Future Acceptability of Respiratory Virus Infection Control Interventions in General Population to Prevent Respiratory Infections
Abstract
:1. Introduction
2. Materials and Methods
Data Analysis
3. Results
3.1. Beliefs about COVID-19
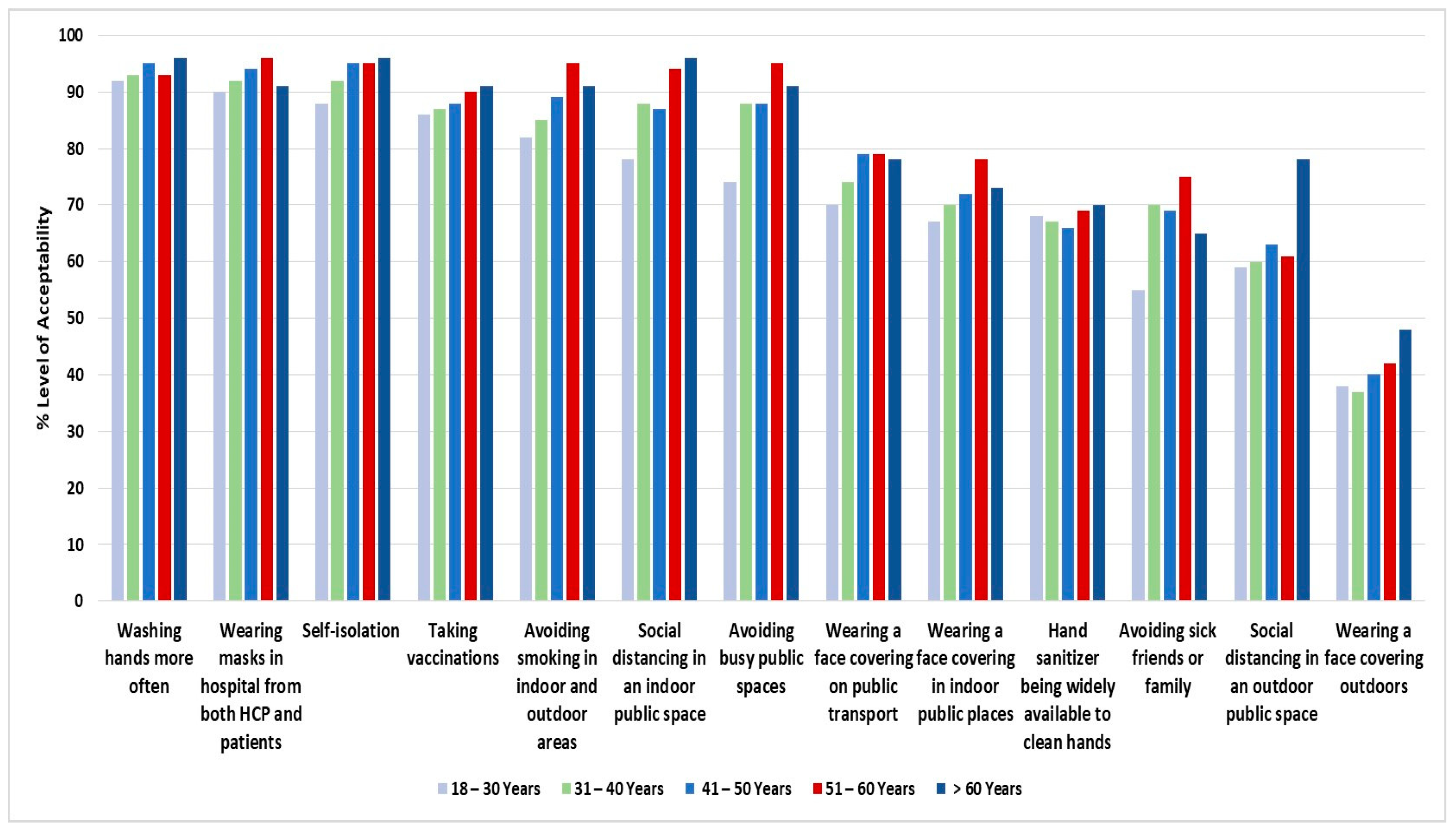
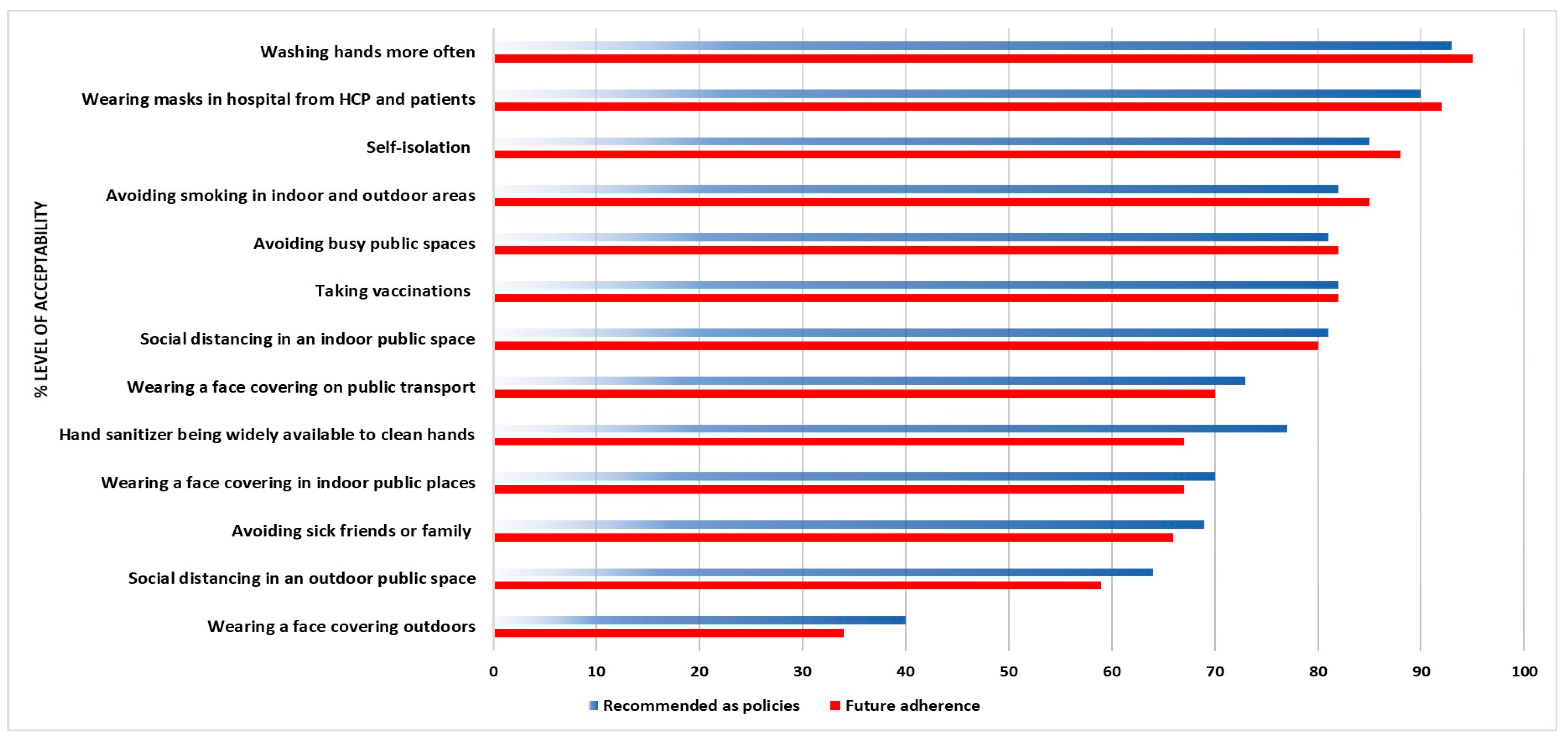
3.2. Future Acceptability with No Policies
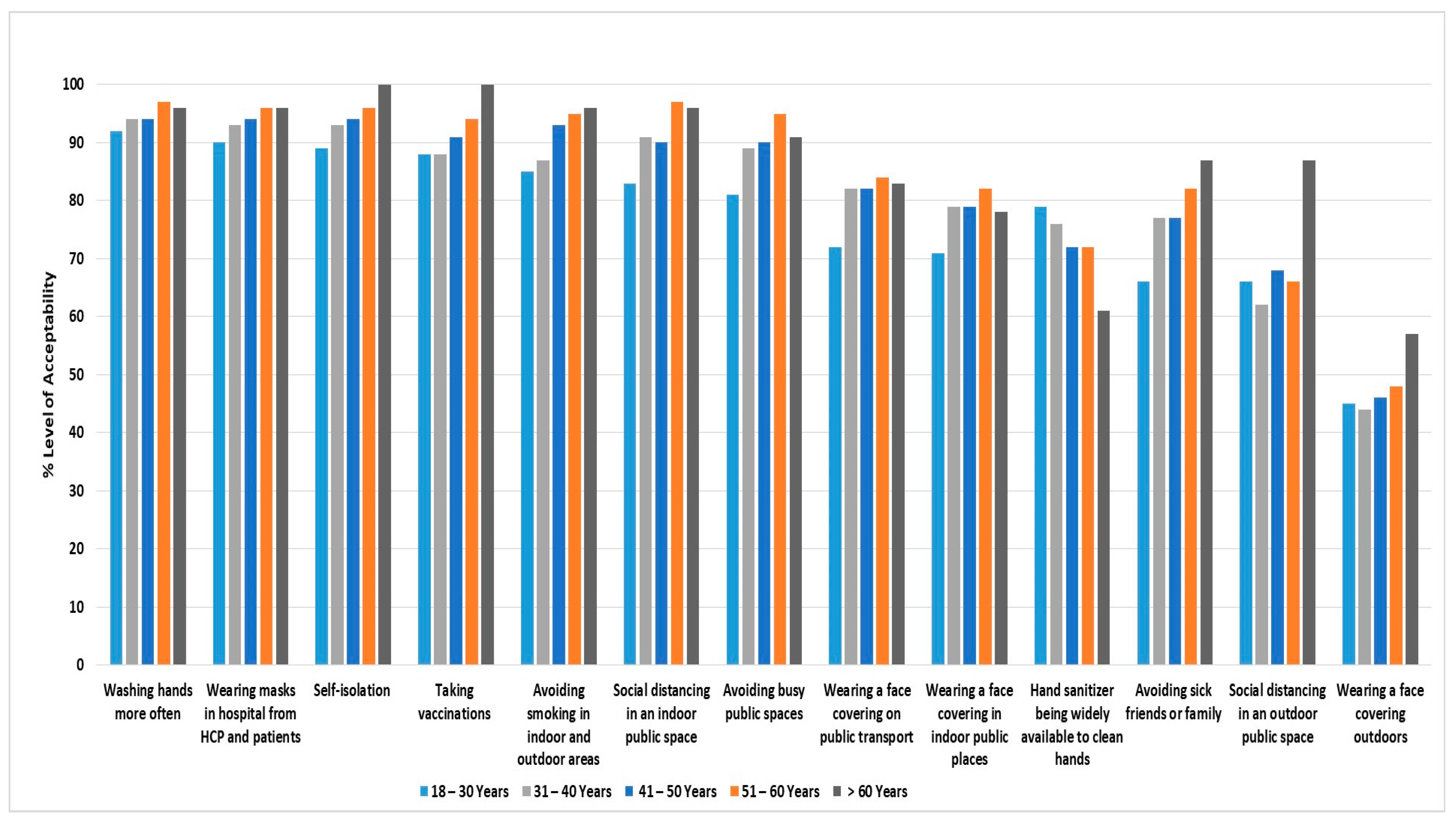
3.3. Acceptability of Future Policies
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- WHO. Coronavirus Disease (COVID-2019) Situation Report 2020. 2019. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/events-as-they-happen (accessed on 20 May 2022).
- Meo, S.A.; Alhowikan, A.M.; Al-Khlaiwi, T.; Meo, I.M.; Halepoto, D.M.; Iqbal, M.; Usmani, A.M.; Hajjar, W.; Ahmed, N. Novel coronavirus 2019-nCoV: Prevalence, biological and clinical characteristics comparison with SARS-CoV and MERS-CoV. Eur. Rev. Med. Pharmacol. Sci. 2020, 24, 2012–2019. [Google Scholar]
- Waseem, R.; Ullah, I.; Irfan, M.; Dominari, A.; Elmahi, O.K.O.; Tahir, M.J. MERS and COVID-19: A double burden for the healthcare system of Saudi Arabia. Health Sci. Rep. 2022, 5, e2515. [Google Scholar] [CrossRef]
- Teasdale, E.; Santer, M.; Geraghty, A.W.; Little, P.; Yardley, L. Public perceptions of non-pharmaceutical interventions for reducing transmission of respiratory infection: Systematic review and synthesis of qualitative studies. BMC Public Health 2014, 14, 589. [Google Scholar] [CrossRef]
- Idris, I.O.; Ayeni, G.O.; Adebisi, Y.A. Why many African countries may not achieve the 2022 COVID-19 vaccination coverage target. Trop. Med. Health 2022, 50, 15. [Google Scholar] [CrossRef]
- Parodi, S.M.; Liu, V.X. From Containment to Mitigation of COVID-19 in the US. JAMA 2020, 323, 1441–1442. [Google Scholar] [CrossRef] [Green Version]
- Kantor, B.N.; Kantor, J. Non-pharmaceutical Interventions for Pandemic COVID-19: A Cross-Sectional Investigation of US General Public Beliefs, Attitudes, and Actions. Front. Med. 2020, 7, 384. [Google Scholar] [CrossRef]
- Cowling, B.J.; Chan, K.H.; Fang, V.J.; Cheng, C.K.; Fung, R.O.; Wai, W.; Sin, J.; Seto, W.H.; Yung, R.; Chu, D.W.S.; et al. Facemasks and hand hygiene to prevent influenza transmission in households: A cluster randomized trial. Ann. Intern. Med. 2009, 151, 437–446. [Google Scholar] [CrossRef] [Green Version]
- Jefferson, T.; Foxlee, R.; Del Mar, C.; Dooley, L.; Ferroni, E.; Hewak, B.; Prabhala, A.; Nair, S.; Rivetti, A. Physical interventions to interrupt or reduce the spread of respiratory viruses: Systematic review. BMJ 2008, 336, 77–80. [Google Scholar] [CrossRef] [Green Version]
- Fricke, L.M.; Glöckner, S.; Dreier, M.; Lange, B. Impact of non-pharmaceutical interventions targeted at COVID-19 pandemic on influenza burden—A systematic review. J. Infect. 2021, 82, 1–35. [Google Scholar] [CrossRef]
- Berghaus, T.M.; Karschnia, P.; Haberl, S.; Schwaiblmair, M. Disproportionate decline in admissions for exacerbated COPD during the COVID-19 pandemic. Respir. Med. 2022, 191, 106120. [Google Scholar] [CrossRef]
- Tan, J.Y.; Conceicao, E.P.; Wee, L.E.; Sim, X.Y.J.; Venkatachalam, I. COVID-19 public health measures: A reduction in hospital admissions for COPD exacerbations. Thorax 2021, 76, 512–513. [Google Scholar] [CrossRef]
- Alqahtani, J.S.; Oyelade, T.; Aldhahir, A.M.; Mendes, R.G.; Alghamdi, S.M.; Miravitlles, M.; Mandal, S.; Hurst, J.R. Reduction in hospitalised COPD exacerbations during COVID-19: A systematic review and meta-analysis. PLoS ONE 2021, 16, e0255659. [Google Scholar] [CrossRef]
- Cheng, D.O.; Hurst, J.R. COVID-19 and ‘basal’ exacerbation frequency in COPD. Thorax 2021, 76, 432–433. [Google Scholar] [CrossRef]
- Al Naam, Y.A.; Elsafi, S.H.; Alkharraz, Z.S.; Alfahad, O.A.; Al-Jubran, K.M.; Al Zahrani, E.M. Community practice of using face masks for the prevention of COVID-19 in Saudi Arabia. PLoS ONE 2021, 16, e0247313. [Google Scholar] [CrossRef]
- Lau, J.T.; Yang, X.; Tsui, H.; Kim, J.H. Monitoring community responses to the SARS epidemic in Hong Kong: From day 10 to day 62. J. Epidemiol. Community Health 2003, 57, 864–870. [Google Scholar] [CrossRef]
- Alhazmi, A.M.; Alshammari, S.A.; Alenazi, H.A.; Shaik, S.A.; AlZaid, H.M.; Almahmoud, N.S.; Alshammari, H.S. Community’s compliance with measures for the prevention of respiratory infections in Riyadh, Saudi Arabia. J. Family Community Med. 2019, 26, 173–180. [Google Scholar]
- Hurst, J.R.; Cumella, A.; Niklewicz, C.N.; Philip, K.E.J.; Singh, V.; Hopkinson, N.S. Acceptability of hygiene, face covering and social distancing interventions to prevent exacerbations in people living with airways diseases. Thorax 2021, 77, 505–507. [Google Scholar] [CrossRef]
- Yardley, L.; Miller, S.; Teasdale, E.; Little, P. Using mixed methods to design a web-based behavioural intervention to reduce transmission of colds and flu. J. Health Psychol. 2011, 16, 353–364. [Google Scholar] [CrossRef]
- Gray, L.; MacDonald, C.; Mackie, B.; Paton, D.; Johnston, D.; Baker, M.G. Community responses to communication campaigns for influenza A (H1N1): A focus group study. BMC Public Health 2012, 12, 205. [Google Scholar] [CrossRef] [Green Version]
- Siu, J.Y. Another nightmare after SARS: Knowledge perceptions of and overcoming strategies for H1N1 influenza among chronic renal disease patients in Hong Kong. Qual. Health Res. 2010, 20, 893–904. [Google Scholar] [CrossRef]
- Cava, M.A.; Fay, K.E.; Beanlands, H.J.; McCay, E.A.; Wignall, R. Risk perception and compliance with quarantine during the SARS outbreak. J. Nurs. Scholarsh. 2005, 37, 343–347. [Google Scholar] [CrossRef]
- Ferng, Y.H.; Wong-McLoughlin, J.; Barrett, A.; Currie, L.; Larson, E. Barriers to mask wearing for influenza-like illnesses among urban Hispanic households. Public Health Nurs. 2011, 28, 13–23. [Google Scholar] [CrossRef]
- Seale, H.; Mak, J.P.I.; Razee, H.; MacIntyre, C.R. Examining the knowledge, attitudes and practices of domestic and international university students towards seasonal and pandemic influenza. BMC Public Health 2012, 12, 307. [Google Scholar] [CrossRef] [Green Version]
- Nizame, F.A.; Nasreen, S.; Unicomb, L.; Southern, D.; Gurley, E.S.; Arman, S.; Kadir, M.A.; Azziz-Baumgartner, E.; Luby, S.P.; Winch, P.J. Understanding community perceptions, social norms and current practice related to respiratory infection in Bangladesh during 2009: A qualitative formative study. BMC Public Health 2011, 11, 901. [Google Scholar] [CrossRef] [Green Version]
- Morrison, L.G.; Yardley, L. What infection control measures will people carry out to reduce transmission of pandemic influenza? A focus group study. BMC Public Health 2009, 9, 258. [Google Scholar] [CrossRef] [Green Version]
- Alqahtani, J.S.; Oyelade, T.; Aldhahir, A.M.; Alghamdi, S.M.; Almehmadi, M.; Alqahtani, A.S.; Quaderi, S.; Mandal, S.; Hurst, J.R. Prevalence, Severity and Mortality associated with COPD and Smoking in patients with COVID-19: A Rapid Systematic Review and Meta-Analysis. PLoS ONE 2020, 15, e0233147. [Google Scholar] [CrossRef]
- Alqahtani, J.S.; AlRabeeah, S.M.; Aldhahir, A.M.; Siraj, R.; Aldabayan, Y.S.; Alghamdi, S.M.; Alqahtani, A.S.; Alsaif, S.S.; Naser, A.Y.; Alwafi, H. Sleep Quality, Insomnia, Anxiety, Fatigue, Stress, Memory and Active Coping during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2022, 19, 4940. [Google Scholar] [CrossRef]
- Alqahtani, J.S. Prevalence, incidence, morbidity and mortality rates of COPD in Saudi Arabia: Trends in burden of COPD from 1990 to 2019. PLoS ONE 2022, 17, e0268772. [Google Scholar] [CrossRef]
- Alqahtani, J.S.; Alghamdi, S.M.; Aldhahir, A.M.; Althobiani, M.; Oyelade, T. Key toolkits of non-pharmacological management in COPD: During and beyond COVID-19. Front. Biosci. 2021, 26, 246–252. [Google Scholar] [CrossRef]
- Kisielinski, K.; Giboni, P.; Prescher, A.; Klosterhalfen, B.; Graessel, D.; Funken, S.; Kempski, O.; Hirsch, O. Is a Mask That Covers the Mouth and Nose Free from Undesirable Side Effects in Everyday Use and Free of Potential Hazards? Int. J. Environ. Res. Public Health 2021, 18, 4344. [Google Scholar] [CrossRef]
- Grundmann, F.; Epstude, K.; Scheibe, S. Face masks reduce emotion-recognition accuracy and perceived closeness. PLoS ONE 2021, 16, e0249792. [Google Scholar] [CrossRef] [PubMed]
- Han, S.; Zhang, T.; Lyu, Y.; Lai, S.; Dai, P.; Zheng, J.; Yang, W.; Zhou, X.H.; Feng, L. Influenza’s plummeting during the COVID-19 pandemic: The roles of mask-wearing, mobility change, and SARS-CoV-2 interference. Engineering 2022. Epub ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Aldabayan, Y.S.; Ridsdale, H.A.; Alrajeh, A.M.; Aldhahir, A.M.; Lemson, A.; Alqahtani, J.S.; Brown, J.S.; Hurst, J.R. Pulmonary rehabilitation, physical activity and aortic stiffness in COPD. Respir. Res. 2019, 20, 166. [Google Scholar] [CrossRef] [Green Version]
- Alqahtani, J.S.; Aldhahir, A.M.; Oyelade, T.; Alghamdi, S.M.; Almamary, A.S. Smoking cessation during COVID-19: The top to-do list. NPJ Prim. Care Respir. Med. 2021, 31, 22. [Google Scholar] [CrossRef] [PubMed]

| Characteristics | N (%) or Median IQR |
|---|---|
| Gender | |
| Male | 571 (28%) |
| Female | 1486 (72%) |
| Age | |
| 18–30 years | 933 (45.4%) |
| 31–40 years | 483 (23.5%) |
| 41–50 years | 448 (21.8%) |
| 51–60 years | 170 (8.3%) |
| >60 years | 23 (1.1%) |
| Body Mass Index (BMI) | 26 (22–30) |
| Education Level | |
| No formal schooling | 12 (0.6%) |
| Elementary school | 14 (0.7%) |
| Intermediate school | 65 (3.2%) |
| High school | 511 (24.8%) |
| Diploma | 240 (11.7%) |
| Bachelor’s | 1114 (54.2%) |
| Master’s | 70 (3.4%) |
| Ph.D. | 31 (1.5%) |
| Region | |
| Central | 545 (26.5%) |
| Eastern | 372 (18.1%) |
| Northern | 183 (8.9%) |
| Southern | 122 (5.9%) |
| Western | 835 (40.6%) |
| Where do you live? | |
| Rural area | 245 (11.5%) |
| Urban area | 1812 (88.1%) |
| Comorbidities | |
| Chronic lung disease | 72 (3.5%) |
| Cardiac disease | 22 (1.1%) |
| High blood pressure | 128 (6.2%) |
| Kidney disease | 9 (0.4%) |
| Diabetes | 123 (6%) |
| Stomach disease | 81 (3.9%) |
| Liver disease | 8 (0.4%) |
| Anemia or other blood disease | 85 (4.1%) |
| Cancer | 7 (0.3%) |
| Depression | 70 (3.4%) |
| Osteoarthritis | 70 (3.4%) |
| Smoking history | |
| Never smoked | 1697 (82.5%) |
| Current smoker | 259 (12.5%) |
| Former smoker | 101 (4.9%) |
| Pack-years | 10 (5–20) |
| If a smoker, have you attempted to quit during the COVID-19 pandemic? | 174/259 (67%) |
| Have you been infected with COVID-19? | |
| Yes | 889 (43.2%) |
| Severity of COVID-19 infection | |
| Mild | 250 (28%) |
| Moderate | 501 (56%) |
| Severe | 138 (16%) |
| Did any of your close family members get infected with COVID-19? | |
| Yes | 1716 (83.4%) |
| No | 314 (16.6%) |
| Have you lost any loved ones because of the COVID-19 infection? | |
| Yes | 572 (27.8%) |
| No | 1485 (72.2%) |
| Have you been vaccinated against COVID-19? | |
| Yes | 2028 (98%) |
| First dose (Incomplete vaccination) | 19 (1%) |
| Second dose | 807 (40%) |
| Booster dose | 1202 (59%) |
| Respiratory Infection Control Measure | Thinking about the Future, after Restrictions Have Been Eased and People Get Vaccinated against COVID-19, Which One Would You Do (Even If It Was Not Policy); N (%) | Which of the Following Do You Think Should Continue in the Future as a Policy For Everyone at All Times? N (%) |
|---|---|---|
| Washing hands more often | 1910 (93%) | 1923 (93%) |
| Wearing masks in hospitals (both HCP and patients) | 1886 (92%) | 1894 (92%) |
| Self-isolating if they were in contact with someone who was infected with COVID-19 | 1878 (91%) | 1889 (92%) |
| Taking vaccinations as recommended by the ministry of Health | 1793 (87%) | 1838 (89%) |
| Avoiding smoking in indoor and outdoor areas | 1759 (86%) | 1814 (88%) |
| Keeping more of a distance from others when in an indoor public space | 1722 (84%) | 1806 (88%) |
| Avoiding busy public spaces | 1689 (82%) | 1838 (89%) |
| Wearing a face covering on public transportation | 1509 (73%) | 1596 (78%) |
| Wearing a face covering in indoor public places | 1438 (70%) | 1554 (76%) |
| Having hand sanitizer be widely available to clean hands | 1382 (67%) | 1565 (76%) |
| Avoiding seeing friends or family if they are unwell with a cold or flu | 1304 (63%) | 1493 (73%) |
| Keeping more of a distance from others when in an outdoor public space | 1243 (60%) | 1353 (66%) |
| Wearing a face covering outdoors | 793 (39%) | 928 (45%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alqahtani, J.S.; Aldhahir, A.M.; AlRabeeah, S.M.; Alsenani, L.B.; Alsharif, H.M.; Alshehri, A.Y.; Alenazi, M.M.; Alnasser, M.; Alqahtani, A.S.; AlDraiwiesh, I.A.; et al. Future Acceptability of Respiratory Virus Infection Control Interventions in General Population to Prevent Respiratory Infections. Medicina 2022, 58, 838. https://doi.org/10.3390/medicina58070838
Alqahtani JS, Aldhahir AM, AlRabeeah SM, Alsenani LB, Alsharif HM, Alshehri AY, Alenazi MM, Alnasser M, Alqahtani AS, AlDraiwiesh IA, et al. Future Acceptability of Respiratory Virus Infection Control Interventions in General Population to Prevent Respiratory Infections. Medicina. 2022; 58(7):838. https://doi.org/10.3390/medicina58070838
Chicago/Turabian StyleAlqahtani, Jaber S., Abdulelah M. Aldhahir, Saad M. AlRabeeah, Lujain B. Alsenani, Haifa M. Alsharif, Amani Y. Alshehri, Mayadah M. Alenazi, Musallam Alnasser, Ahmed S. Alqahtani, Ibrahim A. AlDraiwiesh, and et al. 2022. "Future Acceptability of Respiratory Virus Infection Control Interventions in General Population to Prevent Respiratory Infections" Medicina 58, no. 7: 838. https://doi.org/10.3390/medicina58070838
APA StyleAlqahtani, J. S., Aldhahir, A. M., AlRabeeah, S. M., Alsenani, L. B., Alsharif, H. M., Alshehri, A. Y., Alenazi, M. M., Alnasser, M., Alqahtani, A. S., AlDraiwiesh, I. A., Alghamdi, S. M., Siraj, R. A., Alqahtani, H. S., Sreedharan, J. K., Alqahtani, A. S., & Alzahrani, E. M. (2022). Future Acceptability of Respiratory Virus Infection Control Interventions in General Population to Prevent Respiratory Infections. Medicina, 58(7), 838. https://doi.org/10.3390/medicina58070838










