Prevalence and Association of Transfusion Transmitted Infections with ABO and Rh Blood Groups among Blood Donors at the National Blood Bank, Amman, Jordan
Abstract
1. Introduction
2. Materials and Methods
2.1. Subjects
2.2. Statistical Analysis
3. Results
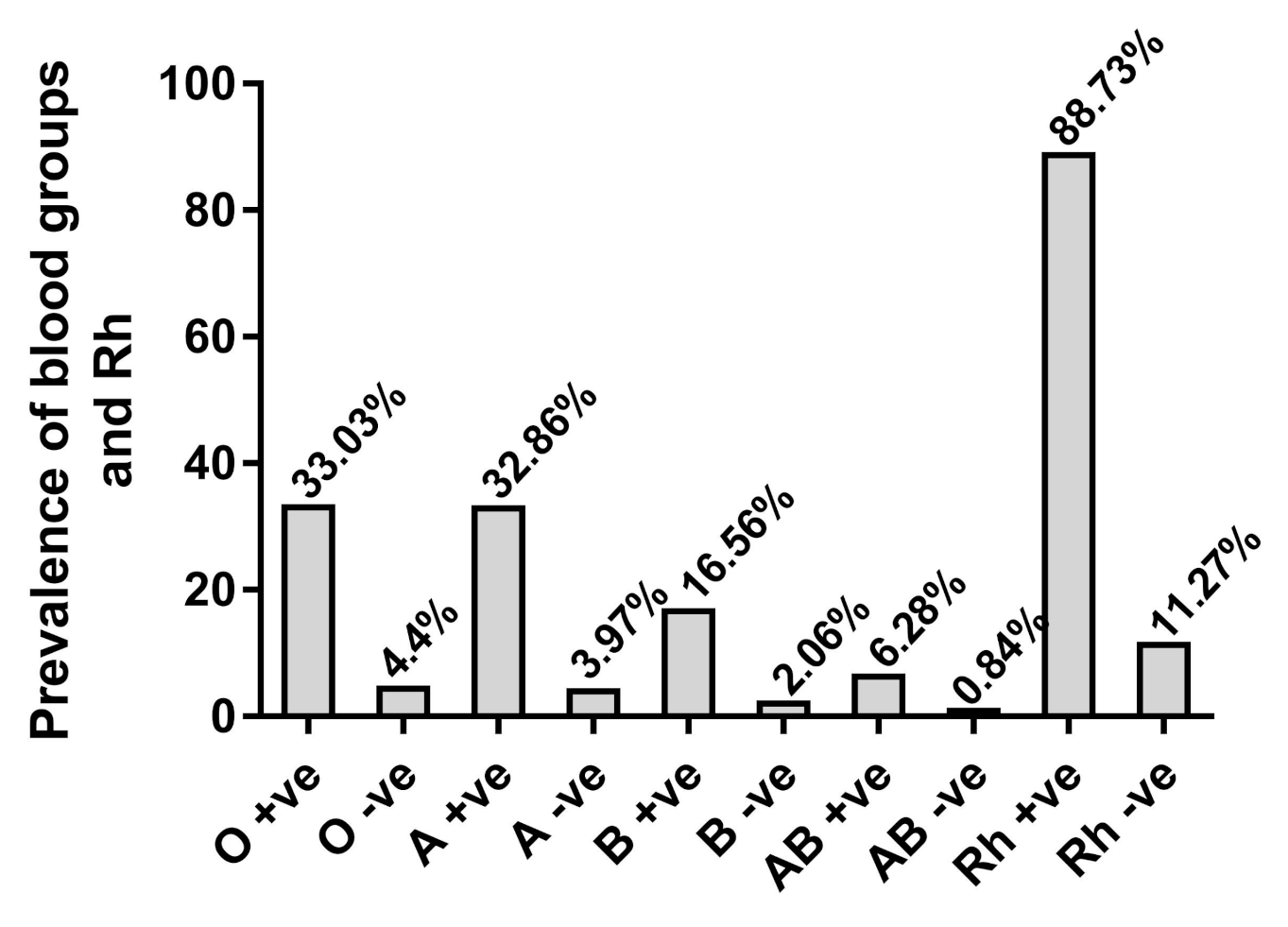
3.1. Distribution of ABO and Rh Blood Groups
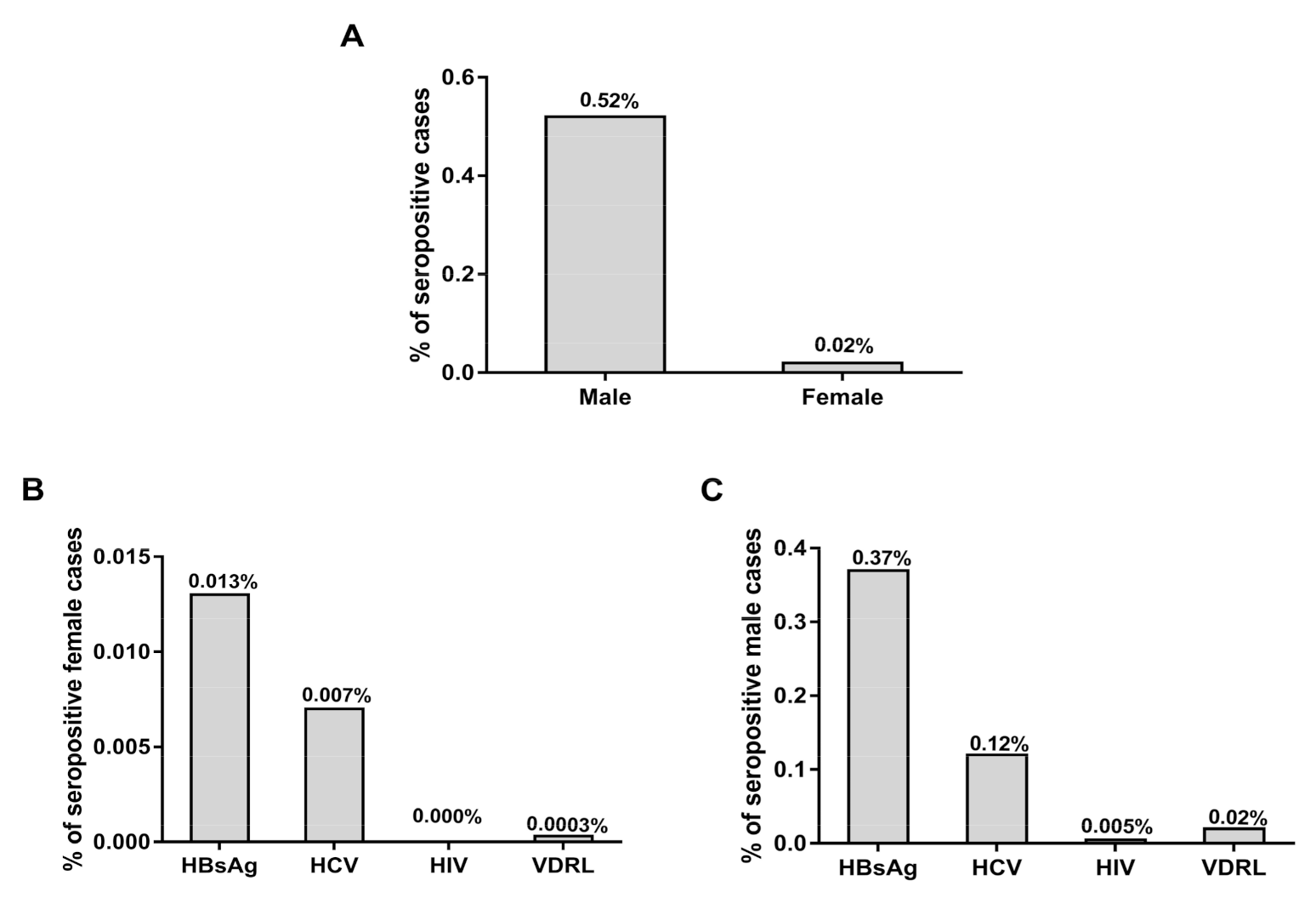
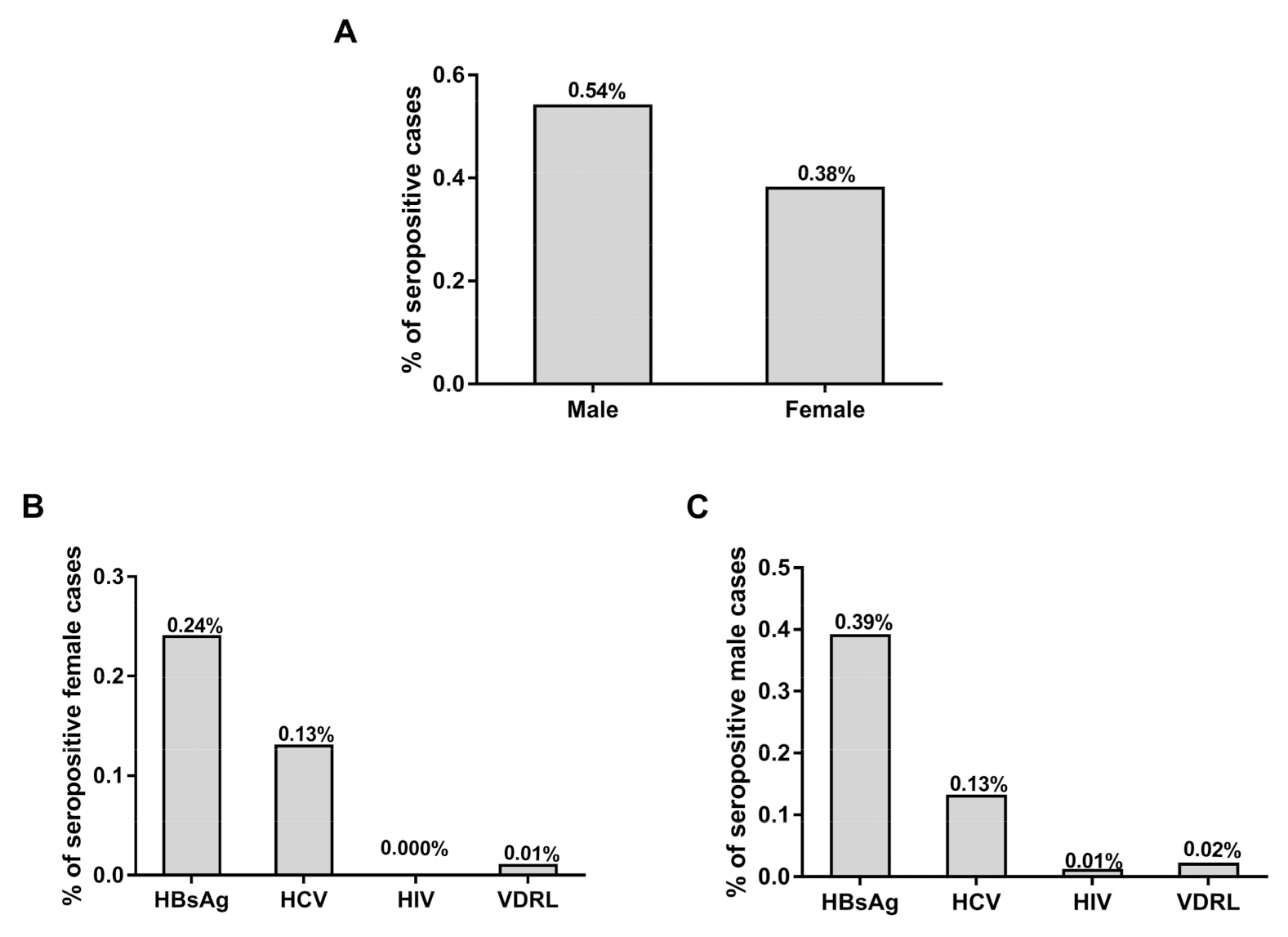
3.2. Prevalence of TTIs among Blood Donors
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Mohammed, Y.; Bekele, A. Seroprevalence of transfusion transmitted infection among blood donors at Jijiga blood bank, eastern Ethiopia: Retrospective 4 years study. BMC Res. Notes 2016, 9, 129. [Google Scholar] [CrossRef] [PubMed]
- Shah, M.; Shah, S.; Gajjar, M.; Bhatnagar, N.; Soni, S.; Patel, V. Prevalence of HIV-I/II, HCV, HBsAg& Syphilis in Blood Donors of Western Region in India. Natl. J. Integr. Res. Med. 2016, 7, 12–15. [Google Scholar]
- Nigam, J.S.; Singh, S.; Kaur, V.; Giri, S.; Kaushal, R.P. The prevalence of transfusion transmitted infections in ABO blood groups and Rh type system. Hematol. Rep. 2014, 6, 5602. [Google Scholar] [CrossRef] [PubMed]
- Li, C.; Xiao, X.; Yin, H.; He, M.; Li, J.; Dai, Y.; Fu, Y.; Ge, J.; Yang, Y.; Luan, Y. Prevalence and prevalence trends of transfusion transmissible infections among blood donors at four Chinese regional blood centers between 2000 and 2010. J. Transl. Med. 2012, 10, 176. [Google Scholar] [CrossRef]
- Gottlieb, M.S.; Schroff, R.; Schanker, H.M.; Weisman, J.D.; Fan, P.T.; Wolf, R.A.; Saxon, A. Pneumocystis carinii pneumonia and mucosal candidiasis in previously healthy homosexual men: Evidence of a new acquired cellular immunodeficiency. N. Engl. J. Med. 1981, 305, 1425–1431. [Google Scholar] [CrossRef]
- Mohammadali, F.; Pourfathollah, A. Association of abo and Rh blood groups to blood-borne infections among blood donors in Tehran-Iran. Iran. J. Public Health 2014, 43, 981. [Google Scholar]
- Branch, D.R. Blood groups and susceptibility to virus infection: New developments. Curr. Opin. Hematol. 2010, 17, 558–564. [Google Scholar] [CrossRef]
- Kokki, I.; Smith, D.; Simmonds, P.; Ramalingam, S.; Wellington, L.; Willocks, L.; Johannessen, I.; Harvala, H. Hepatitis e virus is the leading cause of acute viral hepatitis in Lothian, Scotland. New Microbes. New Infect. 2016, 10, 6–12. [Google Scholar] [CrossRef][Green Version]
- WHO. Global Prevalence and Incidence of Selected Curable Sexually Transmitted Infections: Overview and Estimates; World Health Organization: Geneva, Switzerland, 2001. [Google Scholar]
- Panda, M.; Kar, K. HIV, hepatitis B and C infection status of the blood donors in a blood bank of a tertiary Health Care Centre of Orissa. Indian J. Public Health 2008, 52, 43. [Google Scholar]
- Agarwal, N. Response rate of blood donors in the Uttarakhand region of India after notification of reactive test results on their blood samples. Blood Transfus. 2014, 12, s51. [Google Scholar]
- Omar, A. The infection with HBV and HCV and their relationship to abo blood group among blood donors. J. Fac. Med. 2012, 54, 52–56. [Google Scholar]
- Tyagi, S.; Tyagi, A. Possible correlation of transfusion transmitted diseases with Rh type and abo blood group system. J. Clin. Diagn. Res. JCDR 2013, 7, 1930. [Google Scholar] [CrossRef]
- Gao, X.; Cui, Q.; Shi, X.; Su, J.; Peng, Z.; Chen, X.; Lei, N.; Ding, K.; Wang, L.; Yu, R.; et al. Prevalence and trend of hepatitis C virus infection among blood donors in Chinese mainland: A systematic review and meta-analysis. BMC Infect. Dis. 2011, 11, 88. [Google Scholar] [CrossRef]
- Ghazzawi, I.; Yassin, M.; Alshebly, H.; Sheyyab, S.; Alqudah, B.; Alwahadni, N. Prevalence of hepatitis B and C viruses in hemodialysis patients at JRMS. J. R. Med. Serv. 2015, 102, 1–7. [Google Scholar] [CrossRef]
- Awidi, A.; Tarawneh, M.; El-Khateeb, M.; Hijazi, S.; Shahrouri, M. Incidence of hepatitis b antigen among Jordanian volunteer blood donors. Public Health 1984, 98, 92–96. [Google Scholar] [CrossRef]
- El-Hazmi, M.M. Prevalence of HBV, HCV, HIV-1, 2 and HTLV-I/II infections among blood donors in a teaching hospital in the central region of Saudi Arabia. Saudi Med. J. 2004, 25, 26–33. [Google Scholar] [PubMed]
- Giri, P.A.; Yadav, S.; Parhar, G.S.; Phalke, D.B. Frequency of abo and rhesus blood groups: A study from a rural tertiary care teaching hospital in India. Int. J. Biol. Med. Res. 2011, 2, 988–990. [Google Scholar]
- Alabdulmonem, W.; Shariq, A.; Alqossayir, F.; AbaAlkhail, F.M.; Al-Musallam, A.Y.; Alzaaqi, F.O.; Aloqla, A.A.; Alodhaylah, S.A.; Alsugayyir, A.H.; Aldoubiab, R.K. Sero-prevalence abo and Rh blood groups and their associated transfusion-transmissible infections among blood donors in the central region of Saudi Arabia. J. Infect. Public Health 2020, 13, 299–305. [Google Scholar] [CrossRef] [PubMed]
- Mourant, A.E.; Kipec, A.C. Domaniewska-Sobczak, Kazimiera. In The Distribution of Human Blood Groups; Oxford University Press: London, UK, 1976. [Google Scholar]
- Egesie, U.; Egesie, O.; Usar, I.; Johnbull, T. Distribution of abo, rhesus blood groups and haemoglobin electrophoresis among the undergraduate students of Niger delta university Nigeria. Niger. J. Physiol. Sci. 2008, 23, 5–8. [Google Scholar] [CrossRef]
- Adeyemo, O.A.; Soboyejo, O.B. Frequency distribution 0f ABO, RH blood groups and blood genotypes among the cell biology and genetics students of university of Lagos, Nigeria. Afr. J. Biotechnol. 2006, 5, 2062–2065. [Google Scholar]
- Ullah, S.; Ahmad, T. Distribution of abo and Rh (D) blood groups in the population of District Dir Lower, Khyber Pakhtunkhwa Pakistan. World Appl. Sci. J. 2015, 33, 123–135. [Google Scholar]
- Karim, S.; Hoque, M.M.; Hoque, E.; Begum, H.A.; Rahman, S.M.; Shah, T.A.; Hossain, S.Z. The distribution of abo and rhesus blood groups among blood donor attending transfusion medicine department of Dhaka Medical College Hospital in 2014. J. Dhaka Med. Coll. 2015, 24, 53–56. [Google Scholar] [CrossRef][Green Version]
- Almaiman, A.A.; Almaiman, S.H. Evaluation of blood donors and transfusion transmitted infections and their association with abo and Rh blood groups in Unaizah, Saudi Arabia: A retrospective study. Int. J. Med. Res. Health Sci. 2018, 7, 143–150. [Google Scholar]
- Saghir, S.A.M.; Al–Hassan, F.M.; Alsalahi, O.S.A.; Alhariry, A.-A.; Baqir, H.S. Frequencies of HBV, HCV, HIV, and syphilis markers among blood donors: A hospital-based study in Hodeidah, Yemen. Trop. J. Pharm. Res. 2012, 11, 132–136. [Google Scholar] [CrossRef]
- Xie, D.-D.; Li, J.; Chen, J.-T.; Eyi, U.M.; Matesa, R.A.; Obono, M.M.O.; Ehapo, C.S.; Yang, L.-Y.; Yang, H.; Yang, H.-T. Seroprevalence of human immunodeficiency virus, hepatitis B virus, hepatitis C virus, and Treponema Pallidum infections among blood donors on Bioko Island, Equatorial Guinea. PLoS ONE 2015, 10, e0139947. [Google Scholar] [CrossRef] [PubMed]
- Stokx, J.; Gillet, P.; De Weggheleire, A.; Casas, E.C.; Maendaenda, R.; Beulane, A.J.; Jani, I.V.; Kidane, S.; Mosse, C.D.; Jacobs, J. Seroprevalence of transfusion-transmissible infections and evaluation of the pre-donation screening performance at the Provincial Hospital of Tete, Mozambique. BMC Infect. Dis. 2011, 11, 141. [Google Scholar] [CrossRef]
- Nagalo, B.M.; Bisseye, C.; Sanou, M.; Kienou, K.; Nebié, Y.K.; Kiba, A.; Dahourou, H.; Ouattara, S.; Nikiema, J.B.; Moret, R. Seroprevalence and incidence of transfusion-transmitted infectious diseases among blood donors from regional Blood Transfusion Centres in Burkina Faso, West Africa. Trop. Med. Int. Health 2012, 17, 247–253. [Google Scholar] [CrossRef]
- Othman, B.M.; Monem, M.S.F.S. Prostitutes in Damascus, Syria. Saudi Med. J. 2002, 23, 393–395. [Google Scholar]
- Al Omar, A.S.; Zuebi, F.E. Disease markers in blood donors at King Fahad Hospital, al Baha. Ann. Saudi Med. 1996, 16, 37–41. [Google Scholar] [CrossRef]
- Darwish, M.A.; Raouf, T.A.; Rushdy, P.; Constantine, N.T.; Rao, M.R.; Edelman, R. Risk factors associated with a high Seroprevalence of hepatitis c virus infection in Egyptian blood donors. Am. J. Trop. Med. Hyg. 1993, 49, 440–447. [Google Scholar] [CrossRef]
- Sabino, E.C.; Gonçalez, T.T.; Carneiro-Proietti, A.B.; Sarr, M.; Ferreira, J.E.; Sampaio, D.A.; Salles, N.A.; Wright, D.J.; Custer, B.; Busch, M. HIV prevalence, incidence and residual risk of transmission by transfusions at reds-ii blood centers in brazil. Transfusion 2012, 52, 870. [Google Scholar] [CrossRef]
- Goncalez, T.; Sabino, E.; Murphy, E.; Chen, S.; Chamone, D.; McFarland, W. Human immunodeficiency virus test-seeking motivation in blood donors, Sao Paulo, Brazil. Vox Sang. 2006, 90, 170–176. [Google Scholar] [CrossRef]
- Goncalez, T.; Sabino, E.; Sales, N.; Chen, Y.H.; Chamone, D.; Busch, M.; Murphy, E.; Custer, B.; McFarland, W. Human immunodeficiency virus test-seeking blood donors in a large blood bank in São Paulo, Brazil. Transfusion 2010, 50, 1806–1814. [Google Scholar] [CrossRef]
- Glynn, S.A.; Kleinman, S.H.; Schreiber, G.B.; Busch, M.P.; Wright, D.J.; Smith, J.W.; Nass, C.C.; Williams, A.E. Trends in incidence and prevalence of major transfusion-transmissible viral infections in us blood donors, 1991 to 1996. JAMA 2000, 284, 229–235. [Google Scholar] [CrossRef] [PubMed]
- Behal, R.; Jain, R.; Behal, K.K.; Bhagoliwal, A.; Aggarwal, N.; Dhole, T. Seroprevalence and risk factors for hepatitis b virus infection among general population in northern India. Arq. Gastroenterol. 2008, 45, 137–140. [Google Scholar] [CrossRef] [PubMed]
- Dirisu, J.O.; Alli, T.O.; Adegoke, A.O.; Osazuwa, F. A survey of prevalence of serum antibodies to human immunodeficiency deficiency virus (HIV), hepatitis B virus (HBV) and hepatitis C virus (HCV) among blood donors. North Am. J. Med. Sci. 2011, 3, 35. [Google Scholar] [CrossRef] [PubMed]
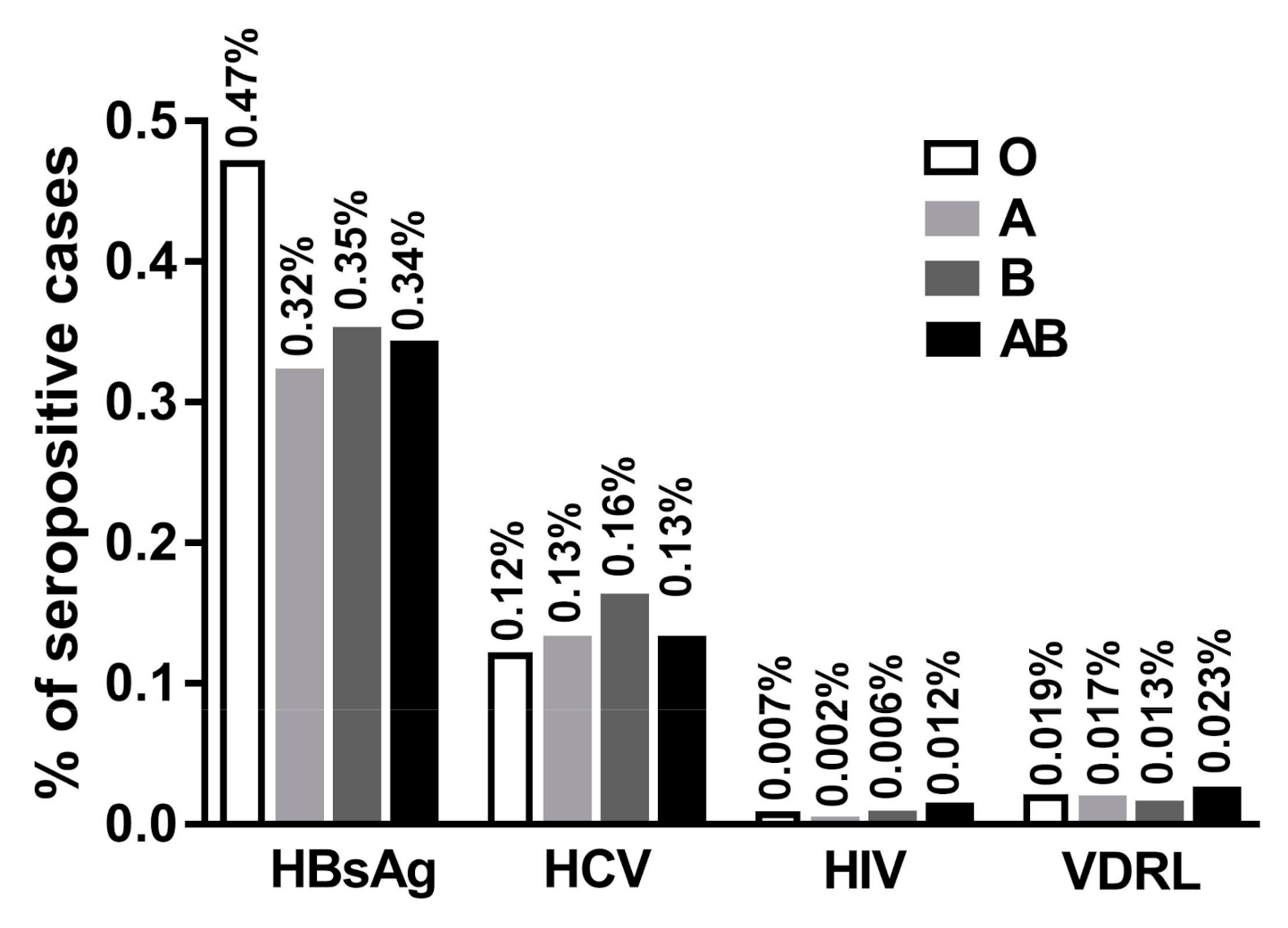
| Blood Group | No and % of Donors | Number and % of Male and Female | HBsAg + ve (%) | HCV + ve (%) | HIV + ve (%) | VDRL + ve (%) |
|---|---|---|---|---|---|---|
| O + ve | 120,586 | M: 114,286 (94.8) | 559 (0.46) | 142 (0.12) | 9 (0.007) | 24 (0.02) |
| F: 6300 (5.2) | 21 (0.02) | 9 (0.007) | 0 (0.00) | 1 (0.000) | ||
| O − ve | 16,065 | M: 15,173 (94.4) | 55 (0.34) | 12 (0.075) | 1 (0.006) | 1 (0.006) |
| F: 892 (5.6) | 5 (0.03) | 1 (0.006) | 0 (0.00) | 0 (0.00) | ||
| A + ve | 119,941 | M: 113,888 (95) | 372 (0.31) | 151 (0.13) | 3 (0.003) | 20 (0.02) |
| F: 6053 (5) | 8 (0.01) | 8 (0.01) | 0 (0.00) | 0 (0.00) | ||
| A − ve | 14,477 | M: 13,655 (94.3) | 43 (0.30) | 17 (0.12) | 0 (0.00) | 3 (0.0.02) |
| F: 822 (5.7) | 1 (0.007) | 0 (0.00) | 0 (0.00) | 0 (0.00) | ||
| B + ve | 60,450 | M: 57,385 (94.9) | 211 (0.35) | 98 (0.16) | 4 (0.007) | 9 (0.015) |
| F: 3065 (5.1) | 7 (0.11) | 4 (0.007) | 0 (0.00) | 0 (0.00) | ||
| B − ve | 7517 | M: 7095 (94.4) | 20 (0.27) | 4 (0.05) | 0 (0.00) | 0 (0.00) |
| F: 422 (5.6) | 1 (0.013) | 0 (0.00) | 0 (0.00) | 0 (0.00) | ||
| AB + ve | 22,920 | M: 21,714 (94.70) | 79 (0.34) | 27 (0.118) | 2 (0.009) | 6 (0.03) |
| F: 1206 (5.3) | 3 (0.01) | 2 (0.009) | 0 (0.00) | 0 (0.00) | ||
| AB − ve | 3073 | M: 2852 (92.8) | 6 (0.20) | 4 (0.13) | 1 (0.32) | 0 (0.00) |
| F: 221 (7.2) | 0 (0.00) | 1 (0.32) | 0 (0.00) | 0 (0.00) | ||
| Total | 365,029 | M: 346,048(94.8) | M:1345(0.37) | M: 455(1.25) | M: 19(0.005) | M: 63(0.02) |
| F: 18,981(5.2) | F: 46(0.013) | F: 25(0.007) | F: 0(0.00) | F: 1(0.0003) |
| Year | No of Donors | HBsAg | HCV | HIV | VDRL |
|---|---|---|---|---|---|
| N (%) | N (%) | N (%) | N (%) | ||
| 2013 | 62,078 | M: 487 (0.784) | M: 111 (0.179) | M: 2 (0.003) | M: 9 (0.014) |
| F: 15 (0.024) | F: 8 (0.013) | F: 0 (0.00) | F: 0 (0.00) | ||
| 2014 | 64,394 | M: 270 (0.419) | M: 71 (0.110) | M: 2 (0.003) | M: 4 (0.006) |
| F: 8 (0.012) | F: 1 (0.002) | F: 0 (0.00) | F: 0 (0.00) | ||
| 2015 | 60,677 | M: 245 (0.404) | M: 99 (0.163) | M: 0 (0.00) | M: 19 (0.031) |
| F: 8 (0.013) | F: 6 (0.010) | F: 0 (0.00) | F: 1 (0.002) | ||
| 2016 | 57,750 | M: 157 (0.272) | M: 74 (0.128) | M: 2 (0.003) | M: 11 (0.019) |
| F: 5 (0.009) | F: 1 (0.002) | F: 0 (0.00) | F: 0 (0.00) | ||
| 2017 | 59,680 | M: 106 (0.178) | M: 52 (0.087) | M: 2 (0.003) | M: 8 (0.013) |
| F: 4 (0.007) | F: 7 (0.012) | F: 0 (0.00) | F: 0 (0.00) | ||
| 2018 | 60,450 | M: 80 (0.132) | M: 48 (0.08) | M: 2 (0.003) | M: 12 (0.019) |
| F: 6 (0.010) | F: 2 (0.003) | F: 0 (0.00) | F: 0 (0.00) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hroob, A.M.A.; Saghir, S.A.M.; Almaiman, A.A.; Alsalahi, O.S.A.; Al-Wajeeh, A.S.; Al-Shargi, O.Y.A.; Al-Balagi, N.; Mahmoud, A.M. Prevalence and Association of Transfusion Transmitted Infections with ABO and Rh Blood Groups among Blood Donors at the National Blood Bank, Amman, Jordan. Medicina 2020, 56, 701. https://doi.org/10.3390/medicina56120701
Hroob AMA, Saghir SAM, Almaiman AA, Alsalahi OSA, Al-Wajeeh AS, Al-Shargi OYA, Al-Balagi N, Mahmoud AM. Prevalence and Association of Transfusion Transmitted Infections with ABO and Rh Blood Groups among Blood Donors at the National Blood Bank, Amman, Jordan. Medicina. 2020; 56(12):701. https://doi.org/10.3390/medicina56120701
Chicago/Turabian StyleHroob, Amir M. Al, Sultan A. M. Saghir, Amer A. Almaiman, Omar S. A. Alsalahi, Abdullah S. Al-Wajeeh, Omar Y. A. Al-Shargi, Nader Al-Balagi, and Ayman M. Mahmoud. 2020. "Prevalence and Association of Transfusion Transmitted Infections with ABO and Rh Blood Groups among Blood Donors at the National Blood Bank, Amman, Jordan" Medicina 56, no. 12: 701. https://doi.org/10.3390/medicina56120701
APA StyleHroob, A. M. A., Saghir, S. A. M., Almaiman, A. A., Alsalahi, O. S. A., Al-Wajeeh, A. S., Al-Shargi, O. Y. A., Al-Balagi, N., & Mahmoud, A. M. (2020). Prevalence and Association of Transfusion Transmitted Infections with ABO and Rh Blood Groups among Blood Donors at the National Blood Bank, Amman, Jordan. Medicina, 56(12), 701. https://doi.org/10.3390/medicina56120701






