Approach to Thrombophilia in Pregnancy—A Narrative Review
Abstract
1. Introduction
2. Aetiology of Thrombophilia
Particularities of the Hemostatic System in Pregnancy
3. Classification of Thrombophilias
3.1. Hereditary Thrombophilia
3.2. Acquired Thrombophilia
3.3. Grading the Risk
3.3.1. High Risk Thrombophilia
Antithrombin III Deficiency (AT III)
Protein C and S Deficiencies
3.3.2. Moderate Risk Thrombophilia
Activated Protein C Resistance and Factor V Leiden
Prothrombin Gene Mutation (Factor II)
Factor VIII
3.3.3. Low Risk Thrombophilia
Hyperhomocysteinemia
4. Thrombophilias and Complications in Pregnancy
4.1. Screening Options
4.2. Clinical Evaluation
4.3. Methodology and Patient Management
4.3.1. Anticoagulants during Pregnancy
4.3.2. Thrombolytics during Pregnancy
4.4. Prevention
Prevention for Adverse Pregnancy-Related Complications
4.5. Prognostic Outcomes
5. Micro RNAs in Pregnancy
6. Conclusions
- In screening, the degree of genetic damage that manifests as thrombotic risk is assessed. Depending on this, treatment with anticoagulant and antiaggregant drugs is tailor-made for each patient.
- Following the high degree of risk amplified by the evolution of pregnancy, the frequency of patient monitoring will be increased to avoid any thrombotic event that could endanger pregnancy.
- Postpartum, antithrombotic prevention will be maintained, therapy being adapted to the degree of risk associated with the severity of thrombophilia.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Campello, E.; Spiezia, L.; Adamo, A.; Simioni, P. Thrombophilia, risk factors and prevention. Expert Rev. Hematol. 2019, 12, 147–158. [Google Scholar] [CrossRef] [PubMed]
- Simcox, L.E.; Ormesher, L.; Tower, C.; Greer, I.A. Thrombophilia and Pregnancy Complications. Int. J. Mol. Sci. 2015, 16, 28418–28428. [Google Scholar] [CrossRef] [PubMed]
- Ahangari, N.; Doosti, M.; Mousavifar, N.; Attaran, M.; Shahrokhzadeh, S.; Memarpour, S.; Ghayoor Karimiani, E. Hereditary thrombophilia genetic variants in recurrent pregnancy loss. Arch. Gynecol. Obstet. 2019, 300, 777–782. [Google Scholar] [CrossRef] [PubMed]
- Pacurar, R.; Ionita, H.; Nicola, D. Trombofiliile Ereditare; Editura Victor Babes: Timisoara, Romania, 2010. [Google Scholar]
- Middeldorp, S. Inherited thrombophilia: A double-edged sword. Hematol. Am. Soc. Hematol. Educ. Program 2016, 2016, 1–9. [Google Scholar] [CrossRef]
- Bates, S.M.; Rajasekhar, A.; Middeldorp, S.; McLintock, C.; Rodger, M.A.; James, A.H.; Vazquez, S.R.; Greer, I.A.; Riva, J.J.; Bhatt, M.; et al. American Society of Hematology 2018 guidelines for management of venous thromboembolism: Venous thromboembolism in the context of pregnancy. Blood Adv. 2018, 2, 3317–3359. [Google Scholar] [CrossRef]
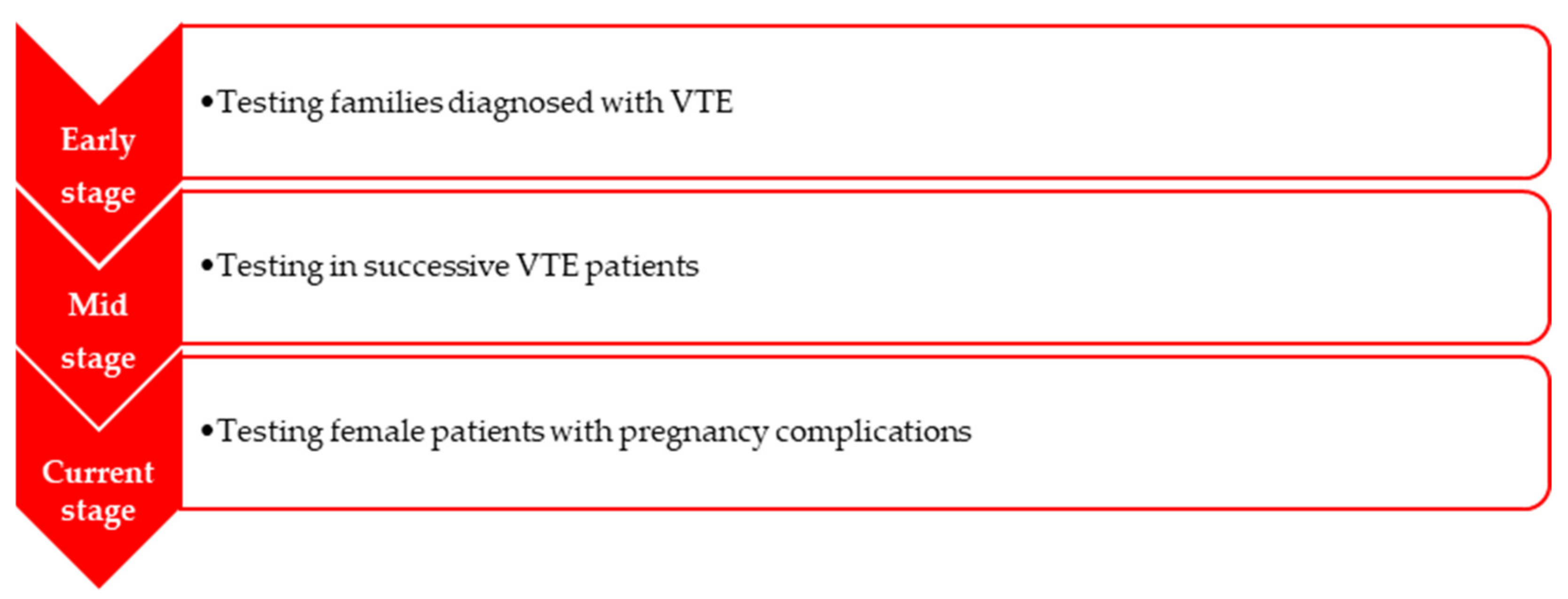
- Middeldorp, S.; Coppens, M. Evolution of thrombophilia testing. Hema 2013, 7, 375–382. [Google Scholar]
- Friederich, P.W.; Sanson, B.J.; Simioni, P.; Zanardi, S.; Huisman, M.V.; Kindt, I.; Prandoni, P.; Büller, H.R.; Girolami, A.; Prins, M.H. Frequency of pregnancy-related venous thromboembolism in anticoagulant factor-deficient women: Implications for prophylaxis. Ann. Intern. Med. 1996, 125, 955–960. [Google Scholar] [CrossRef]
- Fogerty, A.E.; Connors, J.M. Management of inherited thrombophilia in pregnancy. Curr. Opin. Endocrinol. Diabetes Obes. 2009, 16, 464–469. [Google Scholar] [CrossRef]
- Hellgren, M. Hemostasis during normal pregnancy and puerperium. Semin. Thromb. Hemost. 2003, 29, 125–130. [Google Scholar] [CrossRef]
- Dana, M.; Fibach, E. Fetal Hemoglobin in the Maternal Circulation—Contribution of Fetal Red Blood Cells. Hemoglobin 2018, 42, 138–140. [Google Scholar] [CrossRef]
- Bhave, A.A. Coagulopathies in Pregnancy: What an Obstetrician Ought to Know! J. Obstet. Gynaecol. India 2019, 69, 479–482. [Google Scholar] [CrossRef]
- Giannubilo, S.R.; Tranquilli, A.L. Fetal Thrombophilia. In Thrombophilia; IntechOpen: London, UK, 2011. [Google Scholar] [CrossRef]
- Lockwood, C.J. Pregnancy-associated changes in the hemostatic system. Clin. Obstet. Gynecol. 2006, 49, 836–843. [Google Scholar] [CrossRef]
- Daughety, M.M.; Samuelson Bannow, B.T. Hemostasis and Thrombosis in Pregnancy. In Hemostasis and Thrombosis; DeLoughery, T., Ed.; Springer: Cham, Switzerland, 2019. [Google Scholar] [CrossRef]
- Greer, I.A. Thrombosis in pregnancy: Maternal and fetal issues. Lancet 1999, 353, 1258–1265. [Google Scholar] [CrossRef]
- Siennicka, A.; Kłysz, M.; Chełstowski, K.; Tabaczniuk, A.; Marcinowska, Z.; Tarnowska, P.; Kulesza, J.; Torbe, A.; Jastrzębska, M. Reference Values of D-Dimers and Fibrinogen in the Course of Physiological Pregnancy: The Potential Impact of Selected Risk Factors-A Pilot Study. Biomed. Res. Int. 2020, 2020, 3192350. [Google Scholar] [CrossRef]
- Pinjala, R.K.; Reddy, L.R.; Nihar, R.P.; Praveen, G.V.; Sandeep, M. Thrombophilia—How far and how much to investigate? Indian J. Surg. 2012, 74, 157–162. [Google Scholar] [CrossRef][Green Version]
- Makris, M. Thrombophilia: Grading the risk. Blood 2009, 113, 5038–5039. [Google Scholar] [CrossRef]
- Găman, A.M.; Găman, G.D. Deficiency Of Antithrombin III (AT III)—Case Report and Review of the Literature. Curr. Health Sci. J. 2014, 40, 141–143. [Google Scholar] [CrossRef]
- Gupta, A.; Patibandla, S. Protein C Deficiency; StatPearls Publishing: Treasure Island, FL, USA, 2021. [Google Scholar]
- Gupta, A.; Tun, A.M.; Gupta, K.; Tuma, F. Protein S Deficiency; StatPearls Publishing: Treasure Island, FL, USA, 2021. [Google Scholar]
- Dahlbäck, B.; Hildebrand, B. Inherited resistance to activated protein C is corrected by anticoagulant cofactor activity found to be a property of factor V. Proc. Natl. Acad. Sci. USA 1994, 91, 1396–1400. [Google Scholar] [CrossRef]
- Ridker, P.M.; Miletich, J.P.; Hennekens, C.H.; Buring, J.E. Ethnic distribution of factor V Leiden in 4047 men and women. Implications for venous thromboembolism screening. JAMA 1997, 277, 1305–1307. [Google Scholar] [CrossRef]
- Momot, A.P.; Nikolaeva, M.G.; Yasafova, N.N.; Zainulina, M.S.; Momot, K.A.; Taranenko, I.A. Clinical and laboratory manifestations of the prothrombin gene mutation in women of reproductive age. J. Blood Med. 2019, 10, 255–263. [Google Scholar] [CrossRef]
- Mukhopadhyay, I.; Pruthviraj, V.; Rao, P.S.; Biswas, M. Hyperhomocysteinemia in recurrent pregnancy loss and the effect of folic acid and vitamin B12 on homocysteine levels: A prospective analysis. Int. J. Reprod. Contracept. Obstet. Gynecol. 2017, 6, 2258–2261. [Google Scholar] [CrossRef][Green Version]
- Pascual, Z.N.; Langaker, M.D. Physiology, Pregnancy; StatPearls Publishing: Treasure Island, FL, USA, 2021. [Google Scholar]
- Younis, J.S.; Samueloff, A. Gestational vascular complications. Best Pract. Res. Clin. Haematol. 2003, 16, 135–151. [Google Scholar] [CrossRef]
- Szecsi, P.B.; Jørgensen, M.; Klajnbard, A.; Andersen, M.R.; Colov, N.P.; Stender, S. Haemostatic reference intervals in pregnancy. Thromb. Haemost. 2010, 103, 718–727. [Google Scholar] [CrossRef]
- Dobbenga-Rhodes, Y. Shedding Light on Inherited Thrombophilias: The Impact on Pregnancy. J. Perinat. Neonatal Nurs. 2016, 30, 36–44. [Google Scholar] [CrossRef]
- O’Riordan, M.N.; Higgins, J.R. Haemostasis in normal and abnormal pregnancy. Best Pract. Res. Clin. Obstet. Gynaecol. 2003, 17, 385–396. [Google Scholar] [CrossRef]
- Aracic, N.; Roje, D.; Jakus, I.A.; Bakotin, M.; Stefanovic, V. The Impact of Inherited Thrombophilia Types and Low Molecular Weight Heparin Treatment on Pregnancy Complications in Women with Previous Adverse Outcome. Yonsei Med. J. 2016, 57, 1230–1235. [Google Scholar] [CrossRef]
- Lockwood, C.J. Inherited thrombophilias in pregnant patients: Detection and treatment paradigm. Obstet. Gynecol. 2002, 99, 333–341. [Google Scholar] [CrossRef]
- Dossenbach-Glaninger, A.; van Trotsenburg, M.; Oberkanins, C.; Atamaniuk, J. Risk for early pregnancy loss by factor XIII Val34Leu: The impact of fibrinogen concentration. J. Clin. Lab. Anal. 2013, 27, 444–449. [Google Scholar] [CrossRef]
- Ashraf, N.; Visweshwar, N.; Jaglal, M.; Sokol, L.; Laber, D. Evolving paradigm in thrombophilia screening. Blood Coagul. Fibrinolysis Int. J. Haemost. Thromb. 2019, 30, 249–252. [Google Scholar] [CrossRef] [PubMed]
- Lijfering, W.M.; Brouwer, J.L.; Veeger, N.J.; Bank, I.; Coppens, M.; Middeldorp, S.; Hamulyák, K.; Prins, M.H.; Büller, H.R.; van der Meer, J. Selective testing for thrombophilia in patients with first venous thrombosis: Results from a retrospective family cohort study on absolute thrombotic risk for currently known thrombophilic defects in 2479 relatives. Blood 2009, 113, 5314–5322. [Google Scholar] [CrossRef] [PubMed]
- Jennings, I.; Cooper, P. Screening for thrombophilia: A laboratory perspective. Br. J. Biomed. Sci. 2003, 60, 39–51. [Google Scholar] [CrossRef] [PubMed]
- MacCallum, P.; Bowles, L.; Keeling, D. Diagnosis and management of heritable thrombophilias. BMJ Clin. Res. Ed. 2014, 349, g4387. [Google Scholar] [CrossRef] [PubMed]
- Bezgin, T.; Kaymaz, C.; Akbal, Ö.; Yılmaz, F.; Tokgöz, H.C.; Özdemir, N. Thrombophilic Gene Mutations in Relation to Different Manifestations of Venous Thromboembolism: A Single Tertiary Center Study. Clin. Appl. Thromb. Hemost. Off. J. Int. Acad. Clin. Appl. Thromb. Hemost. 2018, 24, 100–106. [Google Scholar] [CrossRef] [PubMed]
- Riva, N.; Gatt, A. Update on the Diagnosis and Anticoagulant Treatment of the Antiphospholipid Syndrome. EMJ. 29 July 2019. Available online: https://www.emjreviews.com/rheumatology/article/update-on-the-diagnosis-and-anticoagulant-treatment-of-the-antiphospholipid-syndrome/ (accessed on 1 March 2022).
- Merriman, L.; Greaves, M. Testing for thrombophilia: An evidence-based approach. Postgrad. Med. J. 2006, 82, 699–704. [Google Scholar] [CrossRef]
- Bates, S.M.; Middeldorp, S.; Rodger, M.; James, A.H.; Greer, I. Guidance for the treatment and prevention of obstetric-associated venous thromboembolism. J. Thromb. Thrombolysis 2016, 41, 92–128. [Google Scholar] [CrossRef]
- Wu, O.; Robertson, L.; Twaddle, S.; Lowe, G.; Clark, P.; Walker, I.; Brenkel, I.; Greaves, M.; Langhorne, P.; Regan, L.; et al. Thrombosis: Risk and Economic Assessment of Thrombophilia Screening (TREATS) Study Screening for thrombophilia in high-risk situations: A meta-analysis and cost-effectiveness analysis. Br. J. Haematol. 2005, 131, 80–90. [Google Scholar] [CrossRef]
- Colucci, G.; Tsakiris, D.A. Thrombophilia screening revisited: An issue of personalized medicine. J. Thromb. Thrombolysis 2020, 49, 618–629. [Google Scholar] [CrossRef]
- Walker, I.D. Thrombophilia in pregnancy. J. Clin. Pathol. 2000, 53, 573–580. [Google Scholar] [CrossRef]
- Chan, W. Diagnosis of venous thromboembolism in pregnancy. Thromb. Res. 2017, 163, 221–228. [Google Scholar] [CrossRef]
- Bates, S.M. Management of pregnant women with thrombophilia or a history of venous thromboembolism. Hematol. Am. Soc. Hematol. Educ. Program 2007, 2007, 143–150. [Google Scholar] [CrossRef][Green Version]
- Marino, T. Anticoagulants and Thrombolytics in Pregnancy. Medscape. 30 June 2017. Available online: https://emedicine.medscape.com/article/164069 (accessed on 10 March 2022).
- Raju, N.; Bates, S.M. Preventing thrombophilia-related complications of pregnancy. Expert Rev. Hematol. 2009, 2, 183–196. [Google Scholar] [CrossRef]
- Bates, S.M.; Greer, I.A.; Middeldorp, S.; Veenstra, D.L.; Prabulos, A.M.; Vandvik, P.O. VTE, thrombophilia, antithrombotic therapy, and pregnancy: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest 2012, 141 (Suppl. S2), e691S–e736S. [Google Scholar] [CrossRef]
- Lagrange, F.; Vergnes, C.; Brun, J.L.; Paolucci, F.; Nadal, T.; Leng, J.J.; Saux, M.C.; Banwarth, B. Absence of placental transfer of pentasaccharide (Fondaparinux, Arixtra) in the dually perfused human cotyledon in vitro. Thromb. Haemost. 2002, 87, 831–835r. [Google Scholar]
- Many, A.; Koren, G. Low-molecular-weight heparins during pregnancy. Can. Fam. Physician Med. Fam. Can. 2005, 51, 199–201. [Google Scholar]
- Dimitrakakis, C.; Papageorgiou, P.; Papageorgiou, I.; Antzaklis, A.; Sakarelou, N.; Michalas, S. Absence of transplacental passage of the low molecular weight heparin enoxaparin. Haemostasis 2000, 30, 243–248. [Google Scholar] [CrossRef]
- Eichinger, S. D-dimer testing in pregnancy. Semin. Vasc. Med. 2005, 5, 375–378. [Google Scholar] [CrossRef]
- Bates, S.M. Preventing thrombophilia-related complications of pregnancy: An update. Expert Rev. Hematol. 2013, 6, 287–300. [Google Scholar] [CrossRef]
- Schreiber, K.; Sciascia, S.; de Groot, P.G.; Devreese, K.; Jacobsen, S.; Ruiz-Irastorza, G.; Salmon, J.E.; Shoenfeld, Y.; Shovman, O.; Hunt, B.J. Antiphospholipid syndrome. Nat. Rev. Dis. Primers 2018, 4, 17103. [Google Scholar] [CrossRef]
- Kozer, E.; Nikfar, S.; Costei, A.; Boskovic, R.; Nulman, I.; Koren, G. Aspirin consumption during the first trimester of pregnancy and congenital anomalies: A meta-analysis. Am. J. Obstet. Gynecol. 2002, 187, 1623–1630. [Google Scholar] [CrossRef]
- De Vries, J.I.; van Pampus, M.G.; Hague, W.M.; Bezemer, P.D.; Joosten, J.H. FRUIT Investigators Low-molecular-weight heparin added to aspirin in the prevention of recurrent early-onset pre-eclampsia in women with inheritable thrombophilia: The FRUIT-RCT. J. Thromb. Haemost. JTH 2012, 10, 64–72. [Google Scholar] [CrossRef]
- Ageno, W.; Crotti, S.; Turpie, A.G. The safety of antithrombotic therapy during pregnancy. Expert Opin. Drug Saf. 2004, 3, 113–118. [Google Scholar] [CrossRef] [PubMed]
- Papadakis, E.; Pouliakis, A.; Aktypi, A.; Christoforidou, A.; Kotsi, P.; Anagnostou, G.; Foifa, A.; Grouzi, E. Low molecular weight heparins use in pregnancy: A practice survey from Greece and a review of the literature. Thromb. J. 2019, 17, 23. [Google Scholar] [CrossRef] [PubMed]
- Morelli, V.M.; Brækkan, S.K.; Hansen, J.B. Role of microRNAs in Venous Thromboembolism. Int. J. Mol. Sci. 2020, 21, 2602. [Google Scholar] [CrossRef] [PubMed]
- Mayor-Lynn, K.; Toloubeydokhti, T.; Cruz, A.C.; Chegini, N. Expression profile of microRNAs and mRNAs in human placentas from pregnancies complicated by preeclampsia and preterm labor. Reprod. Sci. 2011, 18, 46–56. [Google Scholar] [CrossRef]
- Fu, G.; Brkić, J.; Hayder, H.; Peng, C. MicroRNAs in Human Placental Development and Pregnancy Complications. Int. J. Mol. Sci. 2013, 14, 5519–5544. [Google Scholar] [CrossRef]
- Lee, D.C.; Romero, R.; Kim, J.S.; Tarca, A.L.; Montenegro, D.; Pineles, B.L.; Kim, E.; Lee, J.; Kim, S.Y.; Draghici, S.; et al. miR-210 targets iron-sulfur cluster scaffold homologue in human trophoblast cell lines: Siderosis of interstitial trophoblasts as a novel pathology of preterm preeclampsia and small-for-gestational-age pregnancies. Am. J. Pathol. 2011, 179, 590–602. [Google Scholar] [CrossRef]
- Riley, R.D.; Hayden, J.A.; Steyerberg, E.W.; Moons, K.G.; Abrams, K.; Kyzas, P.A.; Malats, N.; Briggs, A.; Schroter, S.; Altman, D.G.; et al. PROGRESS Group Prognosis Research Strategy (PROGRESS) 2: Prognostic factor research. PLoS Med. 2013, 10, e1001380. [Google Scholar] [CrossRef]
- Rodriguez-Rius, A.; Lopez, S.; Martinez-Perez, A.; Souto, J.C.; Soria, J.M. Identification of a Plasma MicroRNA Profile Associated With Venous Thrombosis. Arterioscler. Thromb. Vasc. Biol. 2020, 40, 1392–1399. [Google Scholar] [CrossRef]
- Lee, Y.; Ahn, E.H.; Ryu, C.S.; Kim, J.O.; An, H.J.; Cho, S.H.; Kim, J.H.; Kim, Y.R.; Lee, W.S.; Kim, N.K. Association between microRNA machinery gene polymorphisms and recurrent implantation failure. Exp. Ther. Med. 2020, 19, 3113–3123. [Google Scholar] [CrossRef]
- Barchitta, M.; Maugeri, A.; Quattrocchi, A.; Agrifoglio, O.; Agodi, A. The Role of miRNAs as Biomarkers for Pregnancy Outcomes: A Comprehensive Review. Int. J. Genom. 2017, 2017, 8067972. [Google Scholar] [CrossRef]
| Prevention of Pregnancy-Related Complications | Recommendations |
|---|---|
| No previous VTE HIGH RISK: homozygosity for the mutation of factor V Leiden or the presence of prothrombin gene mutation | |
|
|
|
|
| |
| LOW RISK: other forms of thrombophilias | |
|
|
|
|
| Previous VTE MODERATE AND HIGH RISK: |
|
| One or multiple episodes of VTE: |
|
| LOW RISK: One episode of VTE, linked with a temporary risk factor, that is not pregnancy-related: |
|
| Administrated Agents— Should Be Interrupted 12–24 h Prior to Elective Induction of Delivery | Recommendations If Unplanned Delivery Happens, Neuroaxial Anaesthesia Should Not Be Performed |
|---|---|
| UFH |
|
| LMWH information taken from [49] |
|
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Samfireag, M.; Potre, C.; Potre, O.; Tudor, R.; Hoinoiu, T.; Anghel, A. Approach to Thrombophilia in Pregnancy—A Narrative Review. Medicina 2022, 58, 692. https://doi.org/10.3390/medicina58050692
Samfireag M, Potre C, Potre O, Tudor R, Hoinoiu T, Anghel A. Approach to Thrombophilia in Pregnancy—A Narrative Review. Medicina. 2022; 58(5):692. https://doi.org/10.3390/medicina58050692
Chicago/Turabian StyleSamfireag, Miruna, Cristina Potre, Ovidiu Potre, Raluca Tudor, Teodora Hoinoiu, and Andrei Anghel. 2022. "Approach to Thrombophilia in Pregnancy—A Narrative Review" Medicina 58, no. 5: 692. https://doi.org/10.3390/medicina58050692
APA StyleSamfireag, M., Potre, C., Potre, O., Tudor, R., Hoinoiu, T., & Anghel, A. (2022). Approach to Thrombophilia in Pregnancy—A Narrative Review. Medicina, 58(5), 692. https://doi.org/10.3390/medicina58050692






