Comparative Analysis of the Most Important Cardiovascular Risk Factors Based on Cross-Sectional Studies in the Population of Latvia
Abstract
:1. Introduction
2. Materials and Methods
2.1. Design
2.2. Data Collection
2.3. Risk Factors
- high BP; defined as systolic BP of 140 mmHg or more, and/or diastolic BP of 90 mmHg or more; the subjects were classified as having hypertension if their systolic BP was over 140 mmHg, and/or the diastolic BP over 90 mmHg, and/or if they were on pharmacological treatment for hypertension, including those whose hypertension was controlled (i.e., lower than 140/90 mm Hg);
- overweight and obesity; BMI cut-off points of 25 and 30 kg/m2 were used to determine the overweight and obese subjects, respectively;
- smoking; according to the smoking status, participants were classified into three main categories: daily smokers, ex-smokers, and never-smokers. Daily smokers were defined as smokers who continue smoking now; ex-smokers—smokers who have quitted smoking at least 6 months before examination;
- dyslipidaemias; the cut-off points of dyslipidaemias were as follows: TC ≥5.0 mmol/L, LDL-C ≥ 3.0 mmol/L, HDL-C ≤ 1.0 mmol/L for men, and ≤1.2 mmol/L for women, Tg ≥ 1.7 mmol/L, Glu ≥ 5.6 mmol/L.
2.4. Statistical Analysis
3. Results
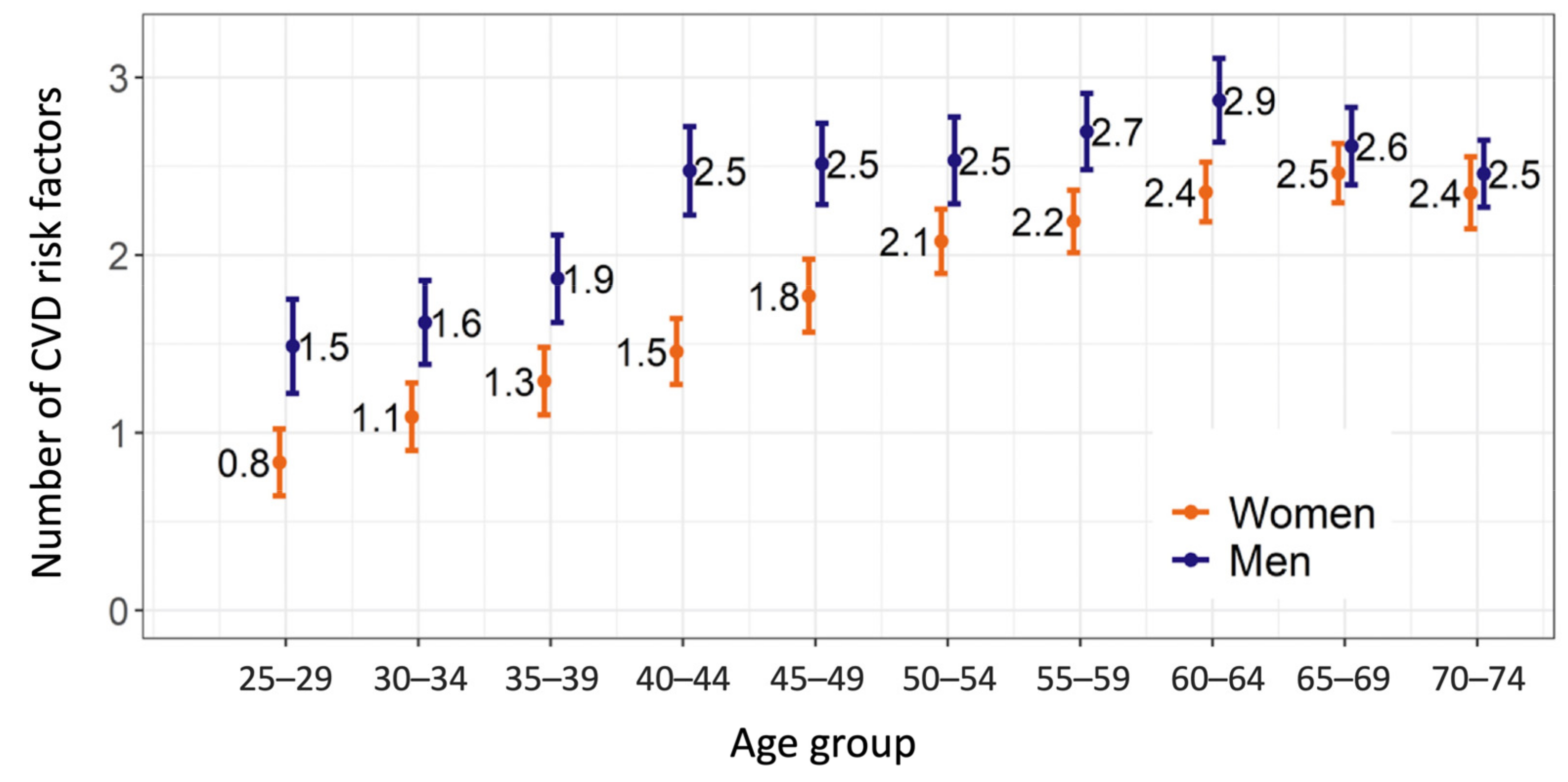
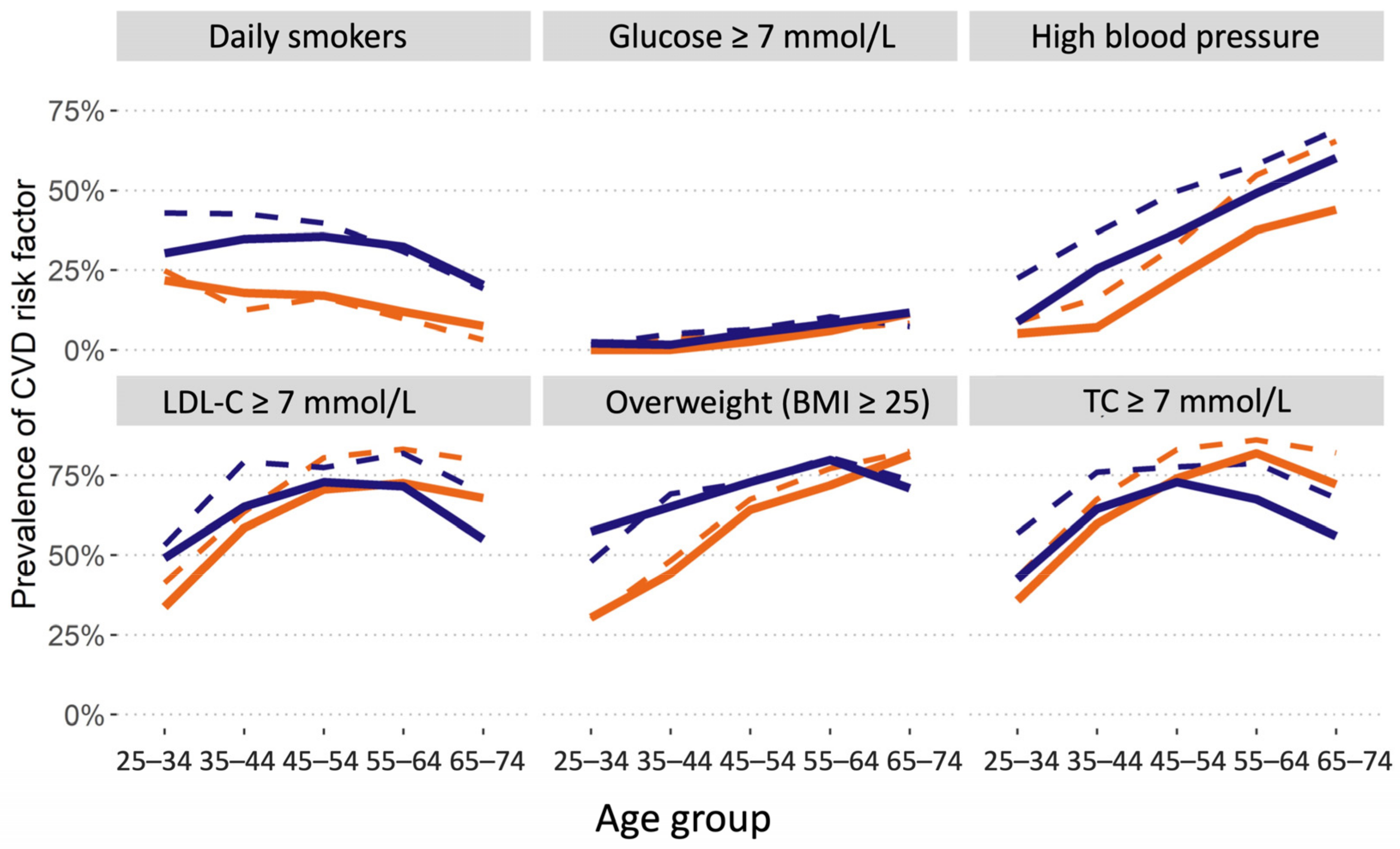
3.1. Cardiovascular Disease Risk Factors
3.2. High Blood Pressure and Hypertension
3.3. Body Mass Index
3.4. Smoking
3.5. Lipids
3.6. Glucose
3.7. Changes in the Cardiovascular Risk Profile over the Past Decade
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Centre for Disease Prevention and Control of Latvia. Health Statistics Database 2021. Available online: https://statistika.spkc.gov.lv/pxweb/lv/Health/ (accessed on 3 April 2022).
- Ērglis, A.; Dzērve, V.; Pahomova-Strautiņa, J.; Narbute, I.; Jēgere, S.; Mintāle, I.; Ligere, R.; Apinis, P.; Lejnieks, A.; Misiņa, D.; et al. A population-based cross-sectional study of cardiovascular risk factor in Latvia. Medicina 2012, 48, 310–316. [Google Scholar] [CrossRef] [PubMed]
- Piepoli, M.F.; Hoes, A.W.; Agewall, S.; Albus, C.; Brotons, C.; Catapano, A.L.; Cooney, M.T.; Corràm, U.; Cosynsm, B.; Verschuren, W.M.; et al. 2016 European Guidelines on cardiovascular disease prevention in clinical practice: The Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of 10 societies and by invited experts)Developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR). Eur. Heart J. 2016, 37, 2315–2381. [Google Scholar] [PubMed]
- Cosentino, F.; Grant, P.J.; Aboyans, V.; Bailey, C.J.; Ceriello, A.; Delgado, V.; Federici, M.; Filippatos, G.; Grobbee, D.E.; Hansen, T.B.; et al. 2019 ESC Guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD. Eur. Heart J. 2020, 41, 255–323. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mach, F.; Baigent, C.; Catapano, A.L.; Koskinas, K.C.; Casula, M.; Badimon, L.; Chapman, M.J.; de Backer, G.G.; Delgado, V.; Ference, B.A.; et al. 2019 ESC/EAS Guidelines for the management of dyslipidaemias: Lipid modification to reduce cardiovascular risk. Eur. Heart J. 2020, 41, 111–188. [Google Scholar] [CrossRef] [PubMed]
- Prättälä, R.; Helasoja, V.; Laaksonen, M.; Laatikainen, T.; Nikander, P.; Puska, P. (Eds.) Cindi Health Monitor: Proposal for Practical Guidelines 2001; WHO Regional Office for Europe and National Public Health Institute: Helsinki, Finland, 2001. [Google Scholar]
- Hospital Anxiety and Depression Scale (HADS). Available online: https://www.svri.org/sites/default/files/attachments/2016-01-13/HADS.pdf (accessed on 3 April 2022).
- Belghazi, J.; El Feghali, R.N.; Moussalem, T.; Rejdych, M.; Asmar, R.G. Validation of four automatic devices for self-measurement of blood pressure according to the International Protocol of the European Society of Hypertension. Vasc. Health Risk Manag. 2007, 3, 389–400. [Google Scholar] [PubMed]
- E.Gulbja Laboratorija Ltd. Available online: https://www.egl.lv/en/about-us/service-centers (accessed on 3 April 2022).
- The R Project for Statistical Computing. Available online: https://www.r-project.org (accessed on 3 April 2022).
- Lumley, T. Survey: Analysis of Complex Survey Samples. R Package version 4.0.2020. Available online: https://cran.r-project.org/web/packages/survey/survey.pdf (accessed on 23 March 2021).
- Forouzanfar, M.H.; Alexander, L.; Anderson, H.R.; Bachman, V.F.; Biryukov, S.; Brauer, M.; Burnett, R.; Casey, D.; Coates, M.M.; Cohen, A.; et al. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks in 188 countries, 1990–2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet 2015, 386, 2287–2323. [Google Scholar] [CrossRef] [Green Version]
- Centre for Disease Prevention and Control of Latvia. Health Behaviour among Latvian Adult Population 2019. Available online: https://www.spkc.gov.lv/lv/veselibu-ietekmejoso-paradumu-petijumi (accessed on 30 January 2021).
- Kotseva, K.; Wood, D.; De Bacquer, D.; De Backer, G.; Rydén, L.; Jennings, C.; Gyberg, V.; Amouyel, P.; Bruthans, J.; Castro Conde, A.; et al. EUROASPIRE IV: A European Society of Cardiology survey on the lifestyle, risk factor and therapeutic management of coronary patients from 24 European countries. Eur. J. Prev. Cardiol. 2016, 23, 636–648. [Google Scholar] [CrossRef] [PubMed]
- NCD Risk Factor Collaboration. Long-term and recent trends in hypertension awareness, treatment, and control in 12 high-income countries: An analysis of 123 nationally representative surveys. Lancet 2019, 394, 639–651. [Google Scholar] [CrossRef] [Green Version]
| Parameter | Men, n (%) | Women, n (%) | Total, n (%) |
|---|---|---|---|
| Age group | |||
| 25–29 | 190 (9.4%) | 197 (9.6%) | 387 (9.5%) |
| 30–34 | 195 (9.7%) | 220 (10.7%) | 415 (10.2%) |
| 35–39 | 206 (10.2%) | 197 (9.6%) | 403 (9.9%) |
| 40–44 | 193 (9.6%) | 201 (9.8%) | 394 (9.7%) |
| 45–49 | 197 (9.8%) | 204 (9.9%) | 401 (9.9%) |
| 50–54 | 192 (9.5%) | 201 (9.8%) | 393 (9.7%) |
| 55–59 | 214 (10.6%) | 210 (10.2%) | 424 (10.4%) |
| 60–64 | 214 (10.6%) | 210 (10.2%) | 424 (10.4%) |
| 65–69 | 212 (10.5%) | 199 (9.7%) | 411 (10.1%) |
| 70–74 | 203 (10.1%) | 215 (10.5%) | 418 (10.3%) |
| Total | 2016 | 2054 | 4070 |
| Parameter | Men, n = 2016 | Women, n = 2054 | Total, n = 4070 |
|---|---|---|---|
| Age group | |||
| Education, n (%) | |||
| Higher (1st/2nd level) | 495 (24.6%) | 818 (39.8%) | 1313 (32.3%) |
| Primary | 271 (13.4%) | 202 (9.8%) | 473 (11.6%) |
| Secondary | 945 (46.9%) | 715 (34.8%) | 1660 (40.8%) |
| Secondary professional | 305 (15.1%) | 319 (15.5%) | 624 (15.3%) |
| Marital status, n (%) | |||
| Divorced | 221 (11.0%) | 264 (12.9%) | 485 (11.9%) |
| Married | 1349 (66.9%) | 1243 (60.5%) | 2592 (63.7%) |
| Never- married | 399 (19.8%) | 321 (15.6%) | 720 (17.7%) |
| Widowers/widows | 47 (2.3%) | 226 (11.0%) | 273 (6.7%) |
| Occupation status, n (%) | |||
| Housewife/Househusband | 26 (1.3%) | 173 (8.4%) | 199 (4.9%) |
| Jobless | 129 (6.4%) | 94 (4.6%) | 223 (5.5%) |
| Laborers | 934 (46.3%) | 522 (25.4%) | 1456 (35.8%) |
| Retired | 430 (21.3%) | 439 (21.4%) | 869 (21.4%) |
| Students | 4 (0.2%) | 10 (0.5%) | 14 (0.3%) |
| White-collar workers | 493 (24.5%) | 816 (39.7%) | 1309 (32.2%) |
| Parameter | Male, n = 2016 | Female, n = 2054 | Total, n = 4070 | p-Value, Men vs. Women |
|---|---|---|---|---|
| Risk factors, n (%) | ||||
| Hypertension | 15.9 (14.4, 17.6) | 20.9 (19.2, 22.8) | 18.6 (17.4, 19.9) | <0.001 |
| High cholesterol | 15.4 (13.8, 17.1) | 22.7 (20.8, 24.7) | 19.3 (18.0, 20.6) | <0.001 |
| Diabetes | 4.5 (3.6, 5.4) | 6.1 (5.1, 7.3) | 5.3 (4.6, 6.1) | 0.023 |
| Current smoking | 40.4 (38.1, 42.7) | 21.0 (19.2, 22.9) | 30.0 (28.5, 31.5) | <0.001 |
| Physical inactivity | 8.6 (7.4, 9.9) | 12.0 (10.7, 13.5) | 10.4 (9.5, 11.4) | <0.001 |
| Medical treatment, n (%) | ||||
| Anti-hypertensive agents | 15.5 (14.0, 17.2) | 20.5 (18.7, 22.3) | 18.2 (17.0, 19.4) | <0.001 |
| Anti-cholesterol agents | 8.0 (6.9, 9.2) | 12.5 (11.1, 14.1) | 10.4 (9.5, 11.4) | <0.001 |
| Parameters | All Population n = 2218 | Men n = 976 | Women n = 1242 | Men vs. Women | |||
|---|---|---|---|---|---|---|---|
| Risk factor | % | [95% CI] | % | [95% CI] | % | [95% CI] | p |
| TC, ≥5 mmol/L | 63.2 | [61.0, 65.3] | 60.7 | [57.3, 64.0] | 65.4 | [62.5, 68.1] | 0.036 |
| LDL-C, <2 mmol/L | 7.9 | [6.8, 9.2] | 7.8 | [6.2, 9.8] | 8.0 | [6.5, 9.8] | 0.870 |
| LDL-C, 2–2.99 mmol/L | 30.1 | [28.0, 32.2] | 29.1 | [26.1, 32.3] | 30.9 | [28.2, 33.7] | 0.406 |
| LDL-C, ≥3 mmol/L | 62.0 | [59.8, 64.2] | 63.1 | [59.7, 66.3] | 61.1 | [58.2, 63.9] | 0.379 |
| HDL-C, ≤ 1 (1.2) mmol/L for men (women) | 14.0 | [12.5, 15.6] | 16.9 | [14.5, 19.5] | 11.5 | [9.8, 13.5] | 0.001 |
| Tg, ≥1.7 mmol/L | 24.7 | [22.9, 26.7] | 29.4 | [26.4, 32.5] | 20.7 | [18.5, 23.2] | <0.001 |
| Glu, 5.6–6.99 mmol/L | 22.1 | [20.4, 24] | 27.1 | [24.2, 30.1] | 17.8 | [15.7, 20.1] | <0.001 |
| Glu, ≥7 mmol/L | 4.5 | [3.7, 5.5] | 5.2 | [3.9, 6.7] | 4.0 | [3.0, 5.2] | 0.168 |
| High blood pressure (≥140 and/or 90) | 28.0 | [26.1, 30.0] | 33.3 | [30.2, 36.4] | 23.5 | [21.1, 26.0] | <0.001 |
| Arterial hypertension | 36.8 | [34.7, 38.9] | 40.3 | [37.0, 43.6] | 33.8 | [31.2, 36.6] | 0.003 |
| Overweight (BMI 25–29.9) | 34.3 | [32.2, 36.4] | 40.6 | [37.3, 44.0] | 28.8 | [26.3, 31.5] | <0.001 |
| Obesity (BMI ≥ 30) | 29.1 | [27.1, 31.1] | 28.2 | [25.3, 31.3] | 29.8 | [27.3, 32.5] | 0.427 |
| Have smoked at least for 1 year during lifetime | 45.3 | [43.1, 47.5] | 60.8 | [57.5, 64.1] | 31.7 | [29.1, 34.5] | <0.001 |
| Daily smokers | 22.8 | [21.0, 24.7] | 31.5 | [28.5, 34.8] | 15.2 | [13.2, 17.4] | <0.001 |
| Age Groups | 25–34 | 35–44 | 45–54 | 55–64 | 65–74 | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Sex | M | W | M | W | M | W | M | W | M | W |
| TC, ≥5 mmol/L | 42.5 | 35.7 | 64.5 | 59.8 | 72.9 | 74.0 | 67.5 | 81.9 *** | 56.0 | 72.2 *** |
| LDL-C, <2 mmol/L | 10.9 | 14.8 | 3.2 | 5.9 | 6.5 | 3.8 | 6.9 | 5.5 | 13.8 | 10.8 |
| LDL-C, 2–2.99 mmol/L | 40.0 | 51.4 * | 31.7 | 35.6 | 20.7 | 25.6 | 21.6 | 21.9 | 31.3 | 21.4 * |
| LDL-C, ≥3 mmol/L | 49.0 | 33.7 ** | 65.1 | 58.5 | 72.8 | 70.6 | 71.5 | 72.6 | 54.9 | 67.8 ** |
| HDL-C, ≤1 (1.2) mmol/L for men (women) | 14.6 | 8.6 | 13.1 | 12.2 | 18.7 | 7.2 *** | 20.8 | 16.0 | 17.8 | 13.3 |
| Tg, ≥1.7 mmol/L | 21.2 | 6.9 *** | 26.4 | 11.6 *** | 39.2 | 18.5 *** | 35.9 | 32.0 | 22.2 | 33.4 ** |
| Glu, 5.6–6.99 mmol/L | 11.3 | 5.8 | 24.6 | 9.8 *** | 31.2 | 16.2 *** | 36.7 | 27.0 * | 37.2 | 29.1 |
| Glu, ≥7 mmol/L | 2.1 | 0.0 | 1.6 | 0.0 | 5.2 | 2.6 | 8.2 | 6.0 | 11.7 | 11.3 |
| High blood pressure (≥140 and/or 90) | 8.8 | 5.1 | 25.4 | 7.0 *** | 36.5 | 22.6 ** | 49.1 | 37.5 * | 60.2 | 44.0 ** |
| Arterial hypertension | 10.0 | 5.1 | 28.0 | 9.4 *** | 43.5 | 32.8 * | 64.4 | 52.9 * | 71.7 | 67.4 |
| Overweight (BMI 25–29.9) | 39.9 | 16.2 *** | 40.7 | 28.0 | 39.6 | 32.8 | 42.2 | 30.1 ** | 40.7 | 37.0 |
| Obesity (BMI ≥ 30) | 17.5 | 14.2 | 24.4 | 16.3 * | 33.2 | 31.3 | 37.6 | 41.7 | 30.2 | 44.3 ** |
| Have smoked at least for 1 year during lifetime | 52.7 | 40.0 * | 59.5 | 36.2 *** | 65.2 | 32.8 *** | 67.7 | 27.3 *** | 59.3 | 22.7 *** |
| Daily smokers | 30.3 | 21.8 | 34.8 | 17.9 *** | 35.5 | 17.0 *** | 32.4 | 11.9 *** | 20.3 | 7.4 *** |
| 2009–2010 | 2019–2020 | 2009–2010 vs. 2019–2020 | |||||
|---|---|---|---|---|---|---|---|
| Mean | 95% CI | Mean | 95% CI | t | df | p | |
| All | 2.3 | [2.3, 2.4] | 2.0 | [2.0, 2.1] | −7.2 | 5883 | <0.001 |
| Men | 2.6 | [2.5, 2.7] | 2.3 | [2.2, 2.4] | −4.5 | 2298 | <0.001 |
| Women | 2.1 | [2.0, 2.1] | 1.8 | [1.7, 19] | −6.1 | 3583 | <0.001 |
| Age Group | 2009–2010 | 2019–2020 | ||
|---|---|---|---|---|
| Men | Women | Men | Women | |
| 25–34 | 15.1% | 28.1% | 16.2% | 35.7% |
| 35–44 | 3.0% | 15.4% | 4.8% | 20.7% |
| 45–54 | 1.1% | 4.7% | 3.0% | 10.4% |
| 55–64 | 1.4% | 2.4% | 1.4% | 3.1% |
| 65–74 | 1.5% | 0.8% | 2.6% | 2.9% |
| Total | 5.0% | 10.2% | 6.1% | 14.3% |
| All Population | Men | Women | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Risk Factor | % | [95% CI] | Δ10y | % | [95% CI] | Δ10y | % | [95% CI] | Δ10y |
| TC, ≥5 mmol/L | 71.8 | [70.0, 73.7] | −8.6 *** | 71.1 | [67.9, 74.2] | −10.4 *** | 72.4 | [70.2, 74.5] | −7.0 *** |
| LDL-C, <2 mmol/L | 4.6 | [3.9, 5.6] | +3.3 *** | 4.1 | [3.0, 5.6] | +3.7 ** | 5.1 | [4.0, 6.4] | +2.9 ** |
| LDL-C, 2–2.99 mmol/L | 24.8 | [23.0, 26.6] | +5.3 *** | 24.2 | [21.2, 27.4] | +4.9 * | 25.3 | [23.3, 27.4] | +5.6 ** |
| LDL-C, ≥3 mmol/L | 70.6 | [68.6, 72.4] | −8.6 *** | 71.7 | [68.4, 74.8] | −8.6 *** | 69.6 | [67.4, 71.8] | −8.5 *** |
| HDL-C, ≤ 1 (1.2) mmol/L for men (women) | 17.0 | [15.5, 18.6] | −3.0 ** | 19.6 | [17.0, 22.4] | −2.7 | 14.9 | [13.3, 16.5] | −3.4 ** |
| Tg, ≥1.7 mmol/L | 26.9 | [25.2, 28.7] | −2.2 | 34.0 | [30.9, 37.2] | −4.6 * | 21.0 | [19.2, 22.8] | −0.3 |
| Glu, 5.6–6.99 mmol/L | 26.8 | [25.2, 28.5] | −4.7 *** | 30.8 | [27.9, 33.8] | −3.7 | 23.4 | [21.6, 25.3] | −5.6 *** |
| Glu, ≥7 mmol/L | 5.0 | [4.2, 5.8] | −0.5 | 5.7 | [4.4, 7.4] | −0.5 | 4.3 | [3.6, 5.2] | −0.3 |
| High blood pressure (≥140 and/or 90) | 39.3 | [37.4, 41.2] | −11.3 *** | 44.1 | [40.8, 47.4] | −10.8 *** | 35.2 | [33.2, 37.4] | −11.7 *** |
| Arterial hypertension | 45.5 | [43.5, 47.4] | −8.7 *** | 49.8 | [46.3, 53.2] | −9.5 *** | 41.9 | [39.7, 44.1] | −8.1 *** |
| Overweight (BMI 25–29.9) | 37.1 | [35.2, 39.1] | −2.8 | 43.8 | [40.5, 47.1] | −3.2 | 31.5 | [29.5, 33.6] | −2.7 |
| Obesity (BMI ≥ 30) | 26.9 | [25.2, 28.5] | +2.2 | 23.6 | [21.0, 26.4] | +4.6 * | 29.6 | [27.6, 31.6] | +0.2 |
| Have smoked at least for 1 year during lifetime | 39.2 | [37.2, 41.2] | +6.1 *** | 58.5 | [55.1, 61.7] | +2.3 | 23.0 | [21.0, 25.0] | +8.7 *** |
| Daily smokers | 24.2 | [22.4, 26.1] | −1.4 | 37.0 | [33.7, 40.3] | −5.5 * | 13.4 | [11.8, 15.2] | 1.8 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Erglis, A.; Bajare, I.; Jegere, S.; Mintale, I.; Barzdins, J.; Luguzis, A.; Apinis, P.; Caksa, A.; Gavare, I.; Dzerve, V. Comparative Analysis of the Most Important Cardiovascular Risk Factors Based on Cross-Sectional Studies in the Population of Latvia. Medicina 2022, 58, 643. https://doi.org/10.3390/medicina58050643
Erglis A, Bajare I, Jegere S, Mintale I, Barzdins J, Luguzis A, Apinis P, Caksa A, Gavare I, Dzerve V. Comparative Analysis of the Most Important Cardiovascular Risk Factors Based on Cross-Sectional Studies in the Population of Latvia. Medicina. 2022; 58(5):643. https://doi.org/10.3390/medicina58050643
Chicago/Turabian StyleErglis, Andrejs, Iveta Bajare, Sanda Jegere, Iveta Mintale, Juris Barzdins, Artis Luguzis, Peteris Apinis, Anda Caksa, Iveta Gavare, and Vilnis Dzerve. 2022. "Comparative Analysis of the Most Important Cardiovascular Risk Factors Based on Cross-Sectional Studies in the Population of Latvia" Medicina 58, no. 5: 643. https://doi.org/10.3390/medicina58050643
APA StyleErglis, A., Bajare, I., Jegere, S., Mintale, I., Barzdins, J., Luguzis, A., Apinis, P., Caksa, A., Gavare, I., & Dzerve, V. (2022). Comparative Analysis of the Most Important Cardiovascular Risk Factors Based on Cross-Sectional Studies in the Population of Latvia. Medicina, 58(5), 643. https://doi.org/10.3390/medicina58050643







