Application of an Expandable Cage for Reconstruction of the Cervical Spine in a Consecutive Series of Eighty-Six Patients
Abstract
1. Introduction
2. Materials and Methods
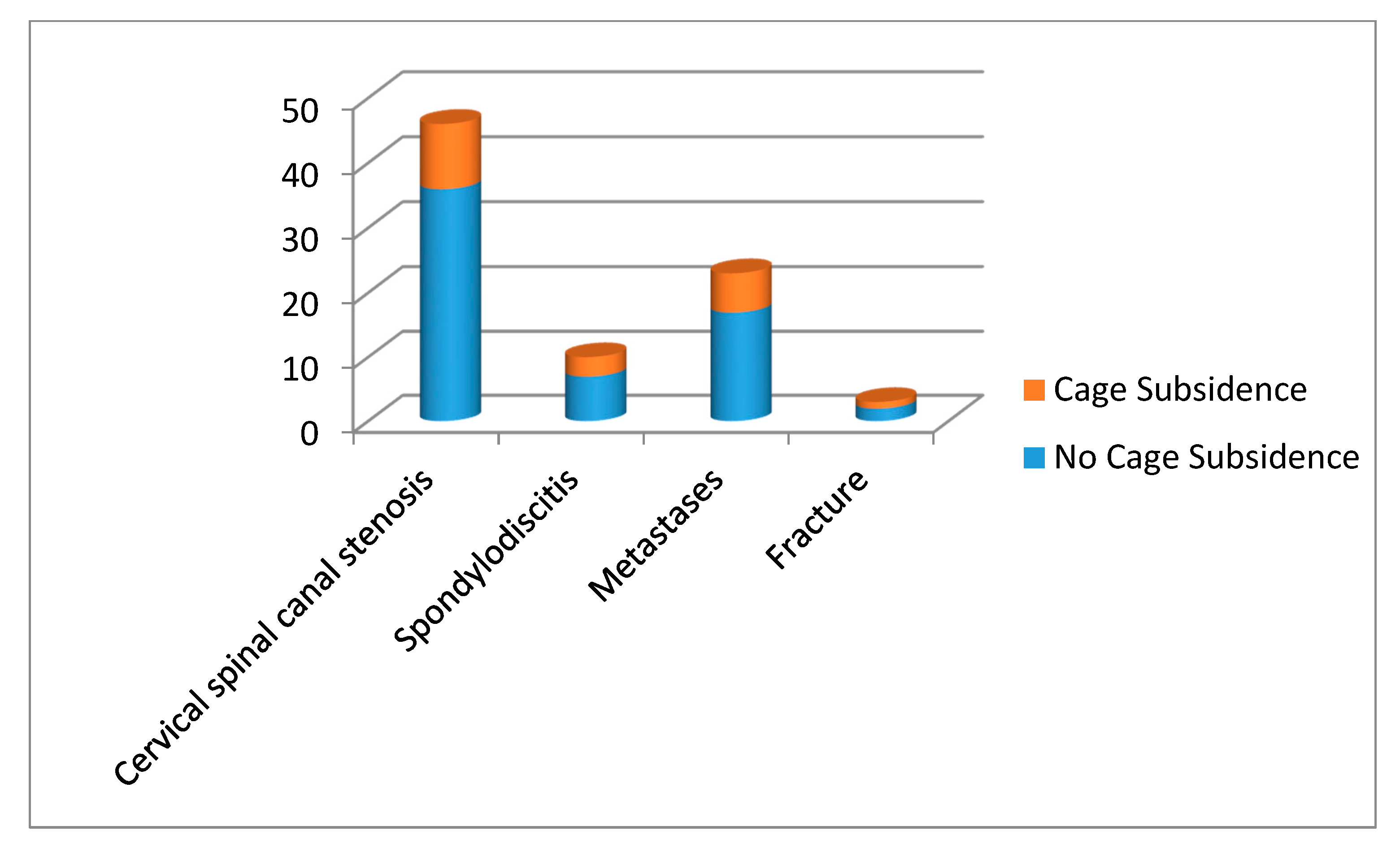
3. Results
3.1. Clinical Outcome
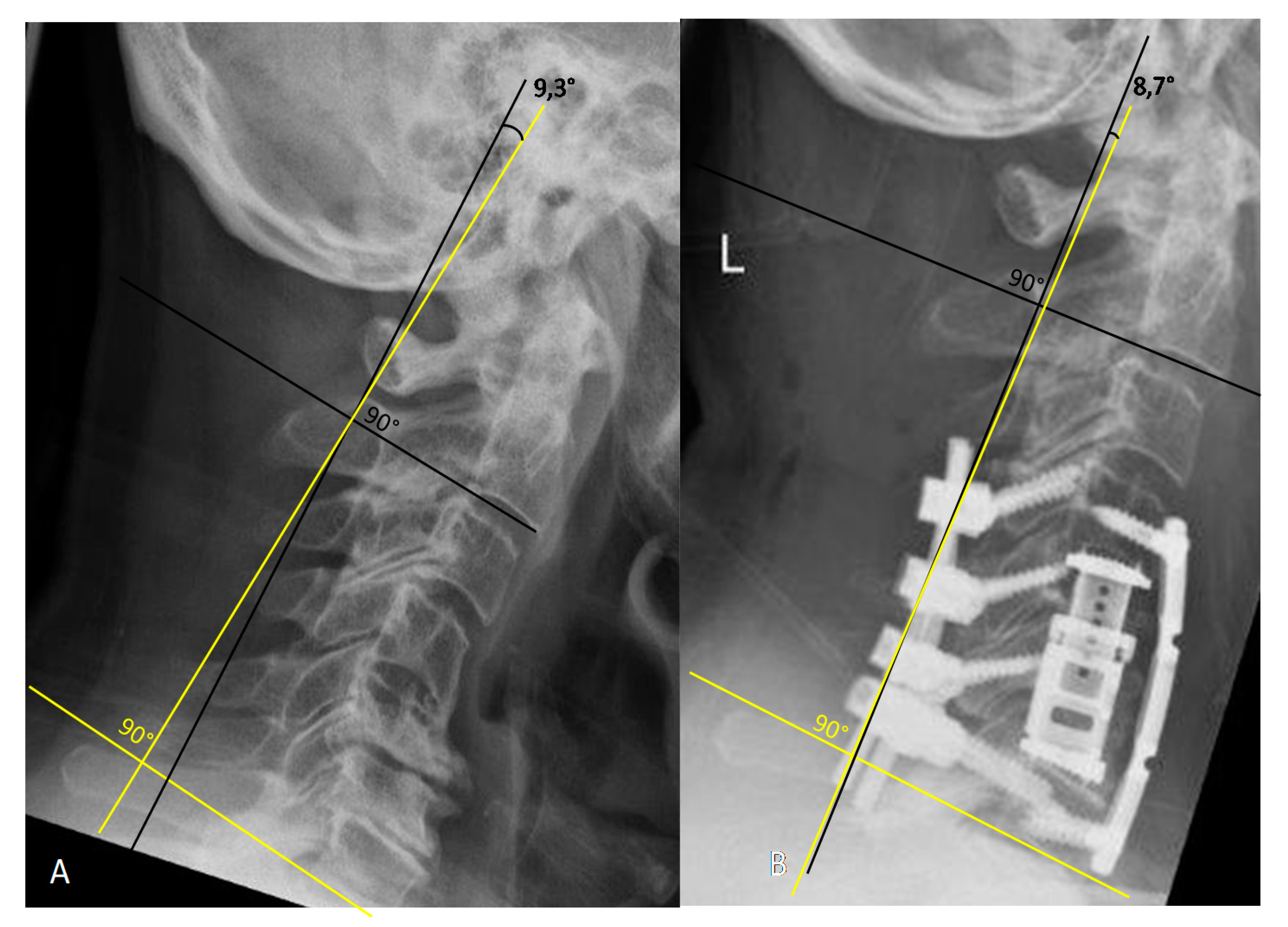
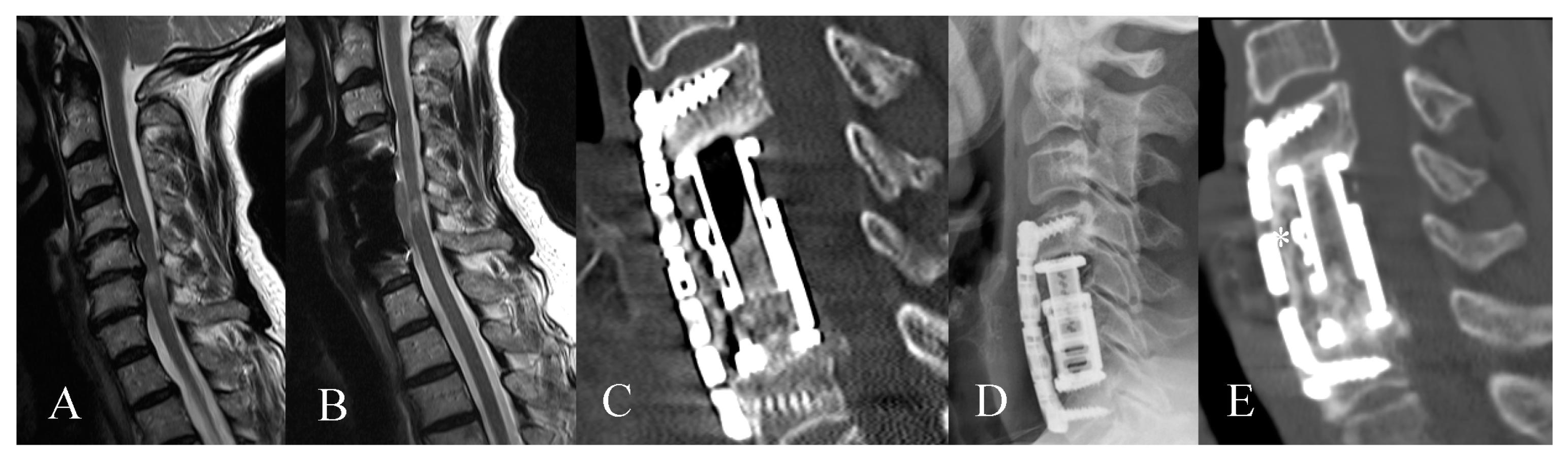
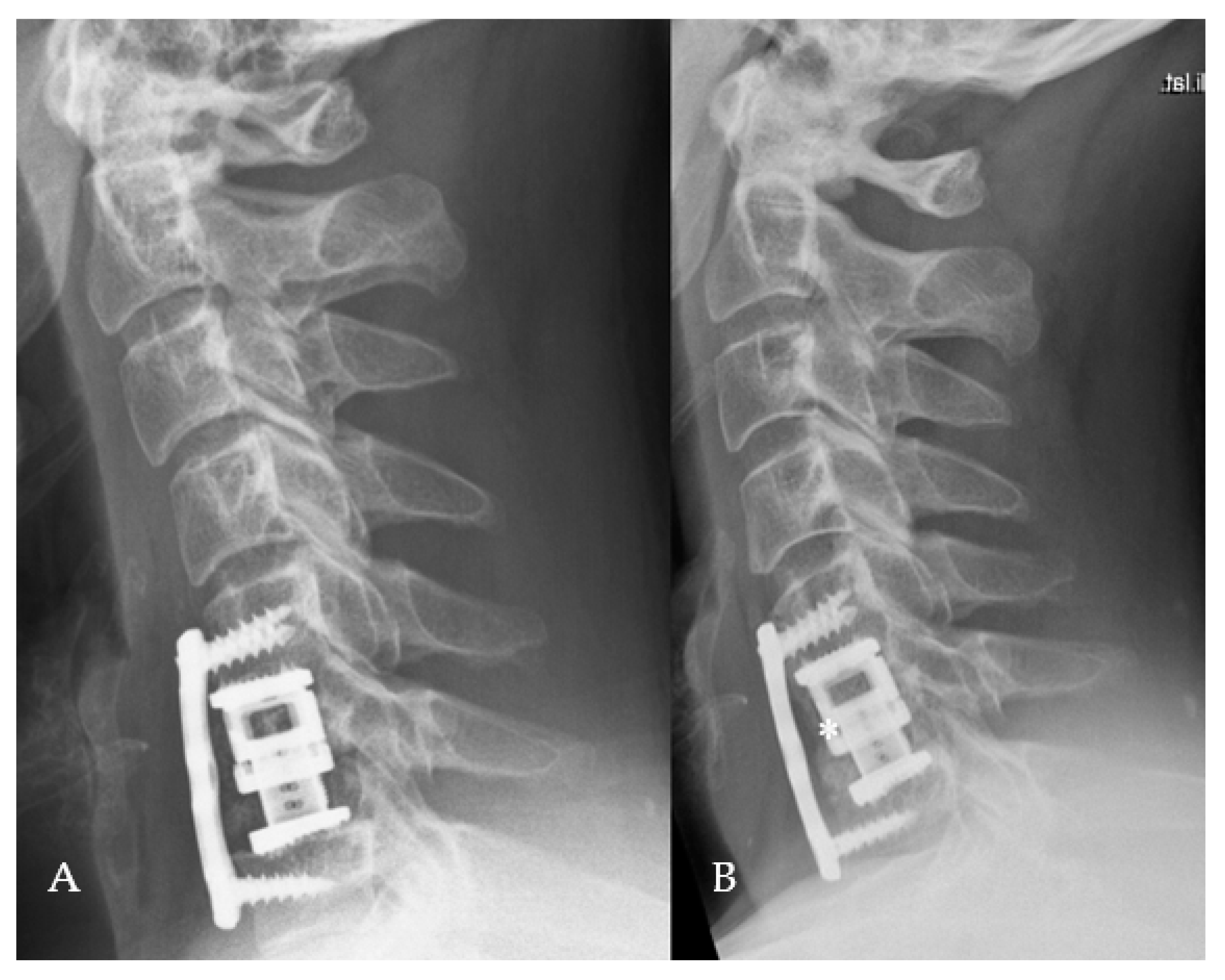
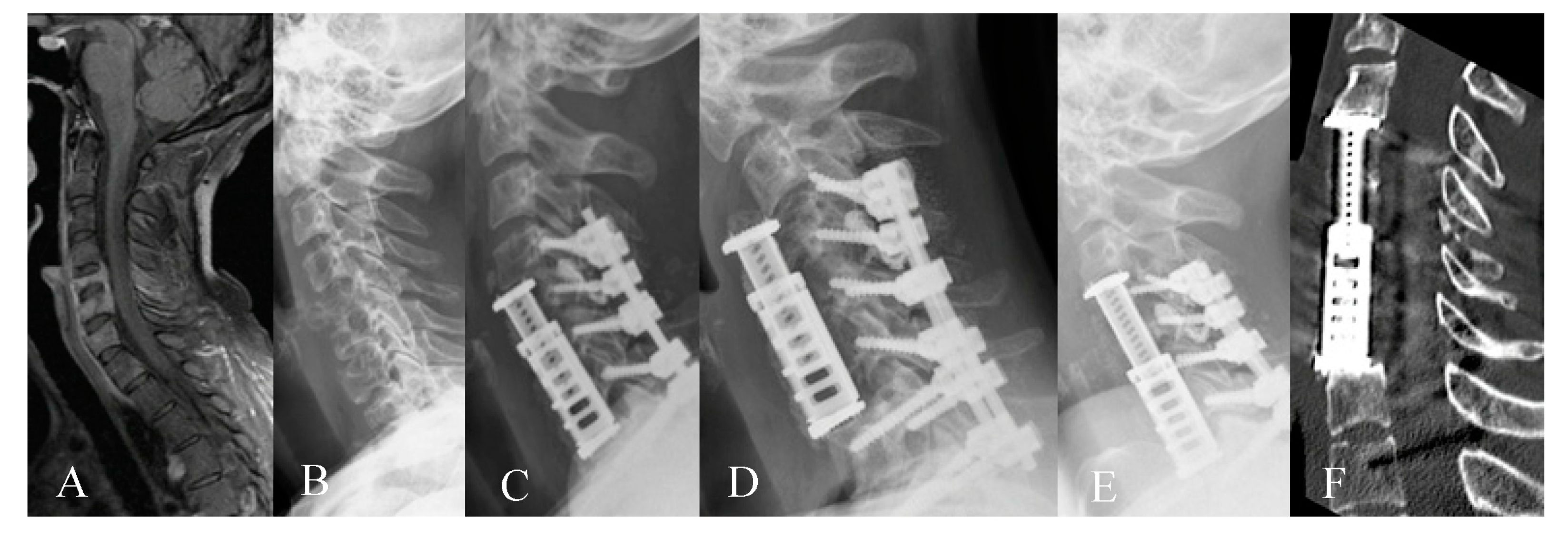
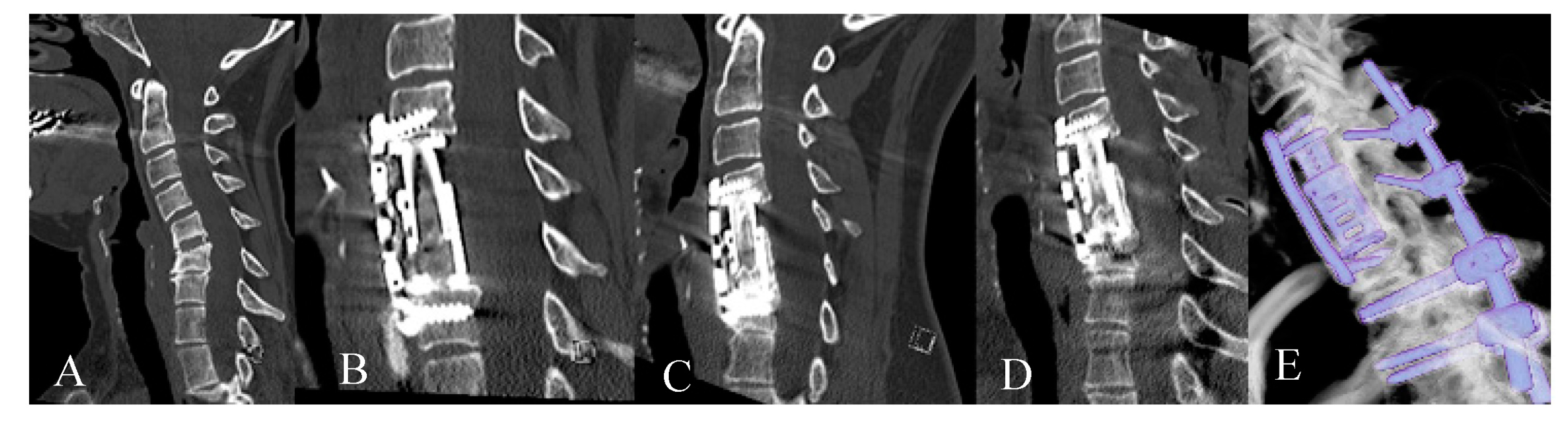
3.2. Radiological Outcome
3.3. Complications
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Waschke, A.; Kaczor, S.; Walter, J.; Duenisch, P.; Kalff, R.; Ewald, C. Expandable titanium cages for anterior column cervical reconstruction and their effect on sagittal profile: A review of 48 cases. Acta Neurochir. (Wien) 2013, 155, 801–807, discussion 807. [Google Scholar] [CrossRef]
- Vanni, D.; Pantalone, A.; Magliani, V.; Salini, V.; Berjano, P. Corpectomy and expandable cage replacement versus third generation percutaneous augmentation system in case of vertebra plana: Rationale and recommendations. J. Spine Surg. 2017, 3, 379–386. [Google Scholar] [CrossRef] [PubMed]
- Graillon, T.; Farah, K.; Rakotozanany, P.; Blondel, B.; Adetchessi, T.; Dufour, H.; Fuentes, S. Anterior approach with expandable cage implantation in management of unstable thoracolumbar fractures: Results of a series of 93 patients. Neurochirurgie 2016, 62, 78–85. [Google Scholar] [CrossRef] [PubMed]
- Calvert, G.; May, L.A.; Theiss, S. Use of permanently placed metal expandable cages for vertebral body reconstruction in the surgical treatment of spondylodiscitis. Orthopedics 2014, 37, e536–e542. [Google Scholar] [CrossRef] [PubMed]
- Alfieri, A.; Gazzeri, R.; Neroni, M.; Fiore, C.; Galarza, M.; Esposito, S. Anterior expandable cylindrical cage reconstruction after cervical spinal metastasis resection. Clin. Neurol. Neurosurg. 2011, 113, 914–917. [Google Scholar] [CrossRef]
- Cappelletto, B.; Giorgiutti, F.; Balsano, M. Evaluation of the effectiveness of expandable cages for reconstruction of the anterior column of the spine. J. Orthop. Surg. (Hong Kong) 2020, 28. [Google Scholar] [CrossRef]
- Woiciechowsky, C. Distractable vertebral cages for reconstruction after cervical corpectomy. Spine (Phila Pa 1976) 2005, 30, 1736–1741. [Google Scholar] [CrossRef]
- Elder, B.D.; Lo, S.F.; Kosztowski, T.A.; Goodwin, C.R.; Lina, I.A.; Locke, J.E.; Witham, T.F. A systematic review of the use of expandable cages in the cervical spine. Neurosurg. Rev. 2016, 39, 1–11, discussion 11. [Google Scholar] [CrossRef]
- Kao, T.H.; Wu, C.H.; Chou, Y.C.; Chen, H.T.; Chen, W.H.; Tsou, H.K. Risk factors for subsidence in anterior cervical fusion with stand-alone polyetheretherketone (PEEK) cages: A review of 82 cases and 182 levels. Arch. Orthop. Trauma Surg. 2014, 134, 1343–1351. [Google Scholar] [CrossRef]
- Viswanathan, A.; Abd-El-Barr, M.M.; Doppenberg, E.; Suki, D.; Gokaslan, Z.; Mendel, E.; Rao, G.; Rhines, L.D. Initial experience with the use of an expandable titanium cage as a vertebral body replacement in patients with tumors of the spinal column: A report of 95 patients. Eur. Spine J. 2012, 21, 84–92. [Google Scholar] [CrossRef][Green Version]
- Scheer, J.K.; Tang, J.A.; Smith, J.S.; Acosta, F.L.; Protopsaltis, T.S.; Blondel, B.; Bess, S.; Shaffrey, C.I.; Deviren, V.; Lafage, V.; et al. Cervical spine alignment, sagittal deformity, and clinical implications: A review. J. Neurosurg. Spine 2013, 19, 141–159. [Google Scholar] [CrossRef] [PubMed]
- Zaïri, F.; Aboukais, R.; Thines, L.; Allaoui, M.; Assaker, R. Relevance of expandable titanium cage for the treatment of cervical spondylotic myelopathy. Eur. Spine J. 2012, 21, 1545–1550. [Google Scholar] [CrossRef] [PubMed]
- Auguste, K.I.; Chin, C.; Acosta, F.L.; Ames, C.P. Expandable cylindrical cages in the cervical spine: A review of 22 cases. J. Neurosurg. Spine 2006, 4, 285–291. [Google Scholar] [CrossRef] [PubMed]
- Kandziora, F.; Pflugmacher, R.; Schaefer, J.; Scholz, M.; Ludwig, K.; Schleicher, P.; Haas, N.P. Biomechanical comparison of expandable cages for vertebral body replacement in the cervical spine. J. Neurosurg. 2003, 99 (Suppl. 1), 91–97. [Google Scholar] [CrossRef]
- Tarantino, R.; Nigro, L.; Donnarumma, P.; Rullo, M.; Santoro, A.; Delfini, R. Cervical reconstruction techniques. After adequate selection of the patient report of a series of 34 patients treated with winged expandable cages. Neurosurg. Rev. 2017, 40, 281–286. [Google Scholar] [CrossRef]
- Brenke, C.; Fischer, S.; Carolus, A.; Schmieder, K.; Ening, G. Complications associated with cervical vertebral body replacement with expandable titanium cages. J. Clin. Neurosci. 2016, 32, 35–40. [Google Scholar] [CrossRef]
- Joubert, C.; Adetchessi, T.; Peltier, E.; Graillon, T.; Dufour, H.; Blondel, B.; Fuentes, S. Corpectomy and Vertebral Body Reconstruction with Expandable Cage Placement and Osteosynthesis via the single stage Posterior Approach: A Retrospective Series of 34 Patients with Thoracic and Lumbar Spine Vertebral Body Tumors. World Neurosurg. 2015, 84, 1412–1422. [Google Scholar] [CrossRef]
- Lau, D.; Song, Y.; Guan, Z.; La Marca, F.; Park, P. Radiological outcomes of static vs. expandable titanium cages after corpectomy: A retrospective cohort analysis of subsidence. Neurosurgery 2013, 72, 529–539, discussion 528–529. [Google Scholar] [CrossRef]
- Keshavarzi, S.; Newman, C.B.; Ciacci, J.D.; Aryan, H.E. Expandable titanium cages for thoracolumbar vertebral body replacement: Initial clinical experience and review of the literature. Am. J. Orthop. 2011, 40, E35–E39. [Google Scholar]
- Burkett, C.J.; Baaj, A.A.; Dakwar, E.; Uribe, J.S. Use of titanium expandable vertebral cages in cervical corpectomy. J. Clin. Neurosci. 2012, 19, 402–405. [Google Scholar] [CrossRef]
- Payer, M. Implantation of a distractible titanium cage after cervical corpectomy: Technical experience in 20 consecutive cases. Acta Neurochir. (Wien) 2006, 148, 1173–1180, discussion 1180. [Google Scholar] [CrossRef] [PubMed]
- Nigro, L.; Tarantino, R.; Donnarumma, P.; Santoro, A.; Delfini, R. C5 palsy after insertion of a winged expandable cervical cage: A case report and literature review. J. Spine Surg. 2017, 3, 300–303. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Bydon, M.; Macki, M.; Kaloostian, P.; Sciubba, D.M.; Wolinsky, J.P.; Gokaslan, Z.L.; Belzberg, A.J.; Bydon, A.; Witham, T.F. Incidence and prognostic factors of c5 palsy: A clinical study of 1001 cases and review of the literature. Neurosurgery 2014, 74, 595–604, discussion 604–605. [Google Scholar] [CrossRef] [PubMed]
- Hashimoto, M.; Mochizuki, M.; Aiba, A.; Okawa, A.; Hayashi, K.; Sakuma, T.; Takahashi, H.; Koda, M.; Takahashi, K.; Yamazaki, M. C5 palsy following anterior decompression and spinal fusion for cervical degenerative diseases. Eur. Spine J. 2010, 19, 1702–1710. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Zhang, X.; Lv, B.; Ding, W.; Shen, Y.; Yang, D.; Bai, Z. Analysis of correlative risk factors for C5 palsy after anterior cervical decompression and fusion. Int. J. Clin. Exp. Med. 2015, 8, 3983–3991. [Google Scholar]
- Gu, Y.; Cao, P.; Gao, R.; Tian, Y.; Liang, L.; Wang, C.; Yang, L.; Yuan, W. Incidence and risk factors of C5 palsy following posterior cervical decompression: A systematic review. PLoS ONE 2014, 9, e101933. [Google Scholar] [CrossRef]
- Zairi, F.; Nzokou, A.; Sunna, T.; Obaid, S.; Weil, A.G.; Bojanowski, M.; Shedid, D. Minimally invasive costotransversectomy for the resection of large thoracic dumbbell tumors. Br. J. Neurosurg. 2017, 31, 179–183. [Google Scholar] [CrossRef]
- Song, K.J.; Choi, B.W.; Ham, D.H.; Kim, H.J. Prognosis of Hardware-Related Problems in Anterior Cervical Discectomy and Fusion with Cage and Plate Constructs. World Neurosurg. 2020, 134, e249–e255. [Google Scholar] [CrossRef]
- Hilibrand, A.S.; Robbins, M. Adjacent segment degeneration and adjacent segment disease: The consequences of spinal fusion? Spine J. 2004, 4 (Suppl. 6), 190S–194S. [Google Scholar] [CrossRef]
- Hashimoto, K.; Aizawa, T.; Kanno, H.; Itoi, E. Adjacent segment degeneration after fusion spinal surgery-a systematic review. Int. Orthop. 2019, 43, 987–993. [Google Scholar] [CrossRef]
- Chou, D.; Lu, D.C.; Weinstein, P.; Ames, C.P. Adjacent-level vertebral body fractures after expandable cage reconstruction. J. Neurosurg. Spine 2008, 8, 584–588. [Google Scholar] [CrossRef] [PubMed]
- Koller, H.; Hempfing, A.; Ferraris, L.; Maier, O.; Hitzl, W.; Metz-Stavenhagen, P. 4- and 5-level anterior fusions of the cervical spine: Review of literature and clinical results. Eur. Spine J. 2007, 16, 2055–2071. [Google Scholar] [CrossRef] [PubMed]
- Sasso, R.C.; Ruggiero, R.A.; Reilly, T.M.; Hall, P.V. Early reconstruction failures after multilevel cervical corpectomy. Spine (Phila Pa 1976) 2003, 28, 140–142. [Google Scholar] [CrossRef] [PubMed]
- Butler, J.S.; Morrissey, P.B.; Wagner, S.C.; Kaye, I.D.; Sebastian, A.S.; Schroeder, G.D.; Vaccaro, A.R.; Hilibrand, A.S. Surgical Strategies to Prevent Adjacent Segment Disease in the Cervical Spine. Clin. Spine Surg. 2019, 32, 91–97. [Google Scholar] [CrossRef] [PubMed]
- Emstad, E.; Del Monaco, D.C.; Fielding, L.C.; Block, J.E. The VariLift(®) Interbody Fusion System: Expandable, standalone interbody fusion. Med. Devices (Auckl.) 2015, 8, 219–230. [Google Scholar]
- Rhee, J.M.; Park, J.B.; Yang, J.Y.; Riew, D.K. Indications and techniques for anterior cervical plating. Neurol. India 2005, 53, 433–439. [Google Scholar]
- Utter, A.; Benzel, E.C. Anterior Cervical Corpectomy and Fusion to Plate or Not to Plate. In Benzel’s Spine Surgery, 2-Volume Set, 4th ed.; Steinmetz, M.P., Benzel, E.C., Eds.; Elsevier: Amsterdam, The Netherlands, 2015. [Google Scholar]
- Vaccaro, A.R.; Falatyn, S.P.; Scuderi, G.J.; Eismont, F.J.; McGuire, R.A.; Singh, K.; Garfin, S.R. Early failure of long segment anterior cervical plate fixation. J. Spinal Disord. 1998, 11, 410–415. [Google Scholar] [CrossRef]
- Do Koh, Y.; Lim, T.H.; Won You, J.; Eck, J.; An, H.S. A biomechanical comparison of modern anterior and posterior plate fixation of the cervical spine. Spine (Phila Pa 1976) 2001, 26, 15–21. [Google Scholar] [CrossRef]
- Riew, K.D.; Hilibrand, A.S.; Palumbo, M.A.; Bohlman, H.H. Anterior cervical corpectomy in patients previously managed with a laminectomy: Short-term complications. J. Bone Joint Surg. Am. 1999, 81, 950–957. [Google Scholar] [CrossRef]


| Patient Characteristics | Number |
|---|---|
| Gender | |
| Male | 45 (52.3%) |
| Female | 41 (47.7%) |
| Mean age | 61.3 years (11–89) |
| Mean follow-up | 30.7 months |
| Mean surgery time | 191 min (67–447) |
| Mean hospital stay | 10.6 days (3–53) |
| Indications | |
| Spinal canal stenosis with myelopathy | 46 (53.5%) |
| Metastasis | 24 (27.9%) |
| Spondylodiscitis | 12 (14%) |
| Fracture | 4 (4.6%) |
| Operative therapy at primary surgery | |
| Standalone | 47 (54.6%) |
| Without plate | 13 |
| With plate | 34 |
| 360° fusion | 39 (45.4%) |
| Without plate | 28 |
| With plate | 11 |
| Corpectomy level at primary surgery | |
| Single level | 34 (39.5%) |
| C2 | 1 |
| C3 | 3 |
| C4 | 5 |
| C5 | 9 |
| C6 | 11 |
| C7 | 5 |
| Standalone | 14 |
| Without plate | 5 |
| With plate | 9 |
| 360° fusion | 20 |
| Without plate | 12 |
| With plate | 8 |
| Multiple level | 52 (60.5%) |
| C3 and C4 | 2 |
| C4 and C5 | 13 |
| C5 and C6 | 24 |
| C6 and C7 | 5 |
| C7 and Th1 | 2 |
| C4,5,6 | 2 |
| C5,6,7 | 1 |
| C4,5,6,7 | 1 |
| C5,6,7, Th1 | 1 |
| C7, Th1, Th2 | 1 |
| Standalone | 33 |
| Without plate | 8 |
| With plate | 25 |
| 360° fusion | 19 |
| Without plate | 16 |
| With plate | 3 |
| Levels of dorsal stabilization at primary surgery | 39 |
| C0-C5 | 1 |
| C1–7 | 1 |
| C2–4 | 1 |
| C2–5 | 2 |
| C2–6 | 1 |
| C3–5 | 1 |
| C3–6 | 7 |
| C3–7 | 3 |
| C4–6 | 3 |
| C4–7 | 3 |
| C5–7 | 3 |
| C2-Th1 | 1 |
| C3-Th1 | 1 |
| C3-Th2 | 1 |
| C3-Th3 | 2 |
| C4-Th1 | 1 |
| C4-Th4 | 2 |
| C5-Th2 | 1 |
| C6-Th1 | 1 |
| Th2–8 | 1 |
| Th6–10 | 1 |
| Th3–12 | 1 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pojskic, M.; Saβ, B.; Nimsky, C.; Carl, B. Application of an Expandable Cage for Reconstruction of the Cervical Spine in a Consecutive Series of Eighty-Six Patients. Medicina 2020, 56, 642. https://doi.org/10.3390/medicina56120642
Pojskic M, Saβ B, Nimsky C, Carl B. Application of an Expandable Cage for Reconstruction of the Cervical Spine in a Consecutive Series of Eighty-Six Patients. Medicina. 2020; 56(12):642. https://doi.org/10.3390/medicina56120642
Chicago/Turabian StylePojskic, Mirza, Benjamin Saβ, Christopher Nimsky, and Barbara Carl. 2020. "Application of an Expandable Cage for Reconstruction of the Cervical Spine in a Consecutive Series of Eighty-Six Patients" Medicina 56, no. 12: 642. https://doi.org/10.3390/medicina56120642
APA StylePojskic, M., Saβ, B., Nimsky, C., & Carl, B. (2020). Application of an Expandable Cage for Reconstruction of the Cervical Spine in a Consecutive Series of Eighty-Six Patients. Medicina, 56(12), 642. https://doi.org/10.3390/medicina56120642







