Diagnostic Criteria for Metabolic Syndrome in High-Altitude Regions: A Systematic Review
Abstract
:1. Introduction
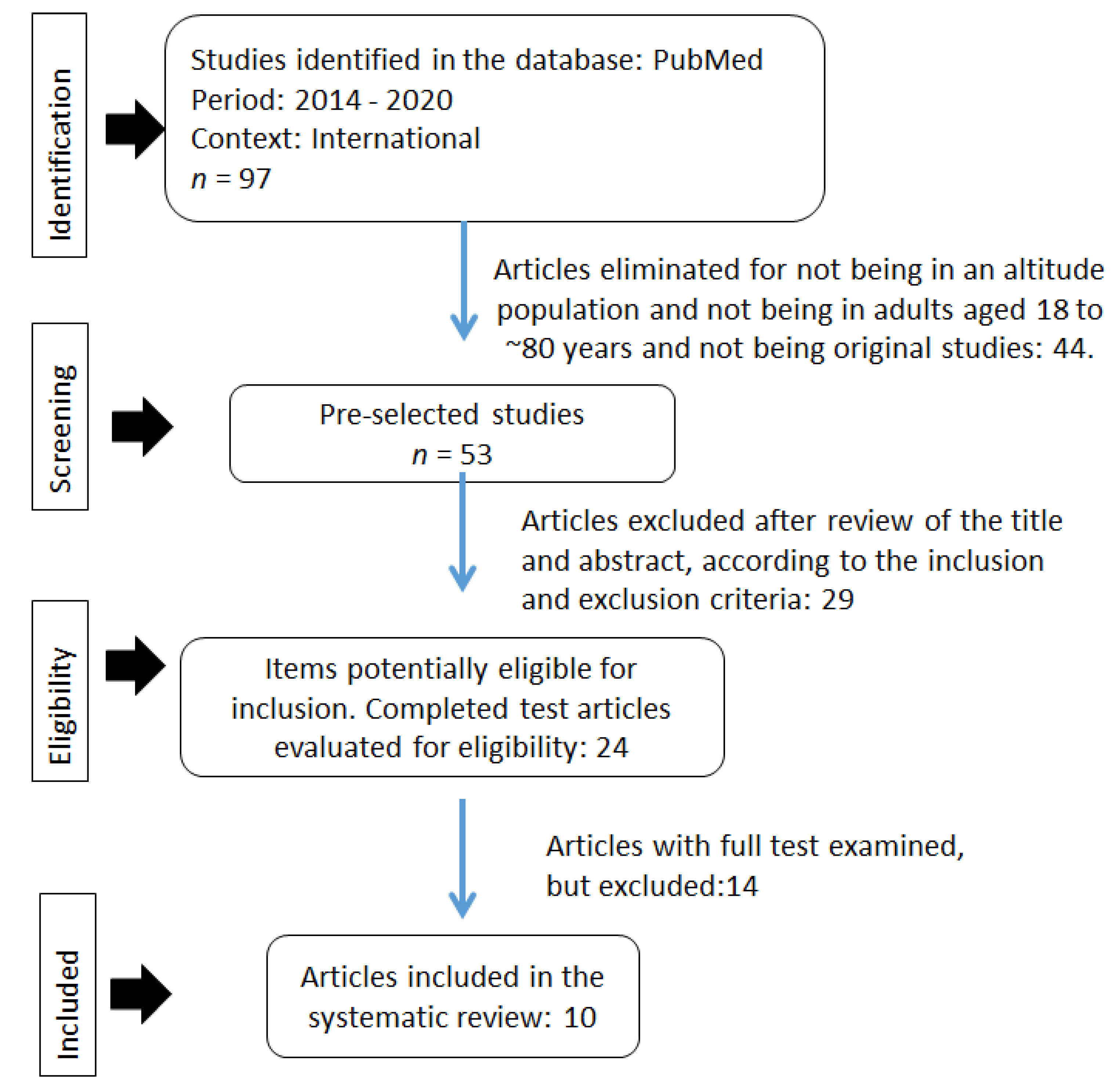
2. Materials and Methods
2.1. Type of Study
2.2. Eligibility Criteria
2.3. Search Strategy
2.4. Methodological Quality
2.5. Data Extraction and Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Informed Consent Statement
Conflicts of Interest
References
- Saklayen, M.G. The Global Epidemic of the Metabolic Syndrome. Curr. Hypertens. Rep. 2018, 20, 12. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Reaven, G.M. Role of insulin resistance in human disease (syndrome X): An expanded definition. Annu. Rev. Med. 1993, 44, 121–131. [Google Scholar] [CrossRef] [PubMed]
- Ju, S.Y.; Lee, J.Y.; Kim, D.H. Association of metabolic syndrome and its components with all-cause and cardiovascular mortality in the elderly: A meta-analysis of prospective cohort studies. Medicine (Baltimore) 2017, 96, e8491. [Google Scholar] [CrossRef]
- Wilson, P.W.; D’Agostino, R.B.; Parise, H.; Sullivan, L.; Meigs, J.B. Metabolic syndrome as a precursor of cardiovascular disease and type 2 diabetes mellitus. Circulation 2005, 112, 3066–3072. [Google Scholar] [CrossRef] [PubMed]
- Gami, A.S.; Hodge, D.O.; Herges, R.M.; Olson, E.J.; Nykodym, J.; Kara, T.; Somers, V.K. Apnea obstructiva del sueño, obesidad y riesgo de fibrilación auricular incidente. J. Am. Coll. Cardiol. 2007, 49, 565–571. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mottillo, S.; Filion, K.B.; Genest, J.; Joseph, L.; Pilote, L.; Poirier, P.; Rinfret, S.; Schiffrin, E.L.; Eisenberg, M.J. The metabolic syndrome and cardiovascular risk: A systematic review and meta-analysis. J. Am. Coll. Cardiol. 2010, 56, 1113–1132. [Google Scholar] [CrossRef] [Green Version]
- Miele, C.H.; Schwartz, A.R.; Gilman, R.H.; Pham, L.; Wise, R.A.; Davila-Roman, V.G.; Jun, J.C.; Polotsky, V.Y.; Miranda, J.J.; Leon-Velarde, F.; et al. Increased Cardiometabolic Risk and Worsening Hypoxemia at High Altitude. High Alt. Med. Biol. 2016, 17, 93–100. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pitsavos, C.; Panagiotakos, D.; Weinem, M.; Stefanadis, C. Diet, exercise and the metabolic syndrome. Rev. Diabet. Stud. RDS 2006, 3, 118–126. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sun, K.; Liu, J.; Ning, G. Active smoking and risk of metabolic syndrome: A meta-analysis of prospective studies. PLoS ONE 2012, 7, e47791. [Google Scholar] [CrossRef] [Green Version]
- Sherpa, L.Y.; Stigum, H.; Chongsuvivatwong, V.; Nafstad, P.; Bjertness, E. Prevalence of metabolic syndrome and common metabolic components in high altitude farmers and herdsmen at 3700 m in Tibet. High Alt. Med. Biol. 2013, 14, 37–44. [Google Scholar] [CrossRef]
- Athyros, V.G.; Ganotakis, E.S.; Elisaf, M.; Mikhailidis, D.P. The prevalence of the metabolic syndrome using the National Cholesterol Educational Program and International Diabetes Federation definitions. Curr. Med. Res. Opin. 2005, 21, 1157–1159. [Google Scholar] [CrossRef] [PubMed]
- Song, Q.B.; Zhao, Y.; Liu, Y.Q.; Zhang, J.; Xin, S.J.; Dong, G.H. Sex difference in the prevalence of metabolic syndrome and cardiovascular-related risk factors in urban adults from 33 communities of China: The CHPSNE study. Diabetes Vasc. Dis. Res. 2015, 12, 189–198. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zeng, H.; Lin, H.; Liu, W.; Wang, J.; Wang, L.; Zheng, C.; Shu, W. Prevalence of metabolic syndrome among adults with liver function injury in rural area of Southwest China: A cross-sectional study. Sci. Rep. 2017, 7, 5518. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mazidi, M.; Toth, P.P.; Banach, M. C-reactive Protein Is Associated With Prevalence of the Metabolic Syndrome, Hypertension, and Diabetes Mellitus in US Adults. Angiology 2018, 69, 438–442. [Google Scholar] [CrossRef]
- Elder, S.J.; Lichtenstein, A.H.; Pittas, A.G.; Roberts, S.B.; Fuss, P.J.; Greenberg, A.S.; McCrory, M.A.; Bouchard, T.J.; Saltzman, E.; Neale, M.C. Genetic and environmental influences on factors associated with cardiovascular disease and the metabolic syndrome. J. Lipid Res. 2009, 50, 1917–1926. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gosadi, I.M. Assessment of the environmental and genetic factors influencing prevalence of metabolic syndrome in Saudi Arabia. Saudi Med. J. 2016, 37, 12–20. [Google Scholar] [CrossRef] [PubMed]
- Hruby, A.; Hu, F.B. The Epidemiology of Obesity: A Big Picture. Pharmacoeconomics 2015, 33, 673–689. [Google Scholar] [CrossRef] [PubMed]
- Castro, J.P.; El-Atat, F.A.; McFarlane, S.I.; Aneja, A.; Sowers, J.R. Cardiometabolic syndrome: Pathophysiology and treatment. Curr. Hypertens. Rep. 2003, 5, 393–401. [Google Scholar] [CrossRef]
- Woolcott, O.O.; Castillo, O.A.; Gutierrez, C.; Elashoff, R.M.; Stefanovski, D.; Bergman, R.N. Inverse association between diabetes and altitude: A cross-sectional study in the adult population of the United States. Obesity 2014, 22, 2080–2090. [Google Scholar] [CrossRef]
- Anderson, J.D.; Honigman, B. The effect of altitude-induced hypoxia on heart disease: Do acute, intermittent, and chronic exposures provide cardioprotection? High Alt. Med. Biol. 2011, 12, 45–55. [Google Scholar] [CrossRef]
- Hirschler, V. Cardiometabolic risk factors in native populations living at high altitudes. Int. J. Clin. Pract. 2016, 70, 113–118. [Google Scholar] [CrossRef]
- Alberti, K.G.; Eckel, R.H.; Grundy, S.M.; Zimmet, P.Z.; Cleeman, J.I.; Donato, K.A.; Fruchart, J.C.; James, W.P.T.; Loria, C.M.; Smith, S.C., Jr. Harmonizing the metabolic syndrome: A joint interim statement of the international diabetes federation task force on epidemiology and prevention; national heart, lung, and blood institute; American heart association; world heart federation; international atherosclerosis society; and international association for the study of obesity. Circulation 2009, 120, 1640–1645. [Google Scholar] [CrossRef] [Green Version]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. PLoS Med. 2009, 6, e1000100. [Google Scholar] [CrossRef] [PubMed]
- Huang, X.; Hu, Y.; Du, L.; Lin, X.; Wu, W.; Fan, L.; Li, L.; Zhong, X.; Gong, Q.; Gao, L.; et al. Metabolic syndrome in native populations living at high altitude: A cross-sectional survey in Derong, China. BMJ Open 2020, 10, e032840. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gou, Q.; Shi, R.; Zhang, X.; Meng, Q.; Li, X.; Rong, X.; Chen, X. The prevalence and risk factors of high-altitude pulmonary hypertension among native Tibetans in Sichuan Province, China. High Alt. Med. Biol. 2020, 21, 327–335. [Google Scholar] [CrossRef] [PubMed]
- Lin, B.Y.; Genden, K.; Shen, W.; Wu, P.S.; Yang, W.C.; Hung, H.F.; Fu, C.M.; Yang, K.C. The prevalence of obesity and metabolic syndrome in Tibetan immigrants living in high altitude areas in Ladakh, India. Obes. Res. Clin. Pract. 2018, 12, 365–371. [Google Scholar] [CrossRef] [PubMed]
- Hurtado-Arestegui, A.; Plata-Cornejo, R.; Cornejo, A.; Mas, G.; Carbajal, L.; Sharma, S.; Swenson, E.R.; Johnson, R.J.; Pando, J. Higher prevalence of unrecognized kidney disease at high altitude. J. Nephrol. 2018, 31, 263–269. [Google Scholar] [CrossRef]
- Herrera-Enriquez, K.; Narvaez-Guerra, O. Discordance of metabolic syndrome and abdominal obesity prevalence according to different criteria in Andean highlanders: A community-based study. Diabetes Metab. Syndr. 2017, 11, S359–S364. [Google Scholar] [CrossRef]
- Lopez-Pascual, A.; Arévalo, J.; Martínez, J.A.; González-Muniesa, P. Inverse association between metabolic syndrome and altitude: A cross-sectional study in an adult population of Ecuador. Front. Endocrinol. 2018, 9, 658. [Google Scholar] [CrossRef] [PubMed]
- De Ferrari, A.; Miranda, J.J.; Gilman, R.H.; Dávila-Román, V.G.; León-Velarde, F.; Rivera-Ch, M.; Huicho, L.; Bernabé-Ortiz, A.; Wise, R.A.; Checkley, W. Prevalence, clinical profile, iron status, and subject-specific traits for excessive erythrocytosis in andean adults living permanently at 3825 meters above sea level. Chest 2014, 146, 1327–1336. [Google Scholar] [CrossRef] [Green Version]
- Salazar-Lugo, R.; Barahona, A.; Tarupi, Y.; Victoria, C.; Santamaría, M.; Oleas, M. Factores bioquímicos y nutricionales asociados a la viscosidad sanguínea en adultos de la sierra urbana (Imbabura), Ecuador [Biochemical and nutritional factors associated with blood viscosity in adults living in a mountain chain, (Imbabura), Ecuador]. Investig. Clin. 2016, 57, 293–304. (In Spanish) [Google Scholar]
- National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation 2002, 106, 3143–3421. [Google Scholar] [CrossRef]
- Alberti, K.G.; Zimmet, P.Z. Definition, diagnosis and classification of diabetes mellitus and its complications, part 1: Diagnosis and classification of diabetes mellitus provisional report of a WHO consultation. Diabet. Med. 1998, 15, 539–553. [Google Scholar] [CrossRef]
- Alberti, K.G.; Zimmet, P.; Shaw, J. IDF Epidemiology Task Force Consensus Group. The metabolic syndrome: A new worldwide definition. Lancet 2005, 366, 1059–1062. [Google Scholar] [CrossRef]
- Norboo, T.; Stobdan, T.; Tsering, N.; Angchuk, N.; Tsering, P.; Ahmed, I.; Chorol, T.; Sharma, V.K.; Reddy, P.; Singh, S.B.; et al. Prevalence of hypertension at high altitude: Cross-sectional survey in Ladakh, Northern India 2007–2011. BMJ Open 2015, 5, e007026. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Woolcott, O.O.; Gutierrez, C.; Castillo, O.A.; Elashoff, R.M.; Stefanovski, D.; Bergman, R.N. Inverse association between altitude and obesity: A prevalence study among andean and low-altitude adult individuals of Peru. Obesity 2016, 24, 929–937. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- US Department of Health and Human Services. Appendix 1. Translating scientific evidence about total amount and intensity of physical activity into guidelines. In 2008 Physical Activity Guidelines for Americans; ODPHP Publication No. U0036; USA Department of Health and Human Services, Office of Disease Prevention and Health Promotion: Rockville, MD, USA, 2008. Available online: https://health.gov/paguidelines/pdf/paguide.pdf (accessed on 20 January 2022).
- Bigham, A.; Bauchet, M.; Pinto, D.; Mao, X.; Akey, J.M.; Mei, R.; Scherer, S.W.; Julian, C.G.; Wilson, M.J.; López Herráez, D.; et al. Identifying signatures of natural selection in Tibetan and Andean populations using dense genome scan data. PLoS Genet. 2010, 6, e1001116. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, J.; Sun, W.; Wells, G.A.; Li, Z.; Li, T.; Wu, J.; Zhang, Y.; Liu, Y.; Li, L.; Yu, Y.; et al. Differences in prevalence of hypertension and associated risk factors in urban and rural residents of the northeastern region of the People’s Republic of China: A cross-sectional study. PLoS ONE 2018, 13, e0195340. [Google Scholar] [CrossRef] [Green Version]

| No | Item | Huang et al. [24] | Lopez-Pascual et al. [29] | Sherpa et al. [10] | Lin et al. [26] | Hurtado-Arestegui et al. [27] | De Ferrari et al. [30] | Miele et al. [7] | Gou et al. [25] | Herrera-Enríquez, Narváez-Guerra [28] | Salazar-Lugo et al. [31] |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Define the source of information (survey, record review). | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 2 | List inclusion and exclusion criteria for exposed subjects or refer to previous publications | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 3 | Indicate the time period used to identify patients | Yes | No | Yes | Yes | No | No | No | Yes | Yes | No |
| 4 | Indicate whether subjects were consecutive or not, if not population based. | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 5 | Indicate whether the evaluators of the subjective components of the study were masked to the participants’ status | Yes | No | Yes | No | No | No | No | Yes | No | No |
| 6 | Describe any evaluations performed for quality assurance purposes (e.g., testing/repeat of primary outcome measurements). | No | No | No | No | Yes | No | No | No | No | No |
| 7 | Explain any exclusions of patients from analyses. | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No |
| 8 | Describe how confounders were assessed and/or controlled for. | Yes | Unclear | Yes | No | No | Unclear | No | No | No | No |
| 9 | If applicable, explain how missing data were handled in the analysis. | No | No | Yes | No | No | No | No | No | No | No |
| 10 | Summarize patient response rates and completeness of data collection. | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | yes | Yes |
| 11 | Clarify what follow-up was expected, if any, and the percentage of patients for whom incomplete data or follow-up was obtained | No | No | No | No | No | No | No | No | No | No |
| N° | Author(s) | Year | Title | Journal |
|---|---|---|---|---|
| 1 | Huang et al. [24]. | 2020 | Metabolic syndrome in native populations living at high altitude: a cross-sectional survey in Derong, China. | BMJ Open. |
| 2 | Lopez-Pascual et al. [29]. | 2018 | Inverse Association Between Metabolic Syndrome and Altitude: A Cross-Sectional Study in an Adult Population of Ecuador | Frontiers in Endocrinology, Clinical Diabetes. |
| 3 | Sherpa et al. [10]. | 2013 | Prevalence of metabolic syndrome and common metabolic components in high-altitude farmers and herdsmen at 3700 m in Tibet. | High Altitude & Medicine Biology. |
| 4 | Lin et al. [26]. | 2018 | The prevalence of obesity and metabolic syndrome in Tibetan immigrants living in high altitude areas in Ladakh, India. | Obesity Research & Clinical Practrice. |
| 5 | Hurtado-Arestegui et al. [27] | 2018 | Higher prevalence of unrecognized kidney disease at high altitude. | Journal of Nephrology. |
| 6 | De Ferrari et al. [30] | 2014 | Prevalence, clinical profile, iron status, and subject-specific traits for excessive erythrocytosis in Andean adults living permanently at 3825 m above sea level. | Chest Journal |
| 7 | Miele et al. [7] | 2016 | Increased Cardiometabolic Risk and Worsening Hypoxemia at High Altitude. | High Altitude & Medicine Biology. |
| 8 | Gou et al. [25] | 2020 | The Prevalence and Risk Factors of High-Altitude Pulmonary Hypertension Among Native Tibetans in Sichuan Province, China. | High Altitude & Medicine Biology. |
| 9 | Herrera-Enríquez, Narváez-Guerra [28] | 2017 | Discordance of metabolic syndrome and abdominal obesity prevalence according to different criteria in Andean highlanders: A community-based study. | Diabetes & Metabolic Syndrome: Clinical Research & Reviews |
| 10 | Salazar-Lugo et al. [31] | 2016 | Factores bioquímicos y nutricionales asociados a la viscosidad sanguínea en adultos de la sierra urbana (Imbabura), Ecuador. | Investigación Clínica |
| N° | Author(s) | Samples | Ages (Year) | Altitude (m) | City (Country) |
|---|---|---|---|---|---|
| 1 | Huang et al. [24] | n = 5053 M = 2221 W = 2832 | 18–70 | 2060–3820 | Derong (China) |
| 2 | Lopez-Pascual et al. [29] | n = 260 M = 168 W = 92 | 27–48 | 2758–2787 | Guayaquil, Triunfo y Riobamba (Ecuador) |
| 3 | Sherpa et al. [10] | n = 692 M = 317 W = 375 | 30–80 | 3700 | Lhunzhub y Qushu, Region del Tíbet (China) |
| 4 | Lin et al. [26] | n = 149 M = 47 W = 102 | 40–73 | 3505 | Ladakh (India) |
| 5 | Hurtado-Arestegui et al. [27] | n = 293 M = 145 W = 148 | 40–60 | 3640–4500 | La Paz (Bolivia) |
| 6 | De Ferrari et al. [30] | n = 1065 M = 518 W = 547 | 42–67 | 3825 | Puno, Perú |
| 7 | Miele et al. [7] | n = 1065 M = 518 W = 547 | 42–67 | 3825 | Puno, Perú |
| 8 | Gou et al. [25] | n = 1129 M = 440 W = 689 | 32–60 | 3200 | Sichuan, China |
| 9 | Herrera-Enríquez, Narváez-Guerra [28] | n = 237 M = 110 W = 127 | 48–82 | 3635 | Chivay, Perú |
| 10 | Salazar-Lugo et al. [31] | n = 237 M = 128 W = 109 | 20–60 | 2200 | Imbabura (Ecuador) |
| Country/City | Altitude (masl) |
|---|---|
| China | |
| Derong | 2060 |
| Tibet | 4900 |
| Sichuan | 3200 |
| Ecuador | |
| Riobamba | 2754 |
| Quito | 2850 |
| Imbabura | 2500 |
| India | |
| Ladakh | 3505 |
| Bolivia | |
| La Paz | 3640 |
| Perú | |
| Puno | 3825 |
| Chivay | 3635 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Villegas-Abrill, C.B.; Vidal-Espinoza, R.; Gomez-Campos, R.; Ibañez-Quispe, V.; Mendoza-Mollocondo, C.; Cuentas-Yupanqui, S.R.; Fuentes-López, J.; Urra-Albornoz, C.; Cossio-Bolaños, M. Diagnostic Criteria for Metabolic Syndrome in High-Altitude Regions: A Systematic Review. Medicina 2022, 58, 451. https://doi.org/10.3390/medicina58030451
Villegas-Abrill CB, Vidal-Espinoza R, Gomez-Campos R, Ibañez-Quispe V, Mendoza-Mollocondo C, Cuentas-Yupanqui SR, Fuentes-López J, Urra-Albornoz C, Cossio-Bolaños M. Diagnostic Criteria for Metabolic Syndrome in High-Altitude Regions: A Systematic Review. Medicina. 2022; 58(3):451. https://doi.org/10.3390/medicina58030451
Chicago/Turabian StyleVillegas-Abrill, Claudia Beatriz, Rubén Vidal-Espinoza, Rossana Gomez-Campos, Vladimiro Ibañez-Quispe, Charles Mendoza-Mollocondo, Sara Ruth Cuentas-Yupanqui, José Fuentes-López, Camilo Urra-Albornoz, and Marco Cossio-Bolaños. 2022. "Diagnostic Criteria for Metabolic Syndrome in High-Altitude Regions: A Systematic Review" Medicina 58, no. 3: 451. https://doi.org/10.3390/medicina58030451
APA StyleVillegas-Abrill, C. B., Vidal-Espinoza, R., Gomez-Campos, R., Ibañez-Quispe, V., Mendoza-Mollocondo, C., Cuentas-Yupanqui, S. R., Fuentes-López, J., Urra-Albornoz, C., & Cossio-Bolaños, M. (2022). Diagnostic Criteria for Metabolic Syndrome in High-Altitude Regions: A Systematic Review. Medicina, 58(3), 451. https://doi.org/10.3390/medicina58030451






