Internal Fixation of Garden Type III Femoral Neck Fractures with Sliding Hip Screw and Anti-Rotation Screw: Does Increased Valgus Improve Healing?
Abstract
1. Introduction
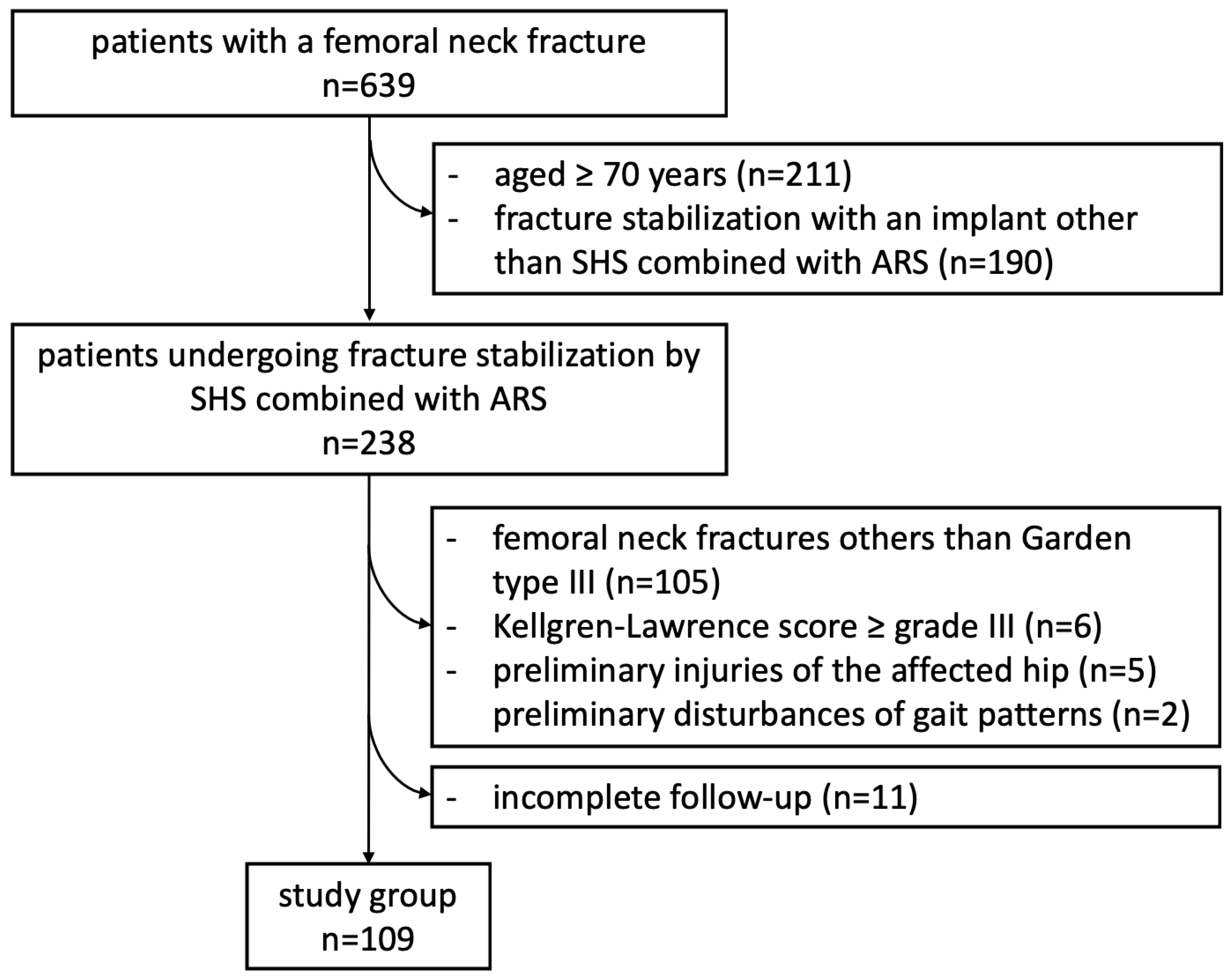
2. Patients and Methods
2.1. Study Design
2.2. Surgical Procedure
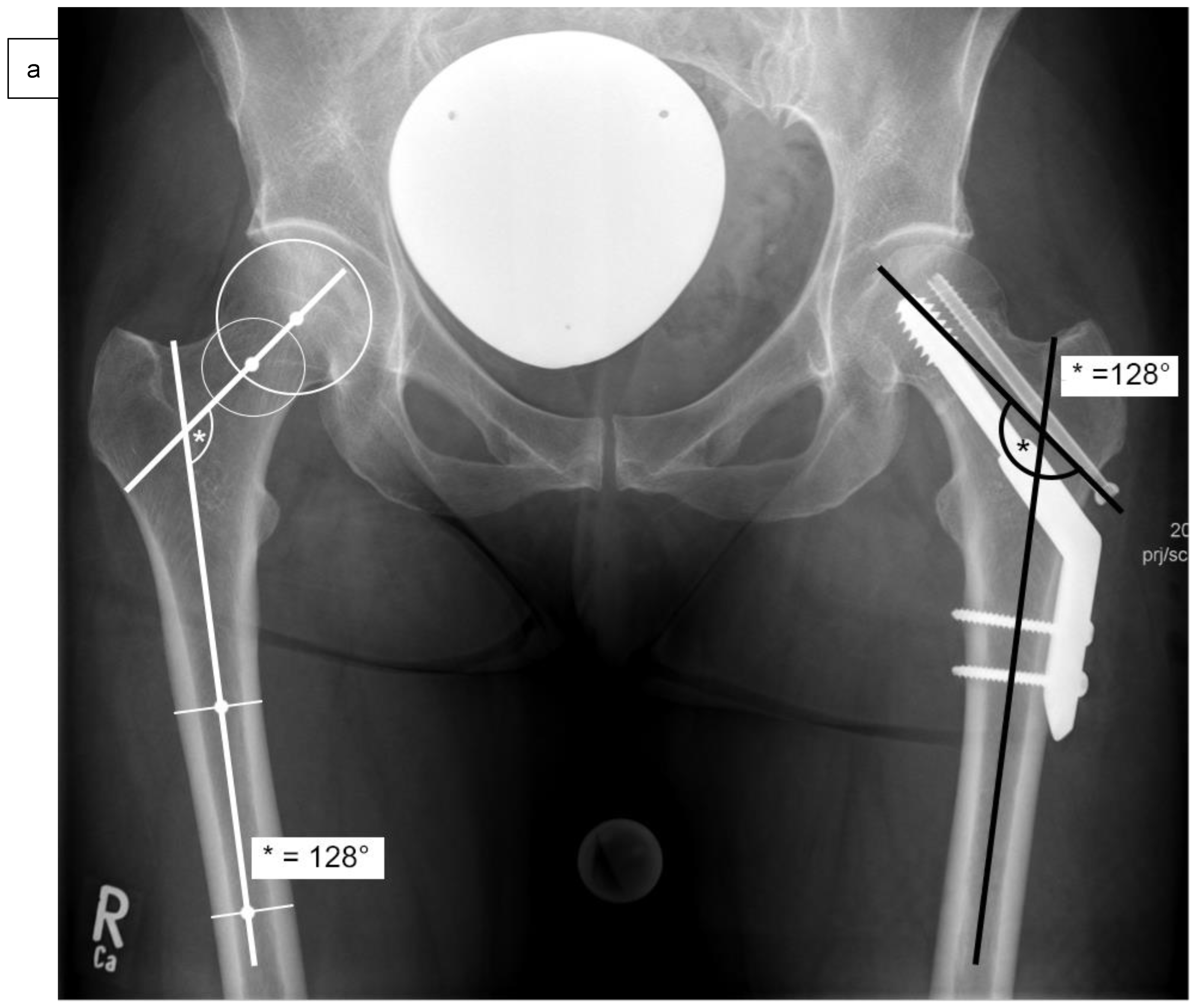
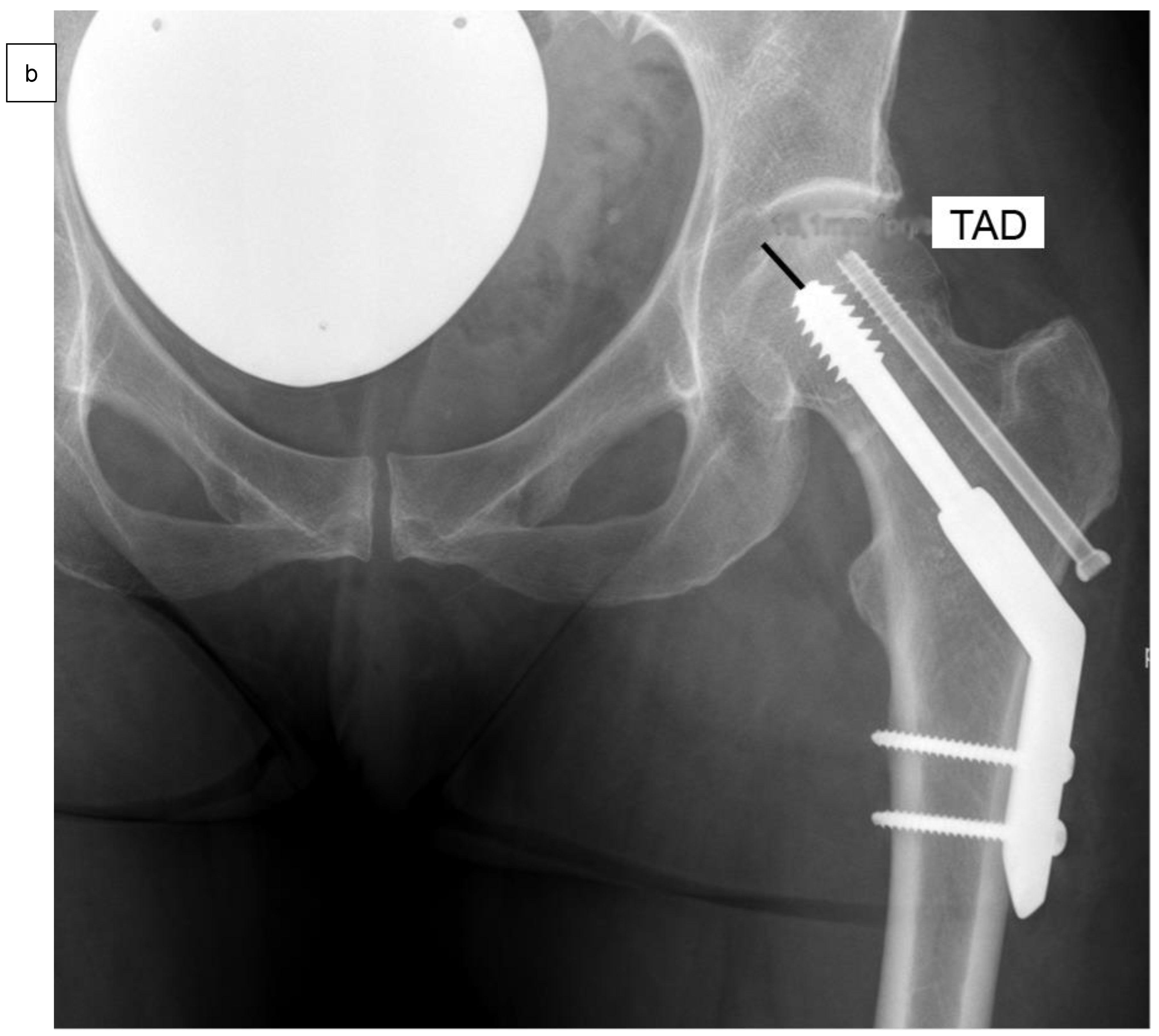
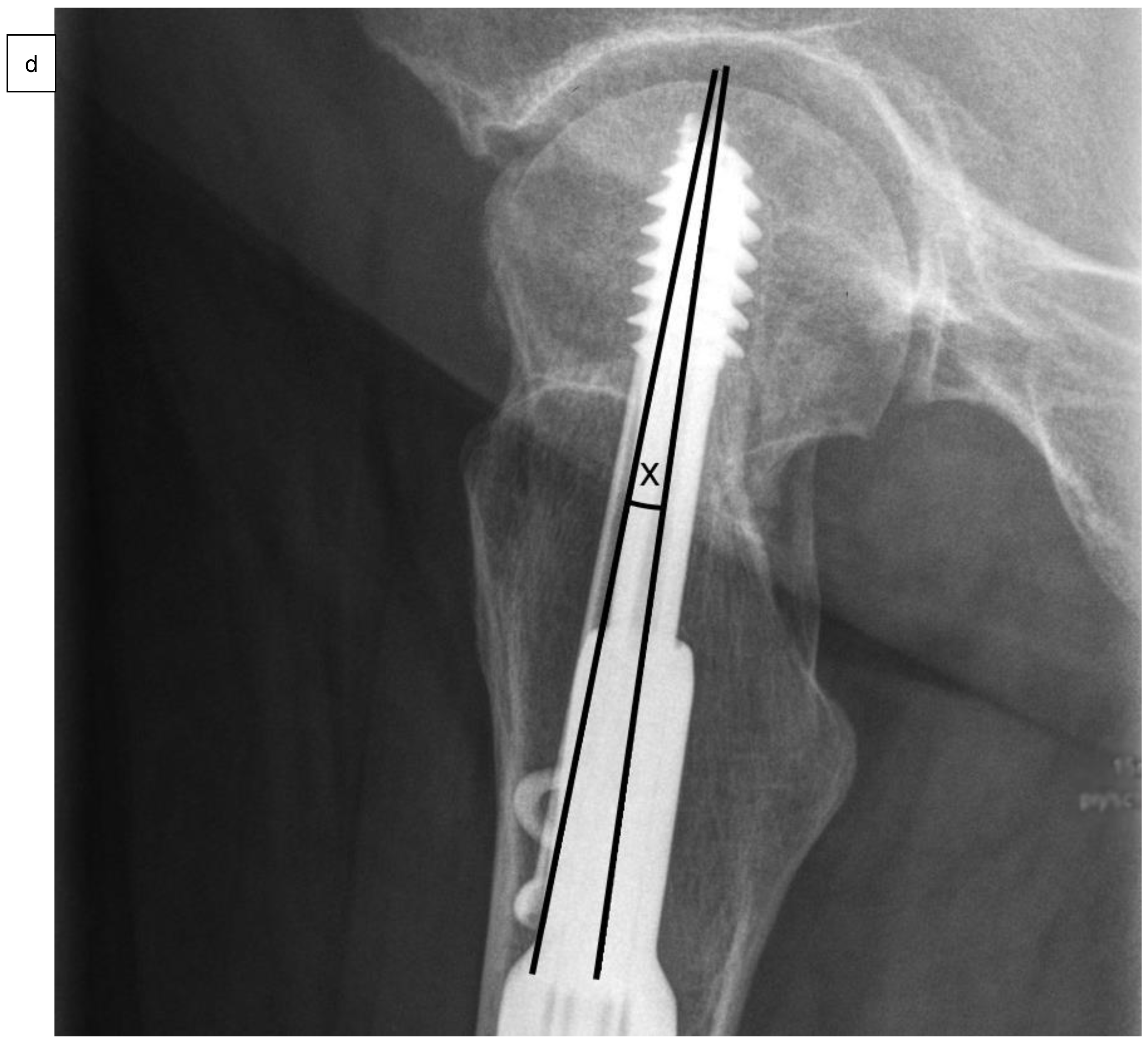
2.3. Clinical and Radiological Assessment
2.4. Follow-Up
2.5. Statistical Analysis
2.6. Ethics and Study Registration
3. Results
3.1. Patient Cohort
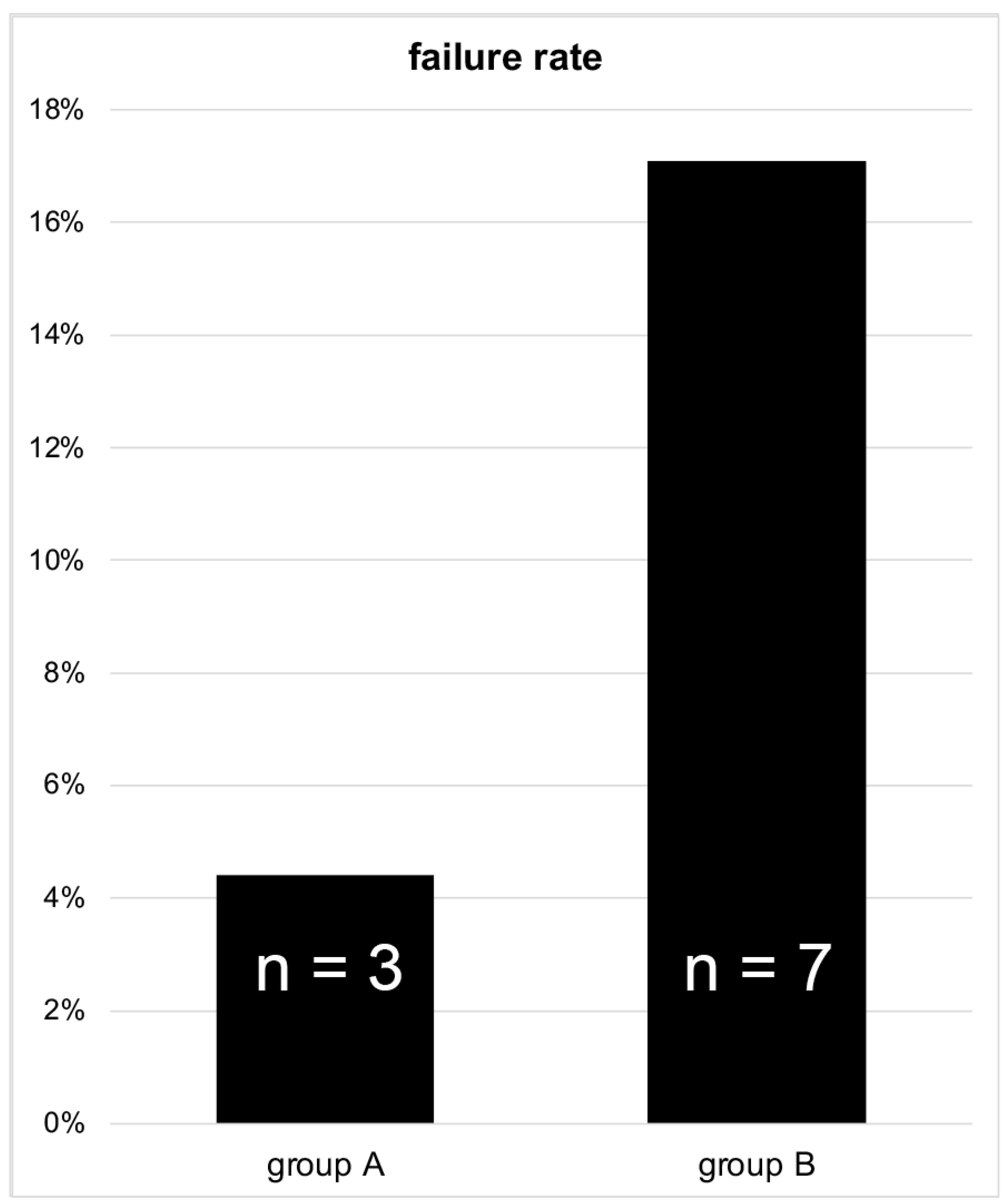
3.2. Treatment Failure
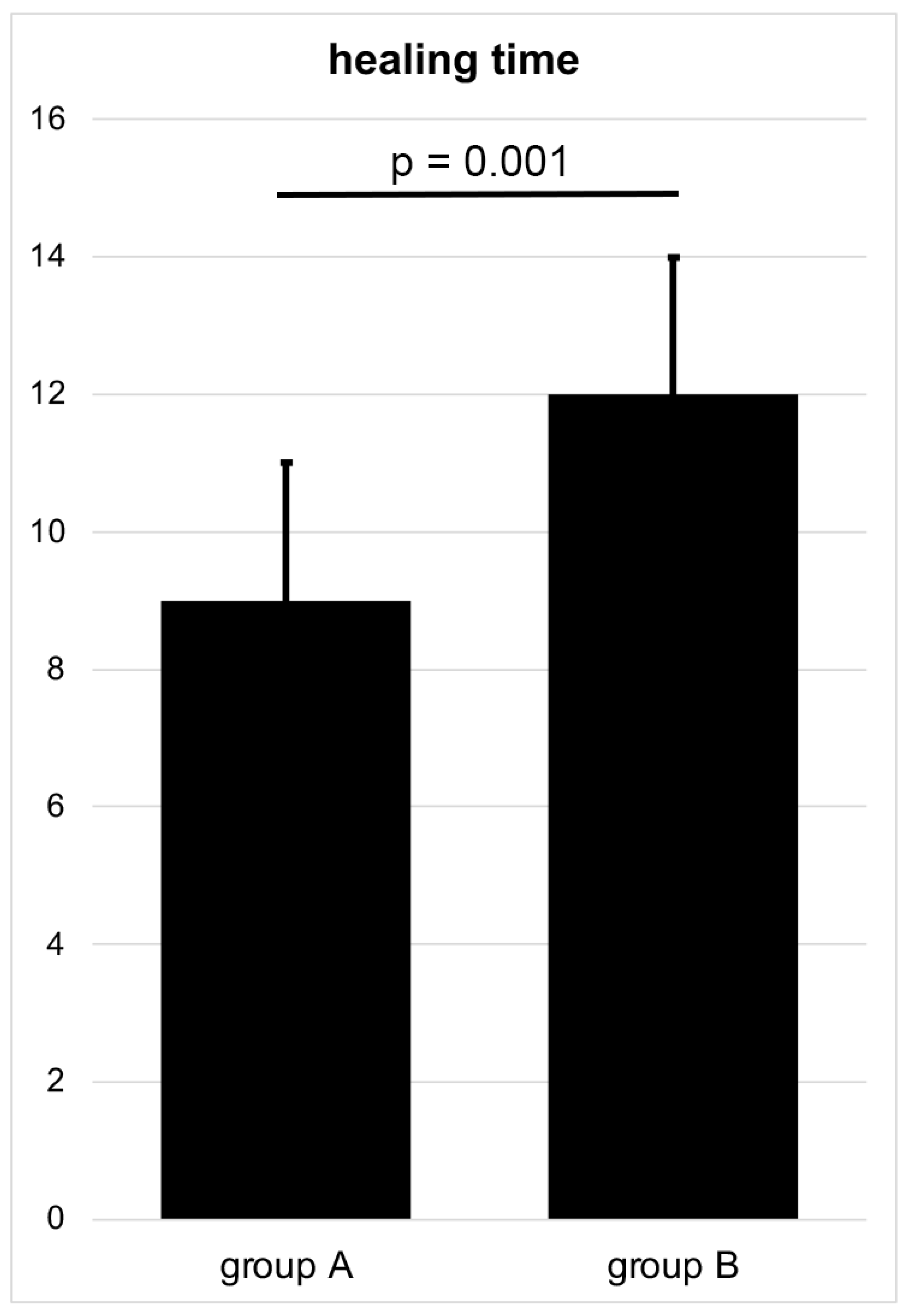
3.3. Healing Time
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Augat, P.; Bliven, E.; Hackl, S. Biomechanics of Femoral Neck Fractures and Implications for Fixation. J. Orthop. Trauma 2019, 33 (Suppl. 1), S27–S32. [Google Scholar] [CrossRef] [PubMed]
- Liporace, F.; Gaines, R.; Collinge, C.; Haidukewych, G.J. Results of internal fixation of Pauwels type-3 vertical femoral neck fractures. J. Bone Jt. Surg. 2008, 90, 1654–1659. [Google Scholar] [CrossRef] [PubMed]
- Ly, T.V.; Swiontkowski, M.F. Treatment of femoral neck fractures in young adults. J. Bone Jt. Surg. 2008, 90, 2254–2266. [Google Scholar]
- Bliven, E.; Sandriesser, S.; Augat, P.; von Rüden, C.; Hackl, S. Biomechanical evaluation of locked plating fixation for unstable femoral neck fractures. Bone Jt. Res. 2020, 9, 314–321. [Google Scholar] [CrossRef] [PubMed]
- Yuan, B.J.; Shearer, D.W.; Barei, D.P.; Nork, S.E. Intertrochanteric Osteotomy for Femoral Neck Nonunion: Does “Undercorrection” Result in an Acceptable Rate of Femoral Neck Union? J. Orthop. Trauma 2017, 31, 420–426. [Google Scholar] [CrossRef] [PubMed]
- Augat, P.; Hollensteiner, M.; von Rüden, C. The role of mechanical stimulation in the enhancement of bone healing. Injury 2021, 52 (Suppl. 2), S78–S83. [Google Scholar] [CrossRef]
- Min, B.-W.; Bae, K.-C.; Kang, C.-H.; Song, K.S.; Kim, S.-Y.; Won, Y.-Y. Valgus intertrochanteric osteotomy for non-union of femoral neck fracture. Injury 2006, 37, 786–790. [Google Scholar] [CrossRef]
- Prakash, J.; Keshari, V.; Chopra, R.K. Experience of valgus osteotomy for neglected and failed osteosynthesis in fractures neck of femur. Int. Orthop. 2020, 44, 705–713. [Google Scholar] [CrossRef]
- Kazley, J.M.; Banerjee, S.; Abousayed, M.M.; Rosenbaum, A.J. Classifications in Brief: Garden Classification of Femoral Neck Fractures. Clin. Orthop. Relat. Res. 2018, 476, 441–445. [Google Scholar] [CrossRef]
- Frandsen, P.; Andersen, E.; Madsen, F.; Skjødt, T. Garden’s classification of femoral neck fractures. An assessment of inter-observer variation. J. Bone Jt. Surgery. Br. 1988, 70, 588–590. [Google Scholar] [CrossRef]
- Sjöholm, P.; Sundkvist, J.; Wolf, O.; Sköldenberg, O.; Gordon, M.; Mukka, S. Preoperative Anterior and Posterior Tilt of Garden I-II Femoral Neck Fractures Predict Treatment Failure and Need for Reoperation in Patients Over 60 Years. JBJS Open Access 2021, 6, e21.00045. [Google Scholar] [CrossRef] [PubMed]
- Nyholm, A.M.; Palm, H.; Sandholdt, H.; Troelsen, A.; Gromov, K.; DFDB Collaborators. Risk of reoperation within 12 months following osteosynthesis of a displaced femoral neck fracture is linked mainly to initial fracture displacement while risk of death may be linked to bone quality: A cohort study from Danish Fracture Database. Acta Orthop. 2019, 91, 1–75. [Google Scholar] [CrossRef] [PubMed]
- Kohn, M.D.; Sassoon, A.A.; Fernando, N.D. Classifications in Brief: Kellgren-Lawrence Classification of Osteoarthritis. Clin. Orthop. Relat. Res. 2016, 474, 1886–1893. [Google Scholar] [CrossRef] [PubMed]
- Baumgaertner, M.R.; Curtin, S.L.; Lindskog, D.M.; Keggi, J.M. The value of the tip-apex distance in predicting failure of fixation of peritrochanteric fractures of the hip. J. Bone Jt. Surg. 1995, 77, 1058–1064. [Google Scholar] [CrossRef]
- Fisher, J.S.; Kazam, J.J.; Fufa, D.; Bartolotta, R.J. Radiologic evaluation of fracture healing. Skelet. Radiol. 2019, 48, 349–361. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; L. Lawrence Earlbaum Associates: Hillsdale, NJ, USA, 1988. [Google Scholar]
- Samsami, S.; Augat, P.; Rouhi, G. Stability of femoral neck fracture fixation: A finite element analysis. Proc. Inst. Mech. Eng. Part H 2019, 233, 892–900. [Google Scholar] [CrossRef]
- Kane, C.; Jo, J.; Siegel, J.; Matuszewski, P.E.; Swart, E. Can we predict failure of percutaneous fixation of femoral neck fractures? Injury 2020, 51, 357–360. [Google Scholar] [CrossRef]
- Dai, Y.; Ni, M.; Dou, B.; Wang, Z.; Zhang, Y.; Cui, X.; Ma, W.; Qin, T.; Xu, X.; Mei, J. Finite element analysis of necessity of reduction and selection of internal fixation for valgus-impacted femoral neck fracture. Comput. Methods Biomech. Biomed. Eng. 2022, 1–8. [Google Scholar] [CrossRef]
- Ramallo, D.A.; Kropf, L.L.; Zaluski, A.D.; Cavalcanti, A.D.S.; Duarte, M.E.L.; Guimarães, J.A.M. Factors Influencing the Outcome of Osteosynthesis in the Fracture of the Femoral Neck in Young Adult Patients. Rev. Bras. Ortop. 2019, 54, 408–415. [Google Scholar] [CrossRef]
- Schwartsmann, C.R.; Jacobus, L.S.; Spinelli, L.D.F.; Boschin, L.C.; Gonçalves, R.Z.; Yépez, A.K.; Barreto, R.P.G.; Silva, M.F. Dynamic hip screw for the treatment of femoral neck fractures: A prospective study with 96 patients. ISRN Orthop. 2014, 2014, 257871. [Google Scholar] [CrossRef]
- Garden, R.S. Malreduction and avascular necrosis in subcapital fractures of the femur. J. Bone Jt. Surgery. Br. 1971, 53, 183–197. [Google Scholar] [CrossRef]
- Moon, N.H.; Shin, W.C.; Jang, J.H.; Seo, H.U.; Bae, J.Y.; Suh, K.T. Surgical Outcomes of Internal Fixation Using Multiple Screws in Femoral Neck Fractures with Valgus Impaction: When Should We Consider Hip Arthroplasty? A Retrospective, Multicenter Study. Hip Pelvis 2019, 31, 136–143. [Google Scholar] [CrossRef]
- Lindequist, S.; Törnkvist, H. Quality of reduction and cortical screw support in femoral neck fractures. An analysis of 72 fractures with a new computerized measuring method. J. Orthop. Trauma 1995, 9, 215–221. [Google Scholar] [CrossRef] [PubMed]
- Park, Y.-C.; Um, K.-S.; Kim, D.-J.; Byun, J.; Yang, K.-H. Comparison of femoral neck shortening and outcomes between in situ fixation and fixation after reduction for severe valgus-impacted femoral neck fractures. Injury 2021, 52, 569–574. [Google Scholar] [CrossRef]
- Konarski, W.; Poboży, T.; Kotela, A.; Śliwczyński, A.; Kotela, I.; Hordowicz, M.; Krakowiak, J. The Risk of Avascular Necrosis Following the Stabilization of Femoral Neck Fractures: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2022, 19, 10050. [Google Scholar] [CrossRef] [PubMed]
- Tian, P.; Kuang, L.; Li, Z.-J.; Xu, G.-J.; Fu, X. Comparison Between Femoral Neck Systems and Cannulated Cancellous Screws in Treating Femoral Neck Fractures: A Meta-Analysis. Geriatr. Orthop. Surg. Rehabil. 2022, 13, 21514593221113533. [Google Scholar] [CrossRef] [PubMed]
- Nieminen, S.; Nurmi, M.; Satokari, K. Healing of femoral neck fractures; influence of fracture reduction and age. Ann. Chir. Gynaecol. 1981, 70, 26–31. [Google Scholar]
- Hente, R.; Maghsudi, M.; Nerlich, M. Reposition der Schenkelhalsfraktur des jüngeren Menschen. Valgus- oder anatomische Reposition? [Repositioning femoral neck fracture in younger patients. Valgus or anatomic reposition?]. Der Unfallchirurg 2001, 104, 1055–1060. (In German) [Google Scholar] [CrossRef]
- Yang, J.-J.; Lin, L.-C.; Chao, K.-H.; Chuang, S.-Y.; Wu, C.-C.; Yeh, T.-T.; Lian, Y.-T. Risk factors for nonunion in patients with intracapsular femoral neck fractures treated with three cannulated screws placed in either a triangle or an inverted triangle configuration. J. Bone Jt. Surg. Am. 2013, 95, 61–69. [Google Scholar] [CrossRef]
- Song, H.K.; Lee, J.J.; Oh, H.C.; Yang, K.H. Clinical implication of subgrouping in valgus femoral neck fractures: Comparison of 31-B1.1 with 31-B1.2 fractures using the OTA/AO classification. J. Orthop. Trauma 2013, 27, 677–682. [Google Scholar] [CrossRef]

| Group A | Group B | p-Value | |
|---|---|---|---|
| Group size Male Female | 68 40 28 | 41 23 18 | |
| Age | 55 ± 11 years | 55 ± 11 years | 0.78 |
| Body mass index | 24.9 ± 3.2 kg/m2 | 23.6 ± 3.5 kg/m2 | 0.07 |
| ASA 1 | 1.6 ± 0.7 | 1.8 ± 0.6 | 0.26 |
| Duration between trauma and fracture stabilization | |||
| ≤24 h >24 h | 65 3 | 40 1 | |
| SHS plate | |||
| 2-hole 4-hole | 61 7 | 38 3 | |
| Barrel angle of SHS | |||
| 130° 135° | 7 61 | 3 38 | |
| Kellgren–Lawrence score | 1.0 ± 0.6 | 1.2 ± 0.6 | 0.14 |
| Cut-to-seam time of the surgical procedure | 58 ± 19 min | 60 ± 21 min | 0.70 |
| Tip-apex distance (TAD) | 10.0 ± 2.9 mm | 9.3 ± 2.8 mm | 0.89 |
| Angle between SHS and ARS in frontal plane | 0.0 ± 0.2° | 0.0 ± 0.3° | 0.56 |
| Angle between SHS and ARS in axial plane | 2.2 ± 1.8° | 2.4 ± 1.5° | 0.76 |
| Femoral neck angle 6 weeks postoperatively | 130.5 ± 3.8° | 142.8 ± 4.3° | 0.001 |
| Difference of the femoral neck angle 6 weeks postoperatively in comparison to the contralateral side | 1.2 ± 1.3° | 12.0 ± 4.2° | 0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hackl, S.; von Rüden, C.; Weisemann, F.; Klöpfer-Krämer, I.; Stuby, F.M.; Högel, F. Internal Fixation of Garden Type III Femoral Neck Fractures with Sliding Hip Screw and Anti-Rotation Screw: Does Increased Valgus Improve Healing? Medicina 2022, 58, 1573. https://doi.org/10.3390/medicina58111573
Hackl S, von Rüden C, Weisemann F, Klöpfer-Krämer I, Stuby FM, Högel F. Internal Fixation of Garden Type III Femoral Neck Fractures with Sliding Hip Screw and Anti-Rotation Screw: Does Increased Valgus Improve Healing? Medicina. 2022; 58(11):1573. https://doi.org/10.3390/medicina58111573
Chicago/Turabian StyleHackl, Simon, Christian von Rüden, Ferdinand Weisemann, Isabella Klöpfer-Krämer, Fabian M. Stuby, and Florian Högel. 2022. "Internal Fixation of Garden Type III Femoral Neck Fractures with Sliding Hip Screw and Anti-Rotation Screw: Does Increased Valgus Improve Healing?" Medicina 58, no. 11: 1573. https://doi.org/10.3390/medicina58111573
APA StyleHackl, S., von Rüden, C., Weisemann, F., Klöpfer-Krämer, I., Stuby, F. M., & Högel, F. (2022). Internal Fixation of Garden Type III Femoral Neck Fractures with Sliding Hip Screw and Anti-Rotation Screw: Does Increased Valgus Improve Healing? Medicina, 58(11), 1573. https://doi.org/10.3390/medicina58111573








