How the changes in the system affect trauma care provision: The assessment of and implications for Lithuanian trauma service performance in 2007–2012
Abstract
1. Introduction
2. Materials and methods
3. Results
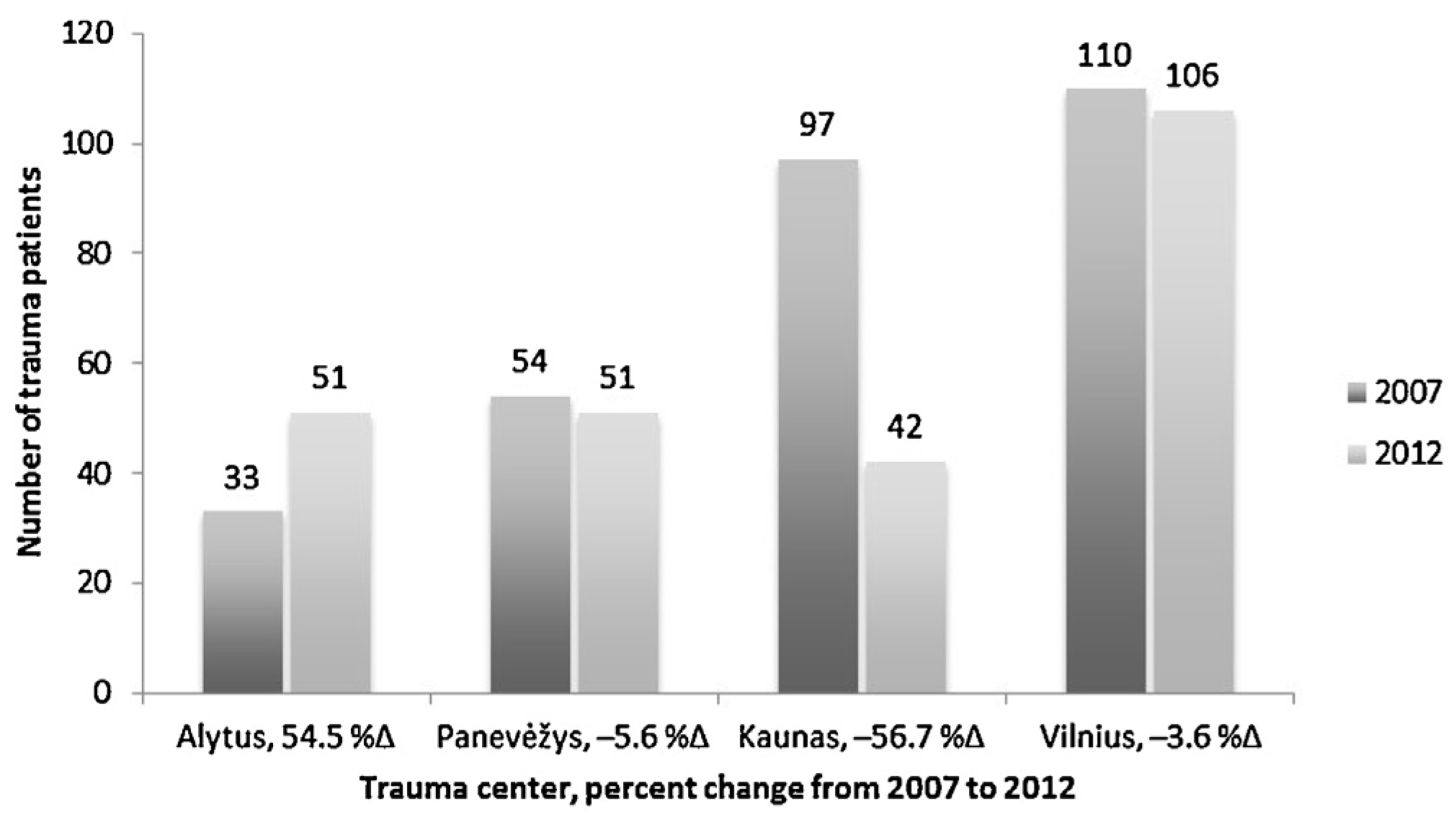
3.1. Study sample
3.2. Pre-hospital care
3.3. Survey
3.4. Reception and resuscitation in the emergency department
4. Discussion
4.1. Implications to the practice
5. Conclusions
Conflicts of interest
Sources of funding
Authors’ contribution
R E F E R E N C E S
- Haagsma, JA; Graetz, N; Bolliger, I; Naghavi, M; Higashi, H; Mullany, EC; et al. The global burden of injury: incidence, mortality, disability-adjusted life years and time trends from the Global Burden of Disease study 2013. Inj Prev 2015. [Epub ahead of print]. [Google Scholar] [CrossRef] [PubMed]
- Latifi, R; Ziemba, M; Leppaniemi, A; Dasho, E; Dogjani, A; Shatri, Z; et al. Trauma system evaluation in developing countries: applicability of American College of Surgeons/Committee on Trauma (ACS/COT) Basic Criteria. Anaesthesia 2013, 68 (Suppl. 1), 30–9. [Google Scholar] [CrossRef] [PubMed]
- Lunevicius, R; Stevens, KA; Puvanachandra, P; Hyder, AA. The epidemiology of injury in the Republic of Lithuania. Scand J Public Health 2010, 38, 386–94. [Google Scholar] [CrossRef] [PubMed]
- Lunevicius, R; Rahman, MH. Assessment of Lithuanian trauma care service using a conceptual framework for assessing the performance of health system. Eur J Public Health 2012, 22, 26–31. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Lunevicius, R. Injury as a principal Lithuanian public health problem and its modus of solution. Lietuvos chirurgija (Lithuanian Surgery) 2009, 7, 6–11. [Google Scholar]
- Lunevicius, R; Herbert, HK; Hyder, AA. The epidemiology of road traffic injuries in the Republic of Lithuania, 1998–2007. Eur J Public Health 2010, 20, 702–6. [Google Scholar] [CrossRef] [PubMed]
- ACSCOT-PHTLS. Trauma systems: the right patient in the right time to the right place, 4th ed.; Mosby: St. Louis, 1999; [chapter 16]. [Google Scholar]
- Committee on Trauma. Resources for optimal care of the injured patient; American College of Surgeons: Chicago, IL, 2006. [Google Scholar]
- MacKenzie, EJ; Rivara, FP; Jurkovich, GJ; Nathens, AB; Frey, KP; Egleston, BL; et al. A national evaluation of the effect trauma-centre care on mortality. N Engl J Med 2006, 354, 366–78. [Google Scholar] [CrossRef] [PubMed]
- Lansink, KW; Leenen, LP. Do designed trauma systems improve outcome? Curr Opin Crit Care 2007, 13, 686–90. [Google Scholar] [CrossRef] [PubMed]
- Cameron, PA; Gabbe, B; Cooper, DJ. A statewide system of trauma care in Victoria: effect on patient survival. Med J Aust 2008, 189, 546–50. [Google Scholar] [PubMed]
- Gabbe, BJ; Simpson, PM; Sutherland, AM; Wolfe, R; Fitzgerald, MC; Judson, R; et al. Improved functional outcomes for major trauma patients in a regionalized, inclusive trauma system. Ann Surg 2012, 255, 1009–15. [Google Scholar] [CrossRef] [PubMed]
- National Trauma Prevention Program 2000–2010. Valstybės žinios, 2000-04-19, No. 32-903. http://www3.lrs.lt/pls/. Accessed 19 May 2009 [in Lithuanian].
- Pundzius, J; Žekas, R; Večkienė, I (Eds.) Lithuanian National Health Board Annual Report 2007. Health and safety: outbreaks and crises. UAB ‘Baltijos kopija’: Vilnius, Lithuania, 2008; pp. 117–48. http://www3.lrs.lt/pls/inter/. Accessed 19 May 2009.
- Creation of organizational system for patients who sustained traumatic injuries from external causes in Lithuania. Human Resources Development Priority 4 ‘Strengthening of administrating capacities and efficiency of public administration, implementation of the measure VP 1-4.3-VRM-0.2-V ‘Public policies promoting reform’. SFMIS number VP 1-4.3-VRM-0.2-V-05-013 [Skubios pagalbos nukentėjusiesiems nuo traumų ir kitų išorinių mirties priežasčių teikimo Lietuvoje organizacinės sistemos sukūrimas. Vykdomas pagal Žmogiškųjų išteklių plėtros veiksmų programos 4 prioriteto ‘Administracinių gebėjimų stiprinimas ir viešojo administravimo efektyvumo didinimas’ įgyvendinimo priemonę VP 1-4.3-VRM-0.2-V ‘Viešųjų politikų reformų skatinimas’. SFMIS mumeris VP 1-4.3–VRM-0.2-V-05-013. Projektas finansuojamas Europos Sąjungos struktūrinių fondų ir Lietuvos Respublikos valstybės biudžeto lėšomis]. http://www.essc.sam.lt/download/961/projektas_tinklalapiui_2.pdf [accessed 06.12.15].
- The evaluation of the effect of measures, administered by the Ministry of Health of the Republic of Lithuania on the golden hour. Project code: No. VP 3-4.2-FM-02-V-06-001 [Lietuvos Respublikos Sveikatos apsaugos ministerijos administruojamų priemonių poveikio ‘Auksinei valandai’ vertinimas (Galutinė vertinimo ataskaita)]. http://www.esinvesticijos.lt/uploads/documents/files/Vertinimodokumentai/Auksinesvalandosgalutinevertinimoataskaita 201502174.docx [accessed 20.12.15].
- Projekto “Traumų ir nelaimingų atsitikimų stebėsenos sistemos sukūrimas”, vykdomo pagal 2007–2013m. Žmogiškųjų išteklių plėtros veiksmų programos 4 prioriteto “Administracinių gebėjimų stiprinimas ir viešojo administravimo efektyvumo didinimas į gyvendinimo priemonę VP 1-4.3-VRM-02-V” Viešųjų politikų reformų skatinimas, 1.2.2 veiklos ‘Užsienio šalių gerosios patirties traumų ir nelaimingų atsitikimų stebėsenos srityje analizė’. http://www.hi.lt/uploads/pdf/projektai/Traumu/Veiklos%201_2_2%20ataskaita.pdf [accessed 06.12.15].
- Galimybių studijos ir gairių traumų registrui sukūrimas remiantis gerąja Norvegijos kolegų patirtimi. Bendras VU Vaikų ligoninės ir Norvegijos partnerių projektas; 2010. http://www.vaikuligonine.lt/naujienos_pilnos.php?nid=246 [accessed 06.12.15].
- Marozas, R; Rimdeika, R; Jasinskas, N; Vaitkaitiene, E; Vaitkaitis, D. The ability of Lithuanian ambulance services to provide first medical aid in trauma cases. Medicina (Kaunas) 2007, 43, 463–71. [Google Scholar] [PubMed]
- Champion, HR; Sacco, WJ; Copes, WS; Gann, DS; Gennarelli, TA; Flanagan, ME. A revision of the Trauma Score. J Trauma 1989, 29, 623–9. [Google Scholar] [CrossRef] [PubMed]
- Walz, B. Introduction to EMS systems; Delmar, Inc. Thomson Learning™: USA, 2002. [Google Scholar]
- Pamerneckas, A; Macas, A; Blazgys, A; Pilipavicius, G; Toliusis, V. The treatment of multiple injuries: prehospital emergency aid. Medicina (Kaunas) 2006, 42(5), 395–400. [Google Scholar] [PubMed]
- Zikos, D; Diomidous, M; Mpletsa, V. The effect of an electronic documentation system on the trauma patient’s length of stay in an emergency department. J Emerg Nurs 2014, 40, 469–75. [Google Scholar] [CrossRef] [PubMed]
- WHO. Violence and injury prevention. Trauma system maturity index. http://www.who.int/violence_injury_prevention/services/traumacare/maturity_index/en/ [accessed 12.12.15].
- National Peer Review Programme. http://www.nationalpeerreview.nhs.uk [accessed 12.12.15].
- Stelfox, HT; Straus, S; Nathens, A; Bobranska-Artiuch, B. Evidence for quality indicators to evaluate adult trauma care: a systematic review. Crit Care Med 2011, 39, 846–59. [Google Scholar]
- NHS England. National Peer Review Programme. National Peer Review Programme: Major Trauma Measures. Trauma specific measures. Updated by Hill J. November 2014. [Google Scholar]
- Jones, C; Shepherd, S; NHS. Major trauma operational delivery networks. Sample Template Annual Report. October 2014; [Document MTN-AR-01-10-14]. [Google Scholar]
- Jones, C; Shepherd, S; NHS. Major trauma operational delivery networks. National Peer Review Programme: Major Trauma Measures – Matrix. October 2014; [Document MTN-PRM-04-10-14]. [Google Scholar]
- Pamerneckas, A; Adukauskiene, D; Macas, A. Multiple trauma: evaluation of patient’s condition and local injuries by trauma classification systems. Medicina (Kaunas) 2002, 38, 685–694. [Google Scholar] [PubMed]
- The methodology on how to organize trauma care provision for patients with injuries from external causes [Vieninga metodika sveikatos priežiūros įstaigoms, kaip organizuoti pagalbą nukentėjusiems nuo traumų ir kitų išorinių mirties priežasčių atvejais]. Edited: Aušra Rimkutė. UAB ‘Tarptautinė skubiosios medicinos akademija. Sveikatos apsaugos ministerijos Ekstremalių sveikatai situacijų centras; 2014. http://www.essc.sam.lt/lt/vieninga_metodika.html [accessed 20.12.15].
| 1 | |
| 2 |

| Procedure | 2007 | 2012 | χ2 | P value |
|---|---|---|---|---|
| Cervical spine protection by collar Oxygen therapy Airway management Temporal control of external bleeding Pelvic binders and splints Intravenous fluids Pain relief | 90 (30.6) 5 (1.7) 30 (10.2) 37 (12.6) 114 (38.8) 78 (26.5) 99 (33.7) | 90 (36) 16 (6.4) 23 (9.2) 19 (7.6) 95 (38) 89 (35.6) 114 (45.6) | 1.771 8.04 0.155 3.636 0.034 5.224 8.067 | 0.183 0.005* 0.694 0.565 0.853 0.022* 0.005* |
| Values are number (percentage). * Statistically significant. | ||||
| Measures | 2007 | 2012 | P value |
|---|---|---|---|
| Time to ultrasound-scanning Time to laboratory tests Time to radiography Time to CT-scanning Time to key decision making | 54.03 ± 64.29 113.58 ± 242.93 39.84 ± 35.09 88.82 ± 131.04 118.0 ± 104.21 | 23.32 ± 26.32 100.34 ± 196.18 34.66 ± 26.56 63.97 ± 81.26 101.27 ± 82.72 | <0.0001* 0.737 0.526 0.634 0.039* |
| Values are mean (standard deviation). * Statistically significant. | |||
© 2017 The Lithuanian University of Health Sciences. Production and hosting by Elsevier Sp. z o.o. This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0/).
Share and Cite
Dambrauskas, Ž.; Aukštakalnis, V.; Karbonskienė, A.; Kačiurinas, D.; Vokietienė, J.; Lapka, R.; Pamerneckas, A.; Porvaneckas, N.; Stašaitis, K.; Jasinskas, N.; et al. How the changes in the system affect trauma care provision: The assessment of and implications for Lithuanian trauma service performance in 2007–2012. Medicina 2017, 53, 50-57. https://doi.org/10.1016/j.medici.2016.12.002
Dambrauskas Ž, Aukštakalnis V, Karbonskienė A, Kačiurinas D, Vokietienė J, Lapka R, Pamerneckas A, Porvaneckas N, Stašaitis K, Jasinskas N, et al. How the changes in the system affect trauma care provision: The assessment of and implications for Lithuanian trauma service performance in 2007–2012. Medicina. 2017; 53(1):50-57. https://doi.org/10.1016/j.medici.2016.12.002
Chicago/Turabian StyleDambrauskas, Žilvinas, Vytautas Aukštakalnis, Aurika Karbonskienė, Dmitrijus Kačiurinas, Jolanta Vokietienė, Robertas Lapka, Algimantas Pamerneckas, Narūnas Porvaneckas, Kęstutis Stašaitis, Nedas Jasinskas, and et al. 2017. "How the changes in the system affect trauma care provision: The assessment of and implications for Lithuanian trauma service performance in 2007–2012" Medicina 53, no. 1: 50-57. https://doi.org/10.1016/j.medici.2016.12.002
APA StyleDambrauskas, Ž., Aukštakalnis, V., Karbonskienė, A., Kačiurinas, D., Vokietienė, J., Lapka, R., Pamerneckas, A., Porvaneckas, N., Stašaitis, K., Jasinskas, N., Dobožinskas, P., Vaitkaitis, D., & Lunevičius, R. (2017). How the changes in the system affect trauma care provision: The assessment of and implications for Lithuanian trauma service performance in 2007–2012. Medicina, 53(1), 50-57. https://doi.org/10.1016/j.medici.2016.12.002




