hospital cardiac arrest: A systematic review of mobile-phone systems to alert citizens as first responders. Resuscitation 2020, 152, 16. [Google Scholar] [CrossRef]
- Scquizzato, T.; Belloni, O.; Semeraro, F.; Greif, R.; Metelmann, C.; Landoni, G.; Zangrillo, A. Dispatching citizens as first responders to out-of-hospital cardiac arrests. Eur. J. Emerg. Med. 2022, 29, 163–172. [Google Scholar] [CrossRef] [PubMed]
- Taramarcaz, V.; Herren, T.; Golay, E.; Regard, S.; Martin-Achard, S.; Mach, F.; Schnetzler, N.; Ricci, G.; Zamberg, I.; Larribau, R.; et al. A Short Intervention and an Interactive e-Learning Module to Motivate Medical and Dental Students to Enlist as First Responders: Implementation Study. J. Med. Internet Res. 2022, 24, e38508. [Google Scholar] [CrossRef]
- Jensen, J.L.; Kummer, T.A.; Godoy, P.D.d.M. Improvements from a Flipped Classroom May Simply Be the Fruits of Active Learning. CBE Life Sci. Educ. 2015, 14, ar5. [Google Scholar] [CrossRef] [PubMed]
- Hew, K.F.; Lo, C.K. Flipped classroom improves student learning in health professions education: A meta-analysis. BMC Med. Educ. 2018, 18, 38. [Google Scholar] [CrossRef] [PubMed]
- Sturny, L.; Regard, S.; Schiffer, E.; Suppan, L. Basic life support knowledge among junior medical students dataset. Mendeley Data 2020. [Google Scholar] [CrossRef]
- Swiss Confederation CC 810.30 Federal Act of 30 September 2011 on Research Involving Human Beings (Human Research Act, HRA). Available online: https://www.admin.ch/opc/en/classified-compilation/20061313/index.html (accessed on 12 May 2020).
- Eysenbach, G. Improving the quality of Web surveys: The Checklist for Reporting Results of Internet E-Surveys (CHERRIES). J. Med. Internet Res. 2004, 6, e34. [Google Scholar] [CrossRef]
- McCambridge, J.; Kalaitzaki, E.; White, I.R.; Khadjesari, Z.; Murray, E.; Linke, S.; Thompson, S.G.; Godfrey, C.; Wallace, P. Impact of Length or Relevance of Questionnaires on Attrition in Online Trials: Randomized Controlled Trial. J. Med. Internet Res. 2011, 13, e96. [Google Scholar] [CrossRef]
- Eysenbach, G. The Law of Attrition. J. Med. Internet Res. 2005, 7, e11. [Google Scholar] [CrossRef]
- Wurth, S.; Sader, J.; Cerutti, B.; Broers, B.; Bajwa, N.M.; Carballo, S.; Escher, M.; Galetto-Lacour, A.; Grosgurin, O.; Lavallard, V.; et al. Medical students’ perceptions and coping strategies during the first wave of the COVID-19 pandemic: Studies, clinical implication, and professional identity. BMC Med. Educ. 2021, 21, 620. [Google Scholar] [CrossRef]
- Neumann, M.; Fehring, L.; Kinscher, K.; Truebel, H.; Dahlhausen, F.; Ehlers, J.P.; Mondritzki, T.; Boehme, P. Perspective of German medical faculties on digitization in the healthcare sector and its influence on the curriculum. GMS J. Med. Educ. 2021, 38, Doc124. [Google Scholar] [CrossRef]
- Scherl, A.; Dethleffsen, K.; Meyer, M. Interactive knowledge networks for interdisciplinary course navigation within Moodle. Adv. Physiol. Educ. 2012, 36, 284–297. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Minou, I.; Mantas, J. An e-Learning Approach to Hospital Information Systems. Stud. Health Technol. Inform. 2015, 213, 122–125. [Google Scholar] [PubMed]
- Link, T.M.; Marz, R. Computer literacy and attitudes towards e-learning among first year medical students. BMC Med. Educ. 2006, 6, 34. [Google Scholar] [CrossRef]
- Desai, D.; Sen, S.; Desai, S.; Desai, R.; Dash, S. Assessment of online teaching as an adjunct to medical education in the backdrop of COVID-19 lockdown in a developing country—An online survey. Indian J. Ophthalmol. 2020, 68, 2399–2403. [Google Scholar] [CrossRef]
- Armstrong, M.J. Improving email strategies to target stress and productivity in clinical practice. Neurol. Clin. Pract. 2017, 7, 512–517. [Google Scholar] [CrossRef] [PubMed]
- Akbar, F.; Mark, G.; Warton, E.M.; Reed, M.E.; Prausnitz, S.; East, J.A.; Moeller, M.F.; Lieu, T.A. Physicians’ electronic inbox work patterns and factors associated with high inbox work duration. J. Am. Med. Inform. Assoc. 2021, 28, 923–930. [Google Scholar] [CrossRef]
- De Gagne, J.C.; Yang, Y.; Rushton, S.; Koppel, P.D.; Hall, K. Email Use Reconsidered in Health Professions Education: Viewpoint. JMIR Med. Educ. 2020, 6, e19300. [Google Scholar] [CrossRef]
- Papapanou, M.; Routsi, E.; Tsamakis, K.; Fotis, L.; Marinos, G.; Lidoriki, I.; Karamanou, M.; Papaioannou, T.G.; Tsiptsios, D.; Smyrnis, N.; et al. Medical education challenges and innovations during COVID-19 pandemic. Postgrad. Med. J. 2022, 98, 321–327. [Google Scholar] [CrossRef]
| Survey Page, Field, and Question | Type of Question |
|---|---|
| 1—Demographics | |
| How old are you? | RegEx |
| What gender do you identify with? | MCQ |
| 2—Prior training | |
| Have you ever taken a first aid course? | Yes/No |
| What first aid training have you already received? 1 | MAQ 2 |
| For what reason(s) did you not attend a first aid course before? 1 | MAQ 2 |
| Do you or have you engaged in any of these activities? | MAQ |
| Are you a graduate of a health profession? | Yes/No |
| You are (paramedic/nurse/doctor): 1 | MAQ 2 |
| Would you like more first aid training? | MCQ |
| 3—First responders 3 | |
| Did you become a first responder? | Yes/No |
| Are you still active as a first responder? 1 | Yes/No |
| 4—Student in the health sector | |
| Are you a student of a health profession? | Yes/No |
| In which field? 1 | MAQ 2 |
| What field of medicine are you studying? 1 | MAQ 2 |
| Do you plan on specializing in acute medicine (intensive care, anesthesiology, emergency) 1 | MCQ |
| Did you undertake the BLS-AED e-learning course offered to first-year medical students? 1 | MCQ |
| Did you also attend the practice session? 1 | Yes/No |
| 5—BLS knowledge I | |
| Have you ever heard of BLS/ACLS? | Yes/No |
| What does AED stand for? 4,6 | Free text |
| In what year were the first aid guidelines last revised? | RegEx |
| Which number should be called in the event of a medical emergency? 4,5,7 | Free text |
| 6—BLS knowledge II | |
| Which criteria should be met to identify cardiac arrest? 4,5 | MAQ |
| In what order should you proceed to treat a patient in cardiac arrest? 4,5 | Ordering |
| What is the most suitable artery to detect a pulse in an adult patient? 4 | MAQ |
| How deep should chest compressions be performed on an adult? 4,5 | MCQ |
| Which compression to ventilation ratio should be used? 4 | MCQ |
| What is the recommended rate of chest compressions? 4,5 | MCQ |
| Are chest compressions useful if there is no ventilation? 4,5 | MCQ |
| What is the first recommended action for an adult patient who is choking, given that they are unable to speak or cough? 4 | MCQ |
| On a scale of 1 to 10, how comfortable would you say you would be in a resuscitation situation? | 1–10 scale |
| Survey Page, Field, and Question | Type of Question |
|---|---|
| Page 1 | |
| Did you follow the e-learning on the Moodle platform before attending the first resuscitation practice session? | MCQ |
| Why (several answers possible)? 1 | MAQ |
| Did you see a link to e-learning module on Moodle? 1 | Yes/no |
| Did you see an invitation to answer a master thesis questionnaire? 2 | MCQ |
| Why did you only partially follow the e-learning (several answers possible)? 3 | MAQ |
| Page 2 | |
| Did you receive an information e-mail advising you to follow this e-learning course? | MCQ |
| Page 3 | |
| Did you follow the resuscitation course offered in the first year? | MCQ |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ricci, G.; Herren, T.; Taramarcaz, V.; Schnetzler, N.; Dupuis, F.; Schiffer, E.; Suppan, M.; Suppan, L. Basic Life Support Knowledge among Junior Medical and Dental Students, Communication Channels, and the COVID-19 Pandemic. Medicina 2022, 58, 1073. https://doi.org/10.3390/medicina58081073
Ricci G, Herren T, Taramarcaz V, Schnetzler N, Dupuis F, Schiffer E, Suppan M, Suppan L. Basic Life Support Knowledge among Junior Medical and Dental Students, Communication Channels, and the COVID-19 Pandemic. Medicina. 2022; 58(8):1073. https://doi.org/10.3390/medicina58081073
Chicago/Turabian StyleRicci, Gaëtan, Tara Herren, Victor Taramarcaz, Nicolas Schnetzler, François Dupuis, Eduardo Schiffer, Mélanie Suppan, and Laurent Suppan. 2022. "Basic Life Support Knowledge among Junior Medical and Dental Students, Communication Channels, and the COVID-19 Pandemic" Medicina 58, no. 8: 1073. https://doi.org/10.3390/medicina58081073
APA StyleRicci, G., Herren, T., Taramarcaz, V., Schnetzler, N., Dupuis, F., Schiffer, E., Suppan, M., & Suppan, L. (2022). Basic Life Support Knowledge among Junior Medical and Dental Students, Communication Channels, and the COVID-19 Pandemic. Medicina, 58(8), 1073. https://doi.org/10.3390/medicina58081073







