Clinical and Prognostic Values of TRPM7 in Colon and Rectal Cancers
Abstract
1. Introduction
2. Materials and Methods
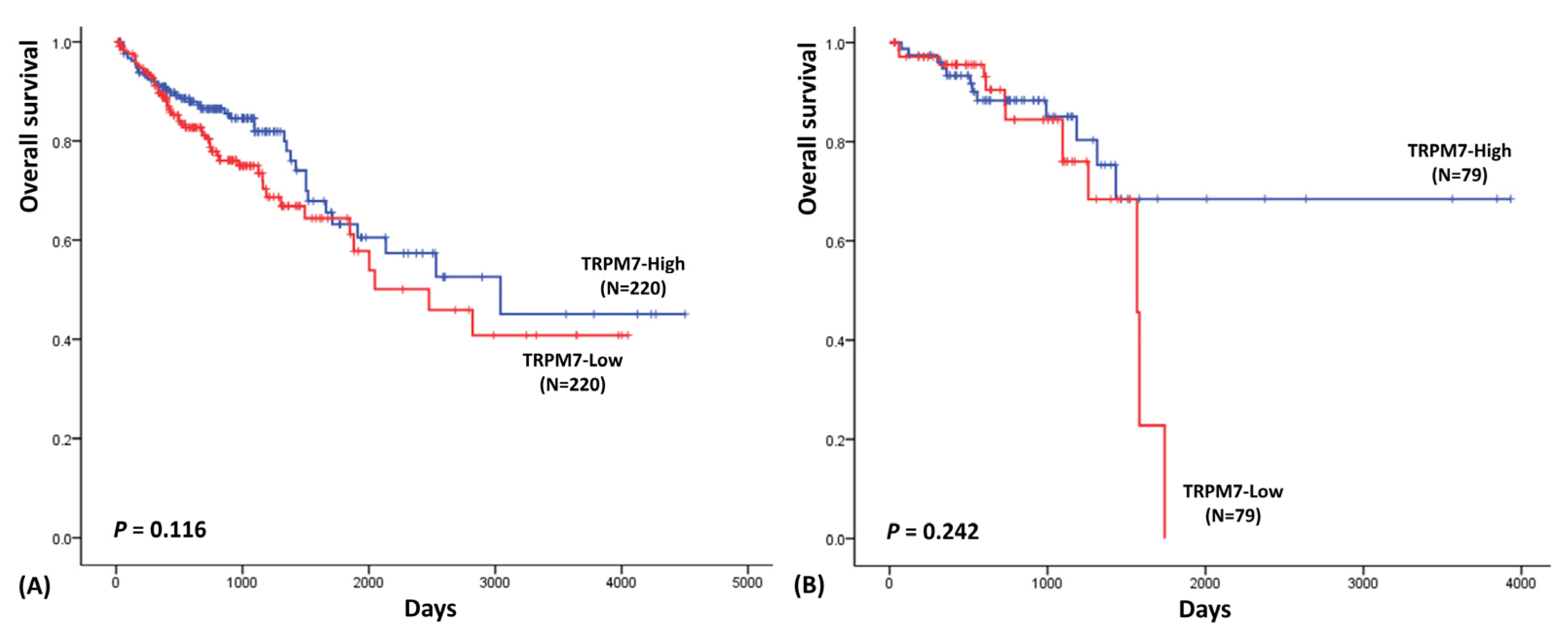
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Conlin, A.; Smith, G.; Carey, F.A.; Wolf, C.R.; Steele, R.J. The prognostic significance of K-ras, p53, and APC mutations in colorectal carcinoma. Gut 2005, 54, 1283–1286. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.; Lee, J.; Park, W.; Kim, S. Bioinformatic exploration for prognostic significance of sphingolipid metabolism-related genes in invasive ductal carcinoma using the cancer genome atlas cohort. Int. J. Gen. Med. 2021, 14, 4423. [Google Scholar] [CrossRef] [PubMed]
- Trapani, V.; Arduini, D.; Cittadini, A.; Wolf, F.I. From magnesium to magnesium transporters in cancer: TRPM7, a novel signature in tumour development. Magnes Res. 2013, 26, 149–155. [Google Scholar] [CrossRef]
- Park, H.S.; Hong, C.; Kim, B.J.; So, I. The pathophysiologic roles of TRPM7 channel. Korean J. Physiol. Pharmacol. 2014, 18, 15–23. [Google Scholar] [CrossRef] [PubMed]
- Sun, Y.; Selvaraj, S.; Varma, A.; Derry, S.; Sahmoun, A.E.; Singh, B.B. Increase in serum Ca2+/Mg2+ ratio promotes proliferation of prostate cancer cells by activating TRPM7 channels. J. Biol. Chem. 2013, 288, 255–263. [Google Scholar] [CrossRef] [PubMed]
- Cordier, C.; Prevarskaya, N.; Lehen’kyi, V. TRPM7 ion channel: Oncogenic roles and therapeutic potential in breast cancer. Cancers 2021, 13, 6322. [Google Scholar] [CrossRef] [PubMed]
- Yang, D.; Kim, J. Emerging role of transient receptor potential (TRP) channels in cancer progression. BMB Rep. 2020, 53, 125–132. [Google Scholar] [CrossRef] [PubMed]
- Clapham, D.E. TRP channels as cellular sensors. Nature 2003, 426, 517–524. [Google Scholar] [CrossRef] [PubMed]
- Jiang, J.; Li, M.; Yue, L. Potentiation of TRPM7 Inward Currents by Protons. J. Gen. Physiol. 2005, 126, 137–150. [Google Scholar] [CrossRef] [PubMed]
- Nadler, M.J.S.; Hermosura, M.C.; Inabe, K.; Perraud, A.-L.; Zhu, Q.; Stokes, A.J.; Kurosaki, T.; Kinet, J.-P.; Penner, R.; Scharenberg, A.M.; et al. LTRPC7 is a Mg·ATP-regulated divalent cation channel required for cell viability. Nature 2001, 411, 590–595. [Google Scholar] [CrossRef] [PubMed]
- Calik, M.; Calik, I.; Artas, G.; Ozercan, I.H. Prognostic value of TRPM7 expression and factor XIIIa-expressing tumor-associated macrophages in gastric cancer. Gastroenterol. Res. Pract. 2021, 2021, 7249726. [Google Scholar] [CrossRef]
- Chen, L.; Cao, R.; Wang, G.; Yuan, L.; Qian, G.; Guo, Z.; Wu, C.-L.; Wang, X.; Xiao, Y. Downregulation of TRPM7 suppressed migration and invasion by regulating epithelial–mesenchymal transition in prostate cancer cells. Med. Oncol. 2017, 34, 127. [Google Scholar] [CrossRef]
- Yee, N.S.; Kazi, A.A.; Li, Q.; Yang, Z.; Berg, A.; Yee, R.K. Aberrant over-expression of TRPM7 ion channels in pancreatic cancer: Required for cancer cell invasion and implicated in tumor growth and metastasis. Biol. Open 2015, 4, 507–514. [Google Scholar] [CrossRef]
- Pugliese, D.; Armuzzi, A.; Castri, F.; Benvenuto, R.; Mangoni, A.; Guidi, L.; Gasbarrini, A.; Rapaccini, G.L.; Wolf, F.I.; Trapani, V. TRPM7 is overexpressed in human IBD-related and sporadic colorectal cancer and correlates with tumor grade. Dig. Liver. Dis. 2020, 52, 1188–1194. [Google Scholar] [CrossRef]
- Su, F.; Wang, B.-F.; Zhang, T.; Hou, X.-M.; Feng, M.-H. TRPM7 deficiency suppresses cell proliferation, migration, and invasion in human colorectal cancer via regulation of epithelial-mesenchymal transition. Cancer Biomark. 2019, 26, 451–460. [Google Scholar] [CrossRef]
- Nakayama, M.; Oshima, M. Mutant p53 in colon cancer. J. Mol. Cell Biol. 2019, 11, 267–276. [Google Scholar] [CrossRef]
| TRPM7 (Rectal Cancer) | TRPM7 (Colon Cancer) | |||||
|---|---|---|---|---|---|---|
| High (N,%) | Low (N,%) | p-Value | High (N,%) | Low (N,%) | p-Value | |
| Age | ||||||
| <60 | 35 (71.4%) | 14 (28.6%) | <0.001 | 89 (52.4%) | 81 (47.6%) | 0.433 |
| ≥60 | 43 (39.8%) | 65 (60.1%) | 131 (48.5%) | 139 (51.5%) | ||
| Gender | ||||||
| Female | 36 (50.7%) | 35 (49.3%) | 0.816 | 103 (50%) | 103 (50%) | 1.000 |
| Male | 42 (48.8%) | 44 (51.2%) | 117 (50%) | 117 (50%) | ||
| Lymphatic invasion | ||||||
| No | 45 (54.9%) | 37 (45.1%) | 0.092 | 118 (48.4%) | 126 (51.6%) | 0.751 |
| Yes | 23 (41.7%) | 34 (60.7%) | 76 (50%) | 76 (50%) | ||
| CEA (ng/mL) | ||||||
| ≤5 | 31 (50.8%) | 30 (49.2%) | 0.934 | 98 (51.9%) | 91 (48.1%) | 0.372 |
| >5 | 22 (50%) | 22 (50%) | 42 (46.2%) | 49 (53.8%) | ||
| Venous invasion | ||||||
| No | 52 (51%) | 50 (49%) | 0.407 | 142 (48.8%) | 149 (51.2%) | 0.524 |
| Yes | 15 (42.9%) | 20 (57.1%) | 40 (44.4%) | 50 (55.6%) | ||
| Pathologic stage | ||||||
| stage I | 10 (33.3%) | 20 (66.7%) | 0.260 | 42 (59.2%) | 29 (40.8%) | 0.384 |
| stage II | 23 (50%) | 23 (50%) | 83 (48.5%) | 88 (51.5%) | ||
| stage III | 27 (56.3%) | 21 (43.7%) | 59 (46.8%) | 67 (53.2%) | ||
| stage IV | 11 (45.8%) | 13 (54.2%) | 31 (50.8%) | 30 (49.2%) | ||
| M stage | ||||||
| M0 | 56 (47.5%) | 62 (52.5%) | 0.464 | 159 (48.9%) | 166 (51.1%) | 0.785 |
| M1 | 9 (39.1%) | 14 (60.9%) | 31 (50.8%) | 30 (49.2%) | ||
| N stage | ||||||
| N0 | 35 (44.3%) | 44 (55.7%) | 0.342 | 131 (50.8%) | 127 (49.2%) | 0.283 |
| N1 | 22 (51.2%) | 21 (48.8%) | 56 (53.8%) | 48 (46.2%) | ||
| N2 | 19 (59.4%) | 13 (40.6%) | 33 (42.3%) | 45 (57.7%) | ||
| T stage | ||||||
| T1 | 1 (11.1%) | 8 (88.9%) | 0.093 | 4 (36.4%) | 7 (63.6%) | 0.072 |
| T2 | 13 (46.4%) | 15 (53.6%) | 47 (63.5%) | 27 (36.5%) | ||
| T3 | 55 (51.9%) | 51 (48.1%) | 144 (47.5%) | 159 (52.5%) | ||
| T4 | 8 (61.5%) | 5 (38.5%) | 25 (49%) | 26 (51%) | ||
| TRPM7 | APC | KRAS | p53 | Age | CEA | ||
|---|---|---|---|---|---|---|---|
| TRPM7 | R | 1 | 0.534 | 0.319 | −0.240 | −0.239 | −0.026 |
| p | <0.001 | <0.001 | 0.002 | 0.003 | 0.795 | ||
| APC | R | 0.534 | 1 | 0.261 | −0.148 | −0.222 | −0.013 |
| p | <0.001 | 0.001 | 0.064 | 0.005 | 0.893 | ||
| KRAS | R | 0.319 | 0.261 | 1 | −0.085 | 0.014 | −0.007 |
| p | <0.001 | 0.001 | 0.290 | 0.857 | 0.942 | ||
| p53 | R | −0.240 | −0.148 | −0.085 | 1 | 0.078 | −0.104 |
| p | 0.002 | 0.064 | 0.290 | 0.330 | 0.290 | ||
| Age | R | −0.239 | −0.222 | 0.014 | 0.078 | 1 | 0.008 |
| p | 0.003 | 0.005 | 0.857 | 0.330 | 0.932 | ||
| CEA | R | −0.026 | −0.013 | −0.007 | −0.104 | 0.008 | 1 |
| p | 0.795 | 0.893 | 0.942 | 0.290 | 0.932 | ||
| TRPM7 | APC | KRAS | p53 | Age | CEA | ||
|---|---|---|---|---|---|---|---|
| TRPM7 | R | 1 | 0.058 | −0.034 | 0.043 | −0.01 | 0.067 |
| p | 0.224 | 0.554 | 0.364 | 0.832 | 0.265 | ||
| APC | R | 0.058 | 1 | −0.031 | 0.017 | 0.002 | 0.009 |
| p | 0.224 | 0.593 | 0.727 | 0.965 | 0.882 | ||
| KRAS | R | −0.034 | −0.031 | 1 | −0.111 | −0.018 | −0.115 |
| p | 0.554 | 0.593 | 0.052 | 0.748 | 0.096 | ||
| p53 | R | 0.043 | 0.017 | −0.111 | 1 | 0.052 | 0.016 |
| p | 0.364 | 0.727 | 0.052 | 0.281 | 0.793 | ||
| Age | R | −0.01 | 0.002 | −0.018 | 0.052 | 1 | 0.003 |
| p | 0.832 | 0.965 | 0.748 | 0.281 | 0.965 | ||
| CEA | R | 0.067 | 0.009 | −0.115 | 0.016 | 0.003 | 1 |
| p | 0.265 | 0.882 | 0.096 | 0.793 | 0.965 | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, J.-C.; Bae, A.-N.; Lee, H.-J.; Lee, J.-H. Clinical and Prognostic Values of TRPM7 in Colon and Rectal Cancers. Medicina 2022, 58, 1582. https://doi.org/10.3390/medicina58111582
Lee J-C, Bae A-N, Lee H-J, Lee J-H. Clinical and Prognostic Values of TRPM7 in Colon and Rectal Cancers. Medicina. 2022; 58(11):1582. https://doi.org/10.3390/medicina58111582
Chicago/Turabian StyleLee, Jun-Chae, An-Na Bae, Ha-Jin Lee, and Jae-Ho Lee. 2022. "Clinical and Prognostic Values of TRPM7 in Colon and Rectal Cancers" Medicina 58, no. 11: 1582. https://doi.org/10.3390/medicina58111582
APA StyleLee, J.-C., Bae, A.-N., Lee, H.-J., & Lee, J.-H. (2022). Clinical and Prognostic Values of TRPM7 in Colon and Rectal Cancers. Medicina, 58(11), 1582. https://doi.org/10.3390/medicina58111582






