The Effect of Scapular Fixation on Scapular and Humeral Head Movements during Glenohumeral Axial Distraction Mobilization
Abstract
1. Introduction
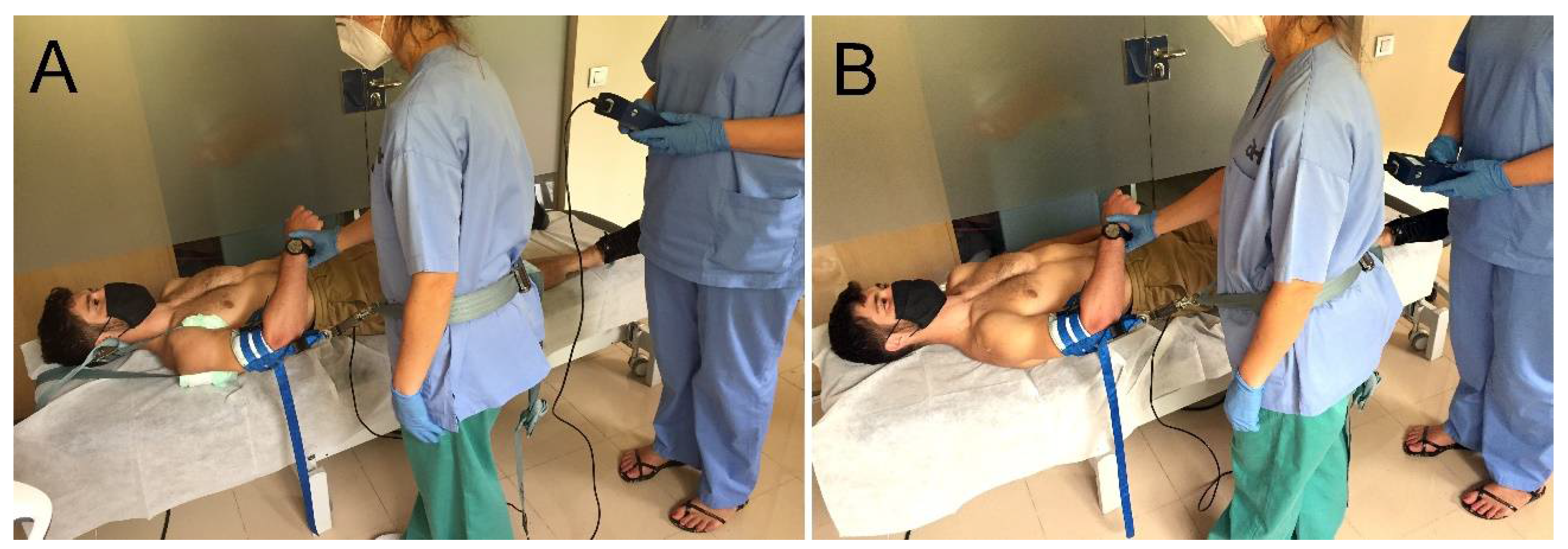
2. Materials and Methods
3. Results
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Djade, C.D.; Porgo, T.V.; Zomahoun, H.T.V.; Perrault-Sullivan, G.; Dionne, C.E. Incidence of shoulder pain in 40 years old and over and associated factors: A systematic review. Eur. J. Pain 2020, 24, 39–50. [Google Scholar] [CrossRef] [PubMed]
- Ludewig, P.M.; Cook, T.M. Translations of the Humerus in Persons with Shoulder Impingement Symptoms. J. Orthop. Sports Phys. Ther. 2002, 32, 248–259. [Google Scholar] [CrossRef] [PubMed]
- Kelley, M.J.; Shaffer, M.A.; Kuhn, J.E.; Michener, L.A.; Seitz, A.L.; Uhl, T.L.; Godges, J.J.; McClure, P.W. Shoulder Pain and Mobility Deficits: Adhesive Capsulitis. J. Orthop. Sports Phys. Ther. 2013, 43, A1–A31. [Google Scholar] [CrossRef] [PubMed]
- Noten, S.; Meeus, M.; Stassijns, G.; Van Glabbeek, F.; Verborgt, O.; Struyf, F. Efficacy of Different Types of Mobilization Techniques in Patients with Primary Adhesive Capsulitis of the Shoulder: A Systematic Review. Arch. Phys. Med. Rehabil. 2016, 97, 815–825. [Google Scholar] [CrossRef]
- Espinoza, H.J.G.; Pavez, F.; Guajardo, C.; Acosta, M.B. Glenohumeral posterior mobilization versus conventional physiotherapy for primary adhesive capsulitis: A randomized clinical trial. Medwave 2015, 15, e6267. [Google Scholar] [CrossRef]
- Johnson, A.J.; Godges, J.J.; Zimmerman, G.J.; Ounanian, L.L. The Effect of Anterior Versus Posterior Glide Joint Mobilization on External Rotation Range of Motion in Patients with Shoulder Adhesive Capsulitis. J. Orthop. Sports Phys. Ther. 2007, 37, 88–99. [Google Scholar] [CrossRef]
- Hsu, A.-T.; Ho, L.; Ho, S.; Hedman, T. Immediate response of glenohumeral abduction range of motion to a caudally directed translational mobilization: A fresh cadaver simulation. Arch. Phys. Med. Rehabil. 2000, 81, 1511–1516. [Google Scholar] [CrossRef]
- Graichen, H.; Stammberger, T.; Bonel, H.M.; Englmeier, K.-H.; Reiser, M.; Eckstein, F. Glenohumeral translation during active and passive elevation of the shoulder—A 3D open-MRI study. J. Biomech. 2000, 33, 609–613. [Google Scholar] [CrossRef]
- Chopp, J.N.; O’Neill, J.M.; Hurley, K.; Dickerson, C.R. Superior humeral head migration occurs after a protocol designed to fatigue the rotator cuff: A radiographic analysis. J. Shoulder Elb. Surg. 2010, 19, 1137–1144. [Google Scholar] [CrossRef]
- Kaltenborn, F.; Evjenth, O.; Kaltenborn, T.; Morgan, D.; Vollowitz, E. Manual Mobilization of the Joints: Joint Examination and Basic Treatment: The Extremities; Olaf Norlis Bokhandel: Oslo, Norway, 2015; Volume I. [Google Scholar]
- Ho, K.-Y.; Hsu, A.-T. Displacement of the head of humerus while performing “mobilization with movements” in glenohumeral joint: A cadaver study. Man. Ther. 2009, 14, 160–166. [Google Scholar] [CrossRef]
- Senbursa, G.; Baltacı, G.; Atay, A. Comparison of conservative treatment with and without manual physical therapy for patients with shoulder impingement syndrome: A prospective, randomized clinical trial. Knee Surg. Sports Traumatol. Arthrosc. 2007, 15, 915–921. [Google Scholar] [CrossRef] [PubMed]
- Şenbursa, G.; Baltaci, G.; Atay, A. The effectiveness of manual therapy in supraspinatus tendinopathy. Acta Orthop. Traumatol. Turc. 2011, 45, 162–167. [Google Scholar] [CrossRef] [PubMed]
- Lin, H.-T.; Hsu, A.-T.; An, K.-N.; Chien, J.-R.C.; Kuan, T.-S.; Chang, G.-L. Reliability of stiffness measured in glenohumeral joint and its application to assess the effect of end-range mobilization in subjects with adhesive capsulitis. Man. Ther. 2008, 13, 307–316. [Google Scholar] [CrossRef] [PubMed]
- Bang, M.D.; Deyle, G.D. Comparison of Supervised Exercise with and Without Manual Physical Therapy for Patients with Shoulder Impingement Syndrome. J. Orthop. Sports Phys. Ther. 2000, 30, 126–137. [Google Scholar] [CrossRef]
- Conroy, D.E.; Hayes, K.W. The Effect of Joint Mobilization as a Component of Comprehensive Treatment for Primary Shoulder Impingement Syndrome. J. Orthop. Sports Phys. Ther. 1998, 28, 3–14. [Google Scholar] [CrossRef]
- Barbosa, R.; Goes, R.; Mazzer, N.; Fonseca, M. The influence of joint mobilization on tendinopathy of the biceps brachii and supraspinatus muscles. Braz. J. Phys. Ther. 2008, 12, 298–303. [Google Scholar] [CrossRef]
- Ong, H.S.; Ji, T.; Zhang, C.P. The Pedicled Latissimus Dorsi Myocutaneous Flap in Head and Neck Reconstruction. Oral Maxillofac. Surg. Clin. N. Am. 2014, 26, 427–434. [Google Scholar] [CrossRef]
- Brudvig, T.J.; Kulkarni, H.; Shah, S. The Effect of Therapeutic Exercise and Mobilization on Patients with Shoulder Dysfunction: A Systematic Review with Meta-analysis. J. Orthop. Sports Phys. Ther. 2011, 41, 734–748. [Google Scholar] [CrossRef]
- Witt, D.W.; Talbott, N.R. In-vivo measurements of force and humeral movement during inferior glenohumeral mobilizations. Man. Ther. 2016, 21, 198–203. [Google Scholar] [CrossRef]
- Witt, D.W.; Talbott, N.R. The effect of shoulder position on inferior glenohumeral mobilization. J. Hand Ther. 2018, 31, 381–389. [Google Scholar] [CrossRef]
- Soldado, F.; Ghizoni, M.F.; Bertelli, J. Injury mechanisms in supraclavicular stretch injuries of the brachial plexus. Hand Surg. Rehabil. 2016, 35, 51–54. [Google Scholar] [CrossRef] [PubMed]
- Zapałowicz, K.; Radek, M. The distribution of brachial plexus lesions after experimental traction: A cadaveric study. J. Neurosurg. Spine 2018, 29, 704–710. [Google Scholar] [CrossRef]
- Tavakkolizadeh, A.; Saifuddin, A.; Birch, R. Imaging of Adult Brachial Plexus Traction Injuries. J. Hand Surg. 2001, 26, 183–191. [Google Scholar] [CrossRef] [PubMed]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences; Lawrence Erlbaum Associates Inc.: Hillsdale, NJ, USA, 1988. [Google Scholar]
- Garwood, E.R.; Souza, R.B.; Zhang, A.; Zhang, A.L.; Ma, C.B.; Link, T.M.; Motamedi, D. Axial traction magnetic resonance imaging (MRI) of the glenohumeral joint in healthy volunteers: Initial experience. Clin. Imaging 2017, 42, 178–182. [Google Scholar] [CrossRef] [PubMed]
- Moon, G.D.; Lim, J.Y.; Kim, D.Y.; Kim, T.H. Comparison of Maitland and Kaltenborn mobilization techniques for improving shoulder pain and range of motion in frozen shoulders. J. Phys. Ther. Sci. 2015, 27, 1391–1395. [Google Scholar] [CrossRef]
- Agarwal, S.; Raza, S.; Moiz, J.A.; Anwer, S.; Alghadir, A.H. Effects of two different mobilization techniques on pain, range of motion and functional disability in patients with adhesive capsulitis: A comparative study. J. Phys. Ther. Sci. 2016, 28, 3342–3349. [Google Scholar] [CrossRef][Green Version]
- Sarkari, E.; Dhakshinamoorthy, P.; Multani, N.K. Comparison of Caudal and Antero-Posterior Glide Mobilisation for the Improvement of Abduction Range of Motion. J. Exerc. Sci. Physiother. 2006, 2, 59–65. [Google Scholar]
- Estébanez-De-Miguel, E.; López-De-Celis, C.; Caudevilla-Polo, S.; González-Rueda, V.; Bueno-Gracia, E.; Pérez-Bellmunt, A. The effect of high, medium and low mobilization forces applied during a hip long-axis distraction mobilization on the strain on the inferior ilio-femoral ligament and psoas muscle: A cadaveric study. Musculoskelet. Sci. Pract. 2020, 47, 102148. [Google Scholar] [CrossRef]
- Estébanez-De-Miguel, E.; Caudevilla-Polo, S.; González-Rueda, V.; Bueno-Gracia, E.; Pérez-Bellmunt, A.; López-De-Celis, C. Ultrasound measurement of the effects of high, medium and low hip long-axis distraction mobilization forces on the joint space width and its correlation with the joint strain. Musculoskelet. Sci. Pract. 2020, 50, 102225. [Google Scholar] [CrossRef]
- Estébanez-De-Miguel, E.; González-Rueda, V.; Bueno-Gracia, E.; Pérez-Bellmunt, A.; López-De-Celis, C.; Caudevilla-Polo, S. The immediate effects of 5-minute high-force long axis distraction mobilization on the strain on the inferior ilio-femoral ligament and hip range of motion: A cadaveric study. Musculoskelet. Sci. Pract. 2020, 50, 102262. [Google Scholar] [CrossRef]
- Rollo, G.; Huri, G.; Meccariello, L.; Familiari, F.; Çetik, R.M.; Cataldi, C.; Conteduca, J.; Giaracuni, M.; Bisaccia, M.; Longo, D.; et al. Scapular body fractures: Short-term results of surgical management with extended indications. Injury 2021, 52, 481–486. [Google Scholar] [CrossRef] [PubMed]
- Estébanez-De-Miguel, E.; Fortún-Agud, M.; Jimenez-Del-Barrio, S.; Caudevilla-Polo, S.; Bueno-Gracia, E.; Tricás-Moreno, J.M. Comparison of high, medium and low mobilization forces for increasing range of motion in patients with hip osteoarthritis: A randomized controlled trial. Musculoskelet. Sci. Pract. 2018, 36, 81–86. [Google Scholar] [CrossRef]
- Vermeulen, H.M.; Rozing, P.M.; Obermann, W.R.; le Cessie, S.; Vlieland, T.V. Comparison of High-Grade and Low-Grade Mobilization Techniques in the Management of Adhesive Capsulitis of the Shoulder: Randomized Controlled Trial. Phys. Ther. 2006, 86, 355–368. [Google Scholar] [CrossRef] [PubMed]
- Maher, S.; Creighton, D.; Kondratek, M.; Krauss, J.; Qu, X. The effect of tibio-femoral traction mobilization on passive knee flexion motion impairment and pain: A case series. J. Man. Manip. Ther. 2010, 18, 29–36. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Courtney, C.A.; Steffen, A.D.; Fernández-De-Las-Peñas, C.; Kim, J.; Chmell, S.J. Joint Mobilization Enhances Mechanisms of Conditioned Pain Modulation in Individuals with Osteoarthritis of the Knee. J. Orthop. Sports Phys. Ther. 2016, 46, 168–176. [Google Scholar] [CrossRef] [PubMed]
- Courtney, C.A.; Witte, P.O.; Chmell, S.J.; Hornby, T.G. Heightened Flexor Withdrawal Response in Individuals with Knee Osteoarthritis Is Modulated by Joint Compression and Joint Mobilization. J. Pain 2010, 11, 179–185. [Google Scholar] [CrossRef] [PubMed]
- Park, S.-S.; Kim, B.-K.; Moon, O.-K.; Choi, W.-S. Effects of joint position on the distraction distance during grade III glenohumeral joint distraction in healthy individuals. J. Phys. Ther. Sci. 2015, 27, 3279–3281. [Google Scholar] [CrossRef][Green Version]

| Magnitude of Force | ICC3, 1 (95% CI) | SEM | MDD95 |
|---|---|---|---|
| Baseline | 0.996 (0.986–0.999) | 0.01 mm | 0.02 |
| Low-force GADM | 0.993 (0.972–0.998) | 0.02 mm | 0.05 |
| Medium-force GADM | 0.996 (0.972–0.998) | 0.01 mm | 0.02 |
| High-force GADM | 0.997 (0.990–0.999) | 0.01 mm | 0.02 |
| Mean ± SD or N (%) | |
|---|---|
| Age (year) | 28.67 ± 9.31 |
| Gender | |
| Men | 11 (73.3%) |
| Women | 4 (26.7%) |
| Dominance | |
| Right | 13 (86.7%) |
| Left | 2 (13.3%) |
| Height (cm) | 175 ± 8.28 |
| Weight (kg) | 71.80 ± 11.80 |
| BMI (kg/m2) | 23.40 ± 2.47 |
| Variable | Magnitude of GADM Force | Scapular Fixation | Non-Scapular Fixation | Mean Difference (95%CI) | Effect Size | p Value |
|---|---|---|---|---|---|---|
| Caudal movement of the humeral head | Low-force (16.21 ± 5.10 N) | 0.74 ± 0.55 mm | 1.21 ± 0.67 mm | 0.47 mm (0.11, 0.83) p = 0.012 | 0.78 | F = 5.262 p = 0.008 |
| Medium-force (46.71 ± 12.39 N) | 1.62 ± 0.82 mm | 3.04 ± 1.45 mm | 1.42 mm (0.89, 1.94) p < 0.001 | 1.21 | ||
| High-force (200.98 ± 51.19 N) | 5.38 ± 1.95 mm | 6.15 ± 2.39 mm | 0.77 mm (1.02, 1.45) p = 0.026 | 0.35 | ||
| Scapular movement | Low-force (16.21 ± 5.10 N) | 55.05 ± 0.12° | 57.06 ± 57° | 2.01° (1.78, 2.23) p < 0.001 | 4.88 | F = 1966.56 p < 0.001 |
| Medium-force (46.71 ± 12.39 N) | 55.75 ± 0.58° | 62.58 ± 78° | 6.84° (6.49, 7.19) p < 0.001 | 9.94 | ||
| High-force (200.98 ± 51.19 N) | 55.91 ± 0.12° | 74.55 ± 1.37° | 18.63° (18.80, 19.18) p < 0.001 | 19.17 |
| Low-Force | Medium-Force | High-Force | ||||
|---|---|---|---|---|---|---|
| T1 N (%) | T2 N (%) | T1 N (%) | T2 N (%) | T1 N (%) | T2 N (%) | |
| Scapular Fixation | ||||||
| Nowhere | 22 (78.6%) | 23 (82.1%) | 2 (7.1%) | 1 (3.6%) | 0 (0%) | 0 (0%) |
| Glenohumeral joint | 6 (21.4%) | 5 (17.9%) | 26 (92.9%) | 27 (96.4%) | 24 (85.7%) | 24 (85.7%) |
| Shoulder girdle | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 4 (14.3%) | 4 (14.3%) |
| Neck | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) |
| Non-scapular Fixation | ||||||
| Nowhere | 22 (78.6%) | 21 (75%) | 17 (60.7%) | 17 (60.7%) | 4 (14.3%) | 4 (14.3%) |
| Glenohumeral joint | 0 (0%) | 0 (0%) | 2 (7.1%) | 1 (3.6%) | 0 (0%) | 0 (0%) |
| Shoulder girdle | 5 (17.9%) | 2 (7.1%) | 6 (21.4%) | 6 (21.4%) | 18 (64.3 %) | 16 (57.1%) |
| Neck | 1 (3.6%) | 5 (17.9%) | 3 (10.7%) | 4 (14.3%) | 6 (21.4%) | 8 (28.6%) |
| p value * | <0.002 | <0.001 | <0.001 | <0.003 | <0.001 | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
López-de-Celis, C.; Estébanez-de-Miguel, E.; Pérez-Bellmunt, A.; Caudevilla-Polo, S.; González-Rueda, V.; Bueno-Gracia, E. The Effect of Scapular Fixation on Scapular and Humeral Head Movements during Glenohumeral Axial Distraction Mobilization. Medicina 2022, 58, 454. https://doi.org/10.3390/medicina58030454
López-de-Celis C, Estébanez-de-Miguel E, Pérez-Bellmunt A, Caudevilla-Polo S, González-Rueda V, Bueno-Gracia E. The Effect of Scapular Fixation on Scapular and Humeral Head Movements during Glenohumeral Axial Distraction Mobilization. Medicina. 2022; 58(3):454. https://doi.org/10.3390/medicina58030454
Chicago/Turabian StyleLópez-de-Celis, Carlos, Elena Estébanez-de-Miguel, Albert Pérez-Bellmunt, Santos Caudevilla-Polo, Vanessa González-Rueda, and Elena Bueno-Gracia. 2022. "The Effect of Scapular Fixation on Scapular and Humeral Head Movements during Glenohumeral Axial Distraction Mobilization" Medicina 58, no. 3: 454. https://doi.org/10.3390/medicina58030454
APA StyleLópez-de-Celis, C., Estébanez-de-Miguel, E., Pérez-Bellmunt, A., Caudevilla-Polo, S., González-Rueda, V., & Bueno-Gracia, E. (2022). The Effect of Scapular Fixation on Scapular and Humeral Head Movements during Glenohumeral Axial Distraction Mobilization. Medicina, 58(3), 454. https://doi.org/10.3390/medicina58030454








