Knowledge about Disease, Medication Therapy, and Related Medication Adherence Levels among Patients with Hypertension
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Subjects
2.2. Questionnaire
2.2.1. Demographic Characteristics
2.2.2. Knowledge about Disease and Its Control
2.2.3. Medication Therapy Overview
2.2.4. Adherence Level
2.3. Statistical Analysis
3. Results
3.1. Demographic Characteristics
3.2. Knowledge about Disease and Its Control
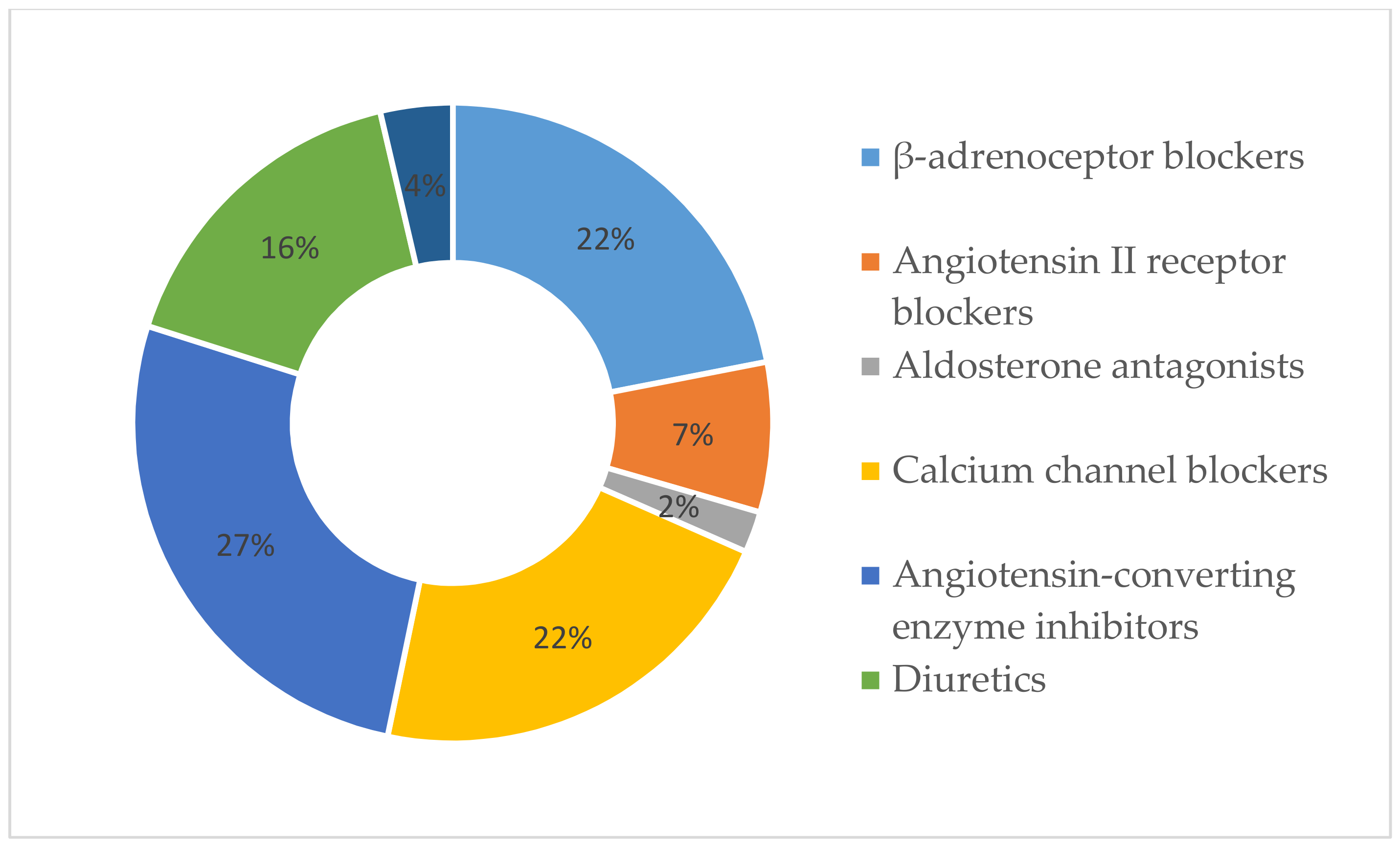
3.3. Medication Therapy Overview
3.4. Difference between Adherent and Non-Adherent Groups
4. Discussion
5. Conclusions
- The adherent patients rated themselves higher than did the non-adherent ones in relation to the extent to which they follow the medication prescriptions of their family physician.
- The adherence level correlated with the patients’ age and did not depend on gender—the older the patient, the more adherent he or she is. The difference between adherence and number of prescribed drugs, number of food supplements, education level, and BMI was not statistically significant. It is important to increase the sample size.
- A higher adherence level was observed for those patients who had been taking medications for hypertension for a longer period of time.
- Anxiety and doubt are possibly the factors that influence the patients’ medication-taking habits; these factors were also the cause for the patient not informing their family physician regarding other medications and nutritional supplements that they were taking.
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- WHO. Blood Pressure. Available online: https://www.who.int/gho/ncd/risk_factors/blood_pressure_prevalence/en/ (accessed on 5 January 2019).
- Cimmaruta, D.; Lombardi, N.; Borghi, C.; Rosano, G.; Rossi, F.; Mugelli, A. Polypill, hypertension and medication adherence: The solution strategy? Int. J. Cardiol. 2018, 252, 181–186. [Google Scholar] [CrossRef] [PubMed]
- Abegaz, T.M.; Shehab, A.; Gebreyohannes, E.A.; Bhagavathula, A.S.; Elnour, A.A. Nonadherence to antihypertensive drugs a systematic review and meta-analysis. Medicine 2017, 96, e5641. [Google Scholar] [CrossRef] [PubMed]
- WHO. Raised Blood Pressure. Available online: https://www.who.int/gho/ncd/risk_factors/blood_pressure_text/en/ (accessed on 5 January 2019).
- World Health Organization. HEARTS Technical Package for Cardiovascular Disease Management in Primary Health Care: Evidence-Based Treatment Protocols. Available online: http://apps.who.int/iris/bitstream/handle/10665/260421/WHO-NMH-NVI-18.2-eng.pdf?sequence=1&ua=1 (accessed on 10 January 2019).
- WHO. Raised Blood Pressure. Available online: https://www.who.int/gho/ncd/risk_factors/blood_pressure_prevalence_text/en/ (accessed on 27 January 2019).
- Payne, K.A.; Esmonde-white, S. Observational Studies of Antihypertensive Medication Use and Compliance: Is Drug Choice a Factor in Treatment Adherence? Curr. Hypertens. Rep. 2000, 2, 515–524. [Google Scholar] [CrossRef] [PubMed]
- Uludag, A.; Sahin, E.M.; Agaoglu, H.; Gungor, S.; Ertekin, Y.H.; Tekin, M. Are blood pressure values compatible with medication adherence in hypertensive patients? Niger. J. Clin. Pract. 2016, 19, 460–464. [Google Scholar] [CrossRef]
- Brown, M.T.; Bussell, J.K. Medication adherence: WHO cares? Mayo Clin. Proc. 2011, 86, 304–314. [Google Scholar] [CrossRef] [PubMed]
- Feldman, M.D.; Christensen, J.F.; Satterfield, J.M. (Eds.) Behavioral Medicine: A Guide for Clinical Practice, 4th ed.; McGraw-Hill: New York, NY, USA, 2014. [Google Scholar]
- Jankowska-Polańska, B.; Uchmanowicz, I.; Dudek, K.; Mazur, G. Relationship between patients’ knowledge and medication adherence among patients with hypertension. Patient Prefer. Adherence 2016, 10, 2437–2447. [Google Scholar] [CrossRef]
- World Health Organization. Adherence to Long-Term Therapies: Evidence for Action. Available online: https://www.who.int/chp/knowledge/publications/adherence_full_report.pdf?ua=1%0Ahttp://apps.who.int/iris/bitstream/handle/10665/42682/9241545992.pdf;jsessionid=CDD86C112AFF1779BA4E602BAAF11AA0?sequence=1 (accessed on 15 December 2018).
- Chen, Y.; Yang, L.; Hu, H.; Chen, J.; Shen, B. How to Become a Smart Patient in the Era of Precision. In Healthcare and Big Data Management; Shen, B., Ed.; Springer Nature: Singapore, 2017; pp. 1–16. [Google Scholar]
- Moon, S.J.; Lee, W.Y.; Hwang, J.S.; Hong, Y.P.; Morisky, D.E. Accuracy of a screening tool for medication adherence: A systematic review and meta-analysis of the Morisky Medication Adherence Scale-8. PLoS ONE 2017, 12, e0187139. [Google Scholar] [CrossRef]
- Okello, S.; Nasasira, B.; Muiru, A.N.W.; Muyingo, A. Validity and Reliability of a Self-Reported Measure of Antihypertensive Medication Adherence in Uganda The Harvard community has made this article openly available. PLoS ONE 2018, 11, 1–11. [Google Scholar]
- Lee, G.K.; Wang, H.H.; Liu, K.Q.; Cheung, Y.; Morisky, D.E.; Wong, M.C. Determinants of Medication Adherence to Antihypertensive Medications among a Chinese Population Using Morisky Medication Adherence Scale. PLoS ONE 2013, 8, e62775. [Google Scholar] [CrossRef]
- Yassine, M.; Al-Hajje, A.; Awada, S.; Rachidi, S.; Zein, S.; Bawab, W.; Zeid, M.B.; El Hajj, M.; Salameh, P. Evaluation of medication adherence in Lebanese hypertensive patients. J. Epidemiol. Glob. Health 2016, 6, 157–167. [Google Scholar] [CrossRef][Green Version]
- Jankowska-Polanska, B.; Uchmanowicz, I.; Chudiak, A.; Dudek, K.; Morisky, D.E.; Szymanska-Chabowska, A. Psychometric properties of the polish version of the eight-item morisky medication adherence scale in hypertensive adults. Patient Prefer. Adherence 2016, 10, 1759–1766. [Google Scholar] [CrossRef] [PubMed]
- Al-Ramahi, R. Adherence to medications and associated factors: A cross-sectional study among Palestinian hypertensive patients. J. Epidemiol. Glob. Health 2015, 5, 125–132. [Google Scholar] [CrossRef] [PubMed]
- Morrison, V.L.; Holmes, E.A.; Parveen, S.; Plumpton, C.O.; Clyne, W.; De Geest, S.; Dobbels, F.; Vrijens, B.; Kardas, P.; Hughes, D.A. Predictors of Self-Reported Adherence to Antihypertensive Medicines: A Multinational, Cross-Sectional Survey. Value Heal 2015, 18, 206–216. [Google Scholar] [CrossRef] [PubMed]
- Arnet, I.; Metaxas, C.; Walter, P.N.; Morisky, D.E.; Hersberger, K.E. The 8-item Morisky Medication Adherence Scale translated in German and validated against objective and subjective polypharmacy adherence measures in cardiovascular patients. J. Eval. Clin. Pract. 2015, 21, 271–277. [Google Scholar] [CrossRef]
- Morisky, D.E.; Ang, A.; Krousel-Wood, M. Predictive validity of a medication adherence measure for hypertension control. J. Clin. Hypertens. 2008, 10, 348–354. [Google Scholar] [CrossRef]
- Morisky, D.E.; DiMatteo, M.R. Improving the measurement of self-reported medication nonadherence. J. Clin. Epidemiol. 2011, 64, 250–254. [Google Scholar]
- Berlowitz, D.R.; Foy, C.G.; Kazis, L.E.; Bolin, L.; Conroy, L.B.; Fitzpatrick, P.; Gure, T.R.; Kimmel, P.L.; Kirscner, K.; Morisky, D.E.; et al. Impact of Intensive Blood Pressure Therapy on Patient-Reported Outcomes: Outcomes Results from the SPRINT Study. N. Engl. J. Med. 2017, 377, 733–744. [Google Scholar] [CrossRef]
- Janežič, A.; Locatelli, I.; Kos, M. Criterion validity of 8-item Morisky Medication Adherence Scale in patients with asthma. PLoS ONE 2017, 12, 1–10. [Google Scholar] [CrossRef]
- Krousel-Wood, M.; Islam, T.; Webber, L.S.; Re, R.; Morisky, D.E.; Muntner, P. New medication adherence scale versus pharmacy fill rates in seniors with hypertension. Am. J. Manag. Care 2009, 15, 59–66. [Google Scholar]
- Jankowska-Polańska, B.; Chudiak, A.; Uchmanowicz, I.; Dudek, K.; Mazur, G. Selected factors affecting adherence in the pharmacological treatment of arterial hypertension. Patient Prefer. Adherence 2017, 11, 363–371. [Google Scholar] [CrossRef]
- WHO. WHO EMRO|High Blood Pressure and Physical activity|World Health Day 2013|World Health Days. Available online: http://www.emro.who.int/media/world-health-day/physical-activity-factsheet-2013.html (accessed on 25 January 2019).
- Han, E.; Sohn, H.S.; Lee, J.Y.; Jang, S. Health Behaviors and Medication Adherence in Elderly Patients. Am. J. Heal. Promot. 2017, 31, 278–286. [Google Scholar] [CrossRef] [PubMed]
- Khan, M.; Shah, S.; Hameed, T. Barriers to and determinants of medication adherence among hypertensive patients attended National Health Service Hospital, Sunderland. J. Pharm. Bioallied Sci. 2014, 6, 104. [Google Scholar] [CrossRef] [PubMed]
- Dimatteo, M.R.; Haskard, K. Physician communication and patient adherence to treatment: A Meta-analysis. Med. Care 2009, 47, 826–834. [Google Scholar]
- Pakalpojumi Speciālistiem. Available online: https://www.eveseliba.gov.lv/sakums/pakalpojumi?fbclid=IwAR0Q6kn_tr5kDEbmK96ToE0r0bvlkwmajyamy-8XCliJe3dNAkMjg84tjbA (accessed on 7 May 2019).
- Tarn, D.M.; Heritage, J.; Paterniti, D.A.; Hays, R.D.; Kravitz, R.L.; Wenger, N.S. Physician communication when prescribing new medications. Arch. Intern. Med. 2006, 166, 1855–1862. [Google Scholar] [CrossRef]
- Davis, E.M.; Packard, K.A.; Jackevicius, C.A. The pharmacist role in predicting and improving medication adherence in heart failure patients. J. Manag. Care Pharm. 2014, 20, 741–755. [Google Scholar] [CrossRef]
- Readdean, K.C.; Heuer, A.J.; Scott Parrott, J. Effect of pharmacist intervention on improving antidepressant medication adherence and depression symptomology: A systematic review and meta-analysis. Res. Soc. Adm. Pharm. 2018, 14, 321–331. [Google Scholar] [CrossRef]
- Butler, M.J.; Tanner, R.M.; Muntner, P.; Shimbo, D.; Bress, A.P.; Shallcross, A.J.; Sims, M.; Ogedegbe, G.; Spruill, T.M. Adherence to antihypertensive medications and associations with blood pressure among African Americans with hypertension in the Jackson Heart Study. J. Am. Soc. Hypertens. 2017, 11, 581–588.e5. [Google Scholar] [CrossRef]
- Ajzen, I. The Theory of Planned Behavior. Organ. Behav. Hum. Decis. Process. 1991, 25, 179–211. [Google Scholar] [CrossRef]
- Ladova, K.; Vlcek, J.; Vytrisalova, M.; Maly, J. Healthy adherer effect-The pitfall in the interpretation of the effect of medication adherence on health outcomes. J. Eval. Clin. Pract. 2014, 20, 111–116. [Google Scholar] [CrossRef]
- Jankowska-Polańska, B.; Blicharska, K.; Uchmanowicz, I.; Morisky, D.E. The influence of illness acceptance on the adherence to pharmacological and non-pharmacological therapy in patients with hypertension. Eur. J. Cardiovasc. Nurs. 2016, 15, 559–568. [Google Scholar] [CrossRef]
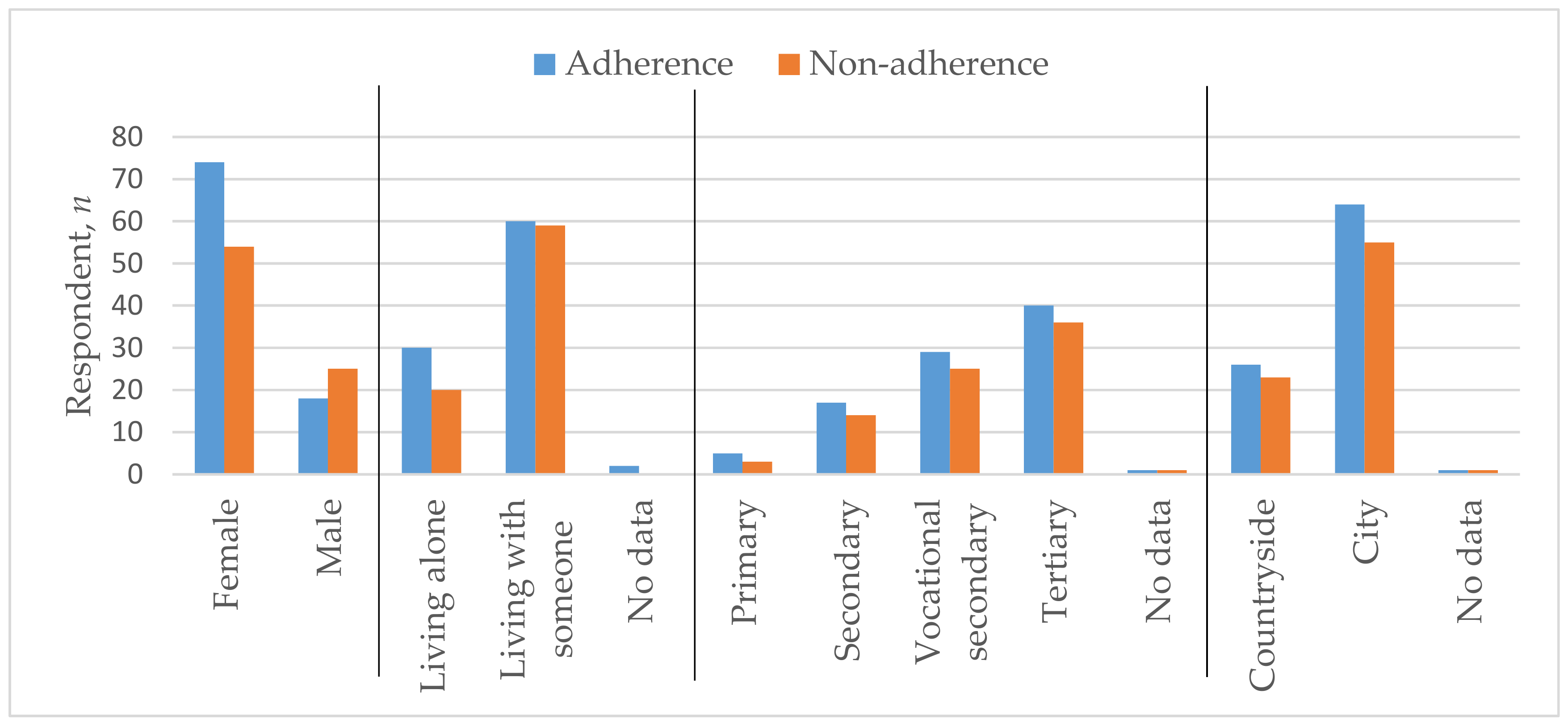
| Characteristic | Adherence | Non-Adherence | ||
|---|---|---|---|---|
| Mean | SD | Mean | SD | |
| Age | 67.73 | 12.27 | 60.52 | 13.63 |
| n | Percent | n | Percent | |
| Sex | ||||
| Female | 74 | 80.4 | 54 | 68.4 |
| Male | 18 | 19.6 | 25 | 31.6 |
| Marital status | ||||
| Living alone | 30 | 32.6 | 20 | 25.3 |
| Living with someone | 60 | 65.2 | 59 | 74.7 |
| Education Level | ||||
| Primary | 5 | 5.4 | 3 | 3.8 |
| Secondary | 17 | 18.5 | 14 | 17.7 |
| Vocational secondary | 29 | 31.5 | 25 | 31.6 |
| Tertiary | 40 | 43.5 | 36 | 45.6 |
| Residence | ||||
| Countryside | 26 | 28.3 | 23 | 29.1 |
| City | 64 | 69.6 | 55 | 69.6 |
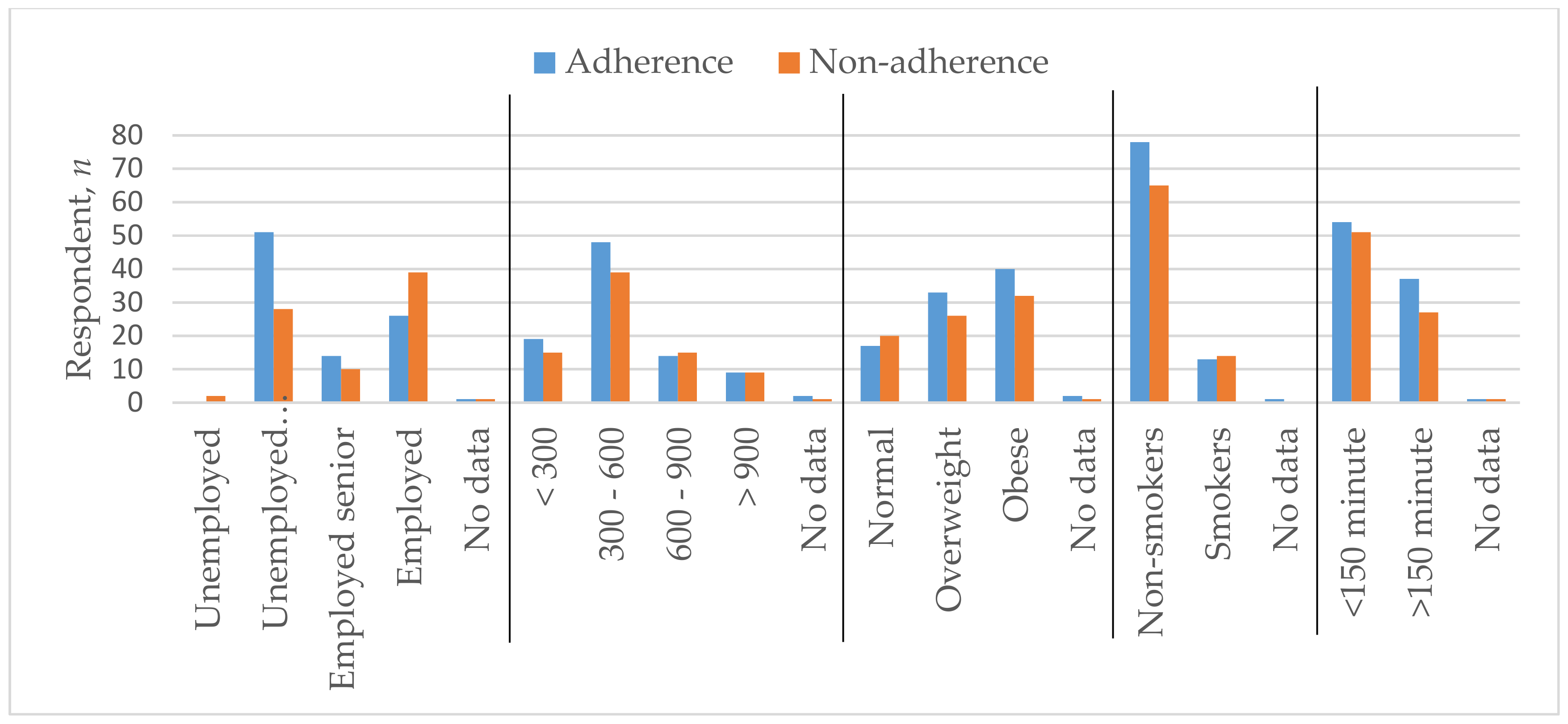
| Employment status | ||||
| Unemployed | 0 | 0.0 | 2 | 2.5 |
| Unemployed senior | 51 | 55.4 | 28 | 35.4 |
| Employed senior | 14 | 15.2 | 10 | 12.7 |
| Employed | 26 | 28.3 | 39 | 49.4 |
| Monthly income after taxes in euros | ||||
| <300 | 19 | 20.7 | 15 | 19.0 |
| 300–600 | 48 | 52.2 | 39 | 49.4 |
| 600–900 | 14 | 15.2 | 15 | 19.0 |
| >900 | 9 | 9.8 | 9 | 11.4 |
| Body mass index (BMI) | ||||
| Normal | 17 | 18.5 | 20 | 25.3 |
| Overweight | 33 | 35.9 | 26 | 32.9 |
| Obese | 40 | 43.5 | 32 | 40.5 |
| Smoking status | ||||
| Non-smoker | 78 | 84.8 | 65 | 82.3 |
| Smoker | 13 | 14.1 | 14 | 17.7 |
| Physical activity | ||||
| <150 min | 54 | 58.7 | 51 | 64.6 |
| >150 min | 37 | 40.2 | 27 | 34.2 |
| Parameter | p-Value | Correlation Coefficient |
|---|---|---|
| Age | 0.001 | 0.263 |
| Daily medicine amount | 0.124 | 0.119 |
| Food supplement amount | 0.551 | 0.047 |
| Duration of disease | 0.012 | 0.192 |
| Following the medication prescriptions of their family physician | <0.0001 | 0.384 |
| Education level | 0.312 | −0.780 |
| BMI | 0.095 | 0.129 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gavrilova, A.; Bandere, D.; Rutkovska, I.; Šmits, D.; Mauriņa, B.; Poplavska, E.; Urtāne, I. Knowledge about Disease, Medication Therapy, and Related Medication Adherence Levels among Patients with Hypertension. Medicina 2019, 55, 715. https://doi.org/10.3390/medicina55110715
Gavrilova A, Bandere D, Rutkovska I, Šmits D, Mauriņa B, Poplavska E, Urtāne I. Knowledge about Disease, Medication Therapy, and Related Medication Adherence Levels among Patients with Hypertension. Medicina. 2019; 55(11):715. https://doi.org/10.3390/medicina55110715
Chicago/Turabian StyleGavrilova, Anna, Dace Bandere, Ieva Rutkovska, Dins Šmits, Baiba Mauriņa, Elita Poplavska, and Inga Urtāne. 2019. "Knowledge about Disease, Medication Therapy, and Related Medication Adherence Levels among Patients with Hypertension" Medicina 55, no. 11: 715. https://doi.org/10.3390/medicina55110715
APA StyleGavrilova, A., Bandere, D., Rutkovska, I., Šmits, D., Mauriņa, B., Poplavska, E., & Urtāne, I. (2019). Knowledge about Disease, Medication Therapy, and Related Medication Adherence Levels among Patients with Hypertension. Medicina, 55(11), 715. https://doi.org/10.3390/medicina55110715





