Regional Variety of Reduction in Retinal Thickness of Diabetic Macular Edema after Anti-VEGF Treatment
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Inclusion and Exclusion Criteria
2.3. Procedures
2.4. Retinal Thickness Measurement Using 3D OCT Mode
2.5. Density of Microaneurysms Measurements by Merged Images
2.6. Statistical Analysis
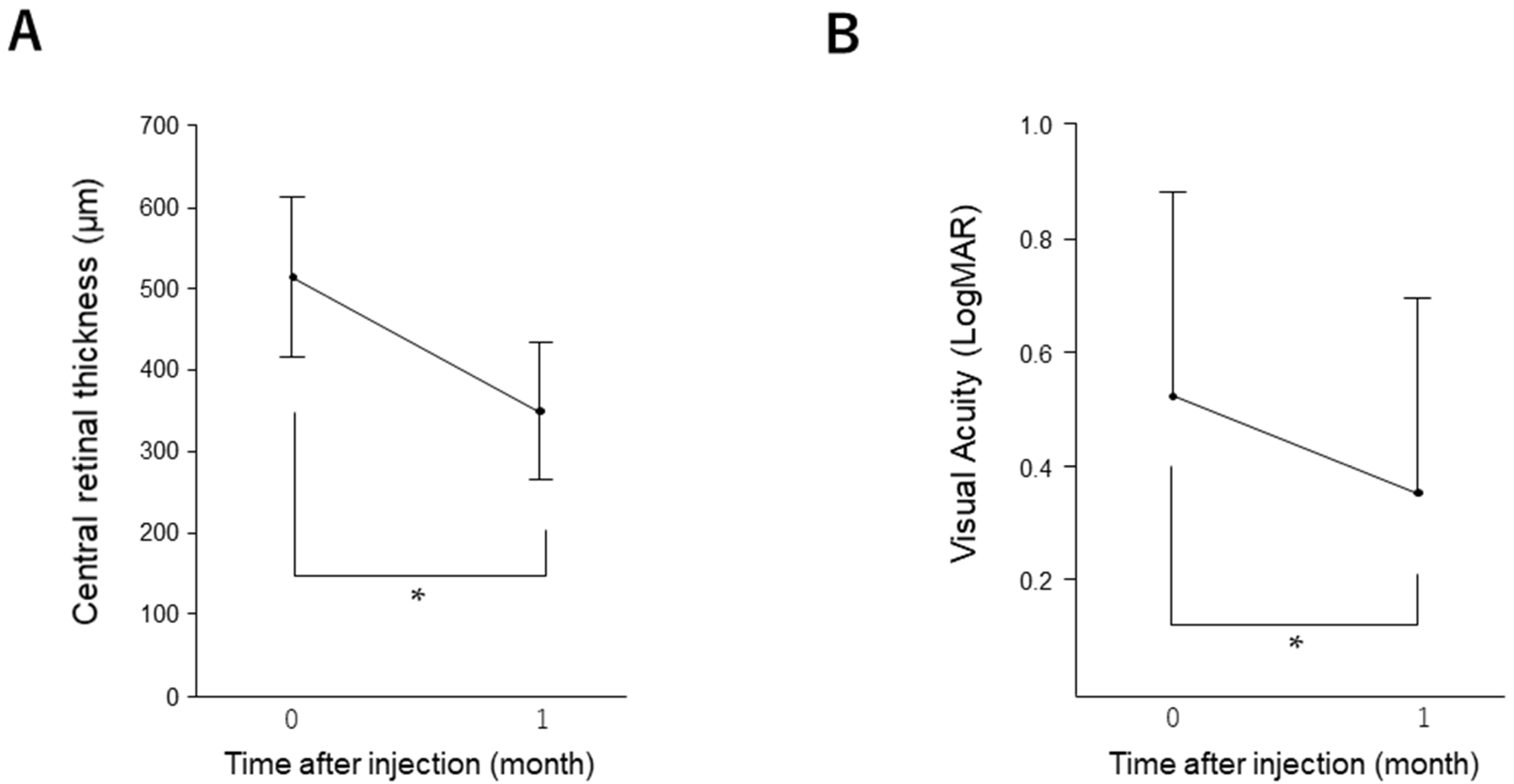
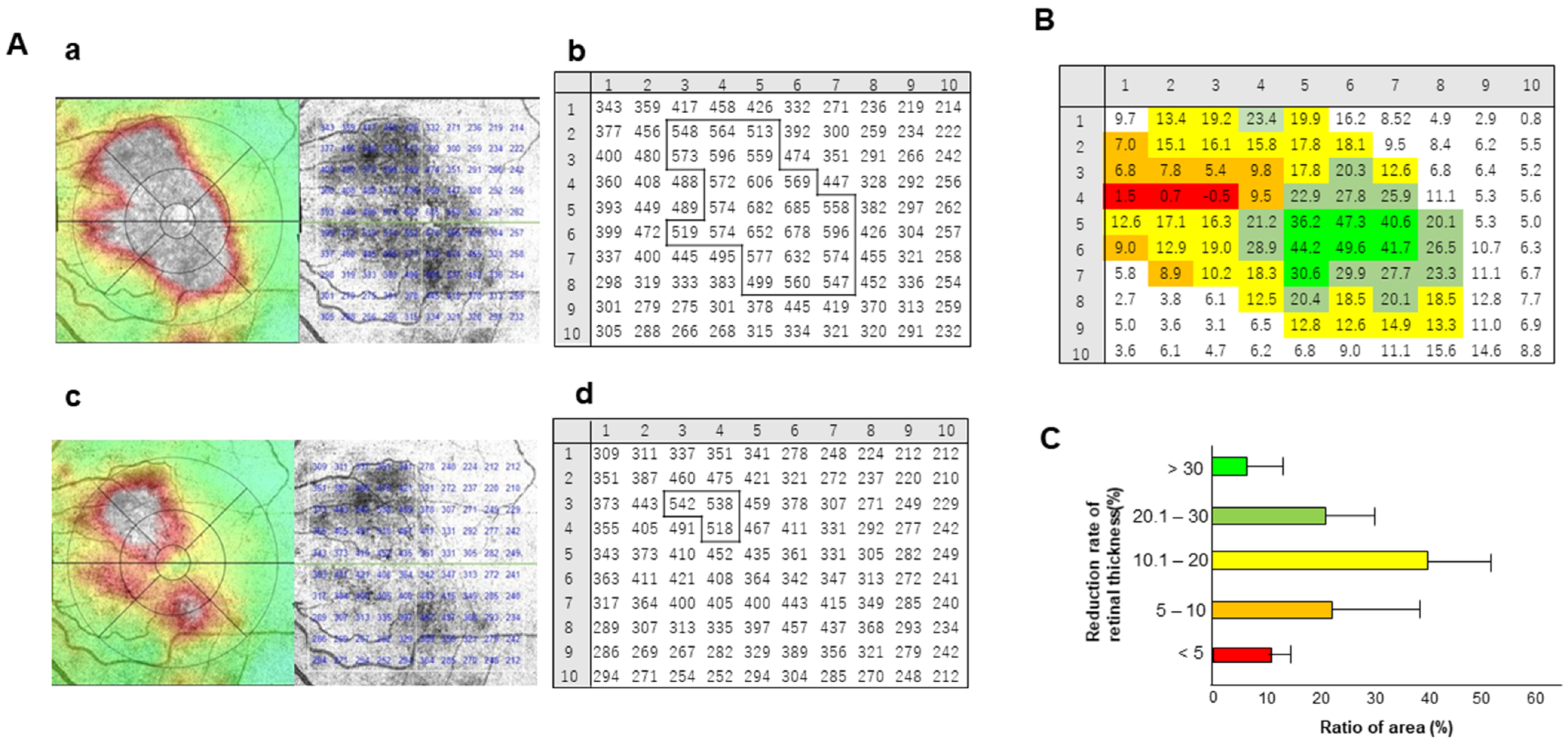
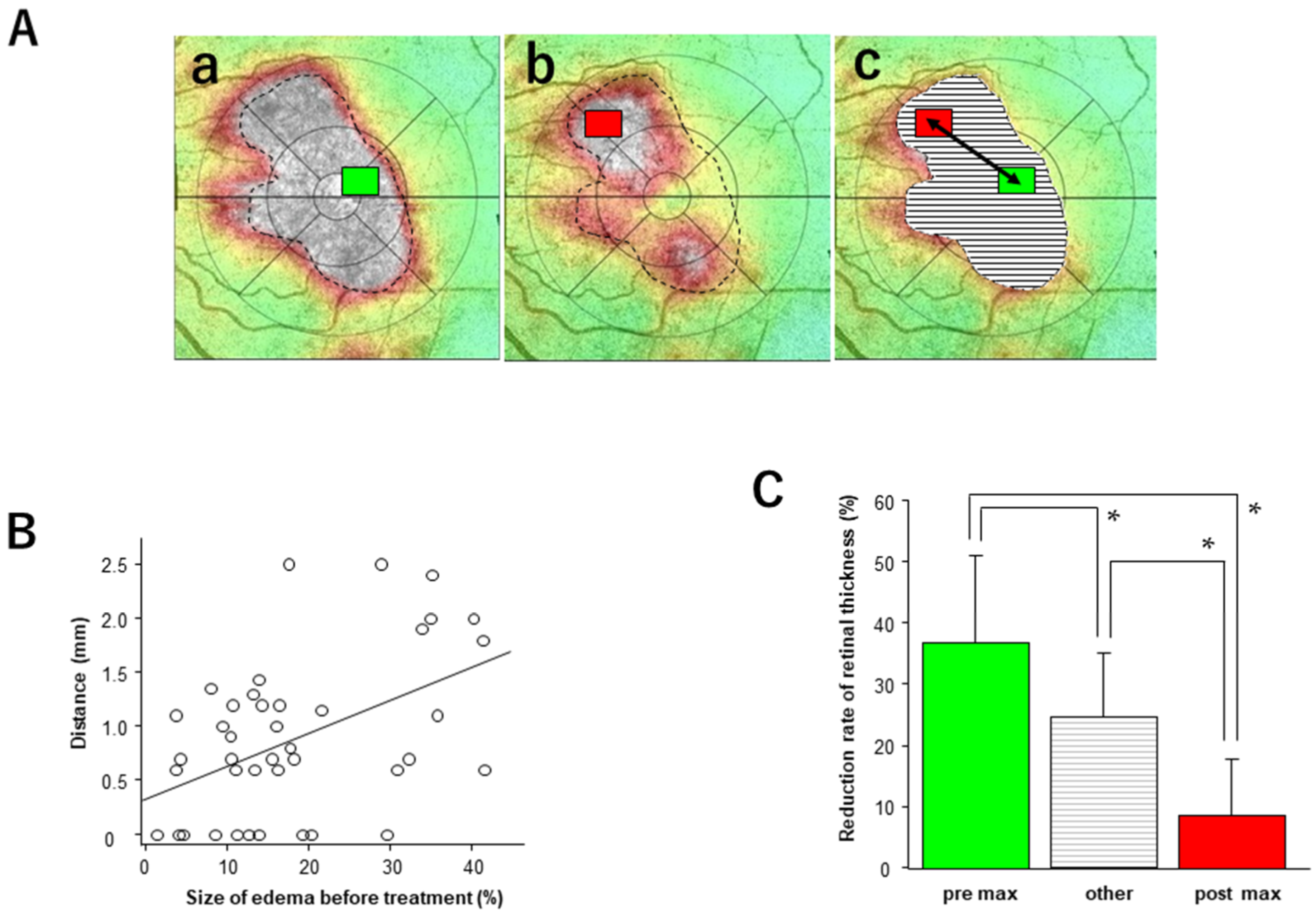
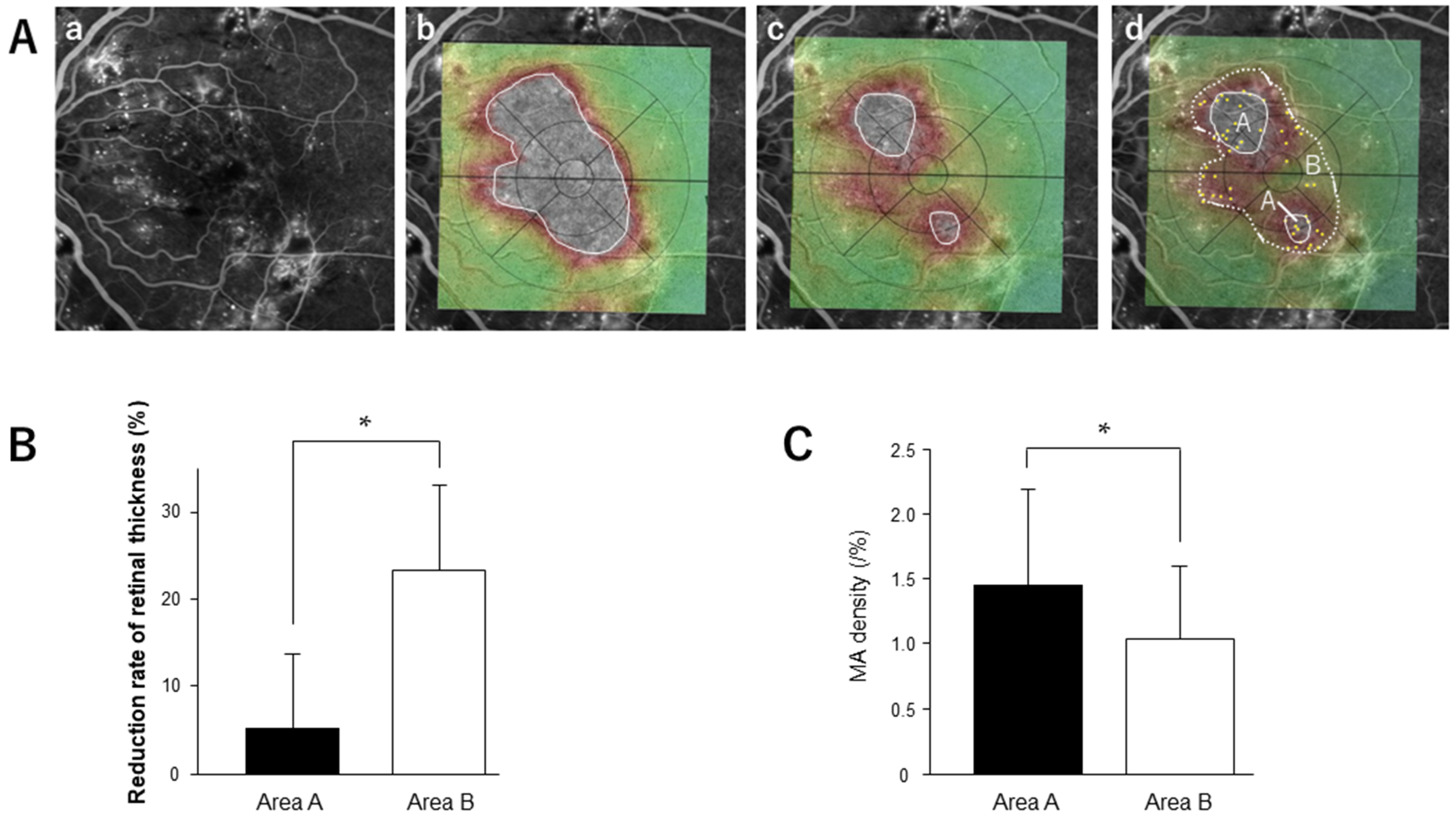
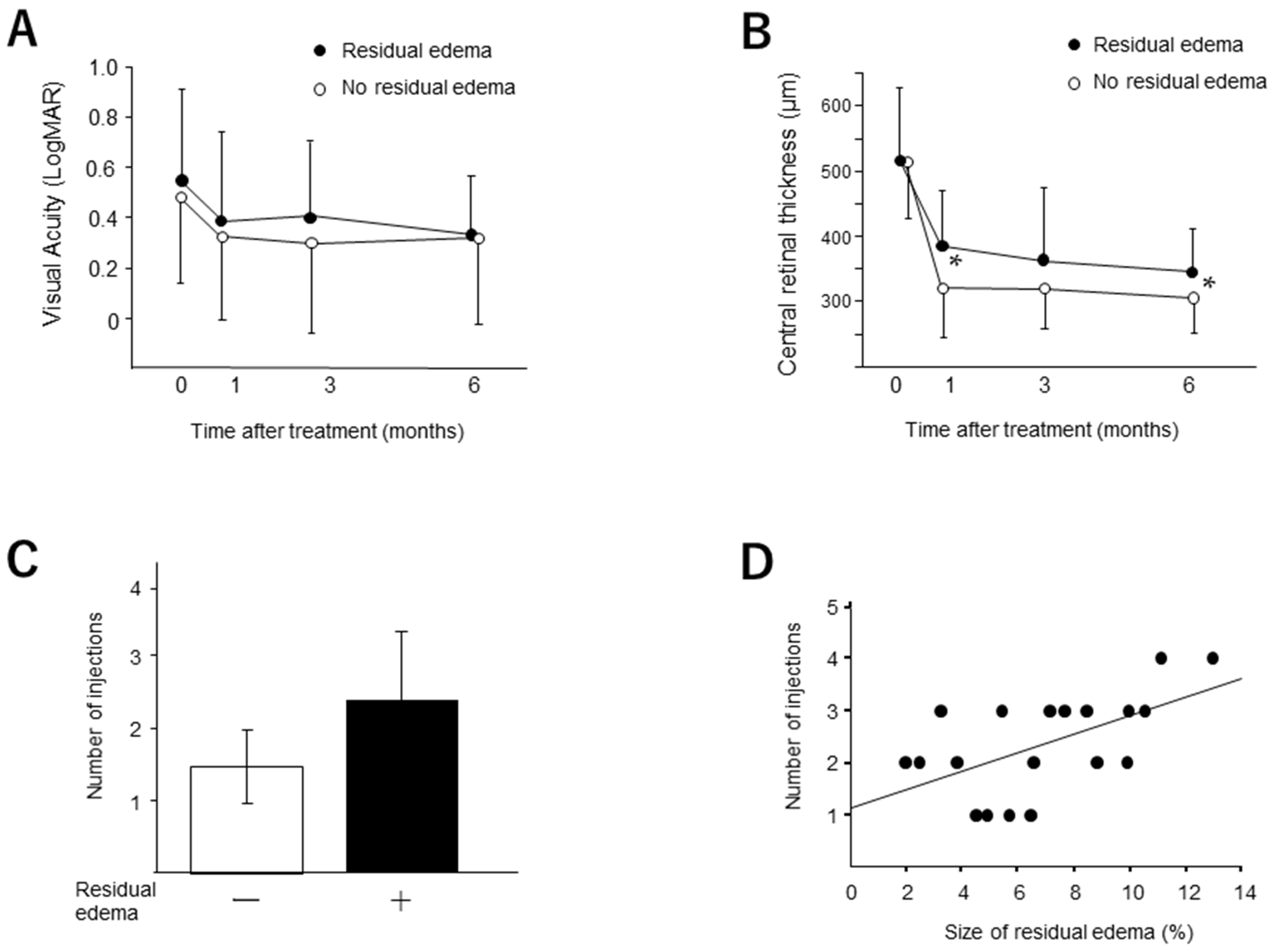
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Terasaki, H.; Ogura, Y.; Kitano, S.; Sakamoto, T.; Murata, T.; Hirakata, A.; Ishibashi, T. Management of diabetic macular edema in Japan: A review and expert opinion. Jpn. J. Ophthalmol. 2018, 62, 1–23. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Saaddine, J.B.; Chou, C.F.; Cotch, M.F.; Cheng, Y.J.; Geiss, L.S.; Gregg, E.W.; Albright, A.L.; Klein, B.E.K.; Klein, R. Prevalence of diabetic retinopathy in the United States, 2005–2008. JAMA 2010, 304, 649–656. [Google Scholar] [CrossRef] [PubMed]
- Das, A.; McGuire, P.G.; Rangasamy, S. Diabetic macular edema: Pathophysiology and novel therapeutic targets. Ophthalmology 2015, 122, 1375–1394. [Google Scholar] [CrossRef] [PubMed]
- Browning, D.J.; Altaweel, M.M.; Bressler, N.M.; Bressler, S.B.; Scott, I.U. Diabetic Retinopathy Clinical Research Network. Diabetic macular edema: What is focal and what is diffuse? Am. J. Ophthalmol. 2008, 146, 649–655.e6. [Google Scholar] [CrossRef] [Green Version]
- Aiello, L.P.; Avery, R.L.; Arrigg, P.G.; Keyt, B.A.; Jampel, H.D.; Shah, S.T.; Pasquale, L.R.; Thieme, H.; Iwamoto, M.A.; Park, J.E.; et al. Vascular endothelial growth factor in ocular fluid of patients with diabetic retinopathy and other retinal disorders. N. Engl. J. Med. 1994, 331, 1480–1487. [Google Scholar] [CrossRef]
- Nguyen, Q.D.; Shah, S.M.; Khwaja, A.A.; Channa, R.; Hatef, E.; Do, D.V.; Boyer, D.; Heier, J.S.; Abraham, P.; Thach, A.B.; et al. Two-year outcomes of the ranibizumab for edema of the mAcula in diabetes (READ-2) study. Ophthalmology 2010, 117, 2146–2151. [Google Scholar] [CrossRef]
- Nguyen, Q.D.; Brown, D.M.; Marcus, D.M.; Boyer, D.S.; Patel, S.; Feiner, L.; Gibson, A.; Sy, J.; Rundle, A.C.; Hopkins, J.J.; et al. Ranibizumab for diabetic macular edema: Results from 2 phase III randomized trials: RISE and RIDE. Ophthalmology 2012, 119, 789–801. [Google Scholar] [CrossRef]
- Ishibashi, T.; Li, X.; Koh, A.; Lai, T.; Lee, F.-L.; Lee, W.-K.; Ma, Z.; Ohji, M.; Tan, N.; Cha, S.B.; et al. The REVEAL study: Ranibizumab Monotherapy or Combined with Laser versus Laser Monotherapy in Asian Patients with Diabetic Macular Edema. Ophthalmology 2015, 122, 1402–1415. [Google Scholar] [CrossRef]
- Mitchell, P.; Bandello, F.; Schmidt-Erfurth, U.; Lang, G.E.; Massin, P.; Schlingemann, R.O.; Sutter, F.; Simader, C.; Burian, G.; Gerstner, O.; et al. The RESTORE study: Ranibizumab monotherapy or combined with laser versus laser monotherapy for diabetic macular edema. Ophthalmology 2011, 118, 615–625. [Google Scholar] [CrossRef] [Green Version]
- Yoshida, S.; Murakami, T.; Nozaki, M.; Suzuma, K.; Baba, T.; Hirano, T.; Sawada, O.; Sugimoto, M.; Takamura, Y.; Tsuiki, E. Review of clinical studies and recommendation for a therapeutic flow chart for diabetic macular edema. Graefe’s Arch. Clin. Exp. Ophthalmol. 2021, 259, 815–836. [Google Scholar] [CrossRef]
- Ogura, Y.; Shiraga, F.; Terasaki, H.; Ohji, M.; Ishida, S.; Sakamoto, T.; Hirakata, A.; Ishibashi, T. Clinical practice pattern in management of diabetic macular edema in Japan: Survey results of Japanese retinal specialists. Jpn. J. Ophthalmol. 2017, 61, 43–50. [Google Scholar] [CrossRef] [PubMed]
- Moisseiev, E.; Abbassi, S.; Thinda, S.; Yoon, J.; Yiu, G.; Morse, L.S. Subthreshold micropulse laser reduces anti-VEGF injection burden in patients with diabetic macular edema. Eur. J. Ophthalmol. 2018, 28, 68–73. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wallick, C.J.; Hansen, R.N.; Campbell, J.; Kiss, S.; Kowalski, J.W.; Sullivan, S.D. Comorbidity and health care resource use among commercially insured non-elderly patients with diabetic macular edema. Ophthalmic Surg. Lasers Imaging Retin. 2015, 46, 744–751. [Google Scholar] [CrossRef] [PubMed]
- Bressler, S.B.; Beaulieu, W.T.; Glassman, A.R.; Gross, J.G.; Melia, M.; Chen, E.; Pavlica, M.R.; Jampol, L.M. Panretinal photocoagulation versus ranibizumab for proliferative diabetic retinopathy: Factors associated with vision and edema outcomes. Ophthalmology 2018, 125, 1776–1783. [Google Scholar] [CrossRef]
- Yoshitake, T.; Murakami, T.; Suzuma, K.; Dodo, Y.; Fujimoto, M.; Tsujikawa, A. Hyperreflective foci in the outer retinal layers as a predictor of the functional efficacy of ranibizumab for diabetic macular edema. Sci. Rep. 2020, 10, 873. [Google Scholar] [CrossRef] [Green Version]
- Yamada, Y.; Takamura, Y.; Morioka, M.; Gozawa, M.; Matsumura, T.; Inatani, M. Microaneurysm density in residual oedema after anti-vascular endothelial growth factor therapy for diabetic macular oedema. Acta Ophthalmol. 2021, 9, e876–e883. [Google Scholar] [CrossRef]
- Hirano, T.; Toriyama, Y.; Iesato, Y.; Imai, A.; Hirabayashi, K.; Nagaoka, T.; Takamura, Y.; Sugimoto, M.; Murata, T. Effect of leaking perifoveal microaneurysms on resolution of diabetic macular edema treated by combination therapy using anti-vascular endothelial growth factor and short pulse focal/grid laser photocoagulation. Jpn. J. Ophthalmol. 2017, 61, 51–60. [Google Scholar] [CrossRef]
- Hirano, T.; Toriyama, Y.; Takamura, Y.; Sugimoto, M.; Nagaoka, T.; Sugiura, Y.; Okamoto, F.; Saito, M.; Noda, K.; Yoshida, S.; et al. Outcomes of a 2-year treat-and-extend regimen with aflibercept for diabetic macular edema. Sci. Rep. 2021, 11, 4488. [Google Scholar] [CrossRef]
- Takamura, Y.; Matsumura, T.; Arimura, S.; Gozawa, M.; Morioka, M.; Inatani, M.; Yamada, Y. Direct photocoagulation guided by merged retinal images for the treatment of focal diabetic macular edema. Int. J. Endo-Crinol. 2018, 2018, 2401094. [Google Scholar] [CrossRef] [Green Version]
- Allingham, M.J.; Mukherjee, D.; Lally, E.B.; Rabbani, H.; Mettu, P.S.; Cousins, S.W.; Farsiu, S. A quantitative approach to predict differential effects of anti-VEGF treatment on diffuse and focal leakage in patients with diabetic macular edema: A pilot study. Transl. Vis. Sci. Technol. 2017, 6, 7. [Google Scholar] [CrossRef] [Green Version]
- Hirano, T.; Toriyama, Y.; Iesato, Y.; Ishibazawa, A.; Sugimoto, M.; Takamura, Y.; Nagaoka, T.; Murata, T. Effect of leaking foveal microaneurysms on the Treatment of center-involving diabetic macular edema: A pilot study. Ophthalmic Res. 2019, 61, 10–18. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.; Moon, B.G.; Cho, A.R.; Yoon, Y.H. Optical coherence tomography angiography of DME and its association with anti-VEGF treatment response. Ophthalmology 2016, 123, 2368–2375. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nozaki, M.; Kato, A.; Yasukawa, T.; Suzuki, K.; Yoshida, M.; Ogura, Y. Indocyanine green angiography-guided focal navigated laser photocoagulation for diabetic macular edema. Jpn. J. Ophthalmol. 2019, 63, 243–254. [Google Scholar] [CrossRef] [PubMed]
- Kato, F.; Nozaki, M.; Kato, A.; Hasegawa, N.; Morita, H.; Yoshida, M.; Ogura, Y. Evaluation of navigated laser photocoagulation (Navilas 577+) for the treatment of refractory diabetic macular edema. J. Ophthalmol. 2018, 2018, 3978514. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yamada, Y.; Takamura, Y.; Matsumura, T.; Gozawa, M.; Morioka, M.; Inatani, M. Regional Variety of Reduction in Retinal Thickness of Diabetic Macular Edema after Anti-VEGF Treatment. Medicina 2022, 58, 933. https://doi.org/10.3390/medicina58070933
Yamada Y, Takamura Y, Matsumura T, Gozawa M, Morioka M, Inatani M. Regional Variety of Reduction in Retinal Thickness of Diabetic Macular Edema after Anti-VEGF Treatment. Medicina. 2022; 58(7):933. https://doi.org/10.3390/medicina58070933
Chicago/Turabian StyleYamada, Yutaka, Yoshihiro Takamura, Takehiro Matsumura, Makoto Gozawa, Masakazu Morioka, and Masaru Inatani. 2022. "Regional Variety of Reduction in Retinal Thickness of Diabetic Macular Edema after Anti-VEGF Treatment" Medicina 58, no. 7: 933. https://doi.org/10.3390/medicina58070933
APA StyleYamada, Y., Takamura, Y., Matsumura, T., Gozawa, M., Morioka, M., & Inatani, M. (2022). Regional Variety of Reduction in Retinal Thickness of Diabetic Macular Edema after Anti-VEGF Treatment. Medicina, 58(7), 933. https://doi.org/10.3390/medicina58070933





