Is Device Removal Necessary after Fixed-Angle Locking Plate Osteosynthesis of Proximal Humerus Fractures?
Abstract
1. Introduction
2. Materials and Methods
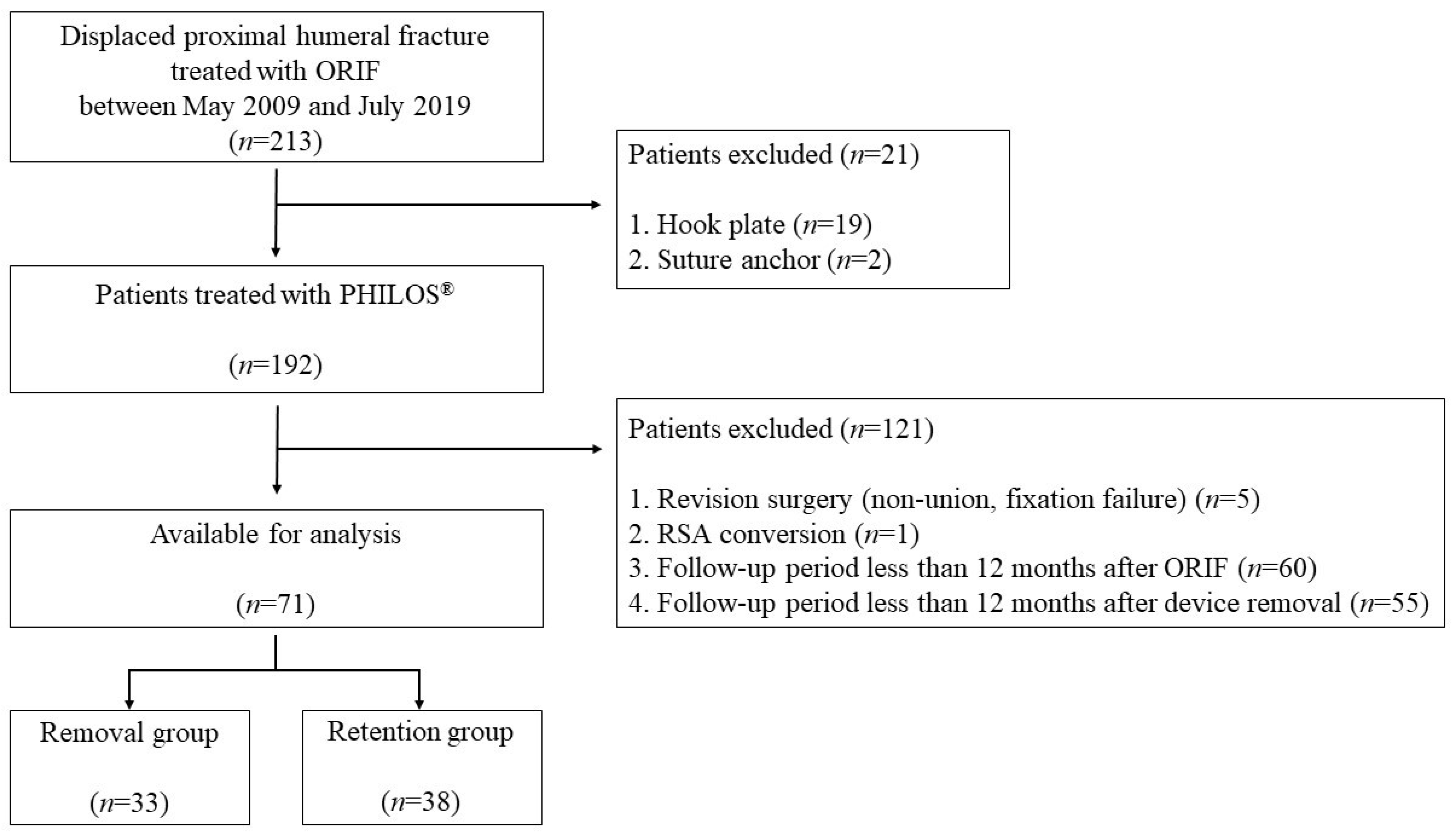
2.1. Study Design and Participants
2.2. Surgical Procedure
2.3. Assessment of Clinical Outcomes
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Roux, A.; Decroocq, L.; El Batti, S.; Bonnevialle, N.; Moineau, G.; Trojani, C.; Boileau, P.; de Peretti, F. Epidemiology of proximal humerus fractures managed in a trauma center. Orthop. Traumatol. Surg. Res. 2012, 98, 715–719. [Google Scholar] [CrossRef]
- Hirschmann, M.T.; Quarz, V.; Audigé, L.; Ludin, D.; Messmer, P.; Regazzoni, P.; Gross, T. Internal fixation of unstable proximal humerus fractures with an anatomically preshaped interlocking plate: A clinical and radiologic evaluation. J. Trauma 2007, 63, 1314–1323. [Google Scholar] [CrossRef] [PubMed]
- Min, Y.K.; Lee, S.J.; Gwak, H.C.; Kang, S.W.; Suh, K.T. Clinical and Radiologic Results Comparing the Periarticular Proximal Humerus Locking Plate and Polarus Nail for Displaced Proximal Humerus Fractures. Clin. Shoulder Elbow. 2017, 20, 208–216. [Google Scholar] [CrossRef][Green Version]
- Acklin, Y.P.; Stoffel, K.; Sommer, C. A prospective analysis of the functional and radiological outcomes of minimally invasive plating in proximal humerus fractures. Injury 2013, 44, 456–460. [Google Scholar] [CrossRef] [PubMed]
- Charalambous, C.P.; Siddique, I.; Valluripalli, K.; Kovacevic, M.; Panose, P.; Srinivasan, M.; Marynissen, H. Proximal humeral internal locking system (PHILOS) for the treatment of proximal humeral fractures. Arch. Orthop. Trauma Surg. 2007, 127, 205–210. [Google Scholar] [CrossRef]
- Fankhauser, F.; Boldin, C.; Schippinger, G.; Haunschmid, C.; Szyszkowitz, R. A new locking plate for unstable fractures of the proximal humerus. Clin. Orthop. Relat. Res. 2005, 430, 176–181. [Google Scholar] [CrossRef]
- Jost, B.; Spross, C.; Grehn, H.; Gerber, C. Locking plate fixation of fractures of the proximal humerus: Analysis of complications, revision strategies and outcome. J. Shoulder Elbow Surg. 2013, 22, 542–549. [Google Scholar] [CrossRef]
- Kim, J.Y.; Lee, J.; Kim, S.H. Comparison between MIPO and the deltopectoral approach with allogenous fibular bone graft in proximal humeral fractures. Clin. Shoulder Elb. 2020, 23, 136–143. [Google Scholar] [CrossRef]
- Lovald, S.; Mercer, D.; Hanson, J.; Cowgill, I.; Erdman, M.; Robinson, P.; Diamond, B. Complications and hardware removal after open reduction and internal fixation of humeral fractures. J. Trauma 2011, 70, 1273–1277; discussion 1277–1278. [Google Scholar] [CrossRef]
- Kirchhoff, C.; Braunstein, V.; Kirchhoff, S.; Sprecher, C.M.; Ockert, B.; Fischer, F.; Leidel, B.A.; Biberthaler, P. Outcome analysis following removal of locking plate fixation of the proximal humerus. BMC Musculoskelet. Disord. 2008, 9, 138. [Google Scholar] [CrossRef]
- Hirschmann, M.T.; Fallegger, B.; Amsler, F.; Regazzoni, P.; Gross, T. Clinical longer-term results after internal fixation of proximal humerus fractures with a locking compression plate (PHILOS). J. Orthop. Trauma 2011, 25, 286–293. [Google Scholar] [CrossRef] [PubMed]
- Acklin, Y.P.; Michelitsch, C.; Sommer, C. Elective implant removal in symptomatic patients after internal fixation of proximal humerus fractures improves clinical outcome. BMC Musculoskelet. Disord. 2016, 17, 119. [Google Scholar] [CrossRef] [PubMed]
- Dimitriou, D.; Waldmann, S.; Antoniadis, A.; Liebhauser, M.; Helmy, N.; Riede, U. Early locking plate removal following open reduction and internal fixation of proximal humeral fractures could prevent secondary implant-related complications. J. Orthop. 2020, 17, 106–109. [Google Scholar] [CrossRef] [PubMed]
- Holloway, G.B.; Schenk, T.; Williams, G.R.; Ramsey, M.L.; Iannotti, J.P. Arthroscopic capsular release for the treatment of refractory postoperative or post-fracture shoulder stiffness. J. Bone Jt. Surg. 2001, 83, 1682–1687. [Google Scholar] [CrossRef] [PubMed]
- Lee, W.Y.; Shin, H.D.; Kim, K.C.; Cha, S.M.; Jeon, Y.S.; Kim, D.H. Open Reduction and Stable Internal Fixation Using a 3.5-mm Locking Hook Plate for Isolated Fractures of the Greater Tuberosity of the Humerus: A 2-Year Follow-up Study Using an Innovative Fixation Method. Clin. Orthop. Surg. 2021, 13, 293–300. [Google Scholar] [CrossRef] [PubMed]
- Busam, M.L.; Esther, R.J.; Obremskey, W.T. Hardware removal: Indications and expectations. J. Am. Acad. Orthop. Surg. 2006, 14, 113–120. [Google Scholar] [CrossRef] [PubMed]
- Jain, R.; Sharma, D.; Mahajan, P.; Garg, A. Patient’s perspective of implant removal in orthopaedic trauma cases in Central India. Clin. Orthop. Surg. 2020, 12, e22. [Google Scholar]
- Reith, G.; Schmitz-Greven, V.; Hensel, K.O.; Schneider, M.M.; Tinschmann, T.; Bouillon, B.; Probst, C. Metal implant removal: Benefits and drawbacks--a patient survey. BMC Surg. 2015, 15, 96. [Google Scholar] [CrossRef]
- Vos, D.I.; Verhofstad, M.H. Indications for implant removal after fracture healing: A review of the literature. Eur. J. Trauma Emerg. Surg. 2013, 39, 327–337. [Google Scholar] [CrossRef]
- Maqdes, A.; Levy, B.; Klouche, S.; Hardy, P. The feasibility and results of an arthroscopic removal of humeral locking plates and glenohumeral arthrolysis after proximal humeral fractures. Knee Surg. Sports Traumatol. Arthrosc. 2014, 22, 456–461. [Google Scholar] [CrossRef]
- Egol, K.A.; Ong, C.C.; Walsh, M.; Jazrawi, L.M.; Tejwani, N.C.; Zuckerman, J.D. Early complications in proximal humerus fractures (OTA Types 11) treated with locked plates. J. Orthop. Trauma 2008, 22, 159–164. [Google Scholar] [CrossRef] [PubMed]
- Bhatia, D.N. Arthroscopic Removal of Proximal Humerus Plates in Chronic Post-traumatic Shoulder Stiffness. Arthrosc. Tech. 2017, 6, e375–e381. [Google Scholar] [CrossRef] [PubMed]
- Katthagen, J.C.; Hennecke, D.; Jensen, G.; Ellwein, A.; Voigt, C.; Lill, H. Arthroscopy after locked plating of proximal humeral fractures: Implant removal, capsular release, and intra-articular findings. Arthroscopy 2014, 30, 1061–1067. [Google Scholar] [CrossRef] [PubMed]
| Removal Group (n = 33) | Retention Group (n = 38) | p Value | |
|---|---|---|---|
| Age, year | 55.2 ± 12.0 | 71.6 ± 9.5 | <0.001 * |
| Sex, male/female, n | 12/21 | 5/33 | 0.022 * |
| Involved side, right/left, n | 19/14 | 26/12 | 0.344 |
| Injury mechanism | 0.053 | ||
| Low-energy trauma | 18 | 12 | |
| High-energy trauma | 15 | 29 | |
| Diabetes mellitus, yes/no, n | 5/28 | 13/25 | 0.066 |
| Time from initial injury to surgery, day | 4.8 ± 3.5 | 5.4 ± 4.8 | 0.567 |
| Fracture Classification (Neer) | 0.619 | ||
| 2-part | 21 | 19 | |
| 3-part | 9 | 18 | |
| 4-part | 3 | 1 | |
| Type of operation | 0.068 | ||
| Plate + tension suture | 25 | 22 | |
| Plate + tension suture + allograft | 3 | 12 | |
| Plate only | 5 | 4 | |
| Operative time (ORIF), minute | 98.1 ± 33.3 | 102.5 ± 45.2 | 0.650 |
| Time after ORIF to implant removal, month | 10.4 ± 6.7 | ||
| Total follow-up periods, month | 39.9 ± 20.3 | 22.4 ± 14.9 | <0.001 * |
| Removal Group (n = 33) | Retention Group (n = 38) | p-Value | |
|---|---|---|---|
| Finial Clinical scores | |||
| VAS pain score | 0.8 ± 1.5 | 1.2 ± 1.1 | 0.283 |
| UCLA score | 32.6 ± 3.2 | 28.7 ± 3.7 | <0.001 * |
| ASES score | 92.5 ± 9.8 | 80.3 ± 10.6 | <0.001* |
| Final Range of motion | |||
| Forward flexion, ° | 159.7° ± 18.5° | 139.6° ± 22.9° | <0.001 * |
| Abduction, ° | 151.1° ± 30.7° | 124.7° ± 24.7° | <0.001 * |
| External rotation, ° | 62.4° ± 13.2° | 48.4° ± 14.8° | <0.001 * |
| Internal rotation | 10.0 ± 2.4 | 13.3 ± 2.6 | <0.001 * |
| Preoperative | Postoperative | p-Value | |
|---|---|---|---|
| Clinical scores | |||
| VAS pain score | 2.8 ± 2.0 | 0.8 ± 1.5 | <0.001 * |
| UCLA score | 23.2 ± 6.0 | 32.6 ± 3.2 | <0.001 * |
| ASES score | 62.6 ± 16.7 | 92.5 ± 9.4 | <0.001 * |
| Range of motion | <0.001 * | ||
| Forward flexion, ° | 126.7° ± 31.0° | 159.7° ± 18.5° | <0.001 * |
| Abduction, ° | 114.7° ± 31.6° | 151.1° ± 30.7° | <0.001 * |
| External rotation, ° | 35.3° ± 17.5° | 62.4° ± 13.2° | <0.001 * |
| Internal rotation | 14.1 ± 3.3 | 10.0 ± 2.4 | <0.001 * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, B.-S.; Kim, D.-H.; Choi, J.-H.; Choi, B.-C.; Cho, C.-H. Is Device Removal Necessary after Fixed-Angle Locking Plate Osteosynthesis of Proximal Humerus Fractures? Medicina 2022, 58, 382. https://doi.org/10.3390/medicina58030382
Kim B-S, Kim D-H, Choi J-H, Choi B-C, Cho C-H. Is Device Removal Necessary after Fixed-Angle Locking Plate Osteosynthesis of Proximal Humerus Fractures? Medicina. 2022; 58(3):382. https://doi.org/10.3390/medicina58030382
Chicago/Turabian StyleKim, Beom-Soo, Du-Han Kim, Jung-Hoon Choi, Byung-Chan Choi, and Chul-Hyun Cho. 2022. "Is Device Removal Necessary after Fixed-Angle Locking Plate Osteosynthesis of Proximal Humerus Fractures?" Medicina 58, no. 3: 382. https://doi.org/10.3390/medicina58030382
APA StyleKim, B.-S., Kim, D.-H., Choi, J.-H., Choi, B.-C., & Cho, C.-H. (2022). Is Device Removal Necessary after Fixed-Angle Locking Plate Osteosynthesis of Proximal Humerus Fractures? Medicina, 58(3), 382. https://doi.org/10.3390/medicina58030382








