A Rare Case of Fatal Endobronchial Mucormycosis Masquerading as Endobronchial Tuberculosis
Abstract
1. Introduction
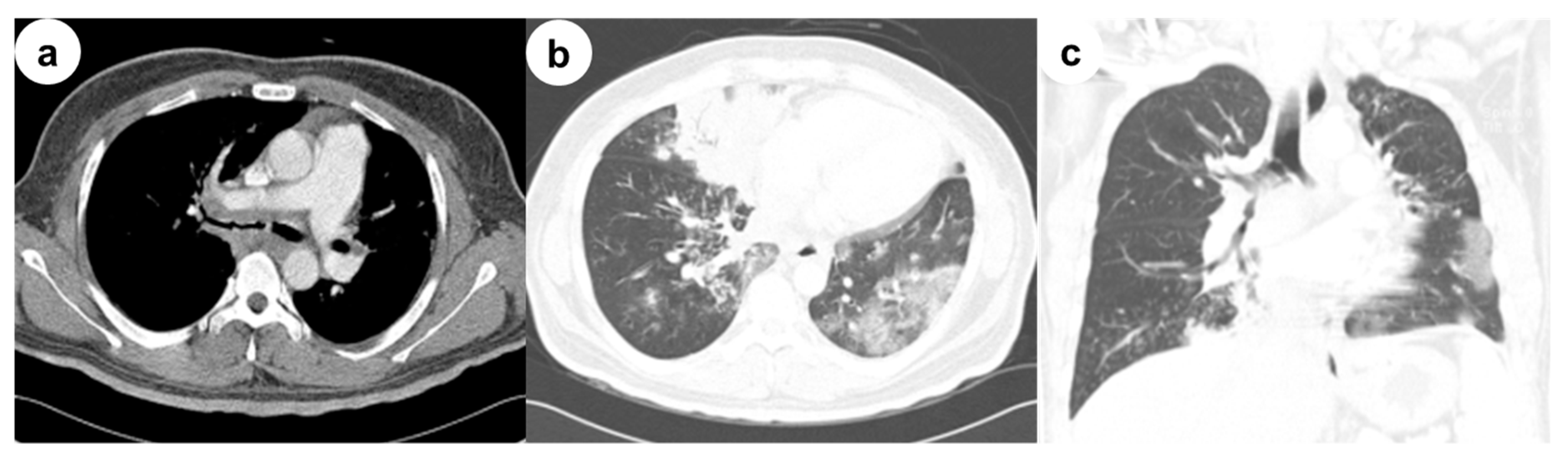
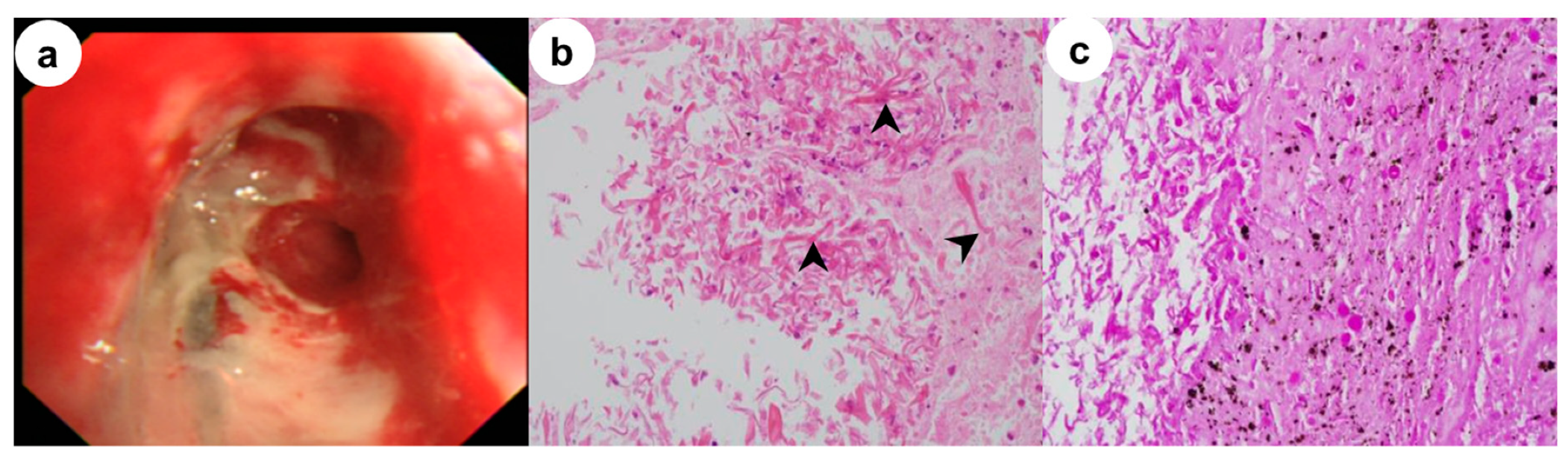
2. Case Report
3. Discussion
4. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Petrikkos, G.; Skiada, A.; Lortholary, O.; Roilides, E.; Walsh, T.J.; Kontoyiannis, D.P. Epidemiology and clinical manifestations of mucormycosis. Clin. Infect. Dis. 2012, 54 (Suppl 1), S23–S34. [Google Scholar] [CrossRef]
- Roden, M.M.; Zaoutis, T.E.; Buchanan, W.L.; Knudsen, T.A.; Sarkisova, T.A.; Schaufele, R.L.; Sein, M.; Sein, T.; Chiou, C.C.; Chu, J.H.; et al. Epidemiology and outcome of zygomycosis: a review of 929 reported cases. Clin. Infect. Dis. 2005, 41, 634–653. [Google Scholar] [CrossRef] [PubMed]
- Lee, F.Y.; Mossad, S.B.; Adal, K.A. Pulmonary mucormycosis: the last 30 years. Arch. Intern. Med. 1999, 159, 1301–1309. [Google Scholar] [CrossRef] [PubMed]
- Karnak, D.; Avery, R.K.; Gildea, T.R.; Sahoo, D.; Mehta, A.C. Endobronchial fungal disease: An under-recognized entity. Respiration 2007, 74, 88–104. [Google Scholar] [CrossRef] [PubMed]
- Bigby, T.D.; Serota, M.L.; Tierney, L.M., Jr.; Matthay, M.A. Clinical spectrum of pulmonary mucormycosis. Chest 1986, 89, 435–439. [Google Scholar] [CrossRef] [PubMed]
- Husari, A.W.; Jensen, W.A.; Kirsch, C.M.; Campagna, A.C.; Kagawa, F.T.; Hamed, K.A.; Azzi, R.L.; Stevens, D.A. Pulmonary mucormycosis presenting as an endobronchial lesion. Chest 1994, 106, 1889–1891. [Google Scholar] [CrossRef] [PubMed]
- He, R.; Hu, C.; Tang, Y.; Yang, H.; Cao, L.; Niu, R. Report of 12 cases with tracheobronchial mucormycosis and a review. Clin. Respir. J. 2018, 12, 1651–1660. [Google Scholar] [CrossRef] [PubMed]
- Sun, H.Y.; Singh, N. Mucormycosis: its contemporary face and management strategies. Lancet Infect. Dis. 2011, 11, 301–311. [Google Scholar] [CrossRef]
- Chung, H.S.; Lee, J.H. Bronchoscopic assessment of the evolution of endobronchial tuberculosis. Chest 2000, 117, 385–392. [Google Scholar] [CrossRef] [PubMed]
- Tedder, M.; Spratt, J.A.; Anstadt, M.P.; Hegde, S.S.; Tedder, S.D.; Lowe, J.E. Pulmonary mucormycosis: results of medical and surgical therapy. Ann. Thorac. Surg. 1994, 57, 1044–1050. [Google Scholar] [CrossRef]
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, M.; Lim, J.H.; Park, M.; Cha, H.K.; Kim, L.; Nam, H.-S. A Rare Case of Fatal Endobronchial Mucormycosis Masquerading as Endobronchial Tuberculosis. Medicina 2020, 56, 64. https://doi.org/10.3390/medicina56020064
Kim M, Lim JH, Park M, Cha HK, Kim L, Nam H-S. A Rare Case of Fatal Endobronchial Mucormycosis Masquerading as Endobronchial Tuberculosis. Medicina. 2020; 56(2):64. https://doi.org/10.3390/medicina56020064
Chicago/Turabian StyleKim, Minjeong, Jun Hyeok Lim, Mihwa Park, Hyung Keun Cha, Lucia Kim, and Hae-Seong Nam. 2020. "A Rare Case of Fatal Endobronchial Mucormycosis Masquerading as Endobronchial Tuberculosis" Medicina 56, no. 2: 64. https://doi.org/10.3390/medicina56020064
APA StyleKim, M., Lim, J. H., Park, M., Cha, H. K., Kim, L., & Nam, H.-S. (2020). A Rare Case of Fatal Endobronchial Mucormycosis Masquerading as Endobronchial Tuberculosis. Medicina, 56(2), 64. https://doi.org/10.3390/medicina56020064




