Abstract
Melasma is a common pigmentary disorder with a complex pathogenesis, of which the treatment is challenging. Conventional treatment often leads to inconsistent results with unexpected pigmentary side effects and high recurrence rates. Recently, the low-fluence Q-switched Nd:YAG laser (LFQSNY) has been widely used for treating melasma, especially in Asia. We reviewed literatures on the LFQSNY treatment of melasma published between 2009 and May 2022 to evaluate the efficacy and adverse events, including its combination therapy. A systematic PubMed search was conducted and a total of 42 articles were included in this study. It was hard to summarize the heterogenous studies, but LFQSNY appeared to be a generally effective and safe treatment for melasma considering the results of previous conventional therapies. However, mottled hypopigmentation has been occasionally reported to develop and persist as an adverse event of LFQSNY, which may be associated with the high accumulated laser energy. When used aggressively, even LFQSNY can induce hyperpigmentation via unwanted inflammation, especially in darker skin. Although few studies have reported considerable recurrence rates three months after treatment, unfortunately, there is a lack of the long-term follow-up results of LFQSNY in melasma. To enhance the effectiveness and reduce the adverse events, LFQSNY has been used in combination with other treatment modalities in melasma, including topical bleaching agents, oral tranexamic acid, chemical peeling, or diverse energy-based devices, which generally reduced side effects with or without significant superior efficacy compared to LFQSNY alone.
1. Introduction
Melasma is a commonly acquired pigmentary skin disease, most observed in adult females and darker skin types of Fitzpatrick phototypes III-V. Clinically, it presents as symmetrical ill-defined hyperpigmented patches on the face, often causing cosmetically serious psychosocial burdens to patients. The pathogenesis of melasma has not been fully understood; however, several factors including chronic ultraviolet exposure, hormonal changes (pregnancy and oral contraceptives) and genetic backgrounds have been proposed to play a role [1]. Treatment of melasma is one of the most challenging fields to dermatologists. The results are inconsistent and unsatisfactory; recurrence and even worsening of the condition during or after treatment is not uncommon. The classic standard treatment is the topical application of modified Kligman’s triple combination (TC), consisting of hydroquinone (HQ) 4%, tretinoin 0.05%, and fluocinolone acetonide 0.01%. Laser treatment has been relatively contraindicated for melasma due to the risk of inducing inflammation and stimulating melanogenesis through unwanted photothermal effects, especially in darker skin [2,3,4]. The reason for such treatment resistance is not yet understood, but the complex pathogenesis of melasma might be involved. The accumulated knowledge to date has suggested melasma as a complex photoaging disorder rather than a simple pigmentary disease. It is histologically characterized by the features of photoaging or dermal inflammation, in addition to active melanocytes, solar elastosis, increased dermal vascularization, increased mast cell count, and altered basement membrane [1,5,6,7]. This implies that the excessive thermal damage of conventional laser irradiation can stimulate inflammatory change by basement membrane disruption and cell apoptosis, resulting in clinical aggravation of melasma.
However, since the 2000s, the low-fluence Q-switched Nd:YAG laser (LFQSNY), commonly referred to as ‘laser toning (LT)’, has been accepted as a new gold standard of melasma treatment in Asia, where there is high demand for treatment. This technique involves multiple sessions (usually around 10 sessions) of weekly or biweekly 1064 nm QSNY treatment with a low fluence (usually 1–3 J/cm2), a collimated beam with a large spot size, and a frequency of 5–10 Hz. The endpoint of the procedure would be faint erythema. LT is known to selectively destroy melanin in melanophores, whereas melanin-containing cells are left undamaged, resulting in safe depigmentation of melasma [8,9]. In addition, one of the key advantages is that there is no downtime affecting patients’ daily lives since the epidermis remains intact. Instead, rather marginal outcomes and questionable long-term results considering many treatment sessions of 1–2 week-intervals are drawbacks of LFQSNY in melasma. To achieve and maintain better clinical results safely, a combination of LFQSNY with various other treatment modalities are commonly used in clinical practice [10,11]. The aim of this review article is to evaluate the overall efficacy, adverse events, and recurrence rates of LFQSNY for melasma. Moreover, we aim to assess the various combination therapy of LFQSNY in melasma.
2. Materials and Methods
A systematic review of literatures was conducted following the Preferred Reporting Items for Systematic Reviews and Meta Analyses (PRISMA) guidelines. We searched English literature on PubMed using the terms, “Q-switched Nd:YAG laser” or “laser toning” and ”melasma” within the period of 2009–2022. The last search was run on 1 May 2022. The inclusion criteria were any original articles with a clinical study evaluating melasma treatment using LFQSNY, not limited to the prospective, randomized, controlled trials (RCTs). Articles regarding combination treatment (LFQSNY with other treatment modalities) or modified solitary LFQSNY were included. Studies with too small of a sample size (n < 10), those materially difficult to reproduce, or inconsistent laser delivery within a non-randomized trial arm were excluded (Figure 1). Two independent investigators performed extraction of articles according to the criteria. We also manually checked the relevant references of the included literatures to prevent any missing data. Discussion was maintained until the two review authors agreed to accept the settlement. Data encompassing study design, patient and treatment characteristics, melasma type, efficacy outcomes, adverse events, and recurrence rates were summarized (Table 1). Since many studies have used heterogenous outcome measures to assess efficacy, we have tried to include numerous scoring systems such as physician-assessed quantitative and qualitative evaluation, and patient-oriented self-evaluation (Table 2). Sunscreen application was not mentioned in the table because all patients used sunscreen as part of their routine melasma management.
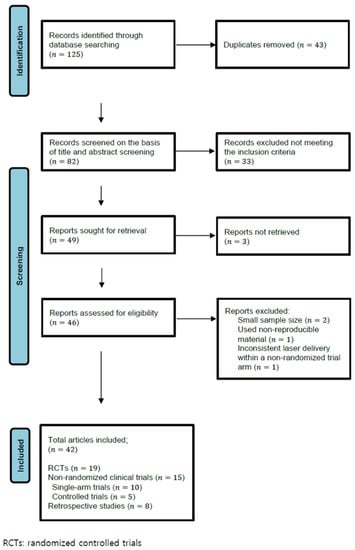
Figure 1.
Literature search and article selection.

Table 1.
Q-switched Nd:YAG laser with or without other treatment modality.

Table 2.
Summaries of the commonly used outcome measures for evaluating melasma.
3. Results
A total of 125 articles were initially identified in the literature search, of which 43 were duplicates and 33 did not meet the inclusion criteria and were thus removed. In the retrieved 46 articles, 4 articles were additionally excluded according to the criteria. A total of 42 articles were finally included: 19 RCTs, 15 non-RCTs (10 single-arm trials, 5 controlled trials), and 8 retrospective studies (Figure 1). A total of 1736 melasma patients were included, whose Fitzpatrick’s skin types consisted of mostly type II-V. Parameters used for LFQSNY varied among studies. The most commonly used spot size was 6–10 mm with a fluence of 0.5–3.8 J/cm2. The number of passes varied from 1 to 10 passes, being most performed in less than 5 passes. Laser treatment sessions were performed usually at intervals of 1–2 weeks with the exception of several studies (especially, studies regarding combination therapy) at intervals of 4 weeks [16,33,37,41]. The time at which efficacy was first evaluated also differed between studies: during the study period, immediately at the end of treatment, 1 to 2 weeks post-treatment, or 1 to 3 months post-treatment. Therefore, direct comparison between heterogeneous studies was difficult, even between those that had the same outcome measures. In addition, validating methods for efficacy differed according to authors. As a subjective outcome measure, the melasma area severity index (MASI) or modified MASI (mMASI) has been frequently adopted. In terms of objective outcome measures, the melanin index (MI) and erythema index (EI) measured from Mexameter® have been frequently used, whereas a few old studies used lightness index (L*I), relative lightness index (RL*I), and color difference (ΔE*ab) using a spectrophotometer. Physician’s Global Assessment (PhGA) and subjective patient satisfaction or patients’ global assessment were also widely adopted indices. The results of the literatures are given in Table 1.
3.1. Low-Fluence Q-Switched Nd:YAG Laser in Melasma
As a monotherapy, LT was performed in 5–15 sessions (usually 9–10) in most studies, showing favorable outcomes not only in subjective measures but also in objective measures [12,21,24,27,28,35,43,44,48,52,53]. Transient erythema and edema were most reported immediately after treatment. Rare, but serious adverse events included pigmentary side effects, such as mottled hypopigmentation (MH) and rebound hyperpigmentation (RH), which were more frequent in darker skin (Fitzpatrick skin type IV, V) [21,44,49,53]. However, some authors have reported aggravation or relapse of melasma three months after cessation of treatment [18,28,33,43,48,49,51,53]. EI scores were higher in refractory melasma [24].
There are few long-term studies of LFQSNY in melasma, whereas in most clinical trials the patients were followed up 1–3 months after completion of treatment. Gokalp et al. in a retrospective trial reported that relapse was observed in 20 out of 34 patients at a 1 year follow-up after a median of 8 sessions of LFQSNY [27]. Three months follow-up results have been considerably reported in literatures showing various recurrence rates. Dev T. et al. and Wattanakrai et al. described that melasma recurred in all their patients who were followed up for 3 months [18,49], whereas Hofbauer et al. and Zhou et al. mentioned 81% and 64% recurrence rates, respectively [28,43]. However, contrarily, many other authors have reported significant improvement at 3 months after treatment [15,17,39,41,44].
In comparison with other treatment for melasma, there was no significant difference in terms of efficacy and adverse events between LFQSNY and low-fluence 755 nm Q-switched alexandrite laser (QSAL). However, QSAL required much fewer passes than QSNY to reach the end point (1–2 vs. up to 8 passes), which is associated with the higher level of melanin absorption of 755 nm wavelength compared to 1064 nm [34]. Compared to LFQSNY, 532 nm QSNY did not significantly reduce MASI score. Moreover, MH and PIH were more frequently observed in the 532 nm QSNY group compared to the LFQSNY group (27.5% vs. 4.8%) [46]. Compared to the glycolic acid (GA) peel, LFQSNY significantly reduced MASI score. Severe adverse events were rarely reported in both treatment groups [46]. In a study comparing LFQSNY and topical silymarin cream, there was no significant difference in the reduction in mMASI score and the incidence of adverse effects in both groups [14]. Dev T. et al. reported that there was no significant difference in the reduction in mMASI, MI score, and subjective evaluation of patients between LFQSNY and TC cream [18]. LFQSNY showed significant reductions in the RL*I and mMASI score and favorable patients’ satisfaction compared to 2% HQ cream [49].
Certain studies tried to find the differences in efficacy and adverse events according to pulse duration or pulse delivery [13,26,33]. Comparing QSNY and picosecond Nd:YAG laser (PSNY) in terms of the efficacy, there was no significant difference between both modalities [13]. Dual-pulsed QSNY, which is also known as PTP (photoacoustic twin pulse) mode, was noninferior to single-pulsed QSNY in terms of efficacy with significantly less pain [26].
3.2. Combination of Low-Fluence Q-Switched Nd:YAG Laser with Other Energy-Based Device
The combination therapy of LFQSNY and other energy-based devices (EBD) showed better or similar efficacy with fewer adverse events compared to monotherapy [15,19,20,22,25,30,38]. Compared to LFQSNY alone, LFQSNY combined with fractional CO2 laser did not show a significant difference in outcome measures such as mMASI score, MI/EI score (p > 0.05). However, the risk of MH was lower in combination therapy compared to monotherapy. [15] The combination therapy of LFQSNY and fractional Er:YAG laser (FEYL) showed significantly higher improvement in Visioface® scores and MI/EI scores than monotherapy. No serious adverse events were reported in both groups. [25] LFQSNY and fractional Er:Glass laser (FEGL) combined therapy tended to show better results in mMASI score and patients’ self-assessment than LFQSNY alone, which was not statistically significant (p > 0.05). [39] Compared to dual-pulsed LFQSNY alone, its combination with fractional microneedling radiofrequency (FMR) showed significantly superior results in efficacy including MI/EI, PSI, and mMASI scores, as well as less adverse events such as MH and RH [19,20].
The combination of LFQSNY and pulsed dye laser (PDL) showed a significantly higher reduction in the MASI score compared to LFQSNY alone in the patients who had visible vasodilation on dermoscopy. However, there was no statistically significant difference between LFQSNY monotherapy and combination therapy in the patients without visible vasodilation on dermoscopy [22]. The combination of QSNY and long-pulsed Nd:YAG laser (LPNY) have treated melasma patients (including refractory melasma) without serious adverse events [31,47], showing a significantly greater reduction in mMASI score compared to LFQSNY monotherapy. MH and RH also occurred less in the combination therapy (1.1% vs. 14.1%) [30]. The combination of LFQSNY and intense pulsed light (IPL) was found to be an effective alternative for melasma treatment, showing a significant decrease in MASI score with few serious adverse events [32]. The regimen of IPL followed by LFQSNY maintenance was also effective for the treatment of melasma [40], showing significant reduction in mMASI and MI scores compared to monotherapy [38].
3.3. Combination of Low-Fluence Q-Switched Nd:YAG Laser with Non-EBD Therapy
The combination therapy of LFQSNY and 30% GA peel lowered the RL*I, mMASI, and MI scores significantly compared to the LFQSNY monotherapy. Although adverse events were rare in both therapies, PIH and MH occurred in patients with Fitzpatrick skin type V (13.3%) [29,45]. Compared with LFQSNY alone, LFQSNY and Jessner’s peel combination therapy tended to be more effective in the reduction in mMASI score or PhGA, which was not statistically significant. There were no serious adverse events reported in both groups [36]. The combination therapy of LFQSNY and modified Jessner’s solution peel did not show a significant difference in efficacy compared to LFQSNY monotherapy. However, the incidence of MH was lower in the combination therapy group compared to the monotherapy group (0% vs. 21.05%) [23]. Microdermabrasion and LFQSNY combination therapy has been proven to be effective in patients with refractory melasma [41].
In a study comparing LFQSNY and topical 3% tranexamic acid (TXA) gel versus microneedling and topical 3% TXA gel, there was no significant difference in reduction in mMASI score and patient satisfaction. However, this study had adopted very low fluence (0.8 J/cm2) with a spot size of 2.5 mm and 4 mm [17]. The combination therapy of LFQSNY and 20% azelaic acid cream showed significant improvement in MASI score compared to LFQSNY alone. However, there was no significant difference in efficacy between LFQSNY and 20% azelaic acid cream. In comparison with LFQSNY, a burning sensation was reported only in the 20% azelaic acid cream group (5%) [42]. In patients with refractory melasma who did not respond to HQ cream and TCC, LFQSNY and 7% alpha arbutin solution combination therapy showed clinical improvement [51].
LFQSNY and oral tranexamic acid combination therapy showed a significant decrease in mMASI score [17], and a significantly greater reduction in mMASI score compared to LFQSNY monotherapy [37].
4. Discussion
The exact action mechanism of LFQSNY in melasma has not yet been elucidated. Despite the number of the clinical study, there are few studies on the histopathologic and molecular study of melasma as there are few volunteers for skin biopsy due to cosmetic issues. However, based on a couple of studies, the selective destruction of the melanosomes with minimal thermal damage of melanocytes is considered to be the key concept of this technique, which is called ‘subcellular selective photothermolysis’ [8,9]. Using the zebrafish model in which the melanophores are externally visible, Kim et al. showed that at a certain low fluence, QSNY selectively photothermolyse melanosomes without killing melanocytes, whereas widespread apoptosis was observed at a higher fluence [9]. In an electron microscope study of human skin, the number of melanocyte dendrites were decreased, and stage IV melanosomes were selectively destroyed whereas early-stage melanosomes were unchanged after LFQSNY in melasma. As mature stage IV melanosomes are accumulated in the dendrites of melanocytes, it is assumed that the QSNY photothermolyse the mature melanosomes, leading to functionally downregulated melanocytes with fewer dendrites [8]. These findings were consistent with the histologic examination, demonstrating a reduced expression of melanogenic proteins (TRP-1, TRP-2, NGF, a-MSH and tyrosinase) as well as melanin (Fontana-Masson staining) in the lesional skin after LFQSNY, whereas the number of melanocytes (Melan-A and SOX-10) was unchanged after treatment, which reassured the concept of the subcellular selective photothermolysis [54].
4.1. Low-Fluence Q-Switched Nd:YAG Laser in Melasma
In our study, it was impossible to sum up the results of 42 heterogeneous studies. Nevertheless, most studies showed favorable results in both objective and subjective assessment as shown in Table 1. Meanwhile, there were a few studies reporting less effectiveness. Park et al. and Fabi et al. reported a 16.7% and 22% reduction in mMASI score, respectively, both after a total of six treatment sessions of weekly QSNY monotherapy, which might be associated with the insufficient total number of treatment sessions [34,45]. Interestingly, in a prospective, split-faced, randomized trial comparing LFQSNY and TC for 12 weeks, there was no significant difference in efficacy between the groups whereas adverse reactions were significantly more common in the TC side (erythema), which may imply overuse of TC. Nevertheless, it reminds us of the effective value of TC, the classic mainstay of melasma treatment.
Although LFQSNY is a relatively safe treatment for melasma by the aforementioned mechanisms, adverse events occasionally occur. Among them, MH or punctate leukoderma is the major concern since it lasts long without treatment. The incidence rate of MH is unknown. Although a larger portion of published studies have reported no or less incidence of MH, there are a couple of literatures reporting approximately a 10% risk of MH from LFQSNY in East Asian patients with melasma [49,55]. A retrospective analysis of a large number of 177 patients of melasma by Choi et al. demonstrated consistent findings that MH occurred in 21 out of 177 patients (11.9%) within 10 sessions of LFQSNY [30]. Although the underlying mechanism is not understood, the histopathologic exam shows a preserved number of melanocytes even in the MH lesion compared to the adjacent normal skin, which signifies that melanocytes still survive, but are functionally downregulated [54,56]. Intervention to stimulate melanogenesis in melanocytes using focused, narrow-band ultraviolet B therapy has been used with some success [57]. Although there are no statistical analyses, some authors have mentioned that hypopigmentation was generally sustained over 2–3 years, and spontaneous resolution was seen in only <10% of the patients after a 2-year follow-up [54]. Another report estimated that MH resolved in half of cases after 2 years and 80% after 3–4 years from their clinical experience [30]. The risk factor of MH is known to be the excessive cumulative energy; the use of relatively high fluence, short treatment intervals, and too many sessions of total treatment [54,58,59,60]. Therefore, caution is needed to avoid aggressive treatment and treatment should be discontinued as soon as possible upon the development of MH.
There were few long-term follow-up studies on LFQSNY for melasma but several studies mentioned conflicting results three months after cessation of treatment. It may be associated with the difference in the individual lifestyle, including sun exposure, as well as the treatment settings and skin phototype.
More recently, a novel PSNY system has been introduced as a new therapeutic option for pigmentation, which has an even shorter pulse duration of the picosecond (10−12) than the nanosecond (10−9) of QSNY. Theoretically, laser toning using PSNY is expected to have advantages over LFQSNY, since a picosecond laser can deliver a higher peak power effectively with much lower energy and less thermal damage to the surrounding tissue. However, in clinical practice, PSNY is not markedly superior to LFQSNY in melasma, yet it is still preferred in tattoo removal and acne scar treatment. Although there are only few reports, a split-face study comparing LFPSNY and LFQSNY for treating melasma demonstrated that neither was superior in pigment lightening [13]. However, the fractionated picosecond laser beam may enhance the efficacy and safety of melasma treatment by rejuvenating the dermal environment. It produces focal vacuoles in the epidermis and dermis by photomechanical effects, termed ‘laser-induced optical breakdown’, leading to dermal remodeling [61,62,63]. Further studies are needed on this novel laser system.
4.2. Combination Therapy of Low-Fluence Q-Switched Nd:YAG Laser in Melasma
The efficacy, tolerability, and adverse events of combination therapy of LFQSNY and other EBD or non-EBD were briefly summarized in the Table 3. Despite the combination of LFQSNY with fractional CO2 laser, FEYL, FMR, PDL (only in patients with visible vasodilatation on dermoscopy), LPNY, IPL, GA peeling, topical azelaic acid, or oral TXA showed significantly superior efficacy to LFQSNY alone, whereas FEGL and modified Jessner’s solution peel did not. However, it is notable that adverse events, such as MH and RH, were generally reduced in combination therapy (FEGL, FMR, LPNY, modified Jessner’s peeling) compared to LFQSNY alone [15,19,20,23,30]. Since melasma has a heterogeneous pathology as mentioned earlier, pigment-nonspecific treatment which targets the dermal pathology of melasma may exert synergistic effects by ameliorating the dermal environment. Moreover, fractional lasers can facilitate the transport and extrusion of epidermal melanin as well as dermal contents through the microscopic treatment zone, which is called the melanin shuttle function [39]. IPL can enhance the improvement of melasma using a distinct mechanism, different from the QSNY accelerating epidermal turnover. The processes, including the collapse of the melanin cap structures and melanosome concentration, are initiated after IPL irradiation forming an intraepidermal microcrust, which desquamates from the skin within 5–7 days. Although initial improvement is relatively dramatic in IPL, RH can also be frequently encountered as melanosomes are quickly replenished with reactivation of melanocytes. Thus, QSNY maintenance therapy may aid in stabilizing the improved state of melasma after IPL irradiation [40]. Although the results of the comparison are conflicting, it is meaningful that the serious pigmentary adverse events tend to be less frequent in combination therapies, which may be attributed to saving QSNY energy and stabilizing melasma lesions.

Table 3.
Summary of highlighted outcomes in this study.
5. Limitations
Our study has several limitations. First, we did not limit our review to RCTs, but we also included retrospective and non-randomized trials; therefore, a potential bias could not be ruled out. Second, studies reviewed in this study had heterogenous designs with various sample sizes and outcome measures, thus it was difficult to compare the results head-to-head. Third, many studies were conducted over a short period of time. Long-term data regarding the recurrence rate and adverse events were limited. Fourth, we did not focus on the type of melasma. In future studies, a head-to-head comparison using a unified outcome measurement and a time point to evaluate the efficacy will be required, considering long-term data such as recurrence rate and type of melasma.
6. Conclusions
LFQSNY has become a preferred treatment of choice in melasma, in which traditional laser treatment is relatively contraindicated due to the high risk of post-treatment hyperpigmentation and high recurrence rate, especially in dark skin. Despite the unusual adverse events, such as MH, it is considered to be generally effective with minimal adverse events for melasma by selectively destroying melanosome while leaving melanin-containing cells intact. Excessive cumulated laser energy is known to be associated with the development of MH. There is a lack of long-term studies that follow patients post-treatment for longer than three months. Although it is conflicting, a few studies showed a high recurrence rate three months after cessation of LFQSNY. However, by using LFQSNY combined with other melasma treatment modalities, recurrence rates as well as adverse events can be reduced, with or without superior efficacy compared to LFQSNY alone. Since there is still no cure and long-term relapse may be inevitable, the importance of patient counselling on the relapsing course of melasma and the importance of photoprotection cannot be overemphasized.
Author Contributions
All authors contributed to the writing of the manuscript. Conceptualization, Y.S.L. and J.E.C.; data curation, Y.S.L., J.E.C., Y.J.L. and J.M.L.; formal analysis, Y.S.L., J.E.C., J.H.L. and T.Y.H.; investigation, Y.J.L. and J.M.L.; methodology, Y.S.L., J.E.C., J.H.L. and T.Y.H.; project administration, J.E.C.; resources, J.E.C., J.H.L. and T.Y.H.; supervision, J.E.C., J.H.L. and T.Y.H.; validation, Y.S.L., J.E.C., J.H.L. and T.Y.H.; visualization, Y.S.L.; writing—original draft, Y.S.L.; writing—review and editing, J.E.C.; software, and funding acquisition, non-applicable. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
All authors declare no conflict of interest for this article.
References
- Kwon, S.H.; Na, J.I.; Choi, J.Y.; Park, K.C. Melasma: Updates and perspectives. Exp. Dermatol. 2019, 28, 704–708. [Google Scholar] [CrossRef] [PubMed]
- Ko, D.; Wang, R.F.; Ozog, D.; Lim, H.W.; Mohammad, T.F. Disorders of Hyperpigmentation. Part II. Review of management and treatment options for hyperpigmentation. J. Am. Acad. Dermatol. 2022; in press. [Google Scholar] [CrossRef]
- Neagu, N.; Conforti, C.; Agozzino, M.; Marangi, G.F.; Morariu, S.H.; Pellacani, G.; Persichetti, P.; Piccolo, D.; Segreto, F.; Zalaudek, I.; et al. Melasma treatment: A systematic review. J. Dermatol. Treat. 2022, 33, 1816–1837. [Google Scholar] [CrossRef] [PubMed]
- Lai, D.; Zhou, S.; Cheng, S.; Liu, H.; Cui, Y. Laser therapy in the treatment of melasma: A systematic review and meta-analysis. Lasers Med. Sci. 2022, 37, 2099–2110. [Google Scholar] [CrossRef] [PubMed]
- Passeron, T.; Picardo, M. Melasma, a photoaging disorder. Pigment Cell Melanoma Res. 2018, 31, 461–465. [Google Scholar] [CrossRef]
- Kwon, S.H.; Hwang, Y.J.; Lee, S.K.; Park, K.C. Heterogeneous Pathology of Melasma and Its Clinical Implications. Int. J. Mol. Sci. 2016, 17, 824. [Google Scholar] [CrossRef] [PubMed]
- Kim, E.H.; Kim, Y.C.; Lee, E.S.; Kang, H.Y. The vascular characteristics of melasma. J. Dermatol. Sci. 2007, 46, 111–116. [Google Scholar] [CrossRef] [PubMed]
- Mun, J.Y.; Jeong, S.Y.; Kim, J.H.; Han, S.S.; Kim, I.H. A low fluence Q-switched Nd:YAG laser modifies the 3D structure of melanocyte and ultrastructure of melanosome by subcellular-selective photothermolysis. J. Electron. Microsc. 2011, 60, 11–18. [Google Scholar] [CrossRef]
- Kim, J.H.; Kim, H.; Park, H.C.; Kim, I.H. Subcellular selective photothermolysis of melanosomes in adult zebrafish skin following 1064-nm Q-switched Nd:YAG laser irradiation. J. Investig. Dermatol. 2010, 130, 2333–2335. [Google Scholar] [CrossRef]
- Mehrabi, J.N.; Bar-Ilan, E.; Wasim, S.; Koren, A.; Zusmanovitch, L.; Salameh, F.; Isman Nelkenbaum, G.; Horovitz, T.; Zur, E.; Song Lim, T.; et al. A review of combined treatments for melasma involving energy-based devices and proposed pathogenesis-oriented combinations. J. Cosmet. Dermatol. 2022, 21, 461–472. [Google Scholar] [CrossRef]
- Iranmanesh, B.; Khalili, M.; Mohammadi, S.; Amiri, R.; Aflatoonian, M. The efficacy of energy-based devices combination therapy for melasma. Dermatol. Ther. 2021, 34, e14927. [Google Scholar] [CrossRef]
- Micek, I.; Pawlaczyk, M.; Kroma, A.; Seraszek-Jaros, A.; Urbańska, M.; Gornowicz-Porowska, J. Treatment of melasma with a low-fluence 1064 nm Q-switched Nd:YAG laser: Laser toning in Caucasian women. Lasers Surg. Med. 2022, 54, 366–373. [Google Scholar] [CrossRef] [PubMed]
- Hong, J.K.; Shin, S.H.; Park, S.J.; Seo, S.J.; Park, K.Y. A prospective, split-face study comparing 1064-nm picosecond Nd:YAG laser toning with 1064-nm Q-switched Nd:YAG laser toning in the treatment of melasma. J. Dermatol. Treat. 2022, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Ibrahim, S.M.A.; Farag, A.S.; Ali, M.S.; El-Gendy, W. Efficacy and Safety of Topical Silymarin Versus Low Fluence 1064-nm Q Switched Nd:YAG Laser in the Treatment of Melasma: A Comparative Randomized Trial. Lasers Surg. Med. 2021, 53, 1341–1347. [Google Scholar] [CrossRef]
- Esmat, S.; Elramly, A.Z.; Shahin, D.; Hilal, R.F. Combining Low Power Fractional CO2 With QS-NdYAG Toning in the Treatment of Melasma Reduces the Incidence of Punctate Leukoderma. Lasers Surg. Med. 2021, 53, 1325–1340. [Google Scholar] [CrossRef] [PubMed]
- Debasmita, B.; Raj, C.; Ishan, A.; Ipsita, D. A prospective randomized controlled trial of Q-switched Nd:YAG laser with topical 3% tranexamic acid (TA) versus microneedling with topical 3% tranexamic acid (TA) in treatment of melasma. J. Cosmet. Dermatol. 2021, 1–7. [Google Scholar] [CrossRef]
- Agamia, N.; Apalla, Z.; Salem, W.; Abdallah, W. A comparative study between oral tranexamic acid versus oral tranexamic acid and Q-switched Nd-YAG laser in melasma treatment: A clinical and dermoscopic evaluation. J. Dermatol. Treat. 2021, 32, 819–826. [Google Scholar] [CrossRef]
- Dev, T.; Sreenivas, V.; Sharma, V.K.; Sahni, K.; Bhari, N.; Sethuraman, G. A split face randomized controlled trial comparing 1064 nm Q-switched Nd-YAG laser and modified Kligman’s formulation in patients with melasma in darker skin. Int. J. Dermatol. 2020, 59, 1525–1530. [Google Scholar] [CrossRef]
- Kwon, H.H.; Choi, S.C.; Jung, J.Y.; Park, G.H. Combined treatment of melasma involving low-fluence Q-switched Nd:YAG laser and fractional microneedling radiofrequency. J. Dermatol. Treat. 2019, 30, 352–356. [Google Scholar] [CrossRef]
- Jung, J.W.; Kim, W.O.; Jung, H.R.; Kim, S.A.; Ryoo, Y.W. A Face-Split Study to Evaluate the Effects of Microneedle Radiofrequency with Q-Switched Nd:YAG Laser for the Treatment of Melasma. Ann. Dermatol. 2019, 31, 133–138. [Google Scholar] [CrossRef]
- Choi, J.E.; Lee, D.W.; Seo, S.H.; Ahn, H.H.; Kye, Y.C. Low-fluence Q-switched Nd:YAG laser for the treatment of melasma in Asian patients. J. Cosmet. Dermatol. 2018, 17, 1053–1058. [Google Scholar] [CrossRef]
- Kong, S.H.; Suh, H.S.; Choi, Y.S. Treatment of Melasma with Pulsed-Dye Laser and 1064-nm Q-Switched Nd:YAG Laser: A Split-Face Study. Ann. Dermatol. 2018, 30, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Saleh, F.; Moftah, N.H.; Abdel-Azim, E.; Gharieb, M.G. Q-switched Nd: YAG laser alone or with modified Jessner chemical peeling for treatment of mixed melasma in dark skin types: A comparative clinical, histopathological, and immunohistochemical study. J. Cosmet. Dermatol. 2018, 17, 319–327. [Google Scholar] [CrossRef] [PubMed]
- Kaminaka, C.; Furukawa, F.; Yamamoto, Y. The Clinical and Histological Effect of a Low-Fluence Q-Switched 1064-nm Neodymium: Yttrium-Aluminum-Garnet Laser for the Treatment of Melasma and Solar Lentigenes in Asians: Prospective, Randomized, and Split-Face Comparative Study. Dermatol. Surg. 2017, 43, 1120–1133. [Google Scholar] [CrossRef] [PubMed]
- Alavi, S.; Abolhasani, E.; Asadi, S.; Nilforoushzadeh, M. Combination of Q-Switched Nd:YAG and Fractional Erbium:YAG Lasers in Treatment of Melasma: A Randomized Controlled Clinical Trial. J. Lasers Med. Sci. 2017, 8, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Jang, H.W.; Chun, S.H.; Park, H.C.; Ryu, H.J.; Kim, I.H. Comparative study of dual-pulsed 1064 nm Q-switched Nd:YAG laser and single-pulsed 1064 nm Q-switched Nd:YAG laser by using zebrafish model and prospective split-face analysis of facial melasma. J. Cosmet. Laser Ther. 2017, 19, 114–123. [Google Scholar] [CrossRef]
- Gokalp, H.; Akkaya, A.D.; Oram, Y. Long-term results in low-fluence 1064-nm Q-Switched Nd:YAG laser for melasma: Is it effective? J. Cosmet. Dermatol. 2016, 15, 420–426. [Google Scholar] [CrossRef]
- Hofbauer Parra, C.A.; Careta, M.F.; Valente, N.Y.; de Sanches Osório, N.E.; Torezan, L.A. Clinical and Histopathologic Assessment of Facial Melasma After Low-Fluence Q-Switched Neodymium-Doped Yttrium Aluminium Garnet Laser. Dermatol. Surg. 2016, 42, 507–512. [Google Scholar] [CrossRef]
- Vachiramon, V.; Sahawatwong, S.; Sirithanabadeekul, P. Treatment of melasma in men with low-fluence Q-switched neodymium-doped yttrium-aluminum-garnet laser versus combined laser and glycolic acid peeling. Dermatol. Surg. 2015, 41, 457–465. [Google Scholar] [CrossRef]
- Choi, C.P.; Yim, S.M.; Seo, S.H.; Ahn, H.H.; Kye, Y.C.; Choi, J.E. Retrospective analysis of melasma treatment using a dual mode of low-fluence Q-switched and long-pulse Nd:YAG laser vs. low-fluence Q-switched Nd:YAG laser monotherapy. J. Cosmet. Laser Ther. 2015, 17, 2–8. [Google Scholar] [CrossRef]
- Choi, C.P.; Yim, S.M.; Seo, S.H.; Ahn, H.H.; Kye, Y.C.; Choi, J.E. Retreatment using a dual mode of low-fluence Q-switched and long-pulse Nd:YAG laser in patients with melasma aggravation after previous therapy. J. Cosmet. Laser Ther. 2015, 17, 129–134. [Google Scholar] [CrossRef]
- Yun, W.J.; Moon, H.R.; Lee, M.W.; Choi, J.H.; Chang, S.E. Combination treatment of low-fluence 1064-nm Q-switched Nd: YAG laser with novel intense pulse light in Korean melasma patients: A prospective, randomized, controlled trial. Dermatol. Surg. 2014, 40, 842–850. [Google Scholar] [CrossRef]
- Alsaad, S.M.; Ross, E.V.; Mishra, V.; Miller, L. A split face study to document the safety and efficacy of clearance of melasma with a 5 ns q switched Nd YAG laser versus a 50 ns q switched Nd YAG laser. Lasers Surg. Med. 2014, 46, 736–740. [Google Scholar] [CrossRef] [PubMed]
- Fabi, S.G.; Friedmann, D.P.; Niwa Massaki, A.B.; Goldman, M.P. A randomized, split-face clinical trial of low-fluence Q-switched neodymium-doped yttrium aluminum garnet (1064 nm) laser versus low-fluence Q-switched alexandrite laser (755 nm) for the treatment of facial melasma. Lasers Surg. Med. 2014, 46, 531–537. [Google Scholar] [CrossRef] [PubMed]
- Sim, J.H.; Park, Y.L.; Lee, J.S.; Lee, S.Y.; Choi, W.B.; Kim, H.J.; Lee, J.H. Treatment of melasma by low-fluence 1064 nm Q-switched Nd:YAG laser. J. Dermatol. Treat. 2014, 25, 212–217. [Google Scholar] [CrossRef] [PubMed]
- Lee, D.B.; Suh, H.S.; Choi, Y.S. A comparative study of low-fluence 1064-nm Q-switched Nd:YAG laser with or without chemical peeling using Jessner’s solution in melasma patients. J. Dermatol. Treat. 2014, 25, 523–528. [Google Scholar] [CrossRef]
- Shin, J.U.; Park, J.; Oh, S.H.; Lee, J.H. Oral Tranexamic Acid Enhances the Efficacy of Low-Fluence 1064-Nm Quality-Switched Neodymium-Doped Yttrium Aluminum Garnet Laser Treatment for Melasma in Koreans: A Randomized, Prospective Trial. Dermatol. Surg. 2013, 39, 435–442. [Google Scholar] [CrossRef]
- Na, S.Y.; Cho, S.; Lee, J.H. Better clinical results with long term benefits in melasma patients. J. Dermatol. Treat. 2013, 24, 112–118. [Google Scholar] [CrossRef]
- Kim, H.S.; Kim, E.K.; Jung, K.E.; Park, Y.M.; Kim, H.O.; Lee, J.Y. A split-face comparison of low-fluence Q-switched Nd: YAG laser plus 1550 nm fractional photothermolysis vs. Q-switched Nd: YAG monotherapy for facial melasma in Asian skin. J. Cosmet. Laser Ther. 2013, 15, 143–149. [Google Scholar] [CrossRef]
- Na, S.Y.; Cho, S.; Lee, J.H. Intense Pulsed Light and Low-Fluence Q-Switched Nd:YAG Laser Treatment in Melasma Patients. Ann. Dermatol. 2012, 24, 267–273. [Google Scholar] [CrossRef]
- Kauvar, A.N. The evolution of melasma therapy: Targeting melanosomes using low-fluence Q-switched neodymium-doped yttrium aluminium garnet lasers. Semin. Cutan. Med. Surg. 2012, 31, 126–132. [Google Scholar] [CrossRef]
- Bansal, C.; Naik, H.; Kar, H.K.; Chauhan, A. A Comparison of Low-Fluence 1064-nm Q-Switched Nd: YAG Laser with Topical 20% Azelaic Acid Cream and their Combination in Melasma in Indian Patients. J. Cutan. Aesthetic Surg. 2012, 5, 266–272. [Google Scholar] [CrossRef] [PubMed]
- Xi, Z.; Gold, M.H.; Zhong, L.U.; Ying, L.I. Efficacy and Safety of Q-Switched 1064-nm Neodymium-Doped Yttrium Aluminum Garnet Laser Treatment of Melasma. Dermatol. Surg. 2011, 37, 962–970. [Google Scholar] [CrossRef] [PubMed]
- Suh, K.S.; Sung, J.Y.; Roh, H.J.; Jeon, Y.S.; Kim, Y.C.; Kim, S.T. Efficacy of the 1064-nm Q-switched Nd:YAG laser in melasma. J. Dermatol. Treat. 2011, 22, 233–238. [Google Scholar] [CrossRef] [PubMed]
- Park, K.Y.; Kim, D.H.; Kim, H.K.; Li, K.; Seo, S.J.; Hong, C.K. A randomized, observer-blinded, comparison of combined 1064-nm Q-switched neodymium-doped yttrium–aluminium–garnet laser plus 30% glycolic acid peel vs. laser monotherapy to treat melasma. Clin. Exp. Dermatol. 2011, 36, 864–870. [Google Scholar] [CrossRef] [PubMed]
- Kar, H.K.; Gupta, L.; Chauhan, A. A comparative study on efficacy of high and low fluence Q-switched Nd:YAG laser and glycolic acid peel in melasma. Indian J. Dermatol. Venereol. Leprol. 2011, 78, 165–171. [Google Scholar] [CrossRef]
- Kang, H.Y.; Kim, K.J.; Goo, B.C. The dual toning technique for melasma treatment with the 1064 Nd:YAG laser: A preliminary study. Laser Ther. 2011, 20, 189–194. [Google Scholar] [CrossRef][Green Version]
- Brown, A.S.; Hussain, M.; Goldberg, D.J. Treatment of melasma with low fluence, large spot size, 1064-nm Q-switched neodymium-doped yttrium aluminum garnet (Nd:YAG) laser for the treatment of melasma in Fitzpatrick skin types II-IV. J. Cosmet. Laser Ther. 2011, 13, 280–282. [Google Scholar] [CrossRef]
- Wattanakrai, P.; Mornchan, R.; Eimpunth, S. Low-fluence Q-switched neodymium-doped yttrium aluminum garnet (1064 nm) laser for the treatment of facial melasma in Asians. Dermatol. Surg. 2010, 36, 76–87. [Google Scholar] [CrossRef]
- Polnikorn, N. Treatment of refractory melasma with the MedLite C6 Q-switched Nd:YAG laser and alpha arbutin: A prospective study. J. Cosmet. Laser Ther. 2010, 12, 126–131. [Google Scholar] [CrossRef]
- Jeong, S.Y.; Shin, J.B.; Yeo, U.C.; Kim, W.S.; Kim, I.H. Low-Fluence Q-Switched Neodymium-Doped Yttrium Aluminum Garnet Laser for Melasma with Pre- or Post-Treatment Triple Combination Cream. Dermatol. Surg. 2010, 36, 909–918. [Google Scholar] [CrossRef]
- Choi, M.; Choi, J.W.; Lee, S.Y.; Choi, S.Y.; Park, H.J.; Park, K.C.; Youn, S.W.; Huh, C.H. Low-dose 1064-nm Q-switched Nd:YAG laser for the treatment of melasma. J. Dermatol. Treat. 2010, 21, 224–228. [Google Scholar] [CrossRef] [PubMed]
- Cho, S.; Kim, J.S.; Kim, M.J. Melasma treatment in Korean women using a 1064-nm Q-switched Nd:YAG laser with low pulse energy. Clin. Exp. Dermatol. 2009, 34, e847–e850. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.E.; Chang, S.E.; Yeo, U.C.; Haw, S.; Kim, I.H. Histopathological study of the treatment of melasma lesions using a low-fluence Q-switched 1064-nm neodymium:yttrium-aluminium-garnet laser. Clin. Exp. Dermatol. 2013, 38, 167–171. [Google Scholar] [CrossRef] [PubMed]
- Chan, N.P.; Ho, S.G.; Shek, S.Y.; Yeung, C.K.; Chan, H.H. A case series of facial depigmentation associated with low fluence Q-switched 1064 nm Nd:YAG laser for skin rejuvenation and melasma. Lasers Surg. Med. 2010, 42, 712–719. [Google Scholar] [CrossRef]
- Jang, Y.H.; Park, J.Y.; Park, Y.J.; Kang, H.Y. Changes in Melanin and Melanocytes in Mottled Hypopigmentation after Low-Fluence 1064-nm Q-Switched Nd:YAG Laser Treatment for Melasma. Ann. Dermatol. 2015, 27, 340–342. [Google Scholar] [CrossRef]
- Kim, H.S.; Jung, H.D.; Kim, H.O.; Lee, J.Y.; Park, Y.M. Punctate leucoderma after low-fluence 1064-nm quality-switched neodymium-doped yttrium aluminum garnet laser therapy successfully managed using a 308-nm excimer laser. Dermatol. Surg. 2012, 38, 821–823. [Google Scholar] [CrossRef]
- Ryu, H.J.; Kim, J. A case of mottled hypopigmentation after low-fluence 1064-nm Q-switched neodymium-doped yttrium aluminum garnet laser therapy. J. Cosmet. Laser Ther. 2013, 15, 290–292. [Google Scholar] [CrossRef]
- Kim, T.; Cho, S.B.; Oh, S.H. Punctate leucoderma after 1064-nm Q-switched neodymium-doped yttrium aluminum garnet laser with low-fluence therapy: Is it melanocytopenic or melanopenic? Dermatol. Surg. 2010, 36, 1790–1791. [Google Scholar] [CrossRef]
- Wong, Y.; Lee, S.S.; Goh, C.L. Hypopigmentation Induced by Frequent Low-Fluence, Large-Spot-Size QS Nd:YAG Laser Treatments. Ann. Dermatol. 2015, 27, 751–755. [Google Scholar] [CrossRef]
- Choi, Y.J.; Nam, J.H.; Kim, J.Y.; Min, J.H.; Park, K.Y.; Ko, E.J.; Kim, B.J.; Kim, W.S. Efficacy and safety of a novel picosecond laser using combination of 1064 and 595 nm on patients with melasma: A prospective, randomized, multicenter, split-face, 2% hydroquinone cream-controlled clinical trial. Lasers Surg. Med. 2017, 49, 899–907. [Google Scholar] [CrossRef]
- Kim, Y.J.; Suh, H.Y.; Choi, M.E.; Jung, C.J.; Chang, S.E. Clinical improvement of photoaging-associated facial hyperpigmentation in Korean skin with a picosecond 1064-nm neodymium-doped yttrium aluminum garnet laser. Lasers Med. Sci. 2020, 35, 1599–1606. [Google Scholar] [CrossRef] [PubMed]
- Wu, D.C.; Goldman, M.P.; Wat, H.; Chan, H.H.L. A Systematic Review of Picosecond Laser in Dermatology: Evidence and Recommendations. Lasers Surg. Med. 2021, 53, 9–49. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).