The (Patho)Biology of SRC Kinase in Platelets and Megakaryocytes
Abstract
1. Introduction to SRC and SRC Family Kinases
2. SRC Kinase Activity in Platelets in Health and Disease
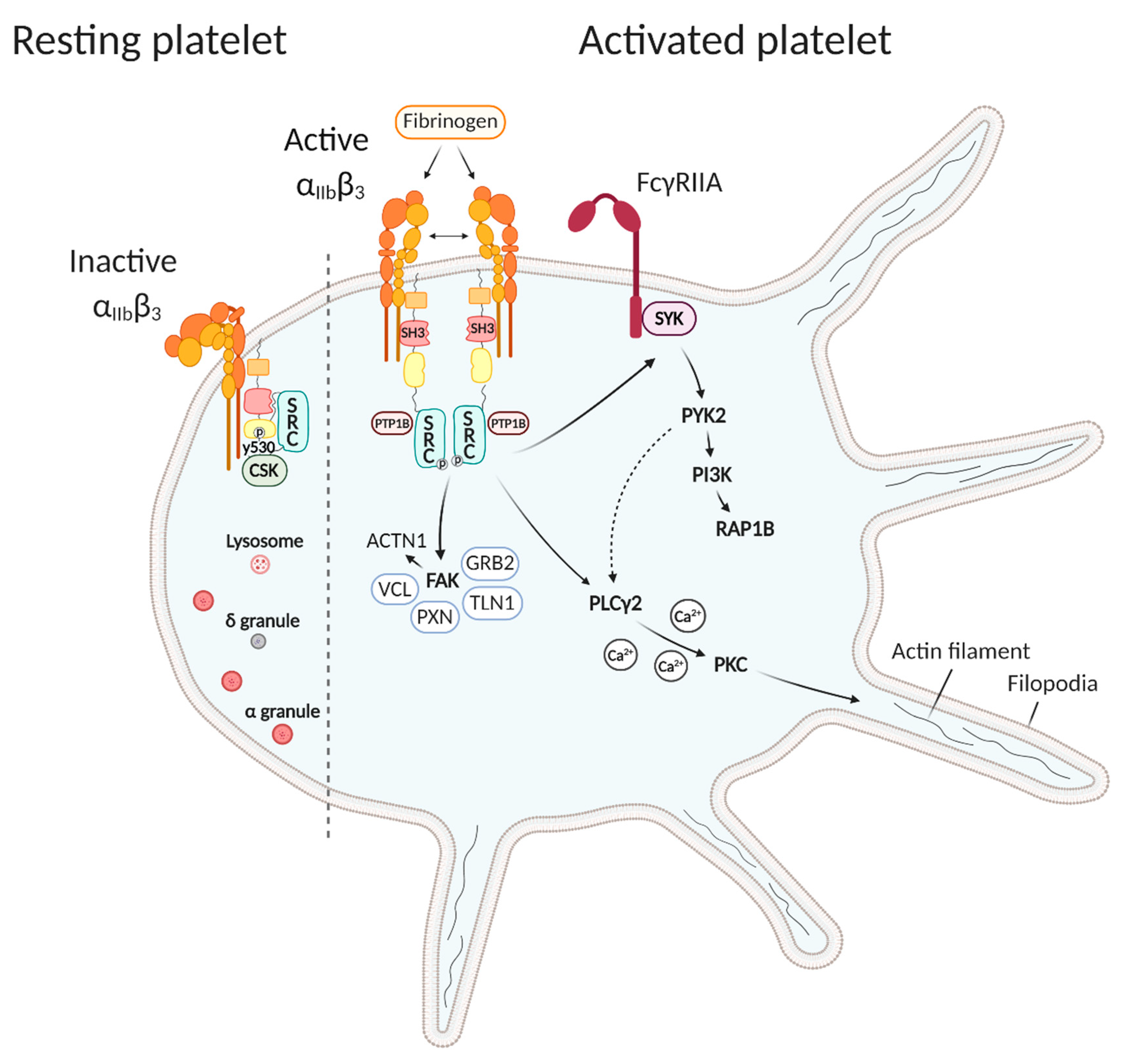
2.1. SRC Kinase Regulates Platelet Activation
2.2. SRC Kinase Deficiency Impairs Platelet Function
3. SRC Kinase activity in Megakaryocytes in Health and Disease
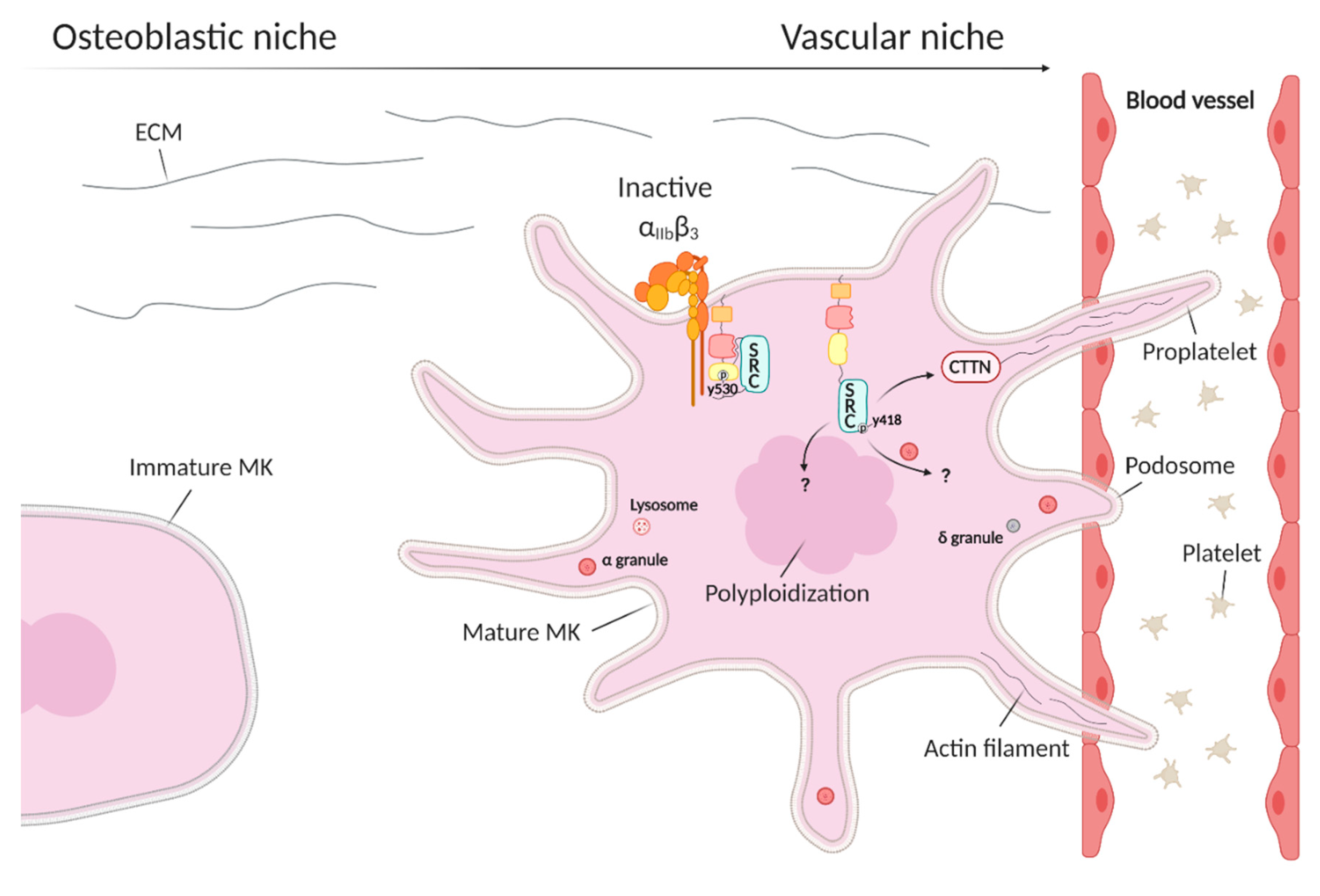
3.1. SRC Kinase Regulates Megakaryopoiesis
3.2. SRC Kinase Deficiency Impairs Megakaryopoiesis
4. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Weiss, R.A.; Vogt, P.K. 100 years of Rous sarcoma virus. J. Exp. Med. 2011, 208, 2351–2355. [Google Scholar] [CrossRef]
- Sefton, B.M.; Hunter, T.; Beemon, K.; Eckhart, W. Evidence that the phosphorylation of tyrosine is essential for cellular transformation by Rous sarcoma virus. Cell 1980, 20, 807–816. [Google Scholar] [CrossRef]
- Hunter, T. Discovering the first tyrosine kinase. Proc. Natl. Acad. Sci. USA 2015, 112, 7877–7882. [Google Scholar] [CrossRef] [PubMed]
- Gibbs, C.P.; Tanaka, A.; Anderson, S.K.; Radul, J.; Baar, J.; Ridgway, A.; Kung, H.J.; Fujita, D.J. Isolation and structural mapping of a human c-src gene homologous to the transforming gene (v-src) of Rous sarcoma virus. J. Virol. 1985, 53, 19–24. [Google Scholar] [CrossRef] [PubMed]
- Wilkerson, V.W.; Bryant, D.L.; Parsons, J.T. Rous sarcoma virus variants that encode src proteins with an altered carboxy terminus are defective for cellular transformation. J. Virol. 1985, 55, 314–321. [Google Scholar] [CrossRef] [PubMed]
- Roskoski, R. Src kinase regulation by phosphorylation and dephosphorylation. Biochem. Biophys. Res. Commun. 2005, 331, 1–14. [Google Scholar] [CrossRef]
- Xu, W.; Harrison, S.C.; Eck, M.J. Three-dimensional structure of the tyrosine kinase c-Src. Nat. Cell Biol. 1997, 385, 595–602. [Google Scholar] [CrossRef] [PubMed]
- Ku, M.; Wall, M.; MacKinnon, R.N.; Walkley, C.R.; Purton, L.E.; Tam, C.; Izon, D.; Campbell, L.; Cheng, H.-C.; Nandurkar, H. Src family kinases and their role in hematological malignancies. Leuk. Lymphoma 2015, 56, 577–586. [Google Scholar] [CrossRef]
- Irby, R.B.; Mao, W.; Coppola, D.; Kang, J.; Loubeau, J.M.; Trudeau, W.L.; Karl, R.C.; Fujita, D.J.; Jove, R.; Yeatman, T.J. Activating SRC mutation in a subset of advanced human colon cancers. Nat. Genet. 1999, 21, 187–190. [Google Scholar] [CrossRef]
- Sugimura, M.; Kobayashi, K.; Sagae, S.; Nishioka, Y.; Ishioka, S.-I.; Terasawa, K.; Tokino, T.; Kudo, R. Mutation of theSRCGene in Endometrial Carcinoma. Jpn. J. Cancer Res. 2000, 91, 395–398. [Google Scholar] [CrossRef]
- Senis, Y.A.; Mazharian, A.; Mori, J. Src family kinases: At the forefront of platelet activation. Blood 2014, 124, 2013–2024. [Google Scholar] [CrossRef] [PubMed]
- Golden, A.; Nemeth, S.P.; Brugge, J.S. Blood platelets express high levels of the pp60c-src-specific tyrosine kinase activity. Proc. Natl. Acad. Sci. USA 1986, 83, 852–856. [Google Scholar] [CrossRef] [PubMed]
- Séverin, S.; Nash, C.A.; Mori, J.; Zhao, Y.; Abram, C.; Lowell, C.A.; Senis, Y.A.; Watson, S.P. Distinct and overlapping functional roles of Src family kinases in mouse platelets. J. Thromb. Haemost. 2012, 10, 1631–1645. [Google Scholar] [CrossRef] [PubMed]
- Durrant, T.N.; Bosch, M.T.V.D.; Hers, I. Integrin αIIbβ3 outside-in signaling. Blood 2017, 130, 1607–1619. [Google Scholar] [CrossRef]
- Arias-Salgado, E.G.; Lizano, S.; Sarkar, S.; Brugge, J.S.; Ginsberg, M.H.; Shattil, S.J. Src kinase activation by direct interaction with the integrin cytoplasmic domain. Proc. Natl. Acad. Sci. USA 2003, 100, 13298–13302. [Google Scholar] [CrossRef]
- Obergfell, A.; Eto, K.; Mocsai, A.; Buensuceso, C.; Moores, S.L.; Brugge, J.S.; Lowell, C.A.; Shattil, S.J. Coordinate interactions of Csk, Src, and Syk kinases with αIIbβ3 initiate integrin signaling to the cytoskeleton. J. Cell Biol. 2002, 157, 265–275. [Google Scholar] [CrossRef]
- Fong, K.P.; Zhu, H.; Span, L.M.; Moore, D.T.; Yoon, K.; Tamura, R.; Yin, H.; DeGrado, W.F.; Bennett, J.S. Directly Activating the Integrin αIIbβ3 Initiates Outside-In Signaling by Causing αIIbβ3 Clustering. J. Biol. Chem. 2016, 291, 11706–11716. [Google Scholar] [CrossRef]
- Arias-Salgado, E.G.; Haj, F.; Dubois, C.; Moran, B.; Kasirer-Friede, A.; Furie, B.C.; Furie, B.; Neel, B.G.; Shattil, S.J. PTP-1B is an essential positive regulator of platelet integrin signaling. J. Cell Biol. 2005, 170, 837–845. [Google Scholar] [CrossRef]
- Calaminus, S.D.; Thomas, S.G.; Mccarty, O.J.T.; Machesky, L.M.; Watson, S.P. Identification of a novel, actin-rich structure, the actin nodule, in the early stages of platelet spreading. J. Thromb. Haemost. 2008, 6, 1944–1952. [Google Scholar] [CrossRef]
- Poulter, N.S.; Pollitt, A.Y.; Davies, A.; Malinova, D.; Nash, G.B.; Hannon, M.J.; Pikramenou, Z.; Rappoport, J.Z.; Hartwig, J.H.; Owen, D.M.; et al. Platelet actin nodules are podosome-like structures dependent on Wiskott–Aldrich syndrome protein and ARP2/3 complex. Nat. Commun. 2015, 6, 7254. [Google Scholar] [CrossRef]
- Boylan, B.; Gao, C.; Rathore, V.; Gill, J.C.; Newman, D.K.; Newman, P.J. Identification of FcγRIIa as the ITAM-bearing receptor mediating αIIbβ3 outside-in integrin signaling in human platelets. Blood 2008, 112, 2780–2786. [Google Scholar] [CrossRef]
- Cipolla, L.; Consonni, A.; Guidetti, G.; Canobbio, I.; Okigaki, M.; Falasca, M.; Ciraolo, E.; Hirsch, E.; Balduini, C.; Torti, M. The proline-rich tyrosine kinase Pyk2 regulates platelet integrin αIIbβ3 outside-in signaling. J. Thromb. Haemost. 2013, 11, 345–356. [Google Scholar] [CrossRef] [PubMed]
- Goncalves, I.; Hughan, S.C.; Schoenwaelder, S.M.; Yap, C.L.; Yuan, Y.; Jackson, S.P. Integrin αIIbβ3-dependent Calcium Signals Regulate Platelet-Fibrinogen Interactions under Flow. J. Biol. Chem. 2003, 278, 34812–34822. [Google Scholar] [CrossRef] [PubMed]
- Wonerow, P.; Pearce, A.C.; Vaux, D.J.; Watson, S.P. A Critical Role for Phospholipase Cγ2 in αIIbβ3-mediated Platelet Spreading. J. Biol. Chem. 2003, 278, 37520–37529. [Google Scholar] [CrossRef]
- Izaguirre, G.; Aguirre, L.; Hu, Y.-P.; Lee, H.Y.; Schlaepfer, D.D.; Aneskievich, B.J.; Haimovich, B. The Cytoskeletal/Non-muscle Isoform of α-Actinin Is Phosphorylated on Its Actin-binding Domain by the Focal Adhesion Kinase. J. Biol. Chem. 2001, 276, 28676–28685. [Google Scholar] [CrossRef] [PubMed]
- Lipfert, L.; Haimovich, B.; Schaller, M.D.; Cobb, B.S.; Parsons, J.T.; Brugge, J.S. Integrin-dependent phosphorylation and activation of the protein tyrosine kinase pp125FAK in platelets. J. Cell Biol. 1992, 119, 905–912. [Google Scholar] [CrossRef] [PubMed]
- Hitchcock, I.S.; Fox, N.E.; Prévost, N.; Sear, K.; Shattil, S.J.; Kaushansky, K. Roles of focal adhesion kinase (FAK) in megakaryopoiesis and platelet function: Studies using a megakaryocyte lineage–specific FAK knockout. Blood 2008, 111, 596–604. [Google Scholar] [CrossRef][Green Version]
- Zhang, Z.; Izaguirre, G.; Lin, S.-Y.; Lee, H.Y.; Schaefer, E.; Haimovich, B. The Phosphorylation of Vinculin on Tyrosine Residues 100 and 1065, Mediated by Src Kinases, Affects Cell Spreading. Mol. Biol. Cell 2004, 15, 4234–4247. [Google Scholar] [CrossRef]
- Haling, J.R.; Monkley, S.J.; Critchley, D.R.; Petrich, B.G. Talin-dependent integrin activation is required for fibrin clot retraction by platelets. Blood 2011, 117, 1719–1722. [Google Scholar] [CrossRef]
- Gao, W.; Shi, P.; Chen, X.; Zhang, L.; Liu, J.; Fan, X.; Luo, X. Clathrin-mediated integrin αIIbβ3 trafficking controls platelet spreading. Platelets 2017, 29, 610–621. [Google Scholar] [CrossRef]
- Giuriato, S.; Bodin, S.; Erneux, C.; Woscholski, R.; Plantavid, M.; Chap, H.; Payrastre, B. pp60c-src associates with the SH2-containing inositol-5-phosphatase SHIP1 and is involved in its tyrosine phosphorylation downstream of αIIbβ3 integrin in human platelets. Biochem. J. 2000, 348, 107. [Google Scholar] [CrossRef]
- Shen, C.; Liu, M.; Xu, R.; Wang, G.; Li, J.; Chen, P.; Ma, W.; Mwangi, J.; Lu, Q.; Duan, Z.; et al. The 14-3-3ζ–c-Src–integrin-β3 complex is vital for platelet activation. Blood 2020, 136, 974–988. [Google Scholar] [CrossRef]
- Wu, Y.; Asazuma, N.; Satoh, K.; Yatomi, Y.; Takafuta, T.; Berndt, M.C.; Ozaki, Y. Interaction between von Willebrand factor and glycoprotein Ib activates Src kinase in human platelets: Role of phosphoinositide 3–kinase. Blood 2003, 101, 3469–3476. [Google Scholar] [CrossRef] [PubMed]
- Nieswandt, B.; Watson, S.P. Platelet-collagen interaction: Is GPVI the central receptor? Blood 2003, 102, 449–461. [Google Scholar] [CrossRef] [PubMed]
- Suzuki-Inoue, K.; Tulasne, D.; Shen, Y.; Bori-Sanz, T.; Inoue, O.; Jung, S.M.; Moroi, M.; Andrews, R.K.; Berndt, M.C.; Watson, S.P. Association of Fyn and Lyn with the Proline-rich Domain of Glycoprotein VI Regulates Intracellular Signaling. J. Biol. Chem. 2002, 277, 21561–21566. [Google Scholar] [CrossRef] [PubMed]
- Rollin, J.; Pouplard, C.; Gratacap, M.-P.; Leroux, D.; May, M.-A.; Aupart, M.; Gouilleux-Gruart, V.; Payrastre, B.; Gruel, Y. Polymorphisms of protein tyrosine phosphatase CD148 influence FcγRIIA-dependent platelet activation and the risk of heparin-induced thrombocytopenia. Blood 2012, 120, 1309–1316. [Google Scholar] [CrossRef]
- Soriano, P.; Montgomery, C.; Geske, R.; Bradley, A. Targeted disruption of the c-src proto-oncogene leads to osteopetrosis in mice. Cell 1991, 64, 693–702. [Google Scholar] [CrossRef]
- Harrison, M.J.; Chimen, M.; Hussain, M.; Iqbal, A.J.; Senis, Y.A.; Nash, G.B.; Watson, S.P.; Rainger, G.E. Signalling through Src family kinase isoforms is not redundant in models of thrombo-inflammatory vascular disease. J. Cell. Mol. Med. 2018, 22, 4317–4327. [Google Scholar] [CrossRef]
- Ablooglu, A.J.; Kang, J.; Petrich, B.G.; Ginsberg, M.H.; Shattil, S.J. Antithrombotic effects of targeting αIIbβ3 signaling in platelets. Blood 2009, 113, 3585–3592. [Google Scholar] [CrossRef]
- Mori, J.; Nagy, Z.; Di Nunzio, G.; Smith, C.W.; Geer, M.J.; Al Ghaithi, R.; Van Geffen, J.P.; Heising, S.; Boothman, L.; Tullemans, B.M.E.; et al. Maintenance of murine platelet homeostasis by the kinase Csk and phosphatase CD148. Blood 2018, 131, 1122–1144. [Google Scholar] [CrossRef]
- Gratacap, M.-P.; Martin, V.; Valéra, M.-C.; Allart, S.; Garcia, C.; Sié, P.; Recher, C.; Payrastre, B. The new tyrosine-kinase inhibitor and anticancer drug dasatinib reversibly affects platelet activation in vitro and in vivo. Blood 2009, 114, 1884–1892. [Google Scholar] [CrossRef] [PubMed]
- Turro, E.; Greene, D.; Wijgaerts, A.; Thys, C.; Lentaigne, C.; Bariana, T.K.; Papadia, S. A dominant gain-of-function mutation in universal tyrosine kinase SRC causes thrombocytopenia, myelofibrosis, bleeding, and bone pathologies. Sci. Transl. Med. 2016, 8, 328ra30. [Google Scholar] [CrossRef] [PubMed]
- De Kock, L.; Thys, C.; Downes, K.; Duarte, D.; Megy, K.; Van Geet, C.; Freson, K. De novo variant in tyrosine kinase SRC causes thrombocytopenia: Case report of a second family. Platelets 2019, 30, 931–934. [Google Scholar] [CrossRef] [PubMed]
- Barozzi, S.; Di Buduo, C.A.; Marconi, C.; Bozzi, V.; Seri, M.; Romano, F.; Balduini, A.; Pecci, A. Pathogenetic and clinical study of a patient with thrombocytopenia due to the p.E527K gain-of-function variant of SRC. Haematology 2020. [Google Scholar] [CrossRef]
- Tullemans, B.M.; Heemskerk, J.W.M.; Kuijpers, M.J.E. Acquired platelet antagonism: Off-target antiplatelet effects of malignancy treatment with tyrosine kinase inhibitors. J. Thromb. Haemost. 2018, 16, 1686–1699. [Google Scholar] [CrossRef] [PubMed]
- Jackson, C.W.; Steward, S.A.; Hutson, N.K.; McDonald, T.P. Genetic and physiological variations in megakaryocyte dna content distributions. Stem Cells 1990, 8, 260–266. [Google Scholar] [CrossRef]
- Machlus, K.R.; Italiano, J.J.E. The incredible journey: From megakaryocyte development to platelet formation. J. Cell Biol. 2013, 201, 785–796. [Google Scholar] [CrossRef]
- Schachtner, H.; Calaminus, S.D.J.; Sinclair, A.; Monypenny, J.; Blundell, M.P.; Leon, C.; Holyoake, T.L.; Thrasher, A.J.; Michie, A.M.; Vukovic, M.; et al. Megakaryocytes assemble podosomes that degrade matrix and protrude through basement membrane. Blood 2013, 121, 2542–2552. [Google Scholar] [CrossRef]
- Lannutti, B.J.; Blake, N.; Gandhi, M.J.; Reems, J.A.; Drachman, J.G. Induction of polyploidization in leukemic cell lines and primary bone marrow by Src kinase inhibitor SU6656. Blood 2005, 105, 3875–3878. [Google Scholar] [CrossRef][Green Version]
- Zou, X.; Qu, M.; Fang, F.; Fan, Z.; Chen, L.; Yue, W.; Xie, X.; Pei, X. Small Molecule Supplements Improve Cultured Megakaryocyte Polyploidization by Modulating Multiple Cell Cycle Regulators. BioMed. Res. Int. 2017, 2017, 1–12. [Google Scholar] [CrossRef]
- Jarocha, D.; Vo, K.K.; Lyde, R.B.; Hayes, V.; Camire, R.M.; Poncz, M. Enhancing functional platelet release in vivo from in vitro–grown megakaryocytes using small molecule inhibitors. Blood Adv. 2018, 2, 597–606. [Google Scholar] [CrossRef]
- Avanzi, M.P.; Chen, A.; He, W.; Mitchell, W.B. Optimizing megakaryocyte polyploidization by targeting multiple pathways of cytokinesis. Transfusion 2012, 52, 2406–2413. [Google Scholar] [CrossRef] [PubMed]
- Mazharian, A.; Ghevaert, C.; Zhang, L.; Massberg, S.; Watson, S.P. Dasatinib enhances megakaryocyte differentiation but inhibits platelet formation. Blood 2011, 117, 5198–5206. [Google Scholar] [CrossRef]
- Zhan, X.; Haudenschild, C.C.; Ni, Y.; Smith, E.; Huang, C. Upregulation of Cortactin Expression During the Maturation of Megakaryocytes. Blood 1997, 89, 457–464. [Google Scholar] [CrossRef] [PubMed]
- Larson, M.K.; Watson, S.P. Regulation of proplatelet formation and platelet release by integrin αIIbβ3. Blood 2006, 108, 1509–1514. [Google Scholar] [CrossRef] [PubMed]
- Mazharian, A.; Thomas, S.G.; Dhanjal, T.S.; Buckley, C.D.; Watson, S.P.; Thomas, S.G. Critical role of Src-Syk-PLCγ2 signaling in megakaryocyte migration and thrombopoiesis. Blood 2010, 116, 793–800. [Google Scholar] [CrossRef] [PubMed]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
De Kock, L.; Freson, K. The (Patho)Biology of SRC Kinase in Platelets and Megakaryocytes. Medicina 2020, 56, 633. https://doi.org/10.3390/medicina56120633
De Kock L, Freson K. The (Patho)Biology of SRC Kinase in Platelets and Megakaryocytes. Medicina. 2020; 56(12):633. https://doi.org/10.3390/medicina56120633
Chicago/Turabian StyleDe Kock, Lore, and Kathleen Freson. 2020. "The (Patho)Biology of SRC Kinase in Platelets and Megakaryocytes" Medicina 56, no. 12: 633. https://doi.org/10.3390/medicina56120633
APA StyleDe Kock, L., & Freson, K. (2020). The (Patho)Biology of SRC Kinase in Platelets and Megakaryocytes. Medicina, 56(12), 633. https://doi.org/10.3390/medicina56120633





