Assessment of coronary care management and hospital mortality from ST-segment elevation myocardial infarction in the Kazakhstan population: Data from 2012 to 2015
Abstract
:1. Introduction
2. Materials and methods
2.1. Study design and subjects
2.2. Data collection
2.3. Definitions
2.4. Statistical analysis
2.5. Ethics statement
3. Results
3.1. Baseline characteristics of the study population
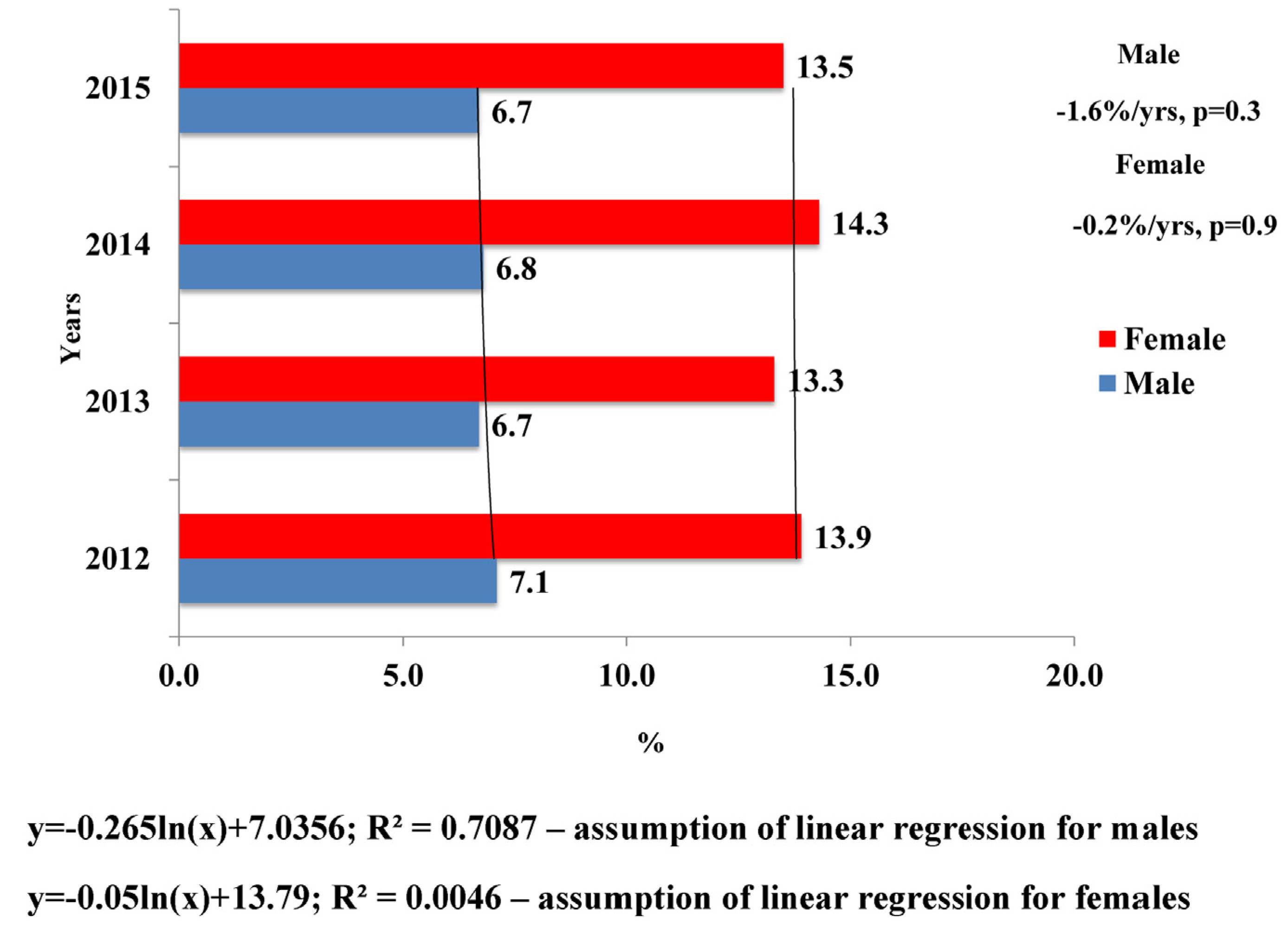
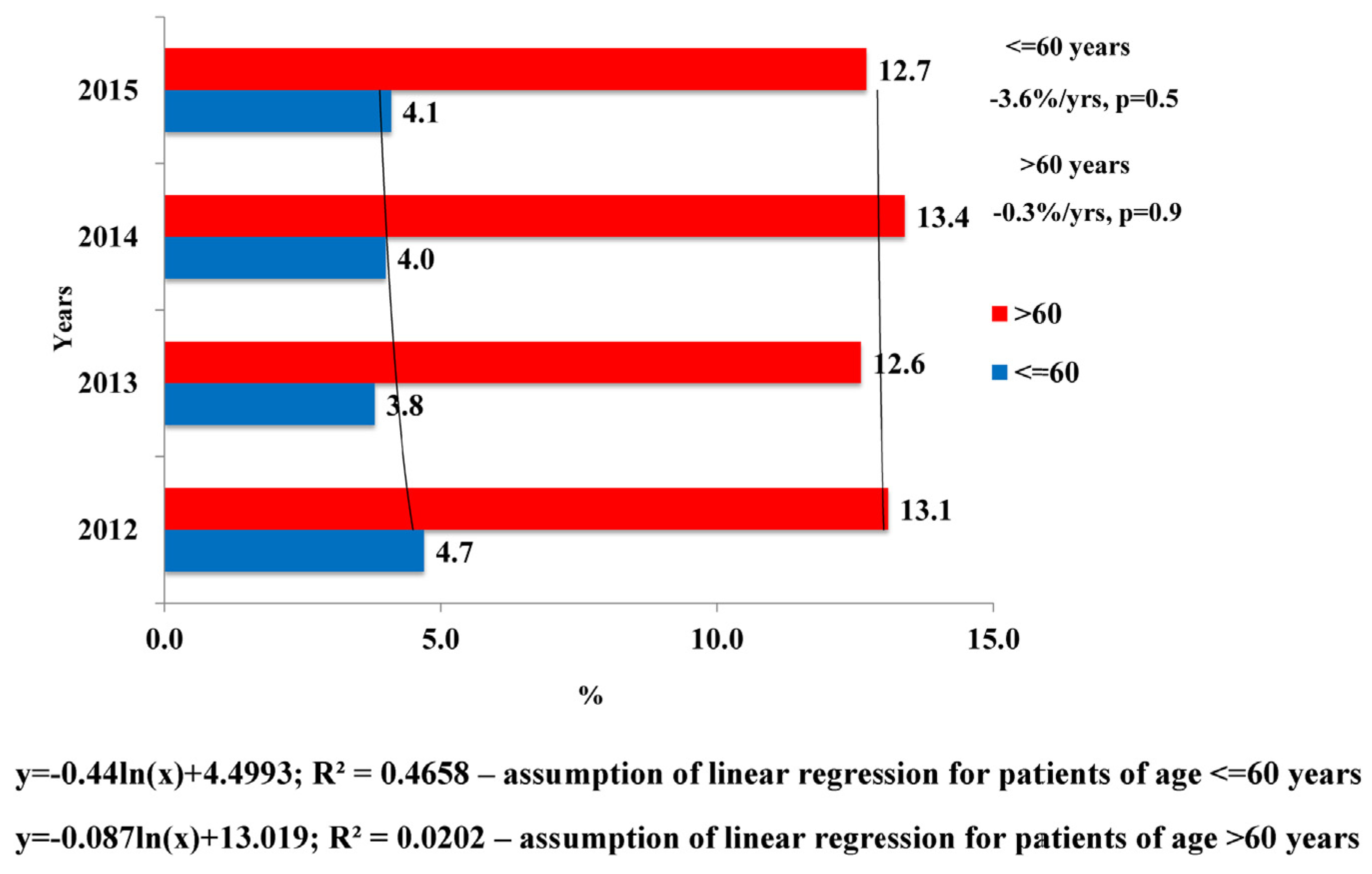
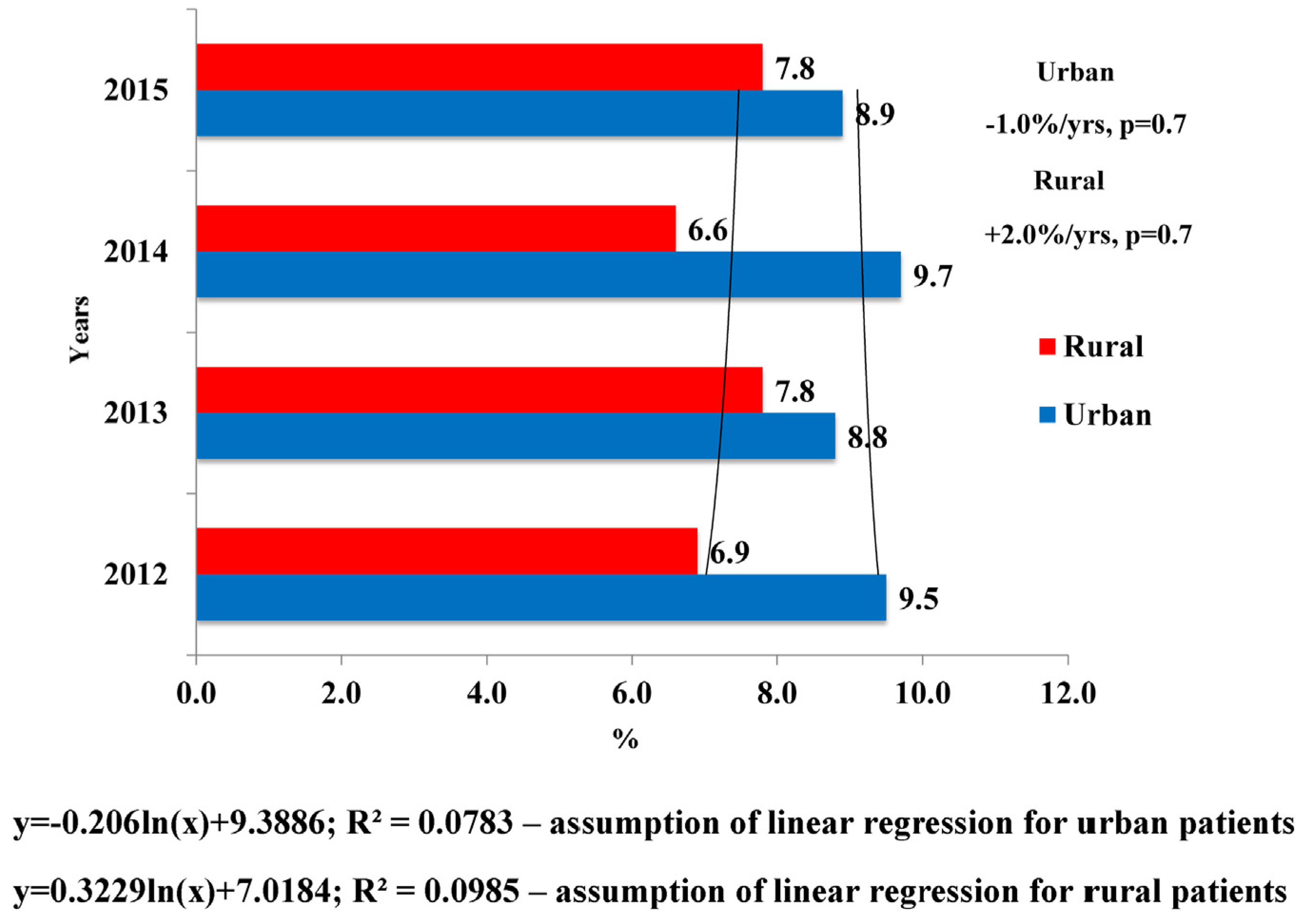
3.2. Clinical outcomes according to sociodemographic factors and time from hospitalization to PCI
3.3. Factors related to hospital mortality due to STEMI with PCI
4. Discussion
5. Conclusions
Conflict of interest
R E F E R E N C E S
- McManus, DD; Gore, J; Yarzebski, J; Spencer, F; Lessard, D; Goldberg, RJ. Recent trends in the incidence, treatment, and outcomes of patients with STEMI and NSTEMI. Am J Med 2011, 124, 40–7. [Google Scholar] [CrossRef] [PubMed]
- Rosamond, WD; Chambless, LE; Heiss, G; Mosley, TH; Coresh, J; Whitsel, E; et al. Twenty-two-year trends in incidence of myocardial infarction, coronary heart disease mortality, and case fatality in 4 US communities, 1987–2008. Circulation 2012, 125, 1848–57. [Google Scholar] [CrossRef] [PubMed]
- Hong, JS; Kang, HC; Lee, SH; Kim, J. Long-term trend in the incidence of acute myocardial infarction in Korea: 1997–2007. Korean Circ J 2009, 39, 467–76. [Google Scholar] [CrossRef] [PubMed]
- Lloyd-Jones, D; Adams, R; Carnethon, M; De Simone, G; Ferguson, TB; Flegal, K; et al. Heart disease and stroke statistics—2009 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation 2009, 119, e21–181. [Google Scholar] [PubMed]
- HFA-DB. 2015. http://www.euro.who.int/en/data-and-evidence/ databases/european-health-for-all-database-hfa-db.
- Schomig, A; Ndrepepa, G; Mehilli, J; Schwaiger, M; Schuhlen, H; Nekolla, S; et al. Therapy-dependent influence of time-to-treatment interval on myocardial salvage in patients with acute myocardial infarction treated with coronary artery stenting or thrombolysis. Circulation 2003, 108, 1084–8. [Google Scholar] [CrossRef] [PubMed]
- Van de Werf, F; Bax, J; Betriu, A; Blomstrom-Lundqvist, C; Crea, F; Falk, V; et al. Management of acute myocardial infarction in patients presenting with persistent ST-segment elevation: the Task Force on the Management of ST-Segment Elevation Acute Myocardial Infarction of the European Society of Cardiology. Eur Heart J 2008, 29, 2909–45. [Google Scholar] [CrossRef] [PubMed]
- Gibson, CM; Pride, YB; Frederick, PD; Pollack, CV, Jr.; Canto, JG; Tiefenbrunn, AJ; et al. Trends in reperfusion strategies, door-to-needle and door-to-balloon times, and in-hospital mortality among patients with ST-segment elevation myocardial infarction enrolled in the National Registry of Myocardial Infarction from 1990 to 2006. Am Heart J 2008, 156, 1035–44. [Google Scholar] [CrossRef] [PubMed]
- Francone, M; Bucciarelli-Ducci, C; Carbone, I; Canali, E; Scardala, R; Calabrese, FA; et al. Impact of primary coronary angioplasty delay on myocardial salvage, infarct size, and microvascular damage in patients with ST-segment elevation myocardial infarction: insight from cardiovascular magnetic resonance. J Am Coll Cardiol 2009, 54, 2145–53. [Google Scholar] [CrossRef] [PubMed]
- Gross, BW; Dauterman, KW; Moran, MG; Kotler, TS; Schnugg, SJ; Rostykus, PS; et al. An approach to shorten time to infarct artery patency in patients with ST-segment elevation myocardial infarction. Am J Cardiol 2007, 99, 1360–3. [Google Scholar] [CrossRef] [PubMed]
- Nam, YH; Cha, KS; Kim, JH; Park, SY; Park, TH; Kim, MH; et al. Reduction of door-to-balloon time by new performance processes in patients with ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention. Angiology 2011, 62, 257–64. [Google Scholar]
- Blankenship, JC; Scott, TD; Skelding, KA; Haldis, TA; Tompkins-Weber, K; Sledgen, MY; et al. Door-to-balloon times under 90 min can be routinely achieved for patients transferred for ST-segment elevation myocardial infarction percutaneous coronary intervention in a rural setting. J Am Coll Cardiol 2011, 57, 272–9. [Google Scholar] [CrossRef] [PubMed]
- Freisinger, E; Fuerstenberg, T; Malyar, NM; Wellmann, J; Keil, U; Breithardt, G; et al. German nationwide data on current trends and management of acute myocardial infarction: discrepancies between trials and real-life. Eur Heart J 2014, 35(15), 979–88. [Google Scholar] [CrossRef] [PubMed]
- Park, YH; Kang, GH; Song, BG; Chun, WJ; Lee, JH; Hwang, SY; et al. Factors related to prehospital time delay in acute ST-segment elevation myocardial infarction. J Korean Med Sci 2012, 27(8), 864–9. [Google Scholar] [CrossRef] [PubMed]
- Khera, S; Kolte, D; Palaniswamy, C; Mujib, M; Aronow, WS; Singh, T; et al. ST-elevation myocardial infarction in the elderly temporal trends in incidence, utilization of percutaneous coronary intervention and outcomes in the United States. Int J Cardiol 2013, 168, 3683–90. [Google Scholar] [CrossRef] [PubMed]
- Doggen, CJ; Zwerink, M; Droste, HM; Brouwers, PJ; van Houwelingen, GK; van Eenennaam, FL; et al. Prehospital paths and hospital arrival time of patients with acute coronary syndrome or stroke, a prospective observational study. BMC Emerg Med 2016, 16, 3. http://dx.doi.org/10.1186/s12873-015-0065-y. [CrossRef] [PubMed]
- Steg, PG; James, SK; Atar, D; Badano, LP; Blömstrom-Lundqvist, C; Borger, MA; et al. ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation The Task Force on the management of ST-segment elevation acute myocardial infarction of the European Society of Cardiology (ESC). Eur Heart J 2012, 33, 2569–619. [Google Scholar] [PubMed]
- O’Gara, PT; Kushner, FG; Ascheim, DD; Casey, DE, Jr.; Chung, MK; de Lemos, JA; et al. ACCF/AHA guideline for the management of ST-elevation myocardial infarction: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2013, 61, 485–510. [Google Scholar]
- Thygesen, K; Alpert, JS; White, HD. Universal definition of myocardial infarction. Eur Heart J 2007, 28, 2525–38. [Google Scholar] [PubMed]
- Song, YB; Hahn, JY; Gwon, HC; Kim, JH; Lee, SH; Jeong, MH. The impact of initial treatment delay using primary angioplasty on mortality among patients with acute myocardial infarction: from the Korea acute myocardial infarction registry. J Korean Med Sci 2008, 23, 357–64. [Google Scholar] [CrossRef] [PubMed]
- Kim, JA; Jeong, JO; Ahn, KT; Park, HS; Jang, WI; Kim, MS; et al. Causative factors for time delays in patients with acute ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention. Korean J Med 2010, 78, 586–94. [Google Scholar]
- Kassaian, SE; Masoudkabir, F; Sezavar, H; Mohammadi, M; Pourmoghaddas, A; Kojouri, J; et al. Clinical characteristics, management and 1-year outcomes of patients with acute coronary syndrome in Iran: the Iranian Project for Assessment of Coronary Events 2 (IPACE2). BMJ Open 2015, 5(12), e007786. [Google Scholar] [CrossRef] [PubMed]
- Studenčan, M; Hricák, V; Kovář, F; Kurray, P; Murín, J; Kamenský, G; et al. Implementation of ESC-STEMI guidelines into clinical practice: an analysis of the Slovak Registry of Acute Coronary Syndromes (SLOVAKS). J Cardiovasc Med (Hagerstown) 2011, 12(5), 353–5. [Google Scholar]
- Poloński, L; Gąsior, M; Gierlotka, M; Kalarus, Z; Cieśliński, A; Dubiel, JS; et al. Polish Registry of Acute Coronary Syndromes (PL-ACS): characteristics, treatments and outcomes of patients with acute coronary syndromes in Poland. Kardiol Pol 2007, 65, 861–72. [Google Scholar]
- Postma, S; Dambrink, JH; de Boer, MJ; Gosselink, AT; Eggink, GJ; van de Wetering, H; et al. Prehospital triage in the ambulance reduces infarct size and improves clinical outcome. Am Heart J 2011, 161, 276–82. [Google Scholar] [CrossRef] [PubMed]
- De Luca, G; Suryapranata, H; Ottervanger, JP; Antman, EM. Time delay to treatment and mortality in primary angioplasty for acute myocardial infarction: every minute of delay counts. Circulation 2004, 109, 1223–5. [Google Scholar] [CrossRef] [PubMed]
- Terkelsen, CJ; Christiansen, EH; Sorensen, JT; Kristensen, SD; Lassen, JF; Thuesen, L; et al. Primary PCI as the preferred reperfusion therapy in STEMI: it is a matter of time. Heart 2009, 95, 362–9. [Google Scholar] [CrossRef] [PubMed]
- Flynn, A; Moscucci, M; Share, D; Smith, D; LaLonde, T; Changezi, H; et al. Trends in door-to-balloon time and mortality in patients with ST-elevation myocardial infarction undergoing primary percutaneous coronary intervention. Arch Intern Med 2010, 170, 1842–9. [Google Scholar] [CrossRef]
- Swaminathan, RV; Wang, TY; Kaltenbach, LA; Kim, LK; Minutello, RM; Bergman, G; et al. Nonsystem reasons for delay in door-to-balloon time and associated in-hospital mortality: a report from the national cardiovascular data registry. J Am Coll Cardiol 2013, 61, 1688–95. [Google Scholar] [CrossRef] [PubMed]
- Érlikh, AD; Gratsianskiĭ, NA; Participants of the RECORD Registry. The RECORD registry. Treatment of patients with acute coronary syndromes in hospitals with and without possibilities to perform invasive coronary procedures. Kardiologiia 2010, 50(7), 8–14. [Google Scholar]
- Bradley, EH; Nallamothu, BK; Herrin, J; Ting, HH; Stern, AF; Nembhard, IM; et al. National efforts to improve door-to-balloon time results from the door-to-balloon alliance. J Am Coll Cardiol 2009, 54, 2423–9. [Google Scholar] [CrossRef] [PubMed]
- Schamroth, C; ACCESS South Africa investigators. Management of acute coronary syndrome in South Africa: insights from the ACCESS (Acute Coronary Events—a Multinational Survey of Current Management Strategies) registry. Cardiovasc J Afr 2012, 23, 365–70. [Google Scholar] [CrossRef] [PubMed]
- Alhabib, KF; Sulaiman, K; Al-Motarreb, A; Almahmeed, W; Asaad, N; Amin, H; et al. Baseline characteristics, management practices, and long-term outcomes of Middle Eastern patients in the Second Gulf Registry of Acute Coronary Events (Gulf RACE-2). Ann Saudi Med 2012, 32(1), 9–18. [Google Scholar] [CrossRef] [PubMed]
- Srimahachota, S; Boonyaratavej, S; Kanjanavanit, R; Sritara, P; Krittayaphong, R; Kunjara-Naayudhya, R; et al. Thai Registry in Acute Coronary Syndrome (TRACS)—an extension of Thai Acute Coronary Syndrome registry (TACS) group: lower in-hospital but still high mortality at one-year. J Med Assoc Thai 2012, 95(4), 508–18. [Google Scholar]
- Mandelzweig, L; Battler, A; Boyko, V; Bueno, H; Danchin, N; Filippatos, G; et al. The second Euro Heart Survey on acute coronary syndromes: characteristics, treatment, and outcome of patients with ACS in Europe and the Mediterranean Basin in 2004. Eur Heart J 2006, 27(19), 2285–93. [Google Scholar] [CrossRef] [PubMed]
| Variable | Study years | P for trend | |||
|---|---|---|---|---|---|
| 2012 | 2013 | 2014 | 2015 | ||
| Gender, n (%) | |||||
| Male | 3684 (72.2) | 4201 (71.8) | 4391 (72.5) | 3734 (72.3) | >0.05 |
| Female | 1420 (27.8) | 1651 (28.2) | 1666 (27.5) | 1429 (27.7) | |
| Age, years | |||||
| ≤60 | 2495 (48.9) | 2735 (46.7) | 2904 (47.9) | 2494 (48.3) | >0.05 |
| >60 | 2608 (51.1) | 3117 (53.3) | 3153 (52.1) | 2669 (51.7) | |
| Living location | |||||
| Urban | 4037 (79.1) | 4451 (76.1) | 4431 (73.2) | 3763 (72.9) | 0.04 |
| Rural | 1067 (20.9) | 1401 (23.9) | 1626 (26.8) | 1400 (27.1) | |
| Time from hospitalization to PCI, min | |||||
| Mean ± SD | 2747.7 ± 5793.9 | 1975.4 ± 4793.8 | 1832.4 ± 4729.9 | 1874.7 ± 4759.2 | >0.05 |
| Median [IQR] | 155.0 [1755.0] | 90.0 [955.0] | 85.0 [730.0] | 73.5 [712.8] | 0.1 |
| Time from hospitalization to PCI, % | |||||
| 0–59 min | 30.5 | 40.0 | 41.2 | 44.1 | 0.09 |
| ≥60 min | 69.5 | 60.0 | 58.8 | 55.9 | |
| Bed-days | |||||
| Mean ± SD | 12.1 ± 5.2 | 11.2 ± 5.2 | 11.6 ± 5.9 | 12.0 ± 6.3 | >0.05 |
| Median [IQR] | 12.0 [4.0] | 11.0 [4.0] | 11.0 [5.0] | 11.0 [6.0] | |
| Hospital mortality, % | 9.0 | 8.5 | 8.9 | 8.6 | >0.05 |
| Recurrent MI, % | 21.3 | 20.1 | 19.8 | 18.2 | 0.03 |
| IQR, interquartile range; PCI, percutaneous coronary intervention; MI, myocardial infarction. | |||||
| Year | Mean time from hospitalization to percutaneous coronary intervention, min | |||||
|---|---|---|---|---|---|---|
| Gender | Age | Living place | ||||
| Male | Female | ≤60 years | >60 years | Urban | Rural | |
| 2012 | 2755.3 | 2565.3 | 2581.6 | 2819.0 | 2515.7 | 3408.9 |
| 2013 | 2030.7 | 1859.9 | 1967.8 | 1995.4 | 1762.4 | 2681.8 |
| 2014 | 1850.7 | 1813.6 | 1783.8 | 1892.6 | 1686.9 | 2258.8 |
| 2015 | 2073.0 | 1668.6 | 1876.4 | 2040.2 | 1857.2 | 2240.1 |
| 2012–2015 | 2177.4 | 1976.8 | 2052.4 | 2186.8 | 1955.6 | 2647.4 |
| APC, % | −9.5 | −13.2 | −10.6 | −10.2 | −9.5 | −14.3 |
| P = 0.3 | P = 0.1 | P = 0.2 | P = 0.3 | P = 0.3 | P = 0.06 | |
| PCI, percutaneous coronary interventions; APC, annual percentage change. | ||||||
| Year | Mean number of bed-days | |||||
|---|---|---|---|---|---|---|
| Gender | Age | Living place | ||||
| Male | Female | ≤60 years | >60 years | Urban | Rural | |
| 2012 | 12.1 | 12.1 | 12.1 | 12.0 | 12.1 | 12.1 |
| 2013 | 11.3 | 11.0 | 11.3 | 11.1 | 11.2 | 11.3 |
| 2014 | 11.7 | 11.4 | 11.8 | 11.5 | 11.6 | 11.7 |
| 2015 | 12.3 | 11.7 | 12.2 | 12.1 | 12.0 | 12.3 |
| 2012–2015 | 11.8 | 11.5 | 11.9 | 11.7 | 11.7 | 11.9 |
| APC, % | +0.8 | −0.7 | +0.7 | +0.6 | +0.2 | +0.9 |
| P = 0.7 | P = 0.8 | P = 0.7 | P = 0.8 | P = 0.9 | P = 0.7 | |
| PCI, percutaneous coronary intervention; APC, annual percentage change. | ||||||
| Variable | Odds ratio (95% CI) | P |
|---|---|---|
| Study years | ||
| 2012 | 1 | |
| 2013 | 0.622 (0.520–0.744) | 0.0001 |
| 2014 | 0.670 (0.561–0.801) | 0.0001 |
| 2015 | 0.676 (0.561–0.814) | 0.0001 |
| Gender | ||
| Male | 1 | |
| Female | 1.464 (1.280–1.675) | 0.0001 |
| Age, years | ||
| ≤60 | 1 | |
| >60 | 2.738 (2.381–3.149) | 0.0001 |
| Living location | ||
| Urban | 1 | |
| Rural | 0.934 (0.805–1.083) | 0.365 |
| Time from hospitalization to PCI, min | ||
| 0–59 | 1 | |
| 60> | 1.232 (1.085–1.400) | 0.001 |
| Bed-days | 0.621 (0.611–0.632) | 0.0001 |
| PCI, percutaneous coronary intervention. Model entered: study year, gender, age, living location, time from hospitalization to PCI, number of bed-days, R2 = 0.52 (Nagelkerke). | ||
© 2017 The Lithuanian University of Health Sciences. Production and hosting by Elsevier Sp. z o.o. This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0/).
Share and Cite
Akimbaeva, Z.; Ismailov, Z.; Akanov, A.A.; Radišauskas, R.; Padaiga, Ž. Assessment of coronary care management and hospital mortality from ST-segment elevation myocardial infarction in the Kazakhstan population: Data from 2012 to 2015. Medicina 2017, 53, 58-65. https://doi.org/10.1016/j.medici.2017.01.006
Akimbaeva Z, Ismailov Z, Akanov AA, Radišauskas R, Padaiga Ž. Assessment of coronary care management and hospital mortality from ST-segment elevation myocardial infarction in the Kazakhstan population: Data from 2012 to 2015. Medicina. 2017; 53(1):58-65. https://doi.org/10.1016/j.medici.2017.01.006
Chicago/Turabian StyleAkimbaeva, Zhanar, Zhumagali Ismailov, Aikan A. Akanov, Ričardas Radišauskas, and Žilvinas Padaiga. 2017. "Assessment of coronary care management and hospital mortality from ST-segment elevation myocardial infarction in the Kazakhstan population: Data from 2012 to 2015" Medicina 53, no. 1: 58-65. https://doi.org/10.1016/j.medici.2017.01.006
APA StyleAkimbaeva, Z., Ismailov, Z., Akanov, A. A., Radišauskas, R., & Padaiga, Ž. (2017). Assessment of coronary care management and hospital mortality from ST-segment elevation myocardial infarction in the Kazakhstan population: Data from 2012 to 2015. Medicina, 53(1), 58-65. https://doi.org/10.1016/j.medici.2017.01.006




