The Effect of an Innovative Biofeedback SKOL-AS® Treatment on the Body Posture and Trunk Rotation in Children with Idiopathic Scoliosis—Preliminary Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Experimental Design
2.3. Methods
2.3.1. Anthropometrics
2.3.2. X-ray Imaging
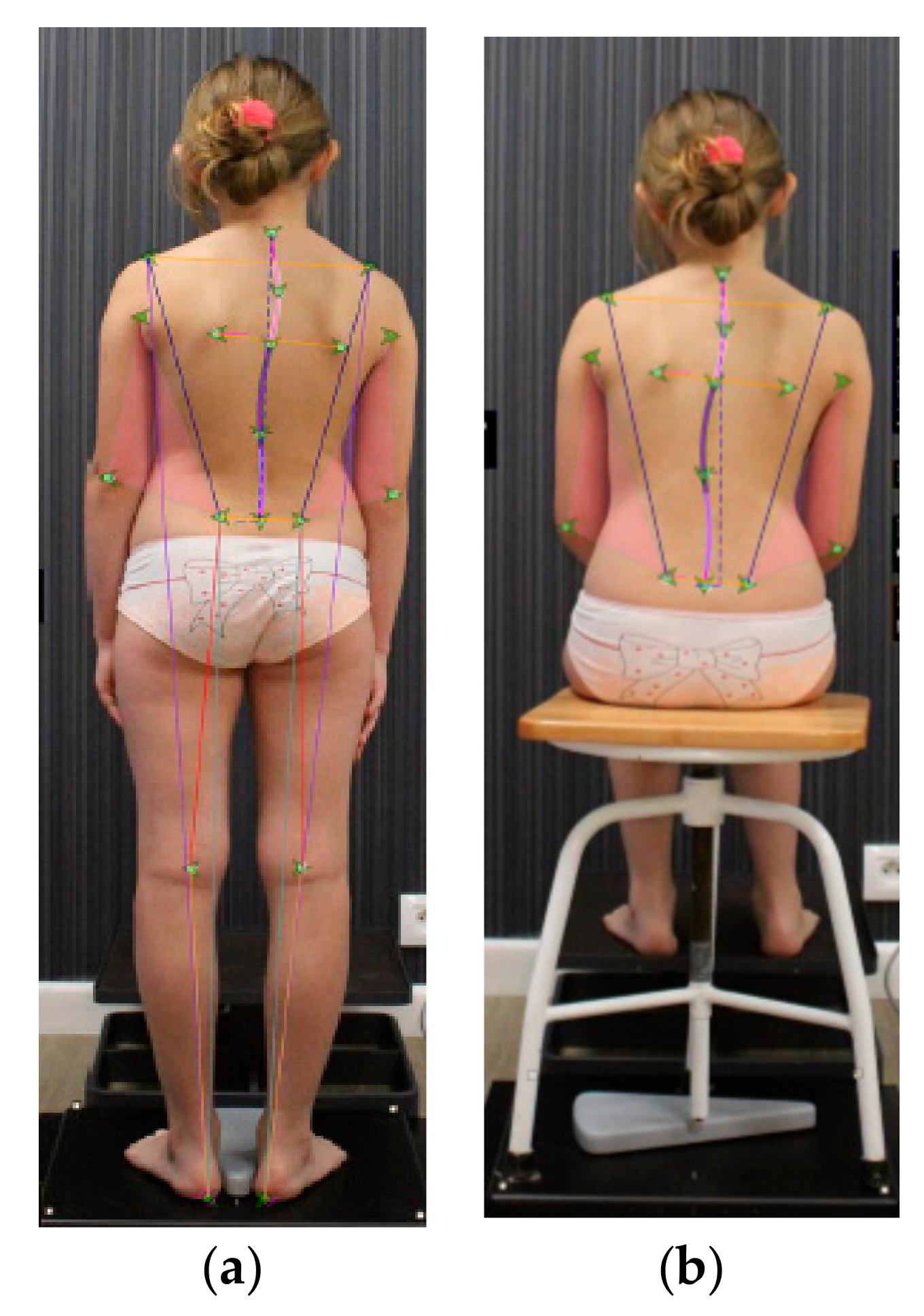
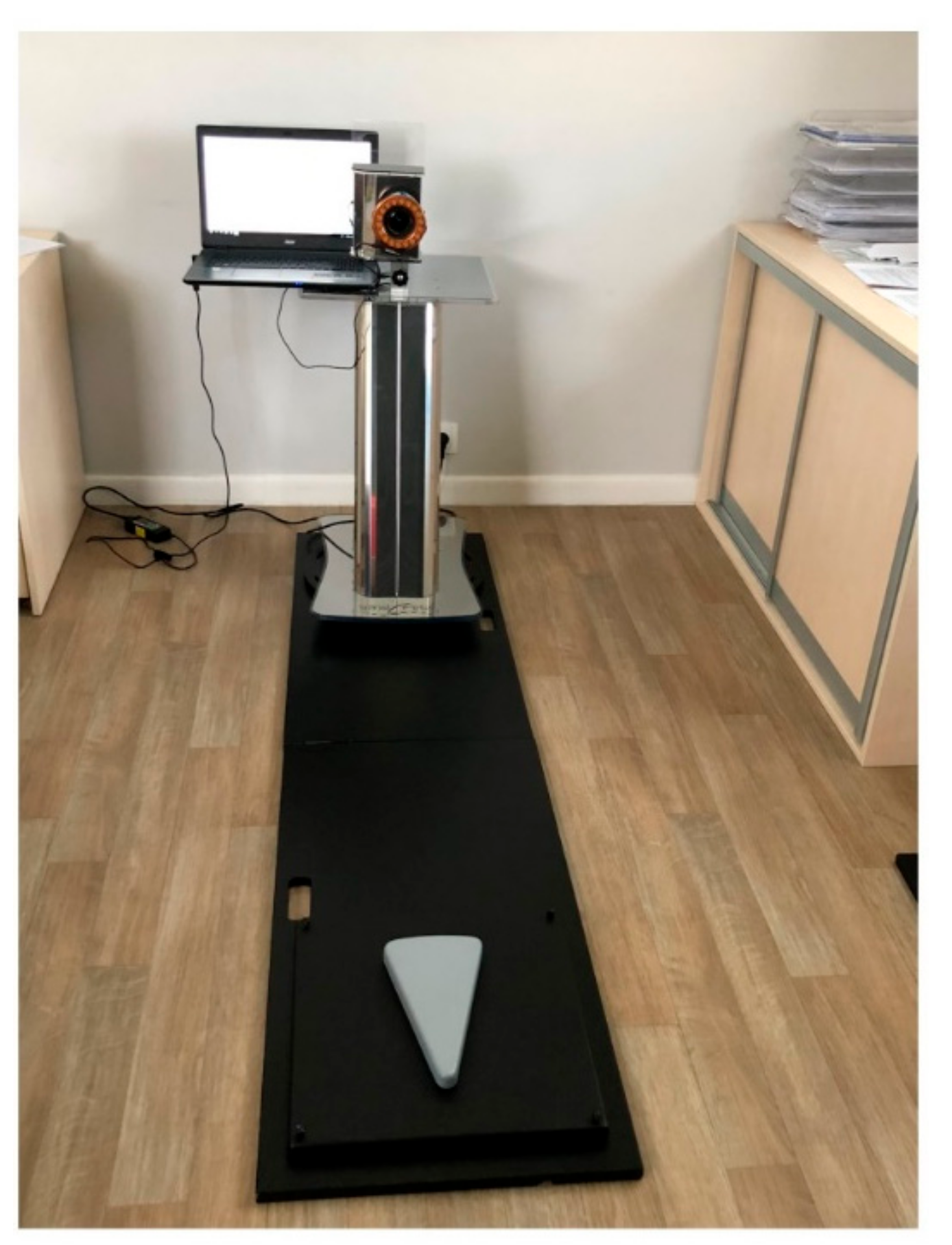
2.3.3. SpinalMeter® Calibration and Posture Assessment
- posterior view in standing:
- (1)
- C7—cervical spine
- (2)
- Th4—thoracic spine
- (3)
- Acromion (right and left side)
- (4)
- Angulus inferior scapulae (right and left side)
- (5)
- L1—lumbar spine
- (6)
- Olecranon—elbow (right and left side)
- (7)
- Iliac crest (right and left side)
- (8)
- PSIS—posterior superior iliac spine (right and left side)
- (9)
- Popliteal fossa—the hollow at the back of the knee (right and left side)
- (10)
- Heel (right and left side)
- posterior view in sitting position: all above mentioned points without 9 and 10
- anterior view:
- (1)
- Right and left eye
- (2)
- Right and left side of the mouth
- (3)
- Clavicle (right and left side)
- (4)
- ASIS—anterior superior iliac spine (right and left side)
- (5)
- Radial styloid process (right and left side)
- (6)
- The middle of the knee (right and left side)
- (7)
- Medial malleolus (right and left side)
- (8)
- First and fifth metatarsal bones (right and left side)
- palpation and the use of reflective markers to mark the spinous processes and specific anatomical points;
- acquisition of digital images;
- processing of the image and the tag applied through a specialist software (SpinalMeter® Evolution v6.14);
- numerical visualization of the patient’s spine;
- visualization with bidimensional image of the spine’s curvature;
- measurement of upper and lower limb.
2.3.4. The Angle of Trunk Rotation (ATR) Assessment
2.3.5. Control Examination
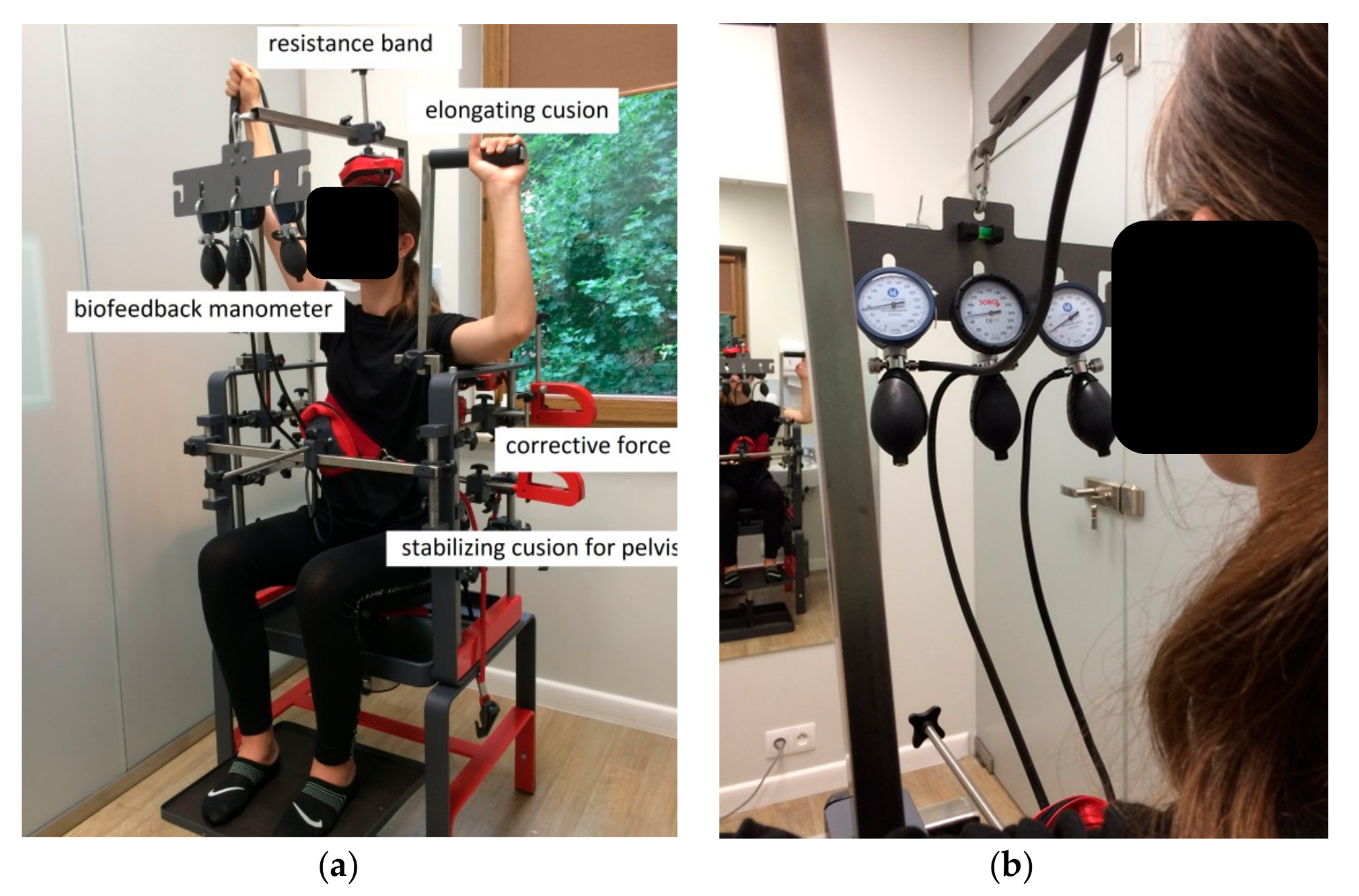
2.3.6. SKOL-AS® Device Therapy
- 1st–2nd session—15 min biofeedback training + 15 min SKOL-AS®
- 3rd–4th session—10 min biofeedback training + 20 min SKOL-AS®
- 5th–8th session—30 min SKOL-AS®
- 9th–24th session—30 min SKOL-AS®
2.3.7. The Learning of Posture Correction during Standing and Sitting Positions
- uggested sitting position: the head and ankles should be straight, shoulders and hips are level, kneecaps face the front, and the chin should be parallel to the floor and aligned with the ears. The lower back should be slightly bent forward to support the body with no extra weight distributed onto the spine.
- Suggested standing position: the head and ankles should be straight, shoulders and hip are level, kneecaps face the front, the head and knees are straight, and the chin should be parallel to the floor and aligned with the ears. The lower back should be slightly bent forward with the aid of the chest, stomach, and buttock muscles.
2.3.8. The Statistical Methods
3. Results
3.1. The Characteristics of the Population Studied
3.2. The Effect of SKOL-AS® Postural Training on the Angle of Trunk Rotation
4. Discussion
5. Conclusions
- The SKOL-AS® biofeedback method uses three-dimensional exercises, thus it seems to be a good way to treat scoliotic spine.
- The decrease in trunk rotation and some anthropometric points asymmetry and the increase in length values proves the effectiveness of the SKOL-AS® treatment. However, some results are questionable and need verification.
- The SKOL-AS® biofeedback method could help patients learn good postural habits and auto-correction of the spine.
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Stokes, I.A. Three-dimensional terminology of spinal deformity. A report presented to the Scoliosis Research Society by the Scoliosis Research Society Working Group on 3-D terminology of spinal deformity. Spine (Phila Pa 1976) 1994, 19, 236–248. [Google Scholar] [CrossRef]
- Scoliosis Research Society. Available online: https://www.srs.org/professionals/online-education-and-resources/glossary/three-dimensional-terminology-of-spinal-deformity (accessed on 22 February 2019).
- Negrini, S.; Donzelli, S.; Aulisa, A.G.; Czaprowski, D.; Schreiber, S.; de Mauroy, J.C.; Diers, H.; Grivas, T.B.; Knott, P.; Kotwicki, T.; et al. 2016 SOSORT guidelines: Orthopaedic and rehabilitation treatment of idiopathic scoliosis during growth. Scoliosis Spinal Disord. 2018, 13, 3. [Google Scholar] [CrossRef] [PubMed]
- Kalichman, L.; Kendelker, L.; Bezalel, T. Bracing and exercise-based treatment for idiopathic scoliosis. J. Bodyw. Mov. 2016, 20, 56–64. [Google Scholar] [CrossRef] [PubMed]
- Zaborowska-Sapeta, K.; Giżewski, T.; Binkiewicz-Glińska, A.; Kamelska-Sadowska, A.M.; Kowalski, I.M. The Duration of the correction loss after removing cheneau brace in patients with adolescent idiopathic scoliosis. Acta Orthop. Traumatol. Turc. 2019, 53, 61–67. [Google Scholar] [CrossRef] [PubMed]
- Odent, T.; Ilharreborde, B.; Miladi, L.; Khouri, N.; Violas, P.; Ouellet, J.; Cunin, V.; Kieffer, J.; Kharrat, K.; Accadbled, F.; et al. Fusionless surgery in early-onset scoliosis. Orthop. Traumatol.-Sur. 2015, 101, s281–s288. [Google Scholar] [CrossRef] [PubMed]
- Kwok, G.H.C. Development of Posture Correction Tank-Top Synchronized with Biofeedback Muscle Training for Adolescents with Early Scoliosis. Master’s Thesis, The Hong Kong Polytechnic University, Hong Kong, China, 2017. [Google Scholar]
- Kappes, B. Biofeedback therapy: Training or treatment. Appl. Psychophys. Biofeedback 2008, 33, 173–179. [Google Scholar]
- Luo, H.J.; Lin, S.X.; Wu, S.K.; Tsai, M.W.; Lee, S.J. Comparison of segmental spinal movement control in adolescents with and without idiopathic scoliosis using modified pressure biofeedback unit. PLoS ONE 2017, 12, e0181915. [Google Scholar] [CrossRef] [PubMed]
- Kallistratos, E.; Mahairas, V.; Papadopoulou, M.; Parintas, T. The development of a novel biofeedback system for the evaluation, recording, control and correction of the spinal posture. Scoliosis 2009, 4 (Suppl. 1), O25. [Google Scholar] [CrossRef]
- Kwok, G.H.C.; Yip, J.; Cheung, M.-C.; Yick, K.-L. Evaluation of myoelectric activity of paraspinal muscles in adolescents with idiopathic scoliosis during habitual standing and sitting. BioMed Res. Int. 2015. [Google Scholar] [CrossRef] [PubMed]
- World Medical Association. Available online: https://www.wma.net/what-we-do/medical-ethics/declaration-of-helsinki/ (accessed on 22 February 2019).
- Cobb, J.R. Outline for the study of scoliosis. Instr. Course Lect. 1948, 5, 261–275. [Google Scholar]
- Bitan, F.D.; Veliskakis, K.P.; Campbell, B.C. Differences in the Risser grading systems in the United States and France. Clin. Orthop. Relat. Res. 2005, 436, 190–195. [Google Scholar] [CrossRef]
- European Patent Application. European Patent Office. Available online: https://patentimages.storage.googleapis.com/45/96/35/613305549c6251/EP3225155A1.pdf (accessed on 23 February 2019).
- Kamelska, A.M.; Protasiewicz-Fałdowska, H.; Zakrzewska, L.; Zaborowska-Sapeta, K.; Kowalski, I.M. Validation of SpinalMeter® biometrical assessment to improve posture diagnosis in children. J. Back Musculoskelet 2019. under review. [Google Scholar]
- Bunnell, W. Selective screening for scoliosis. Clin. Orthop. Relat. R 2005, 434, 40–45. [Google Scholar] [CrossRef]
- Bonagamba, G.H.; Coelho, D.M.; Oliveira, A.S. Inter and intra-rater reliability of the scoliometer. Braz. J. Phys. Ther. 2010, 14, 432–438. [Google Scholar] [CrossRef]
- McKenzie, R. Treat Your Own Back, 9th ed.; Spinal Publications New Zealand: Raumati Beach, New Zealand, 2011. [Google Scholar]
- TIBCO Software Inc. Statistica [Data Analysis Software Program], Version 13. 2017. Available online: http://statistica.io (accessed on 23 February 2019).
- Willner, S. Growth in height of children with scoliosis. Acta Orthop. Scand. 1974, 45, 854–866. [Google Scholar] [CrossRef] [PubMed]
- Calvo, I.J. Ohservations on the growth of the female adolescent spine and its relation to scoliosis. Clin. Orthop. 1957, 10, 40–47. [Google Scholar] [PubMed]
- James, J. Idiopathic scoliosis; The prognosis diagnosis and operative indications related to curve patterns and the age at onset. J. Bone Joint Surg. Br. 1954, 36-B, 36–49. [Google Scholar] [CrossRef] [PubMed]



| Variables/Age (Years) | Gender Man/Woman (Number) | Cobb (°) | ATR (°) | Risser Stage | Age (Years) | Height (m) | Body Mass (kg) | BMI (kg/m2) |
|---|---|---|---|---|---|---|---|---|
| 5–11 | 2/9 | 14 (10–28) | 1 (0–3) | 0 (0–3) | 8 (5–11) | 1.41 (1.19–1.74) | 34.0 (22.0–60.0) | 16.0 (14.3–19.8) |
| 12–16 | 1/15 | 13 (6–23) | 1 (1–3) | 2 (0–4) | 13 (12–16) | 1.61 (1.51–1.74) | 54.0 (34.0–61.5) | 18.9 (14.2–24.1) |
| Variables Age (Years) | Height (m) | BM 1 (kg) | BMI 2 (kg/m2) | Spine Length (cm) | Menarche | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre 3 | Post 4 | p5 | Pre | Post | p | Pre | Post | p | Pre | Post | p | No | Yes | |
| 5–11 | 1.420 | 1.440 | 0.00002 | 34.73 | 35.23 | 0.314 | 16.67 | 16.67 | 0.984 | 45.18 | 44.96 | 0.815 | n = 8 (29%) | n = 2 (7%) |
| ±0.175 | ±0.177 | ±11.83 | ±11.66 | ±1.910 | ±1.819 | ±4.724 | ±5.002 | |||||||
| 12–16 | 1.630 | 1.640 | 0.0008 | 51.22 | 52.16 | 0.004 | 19.32 | 19.41 | 0.390 | 51.22 | 51.08 | 0.79 | n = 6 (21%) | n = 12 (43%) |
| ±0.064 | ±0.064 | ±8.16 | ±8.02 | ±2.574 | ±2.430 | ±3.755 | ±4.192 | |||||||
| Variable Age (Years) | ATR [O] | p | |
|---|---|---|---|
| Pre | Post | ||
| 5–11 | 5.5 | 3.0 | 0.0002 |
| ±2.07 | ±2.45 | ||
| 12–16 | 5.2 | 3.0 | 0.00007 |
| ±2.11 | ±1.21 | ||
| Variables Age (Years) | Posterior View Asymmetry (°) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Shoulder | p | Scapular | p | Pelvic | p | PSIS 1 | p | |||||
| Pre | Post | Pre | Post | Pre | Post | Pre | Post | |||||
| Standing Position | ||||||||||||
| 5–11 | 0.720 ± 1.849 | 1.440 ± 2.203 | 0.261 | 0.470 ± 3.994 | 3.200 ± 3.373 | 0.002 | 0.250 ± 2.120 | −0.270 ± 2.610 | 0.567 | −0.480 ± 2.405 | 0.100 ± 2.130 | 0.431 |
| 12–16 | −0.770 ± 1.839 | −0.150 ± 1.787 | 0.183 | −0.210 ± 3.933 | 0.960 ± 4.476 | 0.262 | −0.400 ± 2.015 | 0.630 ± 1.434 | 0.135 | −0.780 ± 2.150 | −0.810 ± 1.636 | 0.958 |
| p | 0.271 | 0.218 | 0.979 | 0.561 | 0.877 | 0.990 | 0.845 | 0.728 | ||||
| Sitting Position | ||||||||||||
| 5–11 | 1.850 ± 1.675 | 0.650 ± 1.699 | 0.049 | 1.470 ± 3.612 | 3.290 ± 3.521 | 0.033 | 1.510 ± 2.346 | 1.510 ± 2.645 | 0.998 | 0.500 ± 3.266 | 0.860 ± 2.895 | 0.657 |
| 12–16 | 0.230 ± 1.925 | −0.210 ± 1.512 | 0.442 | 1.500 ± 3.568 | 1.010 ± 3.609 | 0.544 | −0.080 ± 1.358 | 0.940 ± 1.461 | 0.037 | −0.130 ± 2.391 | −0.560 ± 2.342 | 0.056 |
| p | 0.104 | 0.647 | 0.999 | 0.454 | 0.225 | 0.901 | 0.570 | 0.208 | ||||
| Variables Age (Years) | Anterior View Asymmetry (°) | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Eye | p | Mouth | p | Clavicle | p | ASIS 1 | p | Radial Styloid Process | p | ||||||
| Pre | Post | Pre | Post | Pre | Post | Pre | Post | Pre | Post | ||||||
| Standing Position | |||||||||||||||
| 5–11 | −1.080 ± 4.082 | 0.560 ± 2.873 | 0.077 | −1.740 ± 3.872 | −1.610 ± 3.997 | 0.909 | −0.690 ± 2.2280 | −0.380 ± 2.087 | 0.510 | 2.050 ± 1.802 | 2.060 ± 1.512 | 0.993 | −1.190 ± 3.070 | −1.110 ± 2.709 | 0.690 |
| 12–16 | −0.980 ± 4.459 | −0.140 ± 3.222 | 0.313 | −0.500 ± 4.049 | 0.100 ± 3.548 | 0.444 | 0.350 ± 2.481 | 0.640 ± 1.843 | 0.436 | 0.110 ± 1.243 | 1.120 ± 1.884 | 0.008 | 0.070 ± 1.558 | 0.240 ± 1.166 | 0.598 |
| p | 0.953 | 0.571 | 0.434 | 0.252 | 0.277 | 0.191 | 0.003 | 0.184 | 0.171 | 0.111 | |||||
| Variables | Age (Years) | Left | Right | |||||
|---|---|---|---|---|---|---|---|---|
| Pre | Post | p | Pre | Post | p | |||
| Length (mm) | Acromion–Heel | 5–11 | 1199.850 ± 33.211 | 1212.430 ± 32.630 | 0.014 | 1197.100 ± 33.501 | 1205.720 ± 32.143 | 0.084 |
| 12–16 | 1384.350 ± 27.537 | 1387.860 ± 27.056 | 0.682 | 1385.490 ± 27.778 | 1388.950 ± 26.652 | 0.625 | ||
| Acromion–PSIS 1 | 5–11 | 341.660 ± 40.274 | 340.080 ± 9.402 | 0.522 | 336.190 ± 41.388 | 332.500 ± 9.385 | 0.183 | |
| 12–16 | 427.780 ± 9.402 | 385.100 ± 7.796 | 0.642 | 423.740 ± 34.317 | 379.670 ± 7.781 | 0.609 | ||
| Acromion–Iliac crest | 5–11 | 273.250 ± 7.302 | 284.420 ± 7.723 | 0.033 | 271.440 ± 35.07 | 281.330 ± 8.627 | 0.050 | |
| 12–16 | 312.290 ± 6.055 | 319.470 ± 6.404 | 0.003 | 351.730 ± 29.076 | 322.450 ± 7.153 | 0.056 | ||
| Iliac crest–Heel | 5–11 | 926.750 ± 54.111 | 928.640 ± 26.905 | 0.999 | 925.950 ± 53.525 | 924.870 ± 61.466 | 0.999 | |
| 12–16 | 1024.050 ± 44.866 | 1068.570 ± 22.308 | 0.408 | 1023.740 ± 44.381 | 1004.290 ± 50.965 | 0.098 | ||
| PSIS–Heel | 5–11 | 866.060 ± 122.502 | 880.650 ± 122.099 | 0.00002 | 867.280 ± 123.607 | 879.900 ± 121.992 | 0.0001 | |
| 12–16 | 969.720 ± 172.643 | 1014.810 ± 45.290 | 0.283 | 971.040 ± 168.358 | 1017.380 ± 44.606 | 0.258 | ||
| Varus–Valgus | 5–11 | 188.210 ± 0.999 | 189.010 ± 1.007 | 0.259 | 185.560 ± 0.991 | 186.500 ± 0.928 | 0.240 | |
| 12–16 | 188.070 ± 0.828 | 188.690 ± 0.835 | 0.018 | 185.780 ± 0.822 | 186.970 ± 0.769 | 0.0002 | ||
| Heel–Popliteus Fossa | 5–11 | 414.040 ± 33.872 | 409.410 ± 12.161 | 0.454 | 416.600 ± 33.781 | 408.340 ± 12.216 | 0.168 | |
| 12–16 | 511.280 ± 28.085 | 476.050 ± 10.084 | 0.438 | 511.240 ± 28.010 | 478.880 ± 10.129 | 0.796 | ||
| Angle (°) | Heel–Popliteus Fossa | 5–11 | 188.210 ± 16.051 | 189.010 ± 1.007 | 0.259 | 185.560 ± 16.395 | 186.500 ± 0.928 | 0.240 |
| 12–16 | 204.850 ± 13.308 | 188.690 ± 0.825 | 0.205 | 203.000 ± 13.594 | 186.970 ± 0.769 | 0.011 | ||
| Variables | Age (Years) | Left Side | Right Side | |||||
|---|---|---|---|---|---|---|---|---|
| Pre | Post | p | Pre | Post | p | |||
| Length (mm) | Acromion–Iliac crest | 5–11 | 273.120 ± 9.195 | 272.610 ± 8.047 | 0.925 | 271.200 ± 8.264 | 276.050 ± 8.147 | 0.408 |
| 12–16 | 315.530 ± 7.624 | 310.330 ± 6.673 | 0.594 | 314.030 ± 6.852 | 314.940 ± 6.755 | 0.020 | ||
| Acromion–PSIS 1 | 5–11 | 357.180 ± 10.604 | 352.030 ± 10.731 | 0.180 | 351.380 ± 9.901 | 348.640 ± 10.851 | 0.630 | |
| 12–16 | 409.610 ± 8.792 | 406.600 ± 8.897 | 0.326 | 404.810 ± 8.209 | 401.550 ± 8.997 | 0.425 | ||
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kamelska-Sadowska, A.M.; Protasiewicz-Fałdowska, H.; Zakrzewska, L.; Zaborowska-Sapeta, K.; Nowakowski, J.J.; Kowalski, I.M. The Effect of an Innovative Biofeedback SKOL-AS® Treatment on the Body Posture and Trunk Rotation in Children with Idiopathic Scoliosis—Preliminary Study. Medicina 2019, 55, 254. https://doi.org/10.3390/medicina55060254
Kamelska-Sadowska AM, Protasiewicz-Fałdowska H, Zakrzewska L, Zaborowska-Sapeta K, Nowakowski JJ, Kowalski IM. The Effect of an Innovative Biofeedback SKOL-AS® Treatment on the Body Posture and Trunk Rotation in Children with Idiopathic Scoliosis—Preliminary Study. Medicina. 2019; 55(6):254. https://doi.org/10.3390/medicina55060254
Chicago/Turabian StyleKamelska-Sadowska, Anna M., Halina Protasiewicz-Fałdowska, Lidia Zakrzewska, Katarzyna Zaborowska-Sapeta, Jacek J. Nowakowski, and Ireneusz M. Kowalski. 2019. "The Effect of an Innovative Biofeedback SKOL-AS® Treatment on the Body Posture and Trunk Rotation in Children with Idiopathic Scoliosis—Preliminary Study" Medicina 55, no. 6: 254. https://doi.org/10.3390/medicina55060254
APA StyleKamelska-Sadowska, A. M., Protasiewicz-Fałdowska, H., Zakrzewska, L., Zaborowska-Sapeta, K., Nowakowski, J. J., & Kowalski, I. M. (2019). The Effect of an Innovative Biofeedback SKOL-AS® Treatment on the Body Posture and Trunk Rotation in Children with Idiopathic Scoliosis—Preliminary Study. Medicina, 55(6), 254. https://doi.org/10.3390/medicina55060254





