An Evaluation of Jaw Tracking Movements in Patients with Total Joint Replacements versus a Control Group
Abstract
:1. Introduction
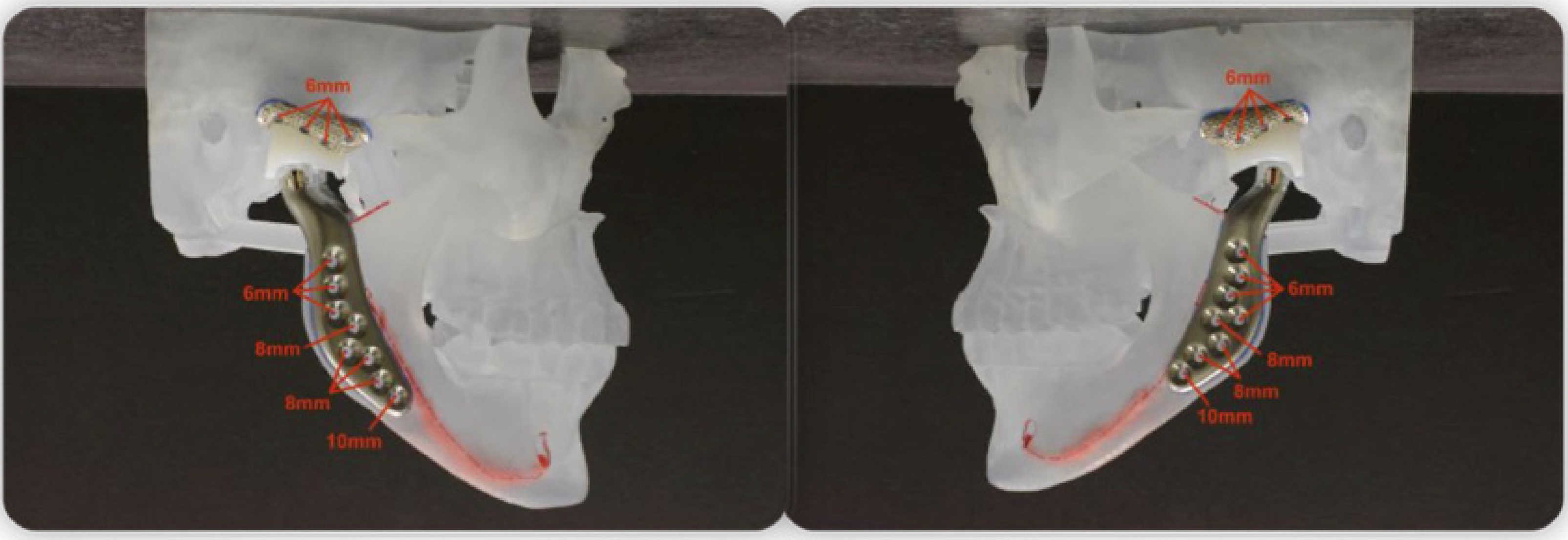
2. Materials and Methods
2.1. Study Design
2.2. Sample
- (1)
- Anterior open bite (AOB);
- (2)
- Class I or II malocclusions;
- (3)
- Subject age range 18–66 years;
- (4)
- Patients who had been diagnosed with condylar resorption and underwent joint replacements;
- (5)
- Patients with a record in the Department of Oral and Maxillofacial Surgery or orthodontic department.
- (1)
- Presence of craniofacial syndromes;
- (2)
- Did not wish to participate;
- (3)
- Age under 18 years;
- (4)
- Presence of craniofacial deformities;
- (5)
- Association with any orofacial trauma.
2.3. Control Group
2.4. Informed Consent
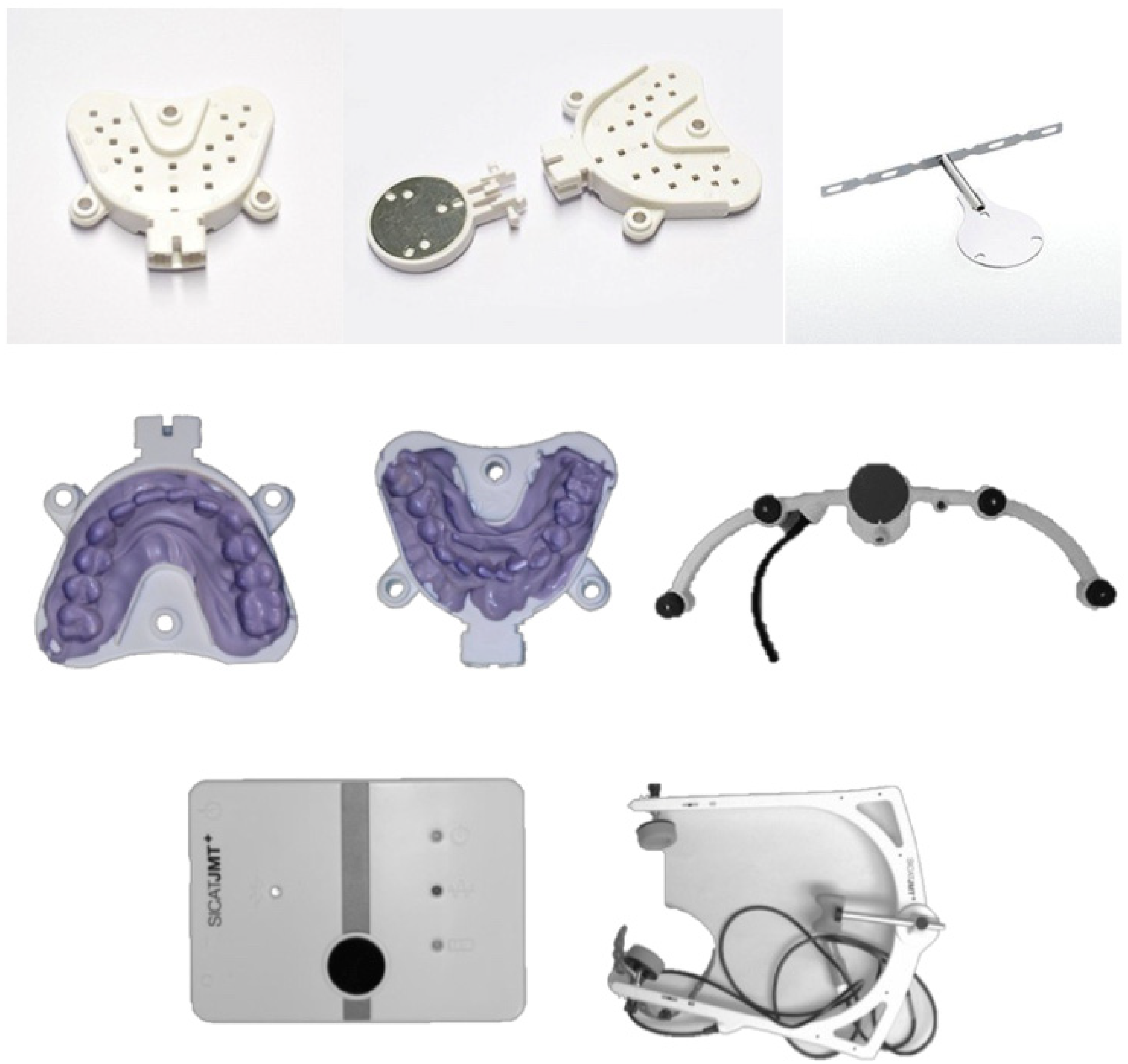
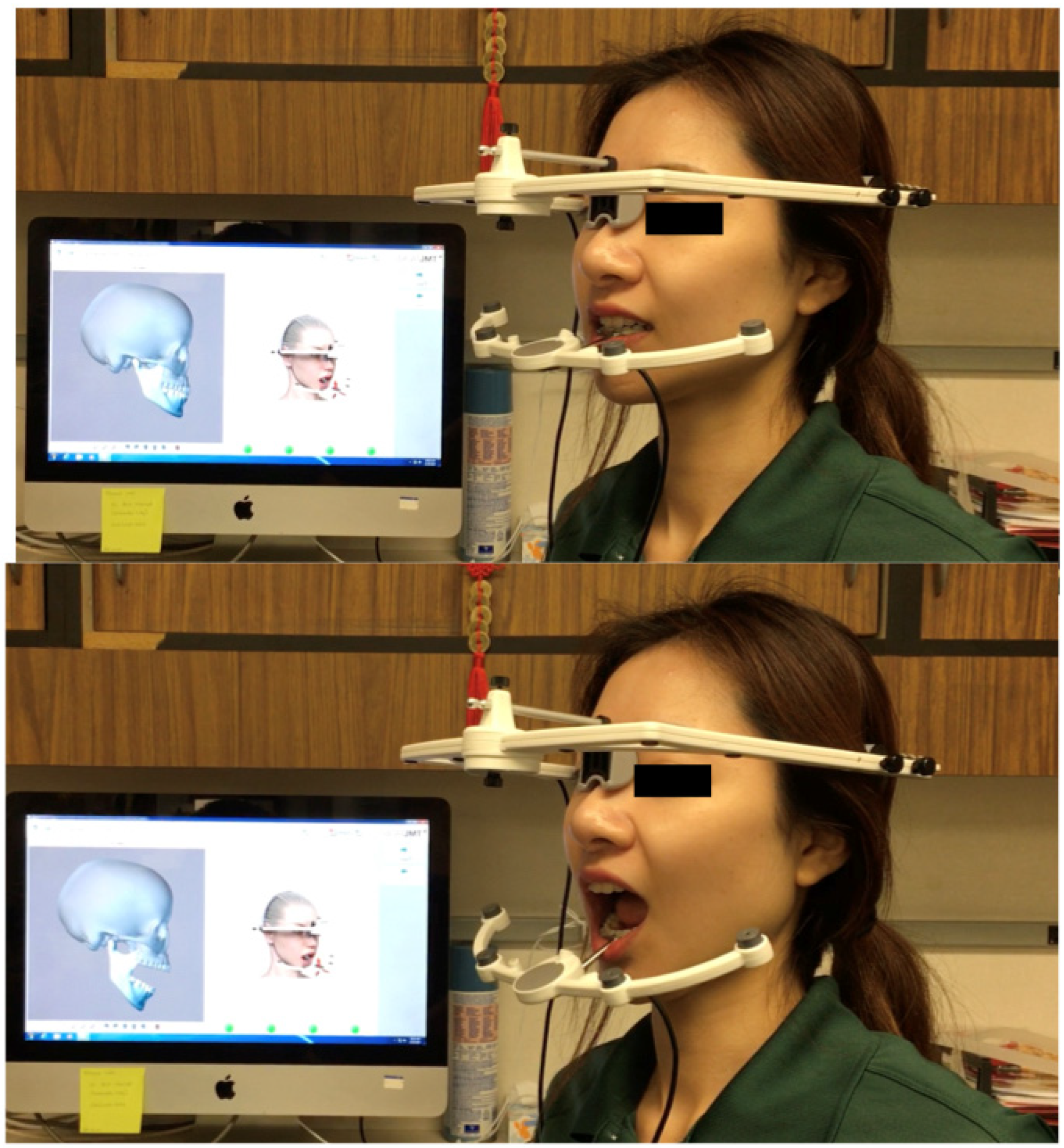
2.5. Jaw Tracking Procedure
2.6. Statistical Analysis
3. Results
3.1. Sample Size
3.2. Clinical Evaluation
3.3. Jaw Movement Evaluation
4. Discussion
5. Conclusions
- TMJ replacement patients showed significantly limited jaw movements compared to the control group. These limitations were present in all range of motion movements.
- A small percentage of TMJ replacement patients still presented low levels of pain but an improved chewing ability and quality of life. This represented an overall improvement in the symptoms experienced by patients.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Okeson, J. Etiology and identification of functional disturbances in the masticatory system. Manag. Temporomandibular Disord. Occlusion 2008, 147–364. [Google Scholar]
- Stoll, M.L.; Kau, C.H.; Waite, P.D.; Cron, R.Q. Temporomandibular joint arthritis in juvenile idiopathic arthritis, now what? Pediatr. Rheumatol. 2018, 16, 32. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stoustrup, P.; Kristensen, K.D.; Küseler, A.; Gelineck, J.; Cattaneo, P.M.; Pedersen, T.K.; Herlin, T. Condylar lesions in relation to mandibular growth in untreated and intra-articular corticosteroid-treated experimental temporomandibular joint arthritis. Clin. Exp. Rheumatol. 2010, 28, 576–583. [Google Scholar] [PubMed]
- Stoustrup, P.; Kristensen, K.D.; Küseler, A.; Verna, C.; Herlin, T.; Pedersen, T.K. Management of temporomandibular joint arthritis-related orofacial symptoms in juvenile idiopathic arthritis by the use of a stabilization splint. Scand. J. Rheumatol. 2013, 43, 137–145. [Google Scholar] [CrossRef]
- Kinard, B.; Goldberg, B.; Kau, C.; Abramowicz, S. Clinical trials of temporomandibular joint involvement of juvenile idiopathic arthritis. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2021, 131, 617–619. [Google Scholar] [CrossRef]
- Kau, C.H.; Allareddy, V.; Stoustrup, P.; Pedersen, T.; Kinard, B.; Cron, R.Q.; Stoll, M.L.; Gilbert, G.H. Management of juvenile idiopathic arthritis: Preliminary qualitative findings from the National Dental Practice-Based Research Network. J. World Fed. Orthod. 2021, 10, 70–73. [Google Scholar] [CrossRef]
- Thilander, B.; Rubio, G.; Pena, L.; De Mayorga, C. Prevalence of temporomandibular dysfunction and its association with malocclusion in children and adolescents: An epidemiologic study related to specified stages of dental development. Angle Orthod. 2002, 72, 146–154. [Google Scholar]
- Celebi, A.A.; Cron, R.; Stoll, M.; Simsek, S.; Kinard, B.; Waite, P.D.; Wang, J.; Vo, V.; Tran, L.; Kau, C.H. Comparison of the Condyle-Fossa Relationship and Resorption Between Patients With and Without Juvenile Idiopathic Arthritis (JIA). J. Oral Maxillofac. Surg. 2022, 80, 422–430. [Google Scholar] [CrossRef]
- Wong, M.E.; Kau, C.H.; Melville, J.C.; Patel, T.; Spagnoli, D.B. Bone Reconstruction Planning Using Computer Technology for Surgical Management of Severe Maxillomandibular Atrophy. Oral Maxillofac. Surg. Clin. N. Am. 2019, 31, 457–472. [Google Scholar] [CrossRef]
- Sansare, K.; Raghav, M.; Mallya, S.; Karjodkar, F. Management-related outcomes and radiographic findings of idiopathic condylar resorption: A systematic review. Int. J. Oral Maxillofac. Surg. 2015, 44, 209–216. [Google Scholar] [CrossRef]
- Kau, C.H.; Bejemir, M.P. Application of virtual three-dimensional surgery planning in management of open bite with idiopathic condylar resorption. Ann. Maxillofac. Surg. 2015, 5, 249–254. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rahman, F.; Celebi, A.A.; Louis, P.J.; Kau, C.H. A comprehensive treatment approach for idiopathic condylar resorption and anterior open bite with 3D virtual surgical planning and self-ligated customized lingual appliance. Am. J. Orthod. Dentofac. Orthop. 2019, 155, 560–571. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Veiszenbacher, E.; Waite, P.D.; Kau, C.H. Comprehensive treatment approach for bilateral idiopathic condylar resorption and anterior open bite with customized lingual braces and total joint prostheses. Am. J. Orthod. Dentofac. Orthop. 2019, 156, 125–136. [Google Scholar] [CrossRef]
- Kau, C.H.; Almakky, O.; Louis, P.J. Team approach in the management of revision surgery to correct bilateral temporomandibular joint replacements. J. Orthod. 2020, 47, 156–162. [Google Scholar] [CrossRef] [PubMed]
- Mercuri, L.G.; Sanders, B.; White, R.D.; Hurder, A.; Henderson, W. Custom CAD/CAM total temporomandibular joint reconstruction system: Preliminary multicenter report. J. Oral Maxillofac. Surg. 1995, 53, 106–116. [Google Scholar] [CrossRef]
- Quinn, P.D. Total temporomandibular joint reconstruction. Oral Maxillofac. Surg. Clin. N. Am. 2000, 12, 93–104. [Google Scholar] [CrossRef]
- Leandro, L.F.; Loureiro, C.C.; Marinho, K.; Guevara, H.A. A ten-year experience and follow-up of three hundred patients fitted with the Biomet/Lorenz Microfixation TMJ replacement system. Int. J. Oral Maxillofac. Surg. 2013, 42, 1007–1013. [Google Scholar] [CrossRef]
- Wojczyńska, A.; Leiggener, C.S.; Bredell, M.; Ettlin, D.A.; Erni, S.; Gallo, L.M.; Colombo, V. Alloplastic total temporomandibular joint replacements: Do they perform like natural joints? Prospective cohort study with a historical control. Int. J. Oral Maxillofac. Surg. 2016, 45, 1213–1221. [Google Scholar] [CrossRef] [Green Version]
- Baltali, E.; Zhao, K.D.; Koff, M.F.; Keller, E.E.; An, K.-N. Accuracy and precision of a method to study kinematics of the temporomandibular joint: Combination of motion data and CT imaging. J. Biomech. 2008, 41, 2581–2584. [Google Scholar] [CrossRef] [Green Version]
- Linsen, S.S.; Schon, A.; Mercuri, L.G.; Teschke, M. Unilateral, Alloplastic Temporomandibular Joint Reconstruction, Biomechanically What Happens to the Contralateral Temporomandibular Joint?-A Prospective Cohort Study. J. Oral Maxillofac. Surg. 2021, 79, 2016–2029. [Google Scholar] [CrossRef]
- Linsen, S.; Schmidt-Beer, U.; Fimmers, R.; Grüner, M.; Koeck, B. Craniomandibular Pain, Bite Force, and Oral Health-Related Quality of Life in Patients with Jaw Resection. J. Pain Symptom Manag. 2009, 37, 94–106. [Google Scholar] [CrossRef] [PubMed]
- Kau, C.H.; He, S.; Liao, L.; Kinderknecht, K.; Ow, A.; Saleh, T.A. The use of a dynamic real-time jaw tracking device and cone beam computed tomography simulation. Ann. Maxillofac. Surg. 2016, 6, 113–119. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aslanidou, K.; Xie, R.; Christou, T.; Lamani, E.; Kau, C.H. Evaluation of temporomandibular joint function after orthognathic surgery using a jaw tracker. J. Orthod. 2020, 47, 140–148. [Google Scholar] [CrossRef] [PubMed]
- Linsen, S.S.; Wolf, M.; Müßig, D. Long-term outcomes of mandibular kinematics following class II malocclusion therapy with removable functional appliance therapy. Cranio 2016, 34, 363–370. [Google Scholar] [CrossRef] [PubMed]
- Goldstein, G.; DeSantis, L.; Goodacre, C. Bruxism: Best Evidence Consensus Statement. J. Prosthodont. 2020, 30, 91–101. [Google Scholar] [CrossRef]
- Lobbezoo, F.; Ahlberg, J.; Glaros, A.G.; Kato, T.; Koyano, K.; Lavigne, G.J.; De Leeuw, R.; Manfredini, D.; Svensson, P.; Winocur, E. Bruxism defined and graded: An international consensus. J. Oral Rehabil. 2012, 40, 2–4. [Google Scholar] [CrossRef]
- Kau, C.H.; Aslanidou, K.; Vlachos, C.; Saleh, T.A. The fabrication of a customized occlusal splint based on the merging of dynamic jaw tracking records, cone beam computed tomography, and CAD-CAM digital impression. J. Orthod. Sci. 2017, 6, 104–109. [Google Scholar] [CrossRef]
- Peltomäki, T.; Rönning, O. Interrelationship between size and tissue-separating potential of costochondral transplants. Eur. J. Orthod. 1991, 13, 459–465. [Google Scholar] [CrossRef]
- Guyuron, B.; Lasa, C.I. Unpredictable growth pattern of costochondral graft. Plast. Reconstr. Surg. 1992, 90, 880–886. [Google Scholar] [CrossRef]
- Wolford, L.M.; Cardenas, L. Idiopathic condylar resorption: Diagnosis, treatment protocol, and outcomes. Am. J. Orthod. Dentofac. Orthop. 1999, 116, 667–677. [Google Scholar] [CrossRef]
- Troulis, M.J.; Tayebaty, F.T.; Papadaki, M.; Williams, W.B.; Kaban, L.B. Condylectomy and Costochondral Graft Reconstruction for Treatment of Active Idiopathic Condylar Resorption. J. Oral Maxillofac. Surg. 2008, 66, 65–72. [Google Scholar] [CrossRef] [PubMed]
- Scheerlinck, J.P.; Stoelinga, P.J.; Blijdorp, P.A.; Brouns, J.J.; Nijs, M.L. Sagittal split advancement osteotomies stabilized with miniplates. A 2-5-year follow-up. Int. J. Oral Maxillofac. Surg. 1994, 23, 127–131. [Google Scholar] [CrossRef]
- Kerstens, H.; Tuinzing, D.; Golding, R.; van der Kwast, W. Condylar atrophy and osteoarthrosis after bimaxillary surgery. Oral Surg. Oral Med. Oral Pathol. 1990, 69, 274–280. [Google Scholar] [CrossRef]
- Bouwman, J.P.; Kerstens, H.C.; Tuinzing, D.B. Condylar resorption in orthognathic surgery. The role of intermaxillary fixation. Oral Surg. Oral Med. Oral Pathol. 1994, 78, 138–141. [Google Scholar] [CrossRef]
- Schellhas, K.; Wilkes, C.; Fritts, H.; Omlie, M.R.; Lagrotteria, L. MR of osteochondritis dissecans and avascular necrosis of the mandibular condyle. Am. J. Roentgenol. 1989, 152, 551–560. [Google Scholar] [CrossRef] [Green Version]
- Ferreira, F.M.; Cunali, R.S.; Bonotto, D.; De Farias, A.C.; Cunali, P.A. Total temporomandibular joint alloplastic reconstruction. Rev. Dor 2014, 15, 211–214. [Google Scholar] [CrossRef]
- Mercuri, L. Alloplastic temporomandibular joint replacement: Rationale for the use of custom devices. Int. J. Oral Maxillofac. Surg. 2012, 41, 1033–1040. [Google Scholar] [CrossRef]
- Guarda-Nardini, L.; Manfredini, D.; Ferronato, G. Temporomandibular joint total replacement prosthesis: Current knowledge and considerations for the future. Int. J. Oral Maxillofac. Surg. 2008, 37, 103–110. [Google Scholar] [CrossRef]
- Wolford, L.M.; Dingwerth, D.J.; Talwar, R.M.; Pitta, M.C. Comparison of 2 temporomandibular joint total joint prosthesis systems. J. Oral Maxillofac. Surg. 2003, 61, 685–690. [Google Scholar] [CrossRef]
- Macfarlane, T.; Glenny, A.-M.; Worthington, H. Systematic review of population-based epidemiological studies of oro-facial pain. J. Dent. 2001, 29, 451–467. [Google Scholar] [CrossRef]
- Mezitis, M.; Rallis, G.; Zachariades, N. The normal range of mouth opening. J. Oral Maxillofac. Surg. 1989, 47, 1028–1029. [Google Scholar] [CrossRef]
- Tzanidakis, K.; Sidebottom, A.J. Outcomes of open temporomandibular joint surgery following failure to improve after arthroscopy: Is there an algorithm for success? Br. J. Oral Maxillofac. Surg. 2013, 51, 818–821. [Google Scholar] [CrossRef] [PubMed]
- Gruber, E.A.; McCullough, J.; Sidebottom, A.J. Medium-term outcomes and complications after total replacement of the temporomandibular joint. Prospective outcome analysis after 3 and 5 years. Br. J. Oral Maxillofac. Surg. 2015, 53, 412–415. [Google Scholar] [CrossRef] [PubMed]
- Wolford, L.M.; Pitta, M.C.; Reiche-Fischel, O.; Franco, P.F. TMJ Concepts/Techmedica custom-made TMJ total joint prosthesis: 5-year follow-up study. Int. J. Oral Maxillofac. Surg. 2003, 32, 268–274. [Google Scholar] [CrossRef] [PubMed]
- Celebi, N.; Rohner, E.C.; Gateno, J.; Noble, P.C.; Ismaily, S.K.; Teichgraeber, J.F.; Xia, J.J. Development of a Mandibular Motion Simulator for Total Joint Replacement. J. Oral Maxillofac. Surg. 2010, 69, 66–79. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Variables | Number | Age (years) | Gender |
|---|---|---|---|
| Total joint replacement group | 15 | 45.4 ± 16.7 | 15 females |
| Control group | 15 | 39.6 ± 9.6 | 15 females |
| Outcome Comparisons | Total Joint Replacement (n = 15) | Control (n = 15) | p-Value |
|---|---|---|---|
| Clicking (Reported) Right | 1 (6.7%) | 0 (0.0%) | 0.0996 |
| Clicking (Reported) Left | 1 (6.7%) | 0 (0.0%) | 0.0996 |
| Clicking (On exam) Right | 0 (0.0%) | 0 (0.0%) | 1.000 |
| Clicking (On exam) Left | 0 (0.0%) | 0 (0.0%) | 1.000 |
| Popping Left | 0 (0.0%) | 1 (6.7%) | 0.0996 |
| Crepitation (Reported) Right | 1 (6.7%) | 1 (6.7%) | 1.0000 |
| Crepitation (Reported) Left | 0 (0.0%) | 0 (0.0%) | 1.000 |
| Crepitation (On exam) Right | 1 (6.7%) | 0 (0.0%) | 1.000 |
| Crepitation (On exam) Left | 0 (0.0%) | 0 (0.0%) | 1.000 |
| Constant pain Right | 1 (6.7%) | 0 (0.0%) | 0.041 |
| Constant pain Left | 1 (7.1%) | 0 (0.0%) | 0.041 |
| Pain in movements Right | 3 (20.0%) | 0 (0.0%) | 0.011 |
| Pain in movements Left | 3 (20.0%) | 0 (0.0%) | 0.011 |
| Stiffness | 3 (20.0%) | 0 (0.0%) | 0.011 |
| Muscular pain | 1 (6.7%) | 0 (0.0%) | 0.041 |
| Headaches | 2 (13.3%) | 0 (0.0%) | 0.011 |
| Migraines | 1 (6.7%) | 0 (0.0%) | 0.012 |
| Bruxism/clenching | 3 (20.0%) | 1 (6.7%) | 0.778 |
| Chewing ability better | 15 (100%) | NA | |
| VAS pain score | 1.9 ± 1.8 | 0.00 | 0.012 * |
| Mandibular Movements | Total Joint Replacement Group (Median Values) | Control Group (Median) | p-Value |
|---|---|---|---|
| Left lateral | 1.9 ± 2.7 (1.5) | 9.7 ± 1.4 (9.2) | <0.0001 |
| Right lateral | 1.7 ± 1.7 (1.2) | 9.7 ± 1.6 (9.3) | <0.0001 |
| Protrusion | 2.8 ± 2.1 (2.3) | 9.9 ± 1.5 (9.3) | <0.0001 |
| Opening (MIO) | 33.5 ± 5.5 (36.2) | 46.6 ± 8.2 (46.1) | <0.0001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rahman, F.; Femiano, F.; Louis, P.J.; Kau, C.H. An Evaluation of Jaw Tracking Movements in Patients with Total Joint Replacements versus a Control Group. Medicina 2022, 58, 738. https://doi.org/10.3390/medicina58060738
Rahman F, Femiano F, Louis PJ, Kau CH. An Evaluation of Jaw Tracking Movements in Patients with Total Joint Replacements versus a Control Group. Medicina. 2022; 58(6):738. https://doi.org/10.3390/medicina58060738
Chicago/Turabian StyleRahman, Farhana, Felice Femiano, Patrick J Louis, and Chung How Kau. 2022. "An Evaluation of Jaw Tracking Movements in Patients with Total Joint Replacements versus a Control Group" Medicina 58, no. 6: 738. https://doi.org/10.3390/medicina58060738
APA StyleRahman, F., Femiano, F., Louis, P. J., & Kau, C. H. (2022). An Evaluation of Jaw Tracking Movements in Patients with Total Joint Replacements versus a Control Group. Medicina, 58(6), 738. https://doi.org/10.3390/medicina58060738








