Romanian Version of the Oral Health Values Scale: Adaptation and Validation
Abstract
:1. Introduction
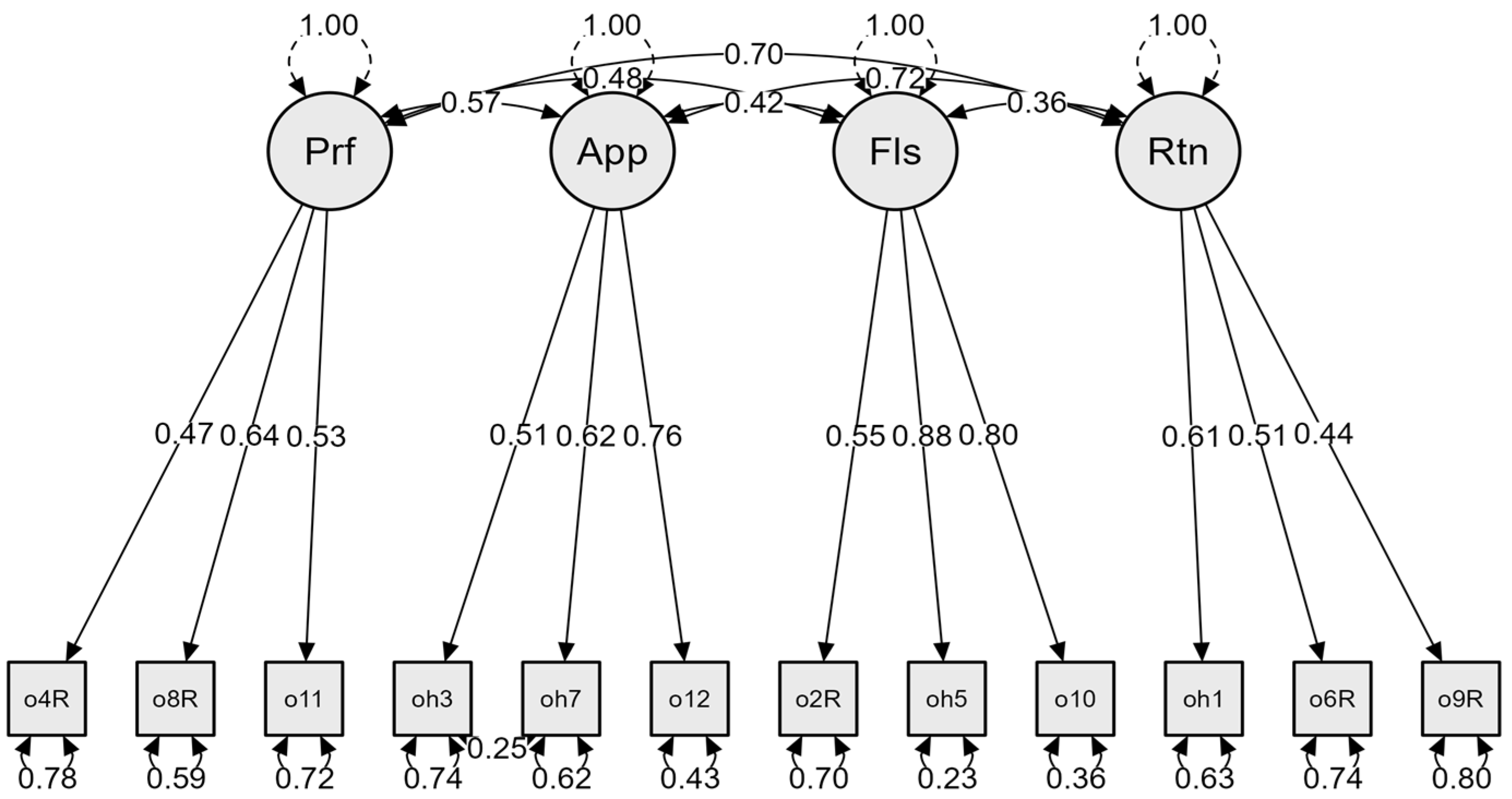
- Professional dental care and the costs associated with it in terms of energy, time, and focus (e.g., Going to a dentist is not worth the cost to me).
- Appearance and health aims to consider dentition as a source of pride and the evaluation of oral health as part of general health (e.g., My smile is an important part of my appearance).
- Flossing as a result of consistent self-care behavior (e.g., Flossing my teeth every day is a high priority for me).
- Retention of natural teeth reflects the values of oral health by means of the implications it has in one’s functioning and personal health (e.g., It is important to me to keep my natural teeth).
Hypotheses
2. Materials and Methods
2.1. Ethical Considerations
2.2. Linguistic Adaptation of the OHVS into Romanian
2.3. Participants and Recruitment Procedure
2.4. Instruments
2.4.1. Oral Health Values Scale
2.4.2. Oral Health Impact Profile OHIP-14
2.4.3. Dental Beliefs Survey-R—R-DBS
2.4.4. Dental Neglect Scale—DNS
2.4.5. Single-Item General Health Literacy Scale—GHL
2.5. The Sociodemographic Data
2.6. Data Analysis
3. Results
3.1. Sociodemographic Characteristics of the Sample
3.2. Factorial Structure
3.3. Reliability and Descriptive Statistics
3.4. Convergent Validity
3.5. Discriminant Validity
3.6. Gender Differences
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
References
- Broadbent, J.M.; Zeng, J.; Foster Page, L.A.; Baker, S.R.; Ramrakha, S.; Thomson, W.M. Oral Health–related Beliefs, Behaviors, and Outcomes through the Life Course. J. Dent. Res. 2016, 95, 808–813. [Google Scholar] [CrossRef] [Green Version]
- Brega, A.G.; Jiang, L.; Johnson, R.L.; Wilson, A.R.; Schmiege, S.J.; Albino, J. Health Literacy and Parental Oral Health Knowledge, Beliefs, Behavior, and Status Among Parents of American Indian Newborns. J. Racial Ethn. Health Disparities 2020, 7, 598–608. [Google Scholar] [CrossRef] [PubMed]
- Fisher-Owens, S.A.; Gansky, S.A.; Platt, L.J.; Weintraub, J.A.; Soobader, M.-J.; Bramlett, M.D.; Newacheck, P.W. Influences on Children’s Oral Health: A Conceptual Model. Pediatrics 2007, 120, e510–e520. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Edwards, C.B.; Randall, C.L.; McNeil, D.W. Development and Validation of the Oral Health Values Scale. Community Dent. Oral Epidemiol. 2021, 49, 454–463. [Google Scholar] [CrossRef] [PubMed]
- Baskaradoss, J.K. Relationship between oral health literacy and oral health status. BMC Oral Health 2018, 18, 172. [Google Scholar] [CrossRef] [PubMed]
- McNeil, D.W.; Randall, C.L. Dental fear and anxiety associated with oral health care: Conceptual and clinical issues. In Behavioral Dentistry, 2nd ed.; Mostofsky, D., Fortune, A., Ames, I.A., Eds.; John Wiley & Sons, Inc.: Hoboken, NY, USA, 2014; pp. 165–192. [Google Scholar]
- Sigurdardottir, A.S.; Geirsdottir, O.G.; Ramel, A.; Arnadottir, I.B. Cross-sectional study of oral health care service, oral health beliefs and oral health care education of caregivers in nursing homes. Geriatr. Nurs. 2022, 43, 138–145. [Google Scholar] [CrossRef]
- Zetu, L.; Zetu, I.; Dogaru, C.B.; Duţă, C.; Dumitrescu, A.L. Gender Variations in the Psychological Factors as Defined by the Extended Health Belief Model of Oral Hygiene Behaviors. Procedia Soc. Behav. Sci. 2014, 127, 358–362. [Google Scholar] [CrossRef] [Green Version]
- Johansson, I.; Torgé, C.J.; Lindmark, U. Is an oral health coaching programme a way to sustain oral health for elderly people in nursing homes? A feasibility study. Int. J. Dent. Hyg. 2020, 18, 107–115. [Google Scholar] [CrossRef]
- National Institute of Dental and Craniofacial Research; National Institute of Health; U.S. Public Health Service, Department of Health and Human Services. The invisible barrier: Literacy and its relationship with oral health. J. Public Health Dent. 2005, 65, 174–182. [Google Scholar] [CrossRef]
- Nakazono, T.T.; Davidson, P.; Andersen, R.M. Oral health beliefs in diverse populations. Adv. Dent. Res. 1997, 11, 235–244. [Google Scholar] [CrossRef]
- Davidson, P.L.; Rams, T.E.; Andfrsen, R.M. Socio-Behavioral Determinants of Oral Hygiene Practices Among USA Ethnic and Age Groups. Adv. Dent. Res. 1997, 11, 245–253. [Google Scholar] [CrossRef] [PubMed]
- Hiratsuka, V.Y.; Robinson, J.M.; Greenlee, R.; Refaat, A. Oral health beliefs and oral hygiene behaviours among parents of urban Alaska Native children. Int. J. Circumpolar Health 2019, 78, 1586274. [Google Scholar] [CrossRef] [Green Version]
- Xiang, B.; Wong, H.M.; Cao, W.; Perfecto, A.P.; McGrath, C.P.J. Development and validation of the Oral health behavior questionnaire for adolescents based on the health belief model (OHBQAHBM). BMC Public Heal. 2020, 20, 701. [Google Scholar] [CrossRef]
- Selvaraj, S.; Naing, N.N.; Wan-Arfah, N.; Karobari, M.I.; Marya, A.; Prasadh, S. Development and Validation of Oral Health Knowledge, Attitude and Behavior Questionnaire among Indian Adults. Medicina 2022, 58, 68. [Google Scholar] [CrossRef] [PubMed]
- Slade, G.D.; Spencer, A.J. Development and evaluation of the Oral Health Impact Profile. Community Dent. Health 1994, 11, 3–11. [Google Scholar] [PubMed]
- Allison, P.; Locker, D.; Jokovic, A.; Slade, G. A Cross-cultural Study of Oral Health Values. J. Dent. Res. 1999, 78, 643–649. [Google Scholar] [CrossRef] [PubMed]
- Kawamura, M. Dental behavioral science. The relationship between perceptions of oral health and oral status in adults. J. Hiroshima Univ. Dent. Soc. 1988, 20, 273–286. [Google Scholar]
- Oancea, R.; Hernandez, D.; Mesaroș, A.S. Key elements of maintaining good oral hygiene in German and Romanian young adults. J. Med. Brasovean 2018, 1, 73–79. [Google Scholar]
- Graça, S.R.; Albuquerque, T.S.; Luis, H.S.; Assunção, V.A.; Malmqvist, S.; Cuculescu, M.; Slusanschi, O.; Johannsen, G.; Galuscan, A.; Podariu, A.C.; et al. Oral Health Knowledge, Perceptions, and Habits of Adolescents from Portugal, Romania, and Sweden: A Comparative Study. J. Int. Soc. Prev. Commun. Dent. 2019, 9, 470–480. [Google Scholar]
- Lucaciu, P.O.; Mester, A.; Constantin, I.; Orban, N.; Cosma, L.; Candrea, S.; Sava-Rosianu, R.; Mesaros, A.S. A WHO Pathfinder Survey of Dental Caries in 6 and 12-Year Old Transylvanian Children and the Possible Correlation with Their Family Background, Oral-Health Behavior, and the Intake of Sweets. Int. J. Environ. Res. Public Health 2020, 17, 4180. [Google Scholar] [CrossRef]
- National Inspectorate of Public Health. Available online: https://www.dsptr.ro/campania-fii-mandru-de-zambetul-tau-ai-grija-de-sanatatea-ta-orala-martie-2021/ (accessed on 10 March 2022).
- Sousa, V.D.; Rojjanasrirat, W. Translation, adaptation and validation of instruments or scales for use in cross-cultural health care research: A clear and user-friendly guideline. J. Eval. Clin. Pract. 2010, 17, 268–274. [Google Scholar] [CrossRef] [PubMed]
- Podsakoff, P.M.; MacKenzie, S.B.; Lee, J.Y.; Podsakoff, N.P. Common method biases in behavioral research: A critical review of the literature and recommended remedies. J. Appl. Psychol. 2003, 88, 879–903. [Google Scholar] [CrossRef] [PubMed]
- Slade, G.D. Derivation and validation of a short-form oral health impact profile. Community Dent. Oral Epidemiol. 1997, 25, 284–290. [Google Scholar] [CrossRef] [PubMed]
- Slusanschi, O.; Moraru, R.; Garneata, L.; Mircescu, G.; Cuculescu, M.; Preoteasa, E. Validation of a Romanian Version of the Short Form of the Oral Health Impact Profile (OHIP-14) for Use in an Urban Adult Population. Oral. Health Prev. Dent. 2013, 11, 235–242. [Google Scholar] [CrossRef]
- Milgrom, P.; Weinstein, P.; Getz, T. Treating Fearful Dental Patients: A Patient Management Handbook, 2nd ed.; University of Washington Continuing Dental Education: Seattle, WA, USA, 1995. [Google Scholar]
- Coolidge, T.; Heima, M.; Coldwell, S.E.; Weinstein, P.; Milgrom, P. Psychometric properties of the Revised Dental Beliefs Survey. Community Dent. Oral Epidemiol. 2005, 33, 289–297. [Google Scholar] [CrossRef]
- Balgiu, B.A.; Sfeatcu, R.; Sluşanski, O.; Dumitrache, M.A. Linguistic and cultural validation of the Romanian version of the Revised Dental Beliefs survey. Int. J. Med. Dent. 2020, 24, 381–389. [Google Scholar]
- Jamieson, L.M.; Thomson, W.M. The Dental Neglect and Dental Indifference scales compared. Community Dent. Oral Epidemiol. 2002, 30, 168–175. [Google Scholar] [CrossRef]
- Thomson, W.M.; Locker, D. Dental neglect and dental health among 26-year-olds in the Dunedin Multidisciplinary Health and Development Study. Community Dent. Oral Epidemiol. 2000, 28, 414–418. [Google Scholar] [CrossRef]
- Coolidge, T.; Heima, M.; Johnson, E.K.; Weinstein, P. The Dental Neglect Scale in adolescents. BMC Oral Health 2009, 9, 2. [Google Scholar] [CrossRef] [Green Version]
- Chew, L.D.; Bradley, K.A.; Boyko, E.J. Brief questions to identify patients with inadequate health literacy. Fam. Med. 2004, 36, 588–594. [Google Scholar]
- Brown, T.A.; Moore, M.T. Confirmatory factor analysis. In Handbook of Structural Equation Modeling; Hoyle, R.H., Ed.; Guilford Press: New York, NY, USA, 2012; pp. 361–379. [Google Scholar]
- Schermelleh-Engel, K.; Moosbrugger, H.; Müller, H. Evaluating the fit of structural equation models: Tests of significance and descriptive goodness-of-fit measures. MPR-Online 2003, 8, 23–74. [Google Scholar]
- West, S.G.; Taylor, A.B.; Wu, W. Model fit and model selection in structural equation modeling. In Handbook of Structural Equation Modeling; Hoyle, R.H., Ed.; The Guilford Press: New York, NY, USA, 2012; pp. 209–231. [Google Scholar]
- Hu, L.T.; Bentler, P.M. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct. Equ. Model. Multidiscip. J. 1999, 6, 1–55. [Google Scholar] [CrossRef]
- Tabachnick, B.G.; Fidell, L.S. Using Multivariate Statistics, 5th ed.; Allyn & Bacon/Pearson Education: Boston, MA, USA, 2007. [Google Scholar]
- Hair, J.F.; Black, W.C.; Babin, B.J.; Anderson, R.E. Multivariate Data Analysis, 7th ed.; Pearson Education Limited: Essex, UK, 2014. [Google Scholar]
- Fornell, C.; Larcker, D.F. Structural equation models with unobservable variables and measurement error: Algebra and statistics. J. Mark. Res. 1981, 18, 382–388. [Google Scholar] [CrossRef]
- Bagozzi, R.P.; Yi, Y.; Phillips, L.W. Assessing Construct Validity in Organizational Research. Adm. Sci. Q. 1991, 36, 421–458. [Google Scholar] [CrossRef]
- Tehseen, S.; Ramayah, T.; Sajilan, S. Testing and Controlling for Common Method Variance: A Review of Available Methods. J. Manag. Sci. 2017, 4, 142–175. [Google Scholar] [CrossRef]
- Babyak, M.A.; Green, S.B. Confirmatory Factor Analysis: An Introduction for Psychosomatic Medicine Researchers. Psychosom. Med. 2010, 72, 587–597. [Google Scholar] [CrossRef]
- Pituch, K.A.; Stevens, J.P. Applied Multivariate Statistics for the Social Sciences Analyses with SAS and IBM’s SPSS, 6th ed.; Routledge Taylor & Frances Group: London, UK, 2016. [Google Scholar]
- Kline, T.J.B. Psychological Testing: A Practical Approach to Design and Evaluation; SAGE Publications: Thousand Oaks, CA, USA, 2005. [Google Scholar]
- Furnham, A. Relationship among Four Big Five Measures of Different Length. Psychol. Rep. 2008, 102, 312–316. [Google Scholar] [CrossRef]
- Pallant, J. SPSS Survival Manual: A Step by Step Guide to Data Analysis Using the SPSS Program, 4th ed.; Open University Press: Maidenhead, UK, 2010. [Google Scholar]
- Liddell, A.; Locker, D. Gender and age differences in attitudes to dental pain and dental control. Community Dent. Oral Epidemiol. 1997, 25, 314–318. [Google Scholar] [CrossRef]
- Thompson, A.E.; Anisimowicz, Y.; Miedema, B.; Hogg, W.; Wodchis, W.P.; Aubrey-Bassler, K. The influence of gender and other patient characteristics on health care-seeking behaviour: A QUALICOPC study. BMC Fam. Pract. 2016, 17, 38. [Google Scholar] [CrossRef] [Green Version]
- Fukai, K.; Takaesu, Y.; Maki, Y. Gender Differences in Oral Health Behavior and General Health Habits in an Adult Population. Bull. Tokyo Dent. Coll. 1999, 40, 187–193. [Google Scholar] [CrossRef] [Green Version]
- Furuta, M.; Ekuni, D.; Irie, K.; Azuma, T.; Tomofuji, T.; Ogura, T.; Morita, M. Sex Differences in Gingivitis Relate to Interaction of Oral Health Behaviors in Young People. J. Periodontol. 2011, 82, 558–565. [Google Scholar] [CrossRef] [PubMed]
- Lipsky, M.S.; Su, S.; Crespo, C.J.; Hung, M. Men and Oral Health: A Review of Sex and Gender Differences. Am. J. Men’s Health 2021, 15, 15579883211016361. [Google Scholar] [CrossRef] [PubMed]
- Bendoraitienė, E.; Zūbienė, J.; Vasiliauskienė, I.; Saldūnaitė, K.; Andruškevičienė, V.; Basevičienė, N.; Slabšinskienė, E. Periodontal status in 18-year-old Lithuanian adolescents: An epidemiological study. Medicina 2017, 53, 253–258. [Google Scholar] [CrossRef] [PubMed]
- Hamasha, A.A.-H.; Alshehri, A.; Alshubaiki, A.; Alssafi, F.; Alamam, H.; Alshunaiber, R. Gender-specific oral health beliefs and behaviors among adult patients attending King Abdulaziz Medical City in Riyadh. Saudi Dent. J. 2018, 30, 226–231. [Google Scholar] [CrossRef]
- Fleming, E.B.; Nguyen, D.; Afful, J.; Carroll, M.D.; Woods, P.D. Prevalence of daily flossing among adults by selected risk factors for periodontal disease-United States, 2011–2014. J. Periodontol. 2018, 89, 933–939. [Google Scholar] [CrossRef] [PubMed]
- Ward, K.; Briddon, M. The hidden costs of a hidden smile: The value of preventive care from the patient’s perspective. J. Public Health Dent. 2020, 80, S83–S85. [Google Scholar] [CrossRef]
| Models | χ2 | df | χ2/df | CFI | IFI | TLI | RMSEA (CI90%) | SRMR | AIC |
|---|---|---|---|---|---|---|---|---|---|
| M1 four factors without correlated errors | 133.101 | 48 | 2.77 | 0.96 | 0.96 | 0.96 | 0.045 (0.036–0.054) | 0.037 | 217.101 |
| M1 four factors with correlated errors | 114.285 | 47 | 2.43 | 0.97 | 0.97 | 0.95 | 0.041 (0.031–0.050) | 0.034 | 200.285 |
| Factors | M | S.D. | Min–Max | α | ω |
|---|---|---|---|---|---|
| Professional dental care | 11.72 | 2.70 | 1–5 | 0.57 | 0.56 |
| Appearance | 13.97 | 1.71 | 1–5 | 0.72 | 0.72 |
| Flossing | 8.93 | 3.30 | 1–5 | 0.78 | 0.79 |
| Retention teeth | 13.47 | 1.81 | 1–5 | 0.46 | 0.46 |
| OHVS total score | 48.12 | 6.75 | 19–60 | 0.76 | 0.76 |
| Items | M | S.D. | Skewness | Kurtosis | α if Item Deleted |
|---|---|---|---|---|---|
| 1 | 4.85 | 0.45 | −3.70 | 15.89 | 0.75 |
| 2 | 2.89 | 1.31 | 0.11 | −1.00 | 0.74 |
| 3 | 4.70 | 0.67 | −2.79 | 8.59 | 0.75 |
| 4 | 4.07 | 1.14 | −1,12 | 0.35 | 0.75 |
| 5 | 2.99 | 1.28 | 0.02 | −1.00 | 0.72 |
| 6 | 4.84 | 0.63 | −4.60 | 21.71 | 0.75 |
| 7 | 4.60 | 0.78 | −2.15 | 4.62 | 0.74 |
| 8 | 4.07 | 1.15 | −1.07 | 0.09 | 0.73 |
| 9 | 3.79 | 1.28 | 0.72 | −0.63 | 0.75 |
| 10 | 3.05 | 1.35 | −0.01 | −1.13 | 0.73 |
| 11 | 3.57 | 1.39 | −0.56 | −0.98 | 0.75 |
| 12 | 4.68 | 0.64 | −2.26 | 5.57 | 0.74 |
| Variables | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
|---|---|---|---|---|---|---|---|---|
| 1. OHVS total | - | |||||||
| 2. Professional dental care | 0.74 *** | - | ||||||
| 3. Appearance | 0.62 *** | 0.31 *** | - | |||||
| 4. Flossing | 0.76 *** | 0.34 *** | 0.30 *** | - | ||||
| 5.Retention | 0.62 *** | 0.37 *** | 0.36 *** | 0.23 *** | - | |||
| 6. OHIP-14 | −0.16 *** | −0.14 *** | −0.07 * | −0.10 ** | −0.15 *** | - | ||
| 7. DNS | 0.37 *** | 0.21 *** | 0.32 ** | 0.36 *** | 0.11 *** | −0.11 ** | - | |
| 8. R-DBS | −0.33 *** | −0.36 *** | −0.19 *** | −0.17 *** | −0.21 *** | 0.20 ** | −0.13 *** | - |
| 9. Health literacy | 0.34 *** | 0.27 *** | 0.23 *** | 0.24 *** | 0.19 ** | −0.14 ** | 0.19 ** | −0.31 *** |
| Factors | 1 | 2 | 3 | 4 |
|---|---|---|---|---|
| Professional dental care | 0.55 * | |||
| Appearance | 0.31 | 0.64 * | ||
| Flossing | 0.34 | 0.30 | 0.75 * | |
| Retention | 0.37 | 0.36 | 0.23 | 0.51 * |
| Factors | Mean Rank | Mann–Whitney U | Z | |
|---|---|---|---|---|
| Males | Females | |||
| Professional dental care | 375.02 | 460.02 | 62,505.00 | 4.56 |
| Appearance | 328.77 | 478.78 | 50,894.50 | 9.13 |
| Flossing | 355.22 | 468.05 | 57,334.50 | 6.02 |
| Retention | 380.34 | 457.87 | 63,840.50 | 4.29 |
| OHVS total score | 329.38 | 478.53 | 51,049.00 | 7.94 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Balgiu, B.A.; Sfeatcu, R.; Mihai, C.; Lupușoru, M.; Bucur, M.V.; Tribus, L. Romanian Version of the Oral Health Values Scale: Adaptation and Validation. Medicina 2022, 58, 544. https://doi.org/10.3390/medicina58040544
Balgiu BA, Sfeatcu R, Mihai C, Lupușoru M, Bucur MV, Tribus L. Romanian Version of the Oral Health Values Scale: Adaptation and Validation. Medicina. 2022; 58(4):544. https://doi.org/10.3390/medicina58040544
Chicago/Turabian StyleBalgiu, Beatrice Adriana, Ruxandra Sfeatcu, Christina Mihai, Mircea Lupușoru, Mirela Veronica Bucur, and Laura Tribus. 2022. "Romanian Version of the Oral Health Values Scale: Adaptation and Validation" Medicina 58, no. 4: 544. https://doi.org/10.3390/medicina58040544
APA StyleBalgiu, B. A., Sfeatcu, R., Mihai, C., Lupușoru, M., Bucur, M. V., & Tribus, L. (2022). Romanian Version of the Oral Health Values Scale: Adaptation and Validation. Medicina, 58(4), 544. https://doi.org/10.3390/medicina58040544







