1. Introduction
High tibial osteotomy is a well-established surgical procedure for the management of medial unicompartmental arthritis of the knee joint [
1,
2,
3,
4]. A lateral closed-wedge high tibial osteotomy has potential disadvantages, including difficulty in intraoperatively controlling the amount of correction and concerns of neurologic deficits [
5,
6]. Due to these disadvantages, open-wedge high tibial osteotomy (OWHTO) is becoming popular [
7].
The mechanical stability of the osteotomy site is a major issue following OWHTO. Correction loss and non-union of the osteotomy site have been observed after surgery [
8,
9,
10]. However, with the introduction of the TomoFix plate (Synthes GmbH, Oberdorf, Switzerland), which is characterized by a T-shaped, long, rigid-angle stable implant, the incidence of non-union following OWHTO has declined significantly [
8,
9].
Plate position and proximal screw angles are important for fixation stability in OWHTO [
11]. Posteromedial plating provides better fixation stability than anteromedial plating [
11,
12]. The proximal screw in the direction of the lateral hinge rather than the posterior tibial cortex is associated with increased stability and less neurovascular injury [
12]. Anatomical contouring to the post-correction medial tibial geometry is also important for decreasing the distance between the plate and cortex [
13,
14]. The TomoFix anatomical plate was developed to improve plate position, proximal screw direction, and post-correction tibial contouring (
Figure 1).
Therefore, the purpose of the current study is to compare postoperative configurations between the new modified plate and the conventional plate (the TomoFix Anatomical plate versus the TomoFix conventional plate). It was hypothesized that the new modified plate would provide a better anatomical fitness than the conventional plate.
2. Materials and Methods
This study enrolled patients with primary medial osteoarthritis who underwent primary OWHTO between March 2015 and February 2021. The included subjects were patients aged <65 years who had osteoarthritis with persistent pain despite conservative management for more than three months. Patients were excluded if they had severe osteoarthritis of the patellofemoral joint or lateral compartment, ligament laxity, rheumatoid arthritis, or flexion contracture > 15°, and required an angle of correction > 20°. A total of 116 cases (112 patients) were enrolled in the current study. Among them, 63 patients underwent surgery using the conventional TomoFix plate and 53 using the TomoFix Anatomical plate. For patients who underwent surgery between March 2015 and July 2018, OWHTO was performed using the TomoFix conventional plate, after which surgery was performed using the TomoFix anatomical plate. Both plates were made of titanium. The patient demographics and preoperative data are summarized in
Table 1. This study was approved by the Ethics Committee of our institution (SMC2021-05-051 at 26 May 2021), and written informed consent was obtained from all patients.
2.1. Surgical Technique
All surgeries were performed by the senior author. The correction angle was measured using Miniaci’s method [
15,
16]. The alignment of the lower limb was adjusted by passing the point located at 62.5% of the tibial plateau width when measured from the edge of the proximal tibial medial plateau [
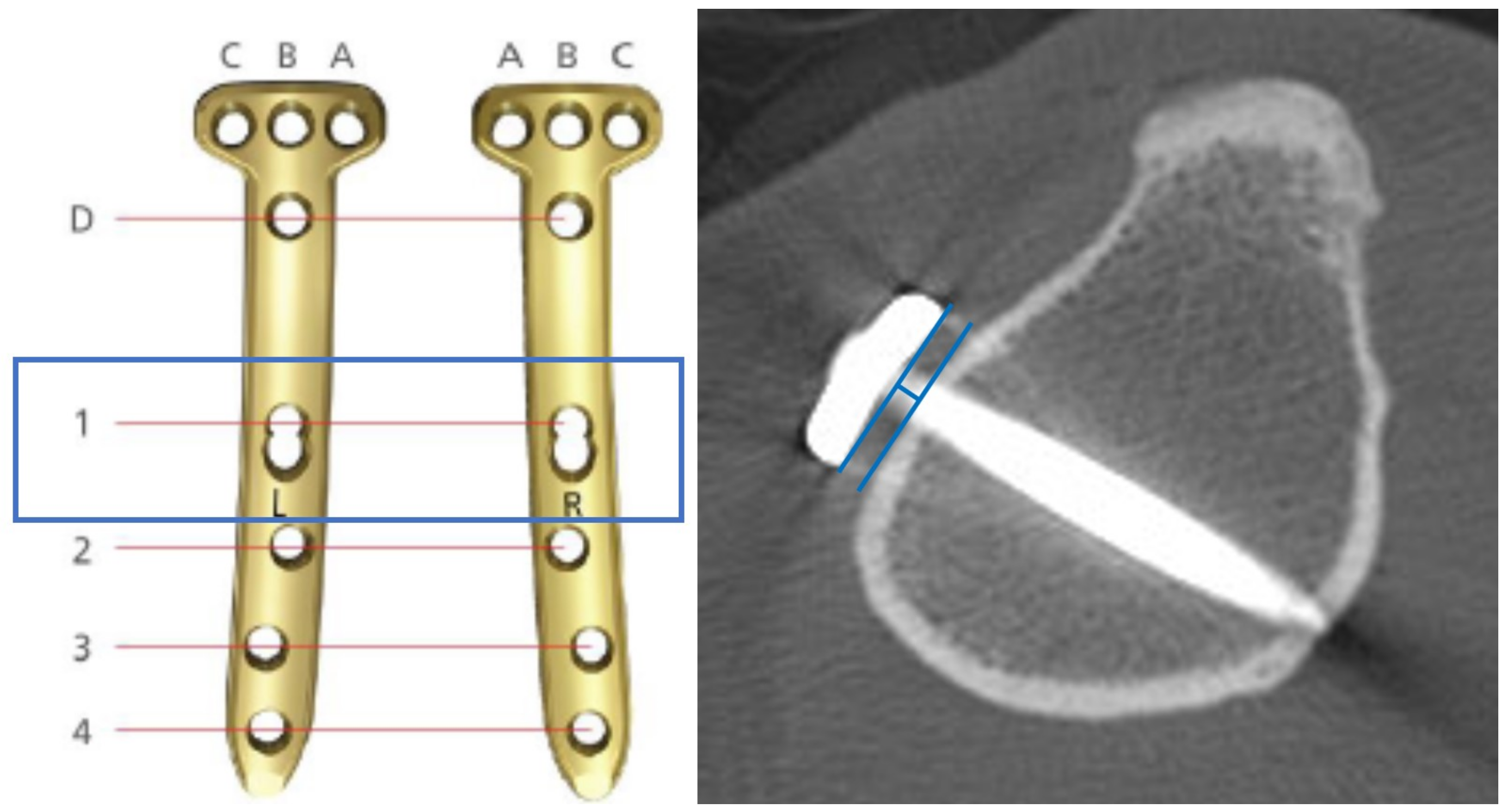
17]. Biplanar osteotomy was performed in all knees. After skin incision, a guide wire was inserted with visual assistance by an image intensifier. The oblique part of the osteotomy was performed with a saw for a distance of up to 1 cm from the lateral cortex. The osteotomy of the vertical part was performed at the posterior aspect of the tibial tubercle, thus not violating the bony portion to which the patellar tendon was attached, leaving most of the tendon attached to the distal tibial fragment. The anterior gap of the osteotomy sited behind the tibial tuberosity was intended to be approximately 1/2 to 2/3 of the posterior opening gap at the posteromedial corner of the proximal tibia to maintain tibial slope. Target alignment was achieved under intraoperative fluoroscopy, and the osteotomy was stabilized using the TomoFix conventional plate or the TomoFix anatomical plate. A cortical screw was used on the most proximal hole of the distal holes (the so-called #1 hole), if the bone-to-plate distance was more than 5 mm, to avoid fixative failure [
18]. An allogenic bone graft (Junyoung Medical, Seoul, South Korea) was inserted into the osteotomy gap to minimize postoperative loss of correction.
The patients were started on isometric quadriceps, active ankle, and straight leg-raising exercises on the day after surgery. Knee motion exercises were initiated on the second postoperative day. Patients were restricted toe toe-touch weight bearing for the first 2 postoperative weeks, followed by partial weight bearing for next 4–6 weeks. Full weight-bearing was permitted by 6–8 weeks.
2.2. Radiographic Evaluation
Plain radiographs were obtained before surgery and three months postoperatively. The radiographs included whole leg standing radiographs (patella facing forward and full knee extension) and lateral views with 30° flexion. The change in limb alignment from before to after surgery was determined by measuring the hip–knee–ankle (HKA) angle on full-length standing radiographs, using a picture archiving and communication system (Centricity; General Electric, Chicago, IL, USA) [
19,
20]. The HKA angle was measured by the angle subtended by a line drawn from the center of the femoral head to the center of the knee and a line drawn from the center of the knee to the center of the talus. The medial proximal tibial angle (MPTA) was measured as the angle between the proximal anatomical axis of the tibia and the tangent along the articular surface of the tibial plateau on full-length standing radiographs [
21]. The angle of the tibial slope was defined using the proximal tibial anatomical axis method [
19]. The MPTA and tibial slope were also compared before and after surgery and between both plate systems.
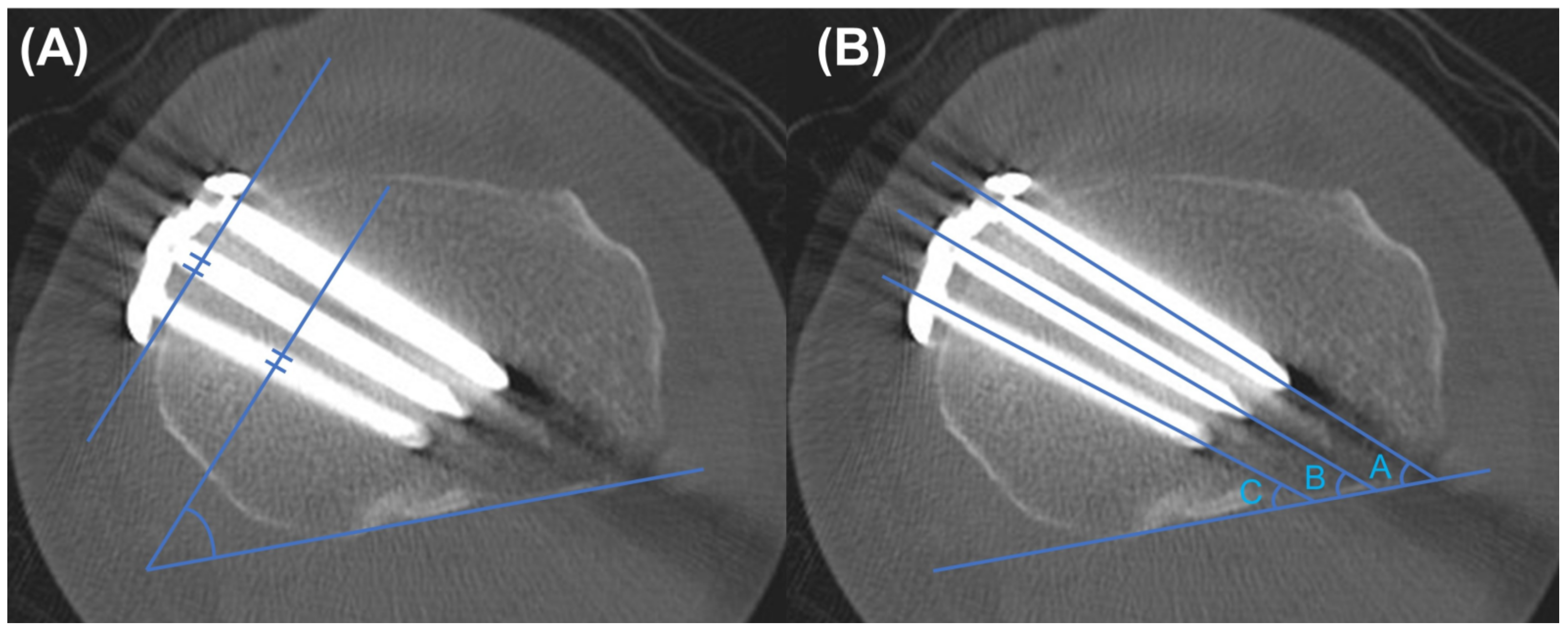
Computed tomography (CT) scans (MDCT; Brilliance 64, Phillips, Cleveland, OH) were performed on the fifth postoperative day. The proximal plate position was evaluated by the proximal plate angle on the axial CT images [
14]. The proximal plate angle was defined as the angle between the posterior cortex line and the line connecting the front and back of the plate proximal area (
Figure 2A). The most proximal screw (A screw, B screw, and C screw, each from front to back, respectively,
Figure 2B) angles were also measured on axial CT images. Each screw angle was defined as the angle between the posterior cortex and the line drawn along the screw. The plate-to-cortex (just below the osteotomy site) distance at #1 hole was measured, and the usage of cortical screw on #1 hole was counted to evaluate the post-correction tibial contouring of the plate (
Figure 3).
All measurements were performed by two orthopedic surgeons with significant experience in OWHTO, but who were not associated with the subject of this study to assess interobserver reliability, and were repeated six weeks later to assess intra-observer reliability.
2.3. Statistical Analysis
The Shapiro–Wilk test was used to investigate the normality of distribution. The Student’s t-test was used for continuous variables, whereas the chi-squared test was used for categorical variables to compare the demographic data and radiographic data. Statistical significance was set at p < 0.05. All data were analyzed using SPSS software (version 22, IBM Corp, Armonk, NY, USA). To have a 90% probability of detecting a 1 mm difference in the plate-to-cortex distance, we needed to enroll 72 patients, assuming an overall standard deviation in 2 mm and a 2-tailed alpha-level of 5%.
3. Results
All inter- and intra-observer intraclass correlation coefficients showed good agreement for all radiographic measurement reliabilities (>0.80).
Compared to the TomoFix conventional group, the TomoFix anatomical group showed similar results in terms of sex distribution, mean age, body mass index, and preoperative and postoperative simple radiographic measurements (
Table 2).
With respect to CT scan measurements, the TomoFix anatomical group showed a greater plate angle than the TomoFix conventional group (39.2° ± 8.1° vs. 31.7° ± 7.0°,
p < 0.001,
Table 3). This result indicates that the TomoFix anatomical plates allowed a more posterior plate position than the conventional plate. Moreover, all screw angles were significantly lower in the TomoFix anatomical group. These results were also caused by positioning the plate more posteriorly than in the TomoFix conventional group.
In the TomoFix conventional group, a cortical screw on #1 hole (the most proximal hole of distal 4 holes) was used in 16 cases (25.4%). However, cortical screws were used in eight cases (15.1%) in the TomoFix anatomical group. The anatomical plate group used fewer cortical screws on #1 hole, but the difference was not statistically significant (p = 0.18). The plate-to-cortex distance was significantly shorter in the TomoFix anatomical group than in the TomoFix conventional group regardless of the use of a cortical screw on the #1 hole. (p < 0.001).
4. Discussion
The principal finding of the current study was that the TomoFix anatomical plate represented a more posteromedial plating position, proximal screw toward the lateral hinge rather than posterior cortex, and improved post-correction tibial contour compared to the TomoFix conventional plate.
Numerous studies have demonstrated that posteromedial plating provides better fixative stability than anteromedial plating in OWHTO [
11,
12,
22]. Takeuchi et al. [
11]. compared the stress on the TomoFix plate between the anteromedial and medial plating positions. They reported that the medial plate position provided significantly less stress on the plate than the anteromedial plate position. Moreover, previous studies reported that the anterior plate position was associated with an increased posterior tibial slope, which might lead to anterior cruciate ligament damage after OWHTO [
23,
24]. The TomoFix conventional plate was a 90° T-shaped plate with no left and right distinction, while the TomoFix anatomical plate had a 5° posterior slope, allowing the plate to be positioned relatively backward. In the current study, the patients using the TomoFix anatomical plate showed a significantly posterior position compared to those using the conventional plate among single-surgeon cases. These results are consistent with the intent of the TomoFix anatomical plate design.
It is well known that an increased plate–bone distance might reduce the fixative stability when using a locking compression plate and screws. Ahmad et al. [
18]. demonstrated that, 5 mm from the bone, the locking plate exhibited increased plastic deformation during cyclical compression and required lower loads to induce mechanical failure when compared to a lesser distance between the bone and plate. Therefore, post-correction anatomical contouring is important for reducing the plate–bone distance in OWHTO. The plate-fitting technique using cortical lag screws was widely performed [
25]. However, it might induce a change in the opening gap or lateral hinge fracture [
26]. In the current study, in the patients with the TomoFix anatomical plate, fewer cortical screws were used on #1 hole (15.1% vs. 25.4%,
p = 0.128). Moreover, the plate-to-cortex distances were significantly shorter in the TomoFix anatomical group regardless of the use of a cortical screw. These results demonstrated that the TomoFix anatomical plate showed better anatomical contouring to the post-correction tibia.
OWHTO is a promising surgery for medial compartmental knee joint osteoarthritis. However, adverse events were reported following OWHTO in 37% to 55% of cases [
25,
27,
28]. Sidhu et al. [
29] demonstrated that a low rate of serious complications (6.5%) requiring unplanned additional surgery was noted after OWHTO using a TomoFix locking plate. However, 52% of the knees required elective hardware removal due to soft tissue irritation. The TomoFix anatomical plate is expected to have a lower hardware removal rate as it has a more posterior position and is more suitable for the post-correction anatomical structure of the tibia.
This study has some limitations. First, although the TomoFix anatomical plate provided a better configuration than the previous version plate system, the superiority of the actual mechanical stability was not proven. An investigation including a mechanical test is needed to identify the association between fixative configuration and mechanical stability in the future. Second, the current study did not include clinical outcomes, including patient-reported outcome measurements, union rate, union period, and correction loss rate. Therefore, this study was not able to identify the effects of plate design changes on clinical outcomes. Third, the two groups had OWHTO performed at different times (TomoFix conventional plate was used between March 2015 and July 2018, TomoFix anatomical plate was used between August 2018 to February 2021), which may have affected the outcome. However, this study was based on data from a single surgeon, which would have had little effect on the results.
5. Conclusions
The TomoFix anatomical plate showed a more posteromedial plating position, proximal screw direction toward the lateral hinge rather than posterior cortex, and improved post-correction tibial contour compared to the TomoFix conventional plate.
Author Contributions
Conceptualization, S.-S.L. and D.-H.L.; methodology, S.-S.L. and D.-H.L.; validation, S.-S.L. and J.P.; formal analysis, S.-S.L. and J.P.; investigation, J.P.; data curation, S.-S.L. and J.P.; writing—original draft preparation, S.-S.L. and D.-H.L.; writing—review and editing, S.-S.L. and D.-H.L.; visualization, S.-S.L. and J.P.; supervision, D.-H.L.; project administration, D.-H.L. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The protocol used to evaluate radiographic findings and intraoperative navigation data was approved by our institution’s investigational review board. (SMC2021-05-051 at May 26 2021).
Informed Consent Statement
Informed consent was obtained from all individual participants included in the study.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare that they have no conflict of interest.
References
- Amendola, A.; Bonasia, D.E. Results of high tibial osteotomy: Review of the literature. Int. Orthop. 2010, 34, 155–160. [Google Scholar] [CrossRef] [Green Version]
- Na, Y.G.; Lee, B.K.; Choi, J.U.; Lee, B.H.; Sim, J.A. Change of joint-line convergence angle should be considered for accurate alignment correction in high tibial osteotomy. Knee Surg. Relat. Res. 2021, 33, 4. [Google Scholar] [CrossRef]
- Lorbergs, A.L.; Birmingham, T.B.; Primeau, C.A.; Atkinson, H.F.; Marriott, K.A.; Giffin, J.R. Improved Methods to Measure Outcomes After High Tibial Osteotomy. Clin. Sports Med. 2019, 38, 317–329. [Google Scholar] [CrossRef] [PubMed]
- Song, I.S.; Kwon, J. Analysis of changes in tibial torsion angle on open-wedge high tibial osteotomy depending on the osteotomy level. Knee Surg. Relat. Res. 2022, 34, 17. [Google Scholar] [CrossRef] [PubMed]
- Coventry, M.B. Upper tibial osteotomy. Clin. Orthop. Relat. Res. 1984, 182, 46–52. [Google Scholar] [CrossRef]
- Staubli, A.E.; De Simoni, C.; Babst, R.; Lobenhoffer, P. TomoFix: A new LCP-concept for open wedge osteotomy of the medial proximal tibia—Early results in 92 cases. Injury 2003, 34 (Suppl. S2), B55–B62. [Google Scholar] [CrossRef]
- Kim, H.J.; Shin, J.Y.; Lee, H.J.; Park, K.H.; Jung, C.H.; Kyung, H.S. Can medial stability be preserved after open wedge high tibial osteotomy? Knee Surg. Relat. Res. 2020, 32, 51. [Google Scholar] [CrossRef]
- Kyung, H.S.; Lee, B.J.; Kim, J.W.; Yoon, S.D. Biplanar Open Wedge High Tibial Osteotomy in the Medial Compartment Osteoarthritis of the Knee Joint: Comparison between the Aescula and TomoFix Plate. Clin. Orthop. Surg. 2015, 7, 185–190. [Google Scholar] [CrossRef]
- Staubli, A.E.; Jacob, H.A. Evolution of open-wedge high-tibial osteotomy: Experience with a special angular stable device for internal fixation without interposition material. Int. Orthop. 2010, 34, 167–172. [Google Scholar] [CrossRef] [Green Version]
- Kang, B.Y.; Lee, D.K.; Kim, H.S.; Wang, J.H. How to achieve an optimal alignment in medial opening wedge high tibial osteotomy? Knee Surg. Relat. Res. 2022, 34, 3. [Google Scholar] [CrossRef]
- Takeuchi, R.; Woon-Hwa, J.; Ishikawa, H.; Yamaguchi, Y.; Osawa, K.; Akamatsu, Y.; Kuroda, K. Primary stability of different plate positions and the role of bone substitute in open wedge high tibial osteotomy. Knee 2017, 24, 1299–1306. [Google Scholar] [CrossRef]
- Wang, J.H.; Bae, J.H.; Lim, H.C.; Shon, W.Y.; Kim, C.W.; Cho, J.W. Medial open wedge high tibial osteotomy: The effect of the cortical hinge on posterior tibial slope. Am. J. Sports Med. 2009, 37, 2411–2418. [Google Scholar] [CrossRef]
- Yoo, O.S.; Lee, Y.S.; Lee, M.C.; Elazab, A.; Choi, D.G.; Jang, Y.W. Evaluation of the screw position and angle using a post-contoured plate in the open wedge high tibial osteotomy according to the correction degree and surgical technique. Clin. Biomech. 2016, 35, 111–115. [Google Scholar] [CrossRef]
- Lee, E.S.; Kim, T.W.; Jo, I.H.; Lee, Y.S. Comparative analysis of fixation configurations and their effect on outcome after medial open-wedge high tibial osteotomy. J. Orthop. Sci. 2020, 25, 627–634. [Google Scholar] [CrossRef] [PubMed]
- Moore, J.; Mychaltchouk, L.; Lavoie, F. Applicability of a modified angular correction measurement method for open-wedge high tibial osteotomy. Knee Surg. Sports Traumatol. Arthrosc. 2017, 25, 846–852. [Google Scholar] [CrossRef]
- Matsushita, T.; Watanabe, S.; Araki, D.; Nagai, K.; Hoshino, Y.; Kanzaki, N.; Matsumoto, T.; Niikura, T.; Kuroda, R. Differences in preoperative planning for high-tibial osteotomy between the standing and supine positions. Knee Surg. Relat. Res. 2021, 33, 8. [Google Scholar] [CrossRef]
- Sabzevari, S.; Ebrahimpour, A.; Roudi, M.K.; Kachooei, A.R. High Tibial Osteotomy: A Systematic Review and Current Concept. Arch. Bone Jt. Surg. 2016, 4, 204–212. [Google Scholar]
- Ahmad, M.; Nanda, R.; Bajwa, A.S.; Candal-Couto, J.; Green, S.; Hui, A.C. Biomechanical testing of the locking compression plate: When does the distance between bone and implant significantly reduce construct stability? Injury 2007, 38, 358–364. [Google Scholar] [CrossRef]
- Lee, S.S.; Nha, K.W.; Lee, D.H. Posterior cortical breakage leads to posterior tibial slope change in lateral hinge fracture following opening wedge high tibial osteotomy. Knee Surg. Sports Traumatol. Arthrosc. 2019, 27, 698–706. [Google Scholar] [CrossRef]
- Batra, S.; Malhotra, R. Medial Ball and Socket Total Knee Arthroplasty in Indian Population: 5-Year Clinical Results. Clin. Orthop. Surg. 2022, 14, 90–95. [Google Scholar] [CrossRef]
- Kubota, M.; Ohno, R.; Sato, T.; Yamaguchi, J.; Kaneko, H.; Kaneko, K.; Ishijima, M. The medial proximal tibial angle accurately corrects the limb alignment in open-wedge high tibial osteotomy. Knee Surg. Sports Traumatol. Arthrosc. 2019, 27, 2410–2416. [Google Scholar] [CrossRef]
- Martinez de Albornoz, P.; Leyes, M.; Forriol, F.; Del Buono, A.; Maffulli, N. Opening wedge high tibial osteotomy: Plate position and biomechanics of the medial tibial plateau. Knee Surg. Sports Traumatol. Arthrosc. 2014, 22, 2641–2647. [Google Scholar] [CrossRef]
- Noyes, F.R.; Mayfield, W.; Barber-Westin, S.D.; Albright, J.C.; Heckmann, T.P. Opening wedge high tibial osteotomy: An operative technique and rehabilitation program to decrease complications and promote early union and function. Am. J. Sports Med. 2006, 34, 1262–1273. [Google Scholar] [CrossRef] [PubMed]
- Black, M.S.; d’Entremont, A.G.; McCormack, R.G.; Hansen, G.; Carr, D.; Wilson, D.R. The effect of wedge and tibial slope angles on knee contact pressure and kinematics following medial opening-wedge high tibial osteotomy. Clin. Biomech. 2018, 51, 17–25. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Valkering, K.P.; van den Bekerom, M.P.; Kappelhoff, F.M.; Albers, G.H. Complications after tomofix medial opening wedge high tibial osteotomy. J. Knee Surg. 2009, 22, 218–225. [Google Scholar] [CrossRef]
- Weng, P.W.; Chen, C.H.; Luo, C.A.; Sun, J.S.; Tsuang, Y.H.; Cheng, C.K.; Lin, S.C. The effects of tibia profile, distraction angle, and knee load on wedge instability and hinge fracture: A finite element study. Med. Eng. Phys. 2017, 42, 48–54. [Google Scholar] [CrossRef]
- Miller, B.S.; Dorsey, W.O.; Bryant, C.R.; Austin, J.C. The effect of lateral cortex disruption and repair on the stability of the medial opening wedge high tibial osteotomy. Am. J. Sports Med. 2005, 33, 1552–1557. [Google Scholar] [CrossRef]
- Nelissen, E.M.; van Langelaan, E.J.; Nelissen, R.G. Stability of medial opening wedge high tibial osteotomy: A failure analysis. Int. Orthop. 2010, 34, 217–223. [Google Scholar] [CrossRef] [Green Version]
- Sidhu, R.; Moatshe, G.; Firth, A.; Litchfield, R.; Getgood, A. Low rates of serious complications but high rates of hardware removal after high tibial osteotomy with Tomofix locking plate. Knee Surg. Sports Traumatol. Arthrosc. 2020, 29, 3361–3367. [Google Scholar] [CrossRef] [PubMed]
| Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).