Qualitative Assessment of Vaccine Hesitancy in Romania
Abstract
1. Introduction
“Vaccine hesitancy refers to delay in acceptance or refusal of vaccination despite availability of vaccination services. Vaccine hesitancy is complex and context specific, varying across time, place, and vaccines. It is influenced by factors such as complacency, convenience, and confidence”.[6]
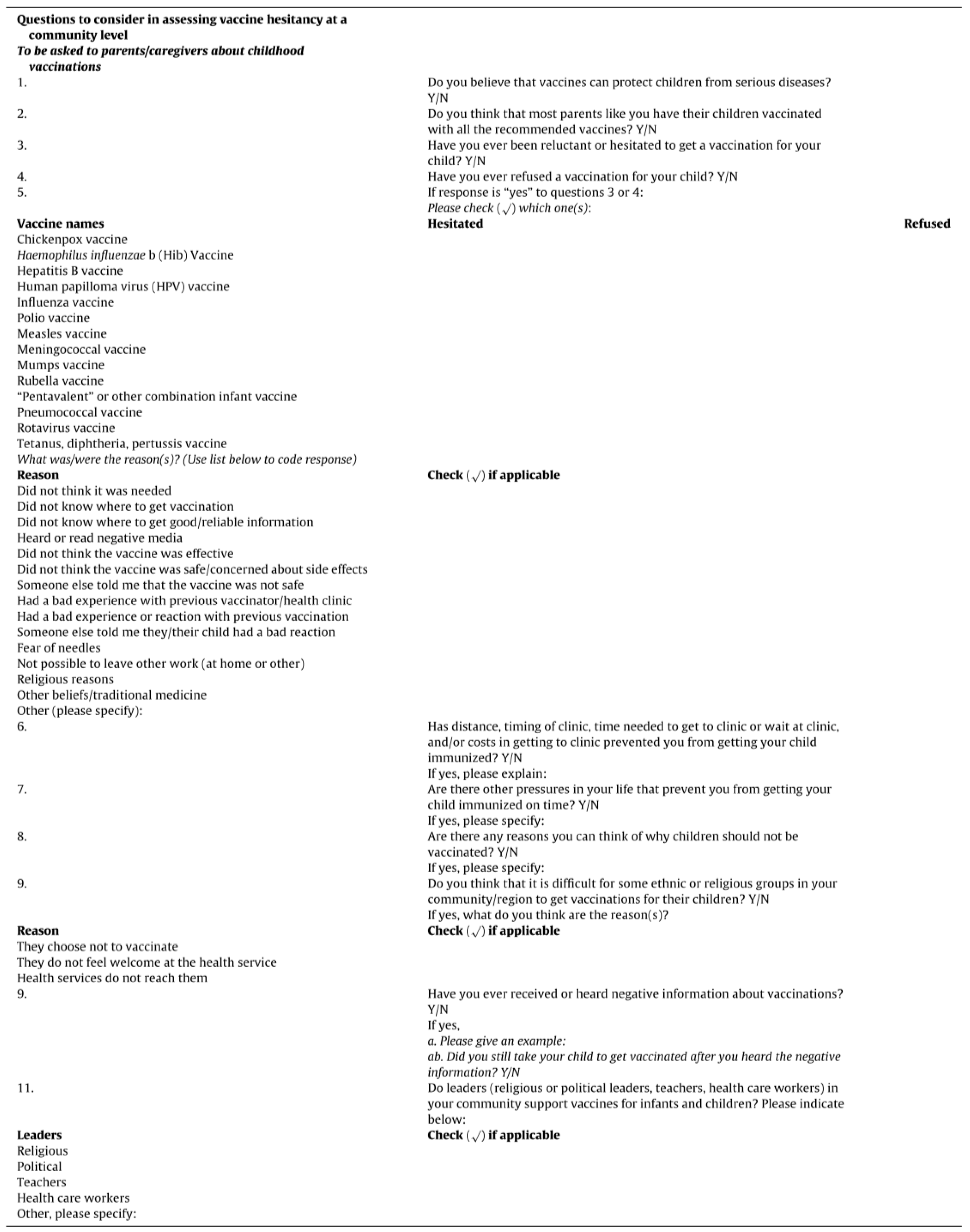
2. Materials and Methods
2.1. Study Design
2.2. Participants
2.3. Participant Recruitment and Informed Consent
2.4. Ethical Approval
2.5. Data Analysis
- Independent familiarization with the data set and MxDt of vaccine hesitancy.
- This was followed by a meeting of the researchers in order to calibrate their understanding of how the 21 items of the SAGE MxDt was related to the dataset, which takes into consideration the variations of meaning implied by the wording of each question.
- Preliminary training, which consists of a sample of 29 statements (4% of total 697 statements) was performed in order to calibrate the researcher’s understanding of how the data was related to the matrix and to minimize possible systematic gaps of interpretations (1 native researcher, 1 foreigner) as well as methodology described previously by Matthew Lombard [21]. This lasted for about 4 hours.
- The two researchers then independently mapped the 697 statements directly against the 21 items of the Matrix, question by question, using a binary method (item present in the statement: 1/item absent from the statement: 0).
- Inter-coder reliability, using “ReCal” [22], an online utility, compatible with Excel, that computes reliability coefficients for nominal, ordinal, or ratio-level data, was calculated for each of the 21 items, across the whole 697 statements, using percent agreement and Cohen’s Kappa [23]. Possible results for “percent agreement” are between 0 and 1, where “0” means that the authors who performed coding did not do better than if they had been working at random, while “1” means perfect agreement between the two raters. Negative results are possible, which means that the two authors did worse than if they would code accidentally. The cut-off values for Kappa were determined according to the methodology described by Hallgreen [24] and Krippendorff [25].
- from 0.0 to 0.2 indicating slight agreement
- 0.21 to 0.40 indicating fair agreement
- 0.41 to 0.60 indicating moderate agreement
- 0.61 to 0.80 indicating substantial agreement
- 0.81 to 1.0 indicating almost perfect or perfect agreement
3. Results
3.1. Brief Overview of Descriptive and Quantitative Results
3.2. Qualitative Thematic Analysis (QTA)
3.2.1. Contextual Influences
Item 1 “Media”
Item 2 “Leaders and Lobbies”
Item 7 “Perception of the Pharmaceutical Industry”
3.2.2. Individual and Group Influences
Item 9 “Beliefs”
Item 10 “Knowledge”
Item 12 “Risk/Benefits (Perceived)”
3.2.3. Vaccine and Vaccination Specific Issues
Item 14 “Risk/Benefit (Rational)”
Item 21 “Health Care Practitioners”
4. Discussion
4.1. Study Strengths
4.2. Study Limitations
4.2.1. Selection Bias
4.2.2. The Questions Were Not Pilot-Tested
4.2.3. Use of Thematic Analysis vs. Computer Software
5. Conclusions
- The prevalence of vaccine hesitant individuals in our study was 30.3%.
- The prevalence of those who refused a vaccination among hesitant individuals was found to be 36.1%.
- The chickenpox (varicella) vaccine generated the most reluctance among hesitant individuals (35%).
- The following vaccines scored above 20% in frequency among vaccine-hesitant participants: measles vaccines (28%), HPV vaccine (24%), mumps vaccine (23%), and rotavirus vaccine (23%).
- Contextual influences identified for VH were “media,” “leaders and lobbies,” and “perception of the pharmaceutical industry.”
- Individual and group influences for VH were “beliefs,” “knowledge,” and “risk/benefits (perceived).”
- Vaccine and vaccination specific issues for VH were “risk/benefit (rational),” and “health care practitioners” (trustworthiness, competence).
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
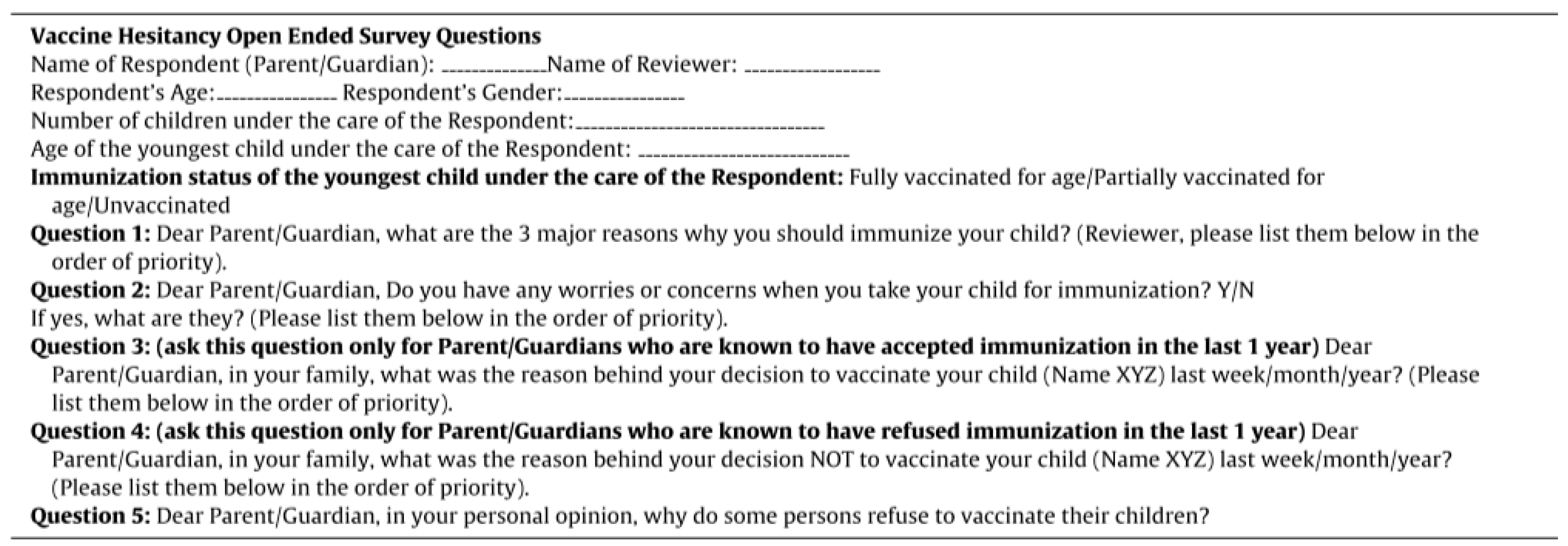
Appendix A
Appendix B
Appendix C
- ❖
- adverse reactions/side effects/any answer (specific or not) describing an adverse reaction
- -
- with no additional statement i.e., “adverse reaction”/”side effects” type of answer -> items 12 +14
- -
- if word “fear” is added (“fear of…”) -> item 9 + 12 + 14
- -
- specific or unspecific statement of a serious adverse reaction (including: “fake news” type and “absurd/obscure” and “serious” type) -> item 1 + 7 + 9 + 10 + 12 + 14
- -
- specific believable/possible statements (ex: fever/allergy/jaundice) -> item 10 + 12 + 14
- ❖
- vaccine
- -
- distance -> item 6 + 20
- -
- lack of availability -> item 18 + 20
- ❖
- personal health issue -> requiring delay or refusal in vaccination -> item 19
- ❖
- trusts/distrust statements
- -
- without additional precision -> item 7 + 11
- -
- about the health care personal -> item 7 + 11 + 21
- -
- health system -> item 5 + 7 + 11 + 21 (+ item 1 if aberrant/absurd/conspiracy-like tone)
- -
- consent -> item 7 + 11 + 21
- ❖
- information (info)
- -
- lack of info -> item 10 + 14 + 21
- ▪
- lack info about healthcare system/manufacturer -> item 7 + 14 + 21
- ▪
- lack info about effects/adverse reaction -> item 7 + 12 + 14 + 21
- -
- bad info/misinformation -> item 1 + 2 + 10
- -
- failure to inform oneself -> item 10 + 13 + 14
- ❖
- health care personal attitude related statements -> item 21
- ❖
- community participations/norms (nursery) -> item 5 + 13
- ❖
- adverse reactions/side effects/any answer (specific or not) describing an adverse reaction
- -
- with no additional statement i.e., “adverse reaction”/”side effects” type of answer -> item 12 +14
- ▪
- if word “fear” is added (“fear of…”) -> item 9 + 12 + 14
- -
- specific or unspecific statement of serious adverse reaction (including: “fake news” type and “absurd/obscure” and “serious adverse reactions” type) -> item 1 + 7 + 9 + 10 + 12 + 14
- -
- specific believable/possible statements (ex: fever/allergy/jaundice) -> item 10 + 12 + 14
- ❖
- health care personal attitude statement -> item 21
- ❖
- vaccine
- -
- content -> item 14
- -
- administration -> item 14 + 16
- -
- safety (vaccine themselves/production process) -> item 12 + 14
- -
- efficiency -> item 14
- -
- timing -> item 19
- -
- new/old -> item 15
- -
- cost -> item 20
- -
- aberrant statement about vaccines effects -> item 1 + 14
- -
- vaccine associated with statement of trust/uncertainty -> item 11 + 14
- -
- vaccine + statement of necessity/no necessity (and, therefore, underlying idea of norm) -> item 13 + 14
- ❖
- personal health issue -> requiring delay or refusal in vaccination -> item 19
- ❖
- religion -> item 4
- ❖
- trusts/distrust statements
- -
- without additional precision -> item 7 + 11
- -
- about the health care personal -> item 7 + 11 + 21
- -
- health system -> item 5 + 7 + 11 + 21 (+ item 1 if aberrant/absurd/conspiracy-like tone)
- -
- consent -> item 7 + 11 + 21
- ❖
- media -> item 1
- ❖
- perception health system (interest, intentions, hidden or not) -> item 2 + 7
- ❖
- information
- -
- lack of info -> item 10 + 14 + 21
- ▪
- lack info about healthcare system/manufacturer -> item 7 + 14 + 21
- ▪
- lack info about effects/adverse reaction -> item 7 + 12 + 14 + 21
- -
- inferior information/misinformation -> item 1 + 2 + 10
- -
- failure to inform oneself -> item 10 + 13 + 14
- ❖
- “adverse reactions”/“side effects”
- -
- with no additional explanation -> item 1 +14
- -
- specific or unspecific statement of serious adverse reaction (including: “fake news” type and “absurd/obscure/unclear” type) -> item 1 + 2 + 7 + 9 + 10 + 12 + 14
- -
- specific statements about believable/true statements -> item 1 + 14
- ❖
- information
- -
- negative information received through friends/family/community -> item 8 + 12 + 14
- -
- negative information from media/unspecific statement -> item 1 + 12 + 14
- ❖
- media -> item 1
- ❖
- campaigns/lobbies -> item 1 + 2
- ❖
- trusts/distrust statements
- -
- without additional precision -> item 1 + 7 + 11
- -
- vaccines as a business -> item 1 + 2 + 7 + 11
- ❖
- vaccine
- -
- safety (content/effects/manufacturing process) -> item 1 + 14 + 12
- -
- vaccine + statement of necessity/no necessity (and, therefore, underlying idea of norm) -> item 1 + 13 + 14
- -
- efficiency -> item 1 + 14
- -
- new/old -> item 1 + 15
- ❖
- health care personal attitude statement -> item 21
- ❖
- adverse reactions/side effects/any answer (specific or not) describing an adverse reaction
- -
- with no additional statement i.e., “adverse reaction”/”side effects” type of answer -> item 12 +14
- -
- if word “fear” is added (“fear of…”) -> item 9 + 12 + 14
- -
- specific or unspecific statement of serious adverse reaction (including: “fake news” type and “absurd/obscure” and “serious adverse reactions” type) -> item 1 + 7 + 9 + 10 + 12 + 14
- -
- specific believable/possible statements (ex: fever/allergy/jaundice) -> item 10 + 12 + 14
- ❖
- vaccines themselves
- -
- content -> item 14
- -
- safety -> item 12 + 14
- -
- efficiency -> item 14
- -
- source of vaccine -> item 18
- -
- administration -> item 16
- -
- pain + vaccination -> item 8 + 16
- -
- timing -> item 19
- -
- new vs. old vaccine -> item 15
- -
- vaccine + statement of necessity/no necessity (and, therefore, underlying idea of norm) -> item 13 + 14
- -
- wrong belief (specific statement about mechanism or consequences that are wrong/not proven) -> item 9 + 10 + 14
- ❖
- trusts/distrust statements
- -
- without additional precision -> item 7 + 11
- -
- about the health care personal -> item 7 + 11 + 21
- -
- health system -> item 5 + 7 + 11 + 21 (+ item 1 if aberrant/absurd/conspiracy-like tone)
- -
- consent -> item 7 + 11 + 21
- ❖
- pharma industry/medical system/healthcare system -> item 7 + item 11
- ❖
- responsibility for negative consequences -> item 5 + 7 + 11
- ❖
- media (all types) -> item 1
- ❖
- personal reasons/personal beliefs -> item 9 + 11
- ❖
- personal health issue -> item 19
- ❖
- information
- -
- lack of information -> item 10 + 14 + 21
- ▪
- about healthcare system/manufacturer -> item 7 + 14 + 21
- ▪
- about effects/adverse reactions -> item 7 + 12 + 14 + 21
- -
- inferior information/misinformation -> item 1 + 2 + 10
- -
- failure to inform oneself -> item 10 + 13 + 14
- ❖
- health care personal attitudes -> item 21
- ❖
- adverse reactions/side effects/any answer (specific or not) describing an adverse reaction
- -
- with no additional statement i.e., “adverse reaction”/ “side effects” type of answer -> item 12 +14
- ▪
- if word “fear” is added (“fear of…”) -> item 9 + 12 + 14
- -
- specific or unspecific statement of serious adverse reaction (including: “fake news” type and “absurd/obscure” and “serious adverse reactions” type) -> item 1 + 7 + 9 + 10 + 12 + 14
- -
- specific believable/possible statements (ex: fever/allergy/jaundice) -> item 10 + 12 + 14
- ❖
- health care personal attitude statement -> item 21
- ❖
- vaccine
- -
- content -> item 14
- -
- administration -> item 14 + 16
- -
- safety (of vaccine themselves/of production process) -> item 12 + 14
- -
- efficiency -> item 14
- -
- timing -> item 19
- -
- new/old -> item 15
- -
- cost -> item 20
- -
- aberrant statement about vaccines effects -> item 1 + 14
- -
- vaccine + statement of trust/uncertainty -> item 11 + 14
- -
- vaccine + statement of necessity/no necessity (and, therefore, an underlying idea of norm) -> item 13 + 14
- ❖
- personal health issue
- ❖
- requiring delay or refusal in vaccination -> item 19
- ❖
- religion -> item 4
- ❖
- trusts/distrust statements
- -
- without additional precision -> item 7 + 11
- -
- about the health care personal -> item 7 + 11 + 21
- -
- health system -> item 5 + 7 + 11 + 21 (+ item 1 if aberrant/absurd/conspiracy-like tone)
- -
- consent -> item 7 + 11 + 21
- ❖
- fear -> item 9
- ❖
- adverse reactions/side effects/any answer (specific or not) describing an adverse reaction
- -
- with no additional statement i.e., “adverse reaction”/”side effects” type of answer -> item 12 +14
- ▪
- if word “fear” is added (“fear of…”) -> item 9 + 12 + 14
- -
- specific or unspecific statement of serious adverse reaction (including: “fake news” type and “absurd/obscure” and “serious adverse reactions” type) -> item 1 + 7 + 9 + 10 + 12 + 14
- -
- specific believable/possible statements (ex: fever/allergy/jaundice) -> item 10 + 12 + 14
- ❖
- vaccine
- -
- content -> item 14
- -
- administration -> item 14 + 16
- -
- safety (of vaccine themselves/of production process) -> item 12 + 14
- -
- efficiency -> item 14
- -
- timing -> item 19
- -
- new/old -> item 15
- -
- cost -> item 20
- -
- aberrant/absurd statement about vaccines effects/mechanism -> item 1 + 14
- -
- vaccine + statement of trust/uncertainty -> item 11 + 14
- -
- vaccine + statement of necessity/no necessity (and, therefore, underlying idea of norm) -> item 13 + 14
- ❖
- trusts/distrust statements
- -
- without additional precision -> item 7 + 11
- -
- about the health care personal -> item 7 + 11 + 21
- -
- health system -> item 5 + 7 + 11 + 21 (+ item 1 if aberrant/absurd/conspiracy-like tone)
- -
- consent -> item 7 + 11 + 21
- ❖
- information
- -
- lack of information -> item 10 + 14 + 21
- ▪
- lack information about healthcare system/manufacturer -> item 7 + 14 + 21
- ▪
- lack information about effects/adverse reactions -> item 7 + 12 + 14 + 21
- -
- inferior information/misinformation -> item 1 + 2 + 10
- -
- failure to inform oneself -> item 10 + 13 + 14
- ❖
- responsibility for negative consequences -> item 5 + 7 + 11
- ❖
- media (all types) -> item 1
- ❖
- personal reasons/personal beliefs -> item 9 + 11
- ❖
- personal health issue -> item 19
- ❖
- “recklessness”/«carelessness»/moral judgment (“doing wrong”) -> item 9 + 10 + 12 + 13
- ❖
- education level/understanding -> item 10
- ❖
- “fear” -> if without any other precision -> item 7 + 9 + 12
- ❖
- health care personal attitude statement -> item 21
References
- World health Organization. Ten Threats to Global Health in 2019. Available online: https://www.who.int/emergencies/ten-threats-to-global-health-in-2019 (accessed on 24 April 2019).
- European Centre for Disease Prevention and Control. Measles. Available online: https://ecdc.europa.eu/en/measles (accessed on 24 April 2019).
- CBS News. Measles Outbreak. Available online: https://www.cbsnews.com/news/measles-outbreak (accessed on 24 April 2019).
- The Strategic Advisory Group of Experts (SAGE). Report of the SAGE Working Group on Vaccine hesitancy. SAGE Rep. 2014, 63. Available online: http://www.who.int/immunization/sage/meetings/2014/october/1_Report_Working_Group_vaccine_hesitancy_final.pdf (accessed on 24 April 2019).
- Larson, H.J.; De Figueiredo, A.; Xiahong, Z.; Schulz, W.S.; Verger, P.; Johnston, I.G.; Cook, A.R.; Jones, N.S. EBioMedicine The State of Vaccine Confidence 2016: Global Insights Through a 67-Country Survey. EBIOM 2016, 12, 295–301. [Google Scholar] [CrossRef] [PubMed]
- Mac Donald, N.E. Vaccine hesitancy: Definition, scope and determinants. Vaccine 2015, 33, 4161–4164. [Google Scholar] [CrossRef] [PubMed]
- Larson, H.J.; Brocard, P. The India HPV-vaccine suspension. Lancet 2010, 376, 572–573. [Google Scholar] [CrossRef]
- Rosselli, R.; Martini, M.; Bragazzi, N.L. The old and the new: Vaccine hesitancy in the era of the Web 2.0. Challenges and opportunities. J. Prev. Med. Hyg. 2016, 57, E47–E50. [Google Scholar] [PubMed]
- McClure, C.C.; Cataldi, J.R.; O’Leary, S.T. Vaccine Hesitancy: Where We Are and Where We Are Going. Clin. Ther. 2017, 39, 1550–1562. [Google Scholar] [CrossRef]
- Tafuri, S.; Gallone, M.S. Addressing the anti-vaccination movement and the role of HCWs. Vaccine 2014, 32, 4860–4865. [Google Scholar] [CrossRef]
- Jung, M. Challenges of Vaccinations in the Era of New Media Communication. Health Care Manag. 2018, 37, 1–5. [Google Scholar] [CrossRef]
- Holden, J. Lancet retracts 12-year-old article linking autism to MMR. CMAJ 2010, 182, 199–200. [Google Scholar]
- Rao, T.S.S.; Andrade, C. The MMR vaccine and autism: Sensation, refutation, retraction, and fraud. Indian J. Psychiatry 2011, 53, 95–96. [Google Scholar]
- Smith, T.C. Vaccine Rejection and Hesitancy: A Review and Call to Action. Open Forum Infect. Dis. 2017, 4, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Peretti-Watel, P.; Larson, H.J.; Ward, J.K.; Schulz, W.S.; Verger, P. Vaccine hesitancy: Clarifying a theoretical framework for an ambiguous notion. PLoS Curr. 2015, 7. [Google Scholar] [CrossRef] [PubMed]
- Larson, H.J.; Clarke, R.M.; Jarrett, C.; Eckersberger, E.; Levine, Z.; Schulz, W.S.; Paterson, P. Measuring trust in vaccination: A systematic review. Hum. Vaccine Immunother. 2018, 14, 1599–1609. [Google Scholar] [CrossRef] [PubMed]
- Shapiro, G.K.; Tatar, O.; Dube, E.; Amsel, R.; Knauper, B.; Naz, A.; Perez, S.; Rosberger, Z. The vaccine hesitancy scale: Psychometric properties and validation. Vaccine 2018, 36, 660–667. [Google Scholar] [CrossRef] [PubMed]
- Larson, H.J.; Jarrett, C.; Schulz, W.S.; Chaudhuri, M.; Zhou, Y.; Dube, E.; Schuster, M.; MacDonald, N.E.; Wilson, R. Measuring vaccine hesitancy: The development of a survey tool. Vaccine 2015, 33, 4165–4175. [Google Scholar] [CrossRef] [PubMed]
- Braun, V.; Clarke, V. What can “thematic analysis” offer health and wellbeing researchers? Int. J. Qual. Stud. Health Well-Being 2014, 9, 20–22. [Google Scholar] [CrossRef] [PubMed]
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef]
- Lombard, M.; Snyder-Duch, J.; Campanella Bracken, C. Intercoder Reliability. In The SAGE Encyclopedia of Communication Research Methods; SAGE Publications Inc.: Thousand Oaks, CA, USA, 2017. [Google Scholar]
- Freelon, D.G. ReCal: Intercoder Reliability Calculation as a Web Service. Int. J. Internet Sci. 2010, 5, 20–33. [Google Scholar]
- Viera, A.J.; Garrett, J.M. Understanding Inter-observer Agreement: The Kappa Statistic. Fam. Med. 2005, 37, 360–363. [Google Scholar]
- Hallgren, K.A. NIH Public Access. Tutor. Quant. Methods Psychol. 2012, 8, 23–34. [Google Scholar] [CrossRef]
- Krippendorff, K. Content Analysis: An Introduction to Its Methodology, 2nd ed.; SAGE Publications, Inc.: Thousand Oaks, CA, USA, 2004; pp. 221–227. [Google Scholar]
- Dubé, E.; Leask, J.; Wolff, B.; Hickler, B.; Balaban, V.; Hosein, E.; Habersaat, K. The WHO Tailoring Immunization Programmes (TIP) approach: Review of implementation to date. Vaccine 2017, 36, 1509–1515. [Google Scholar] [CrossRef] [PubMed]
- Biosta TGV. Available online: https://biostatgv.sentiweb.fr/ (accessed on 20 April 2019).
- VassarStats: Website for Statistical Computation. Available online: http://www.vassarstats.net/ (accessed on 20 April 2019).
- Centrul National de Statistica pentru Boli Transmisibile. Available online: cnscbt.ro/index.php/rapoarte-anuale/ (accessed on 5 June 2019).
- Murrero, M.; Rice, R.E. The Internet and Health Care: Theory, Research and Practice; Routledge: Abingdon, UK, 2013; pp. 27–213. [Google Scholar]
- Van Laer, J.; Van Aelst, P. Internet and social movement action repertoire: Opportunities and limitations. Inform. Commun. Soc. 2010, 13, 1146–1171. [Google Scholar] [CrossRef]
- Betsch, C. Dr. Jekyll or Mr. Hyde? (How) the Internet influences vaccination decisions: Recent evidence and tentative guidelines for online vaccine communication. Vaccine 2012, 30, 3723–3726. [Google Scholar] [CrossRef] [PubMed]
- Witteman, H.O.; Zikmund-Fisher, B.J. The defining characteristics of Web 2.0 and their potential influence in the online vaccination debate. Vaccine 2012, 30, 3734–3740. [Google Scholar] [CrossRef] [PubMed]
- Ward, J.K.; Peretti-Watel, P.; Verger, P. Vaccine criticism on the Internet: Propositions for future research. Hum. Vaccines Immunother. 2016, 12, 1924–1929. [Google Scholar] [CrossRef] [PubMed]
- Kang, G.J.; Ewing-Nelson, S.R.; Mackey, L.; Schlitt, J.T.; Marathe, A.; Abbas, K.M.; Swarup, S. Semantic network analysis of vaccine sentiment in online social media. Vaccine 2017, 35, 3621–3638. [Google Scholar] [CrossRef]
- Miton, H.; Mercier, H. Science and Society Cognitive Obstacles to Pro-Vaccination Beliefs. Trends Cogn. Sci. 2015, 19, 633–636. [Google Scholar] [CrossRef]
- Mcphetres, J.; Zuckerman, M. Religiosity predicts negative attitudes towards science and lower levels of science literacy. PLoS ONE 2018, 13, e0207125. [Google Scholar] [CrossRef]
- Kata, A. Anti-vaccine activists, Web 2.0, and the postmodern paradigm—An overview of tactics and tropes used online by the anti-vaccination movement. Vaccine 2012, 30, 3778–3789. [Google Scholar] [CrossRef]
- Slovic, P.; Finucane, M.L.; Peters, E.; Macgregor, D.G. Risk as Analysis and Risk as Feelings: Some Thoughts about Affect, Reason, Risk, and Rationality. Risk Anal. 2004, 24, 311–322. [Google Scholar] [CrossRef]
- Damasio, A.R. Descartes’ Error: Emotion, Reason, and the Human Brain; Avon Books: New York, NY, USA, 1994; Available online: https://ahandfulofleaves.files.wordpress.com/2013/07/descartes-error_antonio-damasio.pdf (accessed on 20 April 2019).
- Ropeik, D. How society should respond to the risk of vaccine rejection. Hum. Vaccine Immunother. 2013, 9, 1815–1818. [Google Scholar] [CrossRef] [PubMed]
- Karafillakis, E.; Dinca, I.; Apfel, F.; Cecconi, S.; Wűrz, A.; Takacs, J.; Suk, J.; Celentano, L.P.; Kramarz, P.; Larson, H.J. Vaccine hesitancy among healthcare workers in Europe: A qualitative study. Vaccine 2016, 34, 5013–5020. [Google Scholar] [CrossRef] [PubMed]
- Karafillakis, E.; Larson, H.J. The paradox of vaccine hesitancy among healthcare professionals. Clin. Microbiol. Infect. 2018, 24, 799–800. [Google Scholar] [CrossRef] [PubMed]
- Agrinier, N.; Le Maréchal, M.; Fressard, L.; Verger, P.; Pulcini, C. Discrepancies between general practitioners’ vaccination recommendations for their patients and practices for their children. Clin. Microbiol. Infect. 2017, 23, 311–317. [Google Scholar] [CrossRef] [PubMed]
- Suryadevara, M.; Handel, A.; Bonville, C.A.; Cibula, D.A.; Domachowske, J.B. Pediatric provider vaccine hesitancy: An under-recognized obstacle to immunizing children. Vaccine 2015, 33, 6629–6634. [Google Scholar] [CrossRef] [PubMed]
- Dubé, E. Addressing vaccine hesitancy: The crucial role of healthcare providers. Clin. Microbiol. Infect. 2017, 23, 279–280. [Google Scholar] [CrossRef] [PubMed]
- Van der Linden, S.L.; Clarke, C.E.; Maibach, E.W. Highlighting consensus among medical scientists increases public support for vaccines: Evidence from a randomized experiment. BMC Public Health 2015, 15, 1207. [Google Scholar] [CrossRef] [PubMed]
- Morariu, S.; Tarcea, M.; Moldovan, H.; Dobreanu, M. Human Papillomavirus (HPV) Infection and HPV Vaccination: Assessing the Level of Knowledge among Students of the University of Medicine and Pharmacy of Tîrgu Mureş, Romania. Acta Dermatovenerol. Croat. 2016, 24, 193–202. [Google Scholar]
- Paterson, P.; Meurice, F.; Stanberry, L.R.; Glismann, S.; Rosenthal, S.L.; Larson, H.J. Vaccine hesitancy and healthcare providers. Vaccine 2016, 34, 6700–6706. [Google Scholar] [CrossRef]
- Wilson, R.; Paterson, P.; Larson, H.J. Strategies to improve maternal vaccination acceptance. BMC Public Health 2019, 19, 342. [Google Scholar] [CrossRef]
- Betsch, C.; Bödeker, B.; Schmid, P.; Wichmann, O. How baby’s first shot determines the development of maternal attitudes towards vaccination. Vaccine 2018, 36, 3018–3026. [Google Scholar] [CrossRef]
- Mendel-Van Alstyne, J.A.; Nowak, G.J.; Aikin, A.L. What is ‘confidence’ and what could affect it? A qualitative study of mothers who are hesitant about vaccines. Vaccine 2017, 36, 6464–6472. [Google Scholar] [CrossRef]
- Vanderslott, S. Exploring the meaning of pro-vaccine activism across two countries. Soc. Sci. Med. 2019, 222, 59–66. [Google Scholar] [CrossRef]
- WHO Regional Office: Tailoring Immunization Programmes (TIP) An Introductory Overview. 2018. Available online: https://www.who.int/immunization/programmes_systems/Global_TIP_overview_May2018.pdf (accessed on 20 April 2019).
- Jackson, C.; Bedford, H.; Cheater, F.M.; Condon, L.; Emslie, C.; Ireland, L.; Kemsley, P.; Kerr, S.; Lewis, H.J.; Mytton, J.; et al. Needles, Jabs and Jags: A qualitative exploration of barriers and facilitators to child and adult immunisation uptake among Gypsies, Travellers and Roma. BMC Public Health 2017, 17, 1–17. [Google Scholar] [CrossRef]
- De Graaf, P.; Rotar Pavlič, D.; Zelko, E.; Vintges, M.; Willems, S.; Hanssens, L. Primary care for the Roma in Europe: Position paper of the European forum for primary care. Zdr. Varst. 2016, 55, 218–224. [Google Scholar] [CrossRef]
- de Figueiredo, A.; Larson, H.J.; Johnston, I.G.; Smith, D.M.; Jones, N.S. Forecasted trends in vaccination coverage and correlations with socioeconomic factors: A global time-series analysis over 30 years. Lancet 2016, 4, 726–735. [Google Scholar] [CrossRef]
- Omer, S.B.; Salmon, D.A.; Orenstein, W.A.; Halsey, N. Vaccine Refusal, Mandatory Immunization, and the Risks of Vaccine-Preventable Diseases. N. Engl. J. Med. 2009, 360, 1981–1988. [Google Scholar] [CrossRef]
- Dubé, E.; Gagnon, D.; MacDonald, N.E. Strategies intended to address vaccine hesitancy: Review of published reviews. Vaccine 2015, 33, 4191–4203. [Google Scholar] [CrossRef]
- Dubé, E.; Gagnon, D.; Nickels, E.; Jeram, S.; Schuster, M. Mapping vaccine hesitancy-Country-specific characteristics of a global phenomenon. Vaccine 2014, 32, 6649–6654. [Google Scholar] [CrossRef]
- Eskola, J.; Duclos, P.; Schuster, M.; MacDonald, N.E. How to deal with vaccine hesitancy? Vaccine 2015, 33, 4215–4217. [Google Scholar] [CrossRef]
- Goldstein, S.; MacDonald, N.E.; Guirguis, S. Health communication and vaccine hesitancy. Vaccine 2015, 33, 4212–4214. [Google Scholar] [CrossRef]
| Contextual influences |
|
| Individual and group influences |
|
| Vaccine/vaccination specific issues |
|
| Item | Percent Agreement | Scott’s Pi | Cohen’s Kappa | Krippendorff’s Alpha | No. Agreements | No. Disagreements |
|---|---|---|---|---|---|---|
| Item 1 | 94.83 | 0.90 | 0.90 | 0.90 | 660 | 36 |
| Item 2 | 95.55 | 0.88 | 0.88 | 0.88 | 665 | 31 |
| Item 3 | 100.00 | 1 | 1 | 1 | 696 | 0 |
| Item 4 | 99.71 | 0.95 | 0.95 | 0.95 | 694 | 2 |
| Item 5 | 97.84 | 0.60 | 0.60 | 0.60 | 681 | 15 |
| Item 6 | 99.86 | 0.67 | 0.67 | 0.67 | 695 | 1 |
| Item 7 | 92.96 | 0.81 | 0.81 | 0.81 | 647 | 49 |
| Item 8 | 97.41 | 0.54 | 0.54 | 0.54 | 678 | 18 |
| Item 9 | 94.54 | 0.87 | 0.87 | 0.88 | 658 | 38 |
| Item 10 | 94.40 | 0.89 | 0.89 | 0.89 | 657 | 39 |
| Item 11 | 96.12 | 0.79 | 0.79 | 0.79 | 669 | 27 |
| Item 12 | 89.51 | 0.79 | 0.79 | 0.79 | 623 | 73 |
| Item 13 | 98.13 | 0.86 | 0.86 | 0.86 | 683 | 13 |
| Item 14 | 91.81 | 0.81 | 0.81 | 0.81 | 639 | 57 |
| Item 15 | 99.71 | 0.83 | 0.83 | 0.83 | 694 | 2 |
| Item 16 | 99.57 | 0.85 | 0.85 | 0.86 | 693 | 3 |
| Item 17 | 100.00 | 1 | 1 | 1 | 696 | 0 |
| Item 18 | 98.99 | 0.46 | 0.46 | 0.46 | 689 | 7 |
| Item 19 | 98.71 | 0.85 | 0.85 | 0.85 | 687 | 9 |
| Item 20 | 99.71 | 0.86 | 0.86 | 0.86 | 694 | 2 |
| Item 21 | 96.12 | 0.84 | 0.84 | 0.84 | 669 | 27 |
| Item 22 | 99.14 | 0.83 | 0.83 | 0.83 | 690 | 6 |
| SAGE WG Vaccine Hesitancy Model * | |||||
|---|---|---|---|---|---|
| Contextual Influences | Individual and Group Influences | Vaccine and Vaccination-Specific Issues | |||
| Items | Iterations | Items | Iterations | Items | Iterations |
| 1 | 314 | 8 | 27 | 14 | 477 |
| 2 | 165 | 9 | 225 | 15 | 7 |
| 3 | 0 | 10 | 303 | 16 | 10 |
| 4 | 22 | 11 | 68 | 17 | 0 |
| 5 | 23 | 12 | 377 | 18 | 7 |
| 6 | 2 | 13 | 46 | 19 | 31 |
| 7 | 177 | 20 | 7 | ||
| 21 | 101 | ||||
| TOTAL (%) | 703 (29.2) | TOTAL (%) | 1046 (43.5) | TOTAL (%) | 640 (26.6) |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Miko, D.; Costache, C.; Colosi, H.A.; Neculicioiu, V.; Colosi, I.A. Qualitative Assessment of Vaccine Hesitancy in Romania. Medicina 2019, 55, 282. https://doi.org/10.3390/medicina55060282
Miko D, Costache C, Colosi HA, Neculicioiu V, Colosi IA. Qualitative Assessment of Vaccine Hesitancy in Romania. Medicina. 2019; 55(6):282. https://doi.org/10.3390/medicina55060282
Chicago/Turabian StyleMiko, David, Carmen Costache, Horațiu Alexandru Colosi, Vlad Neculicioiu, and Ioana Alina Colosi. 2019. "Qualitative Assessment of Vaccine Hesitancy in Romania" Medicina 55, no. 6: 282. https://doi.org/10.3390/medicina55060282
APA StyleMiko, D., Costache, C., Colosi, H. A., Neculicioiu, V., & Colosi, I. A. (2019). Qualitative Assessment of Vaccine Hesitancy in Romania. Medicina, 55(6), 282. https://doi.org/10.3390/medicina55060282






