A Modified Approach for Minimally Invasive Tubular Microdiscectomy for Far Lateral Disc Herniations: Docking at the Caudal Level Transverse Process
Abstract
:1. Introduction
2. Materials and Methods
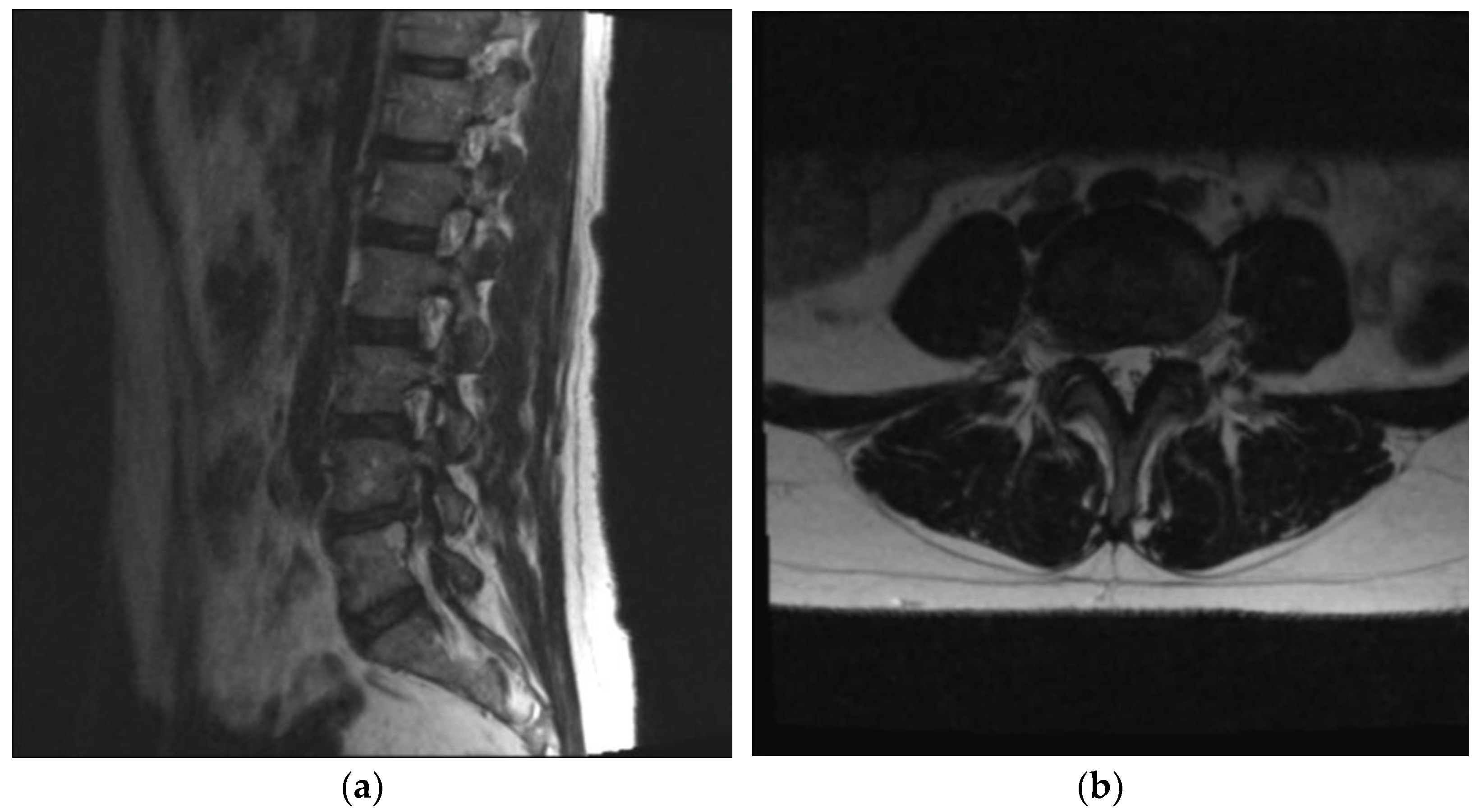
2.1. Clinical Evaluation
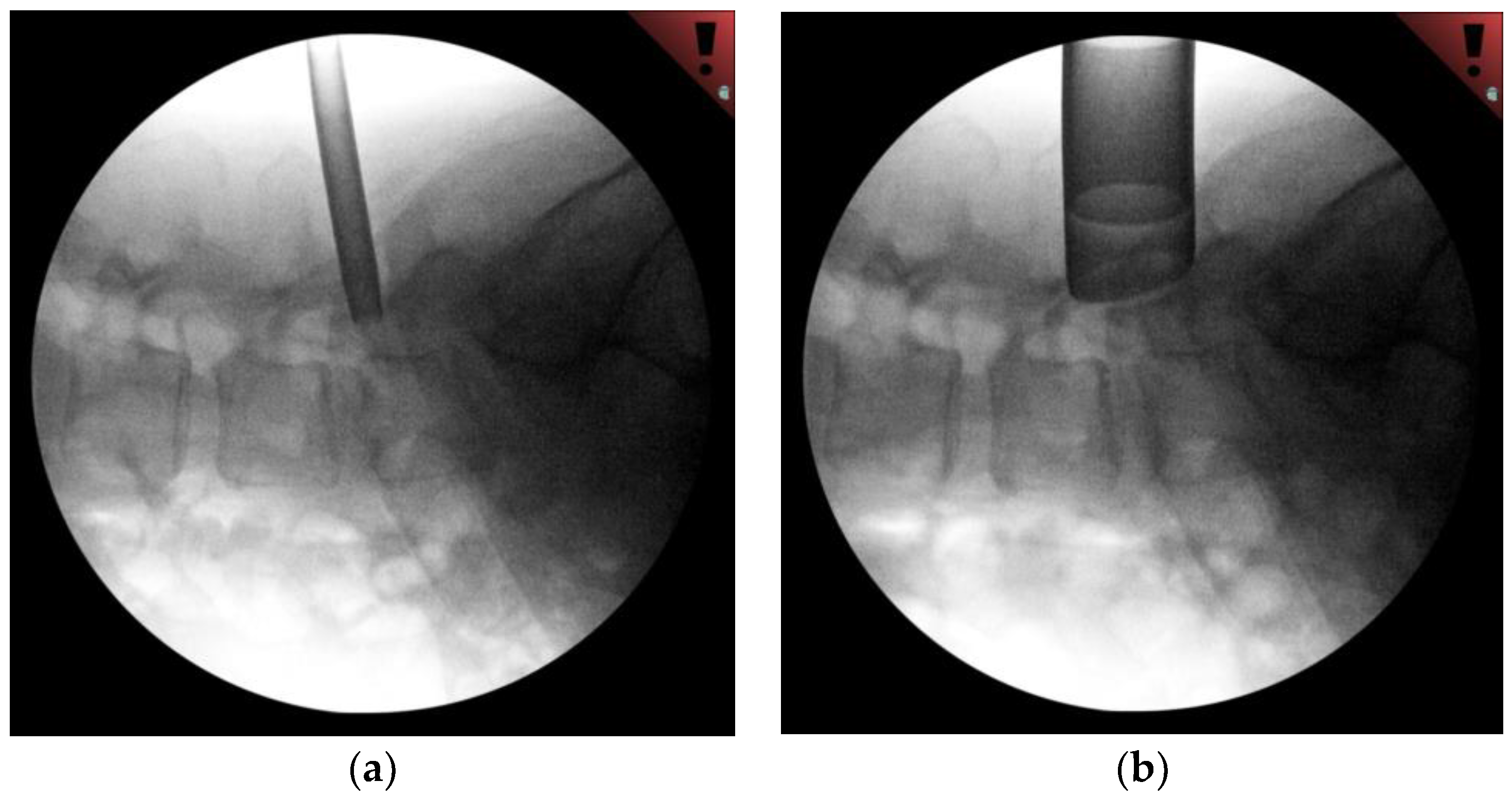
2.2. Technical Description
2.3. Comprehensive Literature Review
3. Results
3.1. Clinical Outcome
3.2. Comprehensive Literature Review Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Epstein, N.E. Foraminal and far lateral lumbar disc herniations: Surgical alternatives and outcome measures. Spinal Cord 2002, 40, 491–500. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Akinduro, O.O.; Kerezoudis, P.; Alvi, M.A.; Yoon, J.W.; Eluchie, J.; Murad, M.H.; Wang, Z.; Chen, S.G.; Bydon, M. Open Versus Minimally Invasive Surgery for Extraforaminal Lumbar Disk Herniation: A Systematic Review and Meta-Analysis. World Neurosurg. 2017, 108, 924–938.e3. [Google Scholar] [CrossRef] [PubMed]
- O’Toole, J.E.; Eichholz, K.M.; Fessler, R.G. Surgical site infection rates after minimally invasive spinal surgery: Clinical article. J. Neurosurg. Spine 2009, 11, 471–476. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lofrese, G.; Mongardi, L.; Cultrera, F.; Trapella, G.; De Bonis, P. Surgical treatment of intraforaminal/extraforaminal lumbar disc herniations: Many approaches for few surgical routes. Acta Neurochir. 2017, 159, 1273–1281. [Google Scholar] [CrossRef] [PubMed]
- Berra, L.V.; Di Rita, A.; Longhitano, F.; Mailland, E.; Reganati, P.; Frati, A.; Santoro, A. Far lateral lumbar disc herniation part 1: Imaging, neurophysiology and clinical features. World J. Orthop. 2021, 12, 961–969. [Google Scholar] [CrossRef] [PubMed]
- Khan, J.M.; McKinney, D.; Basques, B.A.; Louie, P.K.; Carroll, D.; Paul, J.; Varthi, A.; Iyer, S.; An, H.S. Clinical Presentation and Outcomes of Patients With a Lumbar Far Lateral Herniated Nucleus Pulposus as Compared to Those with a Central or Paracentral Herniation. Glob. Spine J. 2019, 9, 480–486. [Google Scholar] [CrossRef]
- Voyadzis, J.M.; Gala, V.C.; Sandhu, F.A.; Fessler, R.G. Minimally invasive approach for far lateral disc herniations: Results from 20 patients. Minim. Invasive Neurosurg. 2010, 53, 122–126. [Google Scholar] [CrossRef]
- Park, H.W.; Park, K.S.; Park, M.S.; Kim, S.M.; Chung, S.Y.; Lee, D.S. The Comparisons of Surgical Outcomes and Clinical Characteristics between the Far Lateral Lumbar Disc Herniations and the Paramedian Lumbar Disc Herniations. Korean J. Spine 2013, 10, 155. [Google Scholar] [CrossRef] [Green Version]
- Marquardt, G.; Bruder, M.; Theuss, S.; Setzer, M.; Seifert, V. Ultra-long-term outcome of surgically treated far-lateral, extraforaminal lumbar disc herniations: A single-center series. Eur. Spine J. 2012, 21, 660–665. [Google Scholar] [CrossRef] [Green Version]
- Tessitore, E.; De Tribolet, N.; Sonntag, V.K.H.; Benzel, E.C. Far-Lateral Lumbar Disc Herniation: The Microsurgical Transmuscular Approach. Neurosurgery 2004, 54, 939–942. [Google Scholar] [CrossRef]
- Hodges, S.D.; Humphreys, S.C.; Jason, C.E.; Covington, L.A. The surgical treatment of far lateral L3-L4 and L4-L5 disc herniations: A modified technique and outcomes analysis of 25 patients. Spine 1999, 24, 1243–1246. [Google Scholar] [CrossRef] [PubMed]
- O’Hara, L.J.; Marshall, R.W. Far lateral lumbar disc herniation. The key to the intertransverse approach. J. Bone Jt. Surg. Ser. B 1997, 79, 943–947. [Google Scholar] [CrossRef]
- Hitchon, P.W.; Awe, O.O.; Close, L.; Sukkarieh, H.G. Minimally invasive pars approach for foraminal disc herniation. J. Clin. Neurosci. 2015, 22, 1128–1132. [Google Scholar] [CrossRef] [PubMed]
- Phan, K.; Dunn, A.E.; Rao, P.J.; Mobbs, R.J. Far lateral microdiscectomy: A minimally-invasive surgical technique for the treatment of far lateral lumbar disc herniation. J. Spine Surg. 2016, 2, 59–63. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Siu, T.L.T.; Lin, K. Microscopic tubular discectomy for far lateral lumbar disc herniation. J. Clin. Neurosci. 2016, 33, 129–133. [Google Scholar] [CrossRef] [PubMed]
- Soliman, H.; Fridley, J.; Telfeian, A.; Choi, D.B.; Galgano, M.; Kosztowski, T.; Gokaslan, Z.L.; Oyelese, A.A. Minimally Invasive, Far Lateral Lumbar Microdiscectomy with Intraoperative Computed Tomography Navigational Assistance and Electrophysiological Monitoring. World Neurosurg. 2019, 122, e1228–e1239. [Google Scholar] [CrossRef] [PubMed]
- Salame, K.; Lidar, Z. Minimally invasive approach to far lateral lumbar disc herniation: Technique and clinical results. Acta Neurochir. 2010, 152, 663–668. [Google Scholar] [CrossRef]
- Ivanov, A.A.; Faizan, A.; Ebraheim, N.A.; Yeasting, R.; Goel, V.K. The effect of removing the lateral part of the pars interarticularis on stress distribution at the neural arch in lumbar foraminal microdecompression at L3–L4 and L4–L5: Anatomic and finite element investigations. Spine 2007, 32, 2462–2466. [Google Scholar] [CrossRef]
- Sari, R.; Elibol, F.K.E.; Özlü, E.B.K.; Elmacı, İ.; Demir, T. Could isthmic approach to far lateral disc hernias cause instability? Clin. Biomech. 2020, 76, 105004. [Google Scholar] [CrossRef]
- Bae, J.S.; Kang, K.H.; Park, J.H.; Lim, J.H.; Jang, I.T. Postoperative clinical outcome and risk factors for poor outcome of foraminal and extraforaminal lumbar disc herniation. J. Korean Neurosurg. Soc. 2016, 59, 143–148. [Google Scholar] [CrossRef] [Green Version]
- Nicoletti, G.F.; Umana, G.E.; Chaurasia, B.; Ponzo, G.; Giuffrida, M.; Vasta, G.; Tomasi, S.O.; Graziano, F.; Cicero, S.; Scalia, G. Navigation-assisted extraforaminal lumbar disc microdiscectomy: Technical note. J. Craniovertebr. Junction Spine 2020, 11, 316. [Google Scholar] [CrossRef] [PubMed]
- Berra, L.V.; Foti, D.; Ampollini, A.; Faraca, G.; Zullo, N.; Musso, C. Contralateral approach for far lateral lumbar disc herniations: A modified technique and outcome analysis of nine patients. Spine 2010, 35, 709–713. [Google Scholar] [CrossRef] [PubMed]
- Ebraheim, N.A.; Xu, R.; Huntoon, M.; Yeasting, R.A. Location of the extraforaminal lumbar nerve roots. An anatomic study. Clin. Orthop. Relat. Res. 1997, 340, 230–235. [Google Scholar] [CrossRef] [PubMed]
- O’Toole, J.E.; Eichholz, K.M.; Fessler, R.G. Minimally invasive far lateral microendoscopic discectomy for extraforaminal disc herniation at the lumbosacral junction: Cadaveric dissection and technical case report. Spine J. 2007, 7, 414–421. [Google Scholar] [CrossRef]
- Ahsan, K.; Khan, S.; Zaman, N.; Ahmed, N.; Montemurro, N.; Chaurasia, B. Fusion versus nonfusion treatment for recurrent lumbar disc herniation. J. Craniovertebr. Junction Spine 2021, 12, 44–53. [Google Scholar] [CrossRef]

| Technique | Paper | Key Anatomic Landmark for Docking |
|---|---|---|
| Mini-Open Paramedian/Wiltse Approach | Park et al. [8] Marquardt et al. [9] Tessitore et al. [10] Hodges et al. [11] O’Hara and Marshall [12] | Facet Joint and Transverse Processes |
| Microscopic tubular MIS Approach | Hitchon et al. [13] | Pars Interarticularis |
| Phan et al. [14] Siu and Lin [15] Solimon et al. [16] | Facet Joint | |
| Salame et al. [17] Voyadzis et al. [7] | Cranial Transverse Process |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Echt, M.; Bakare, A.; Fessler, R.G. A Modified Approach for Minimally Invasive Tubular Microdiscectomy for Far Lateral Disc Herniations: Docking at the Caudal Level Transverse Process. Medicina 2022, 58, 640. https://doi.org/10.3390/medicina58050640
Echt M, Bakare A, Fessler RG. A Modified Approach for Minimally Invasive Tubular Microdiscectomy for Far Lateral Disc Herniations: Docking at the Caudal Level Transverse Process. Medicina. 2022; 58(5):640. https://doi.org/10.3390/medicina58050640
Chicago/Turabian StyleEcht, Murray, Adewale Bakare, and Richard G. Fessler. 2022. "A Modified Approach for Minimally Invasive Tubular Microdiscectomy for Far Lateral Disc Herniations: Docking at the Caudal Level Transverse Process" Medicina 58, no. 5: 640. https://doi.org/10.3390/medicina58050640
APA StyleEcht, M., Bakare, A., & Fessler, R. G. (2022). A Modified Approach for Minimally Invasive Tubular Microdiscectomy for Far Lateral Disc Herniations: Docking at the Caudal Level Transverse Process. Medicina, 58(5), 640. https://doi.org/10.3390/medicina58050640





