The Predictive Value of Serum ACE2 and TMPRSS2 Concentrations in Patients with COVID-19—A Prospective Pilot Study
Abstract
:1. Introduction
2. Methods
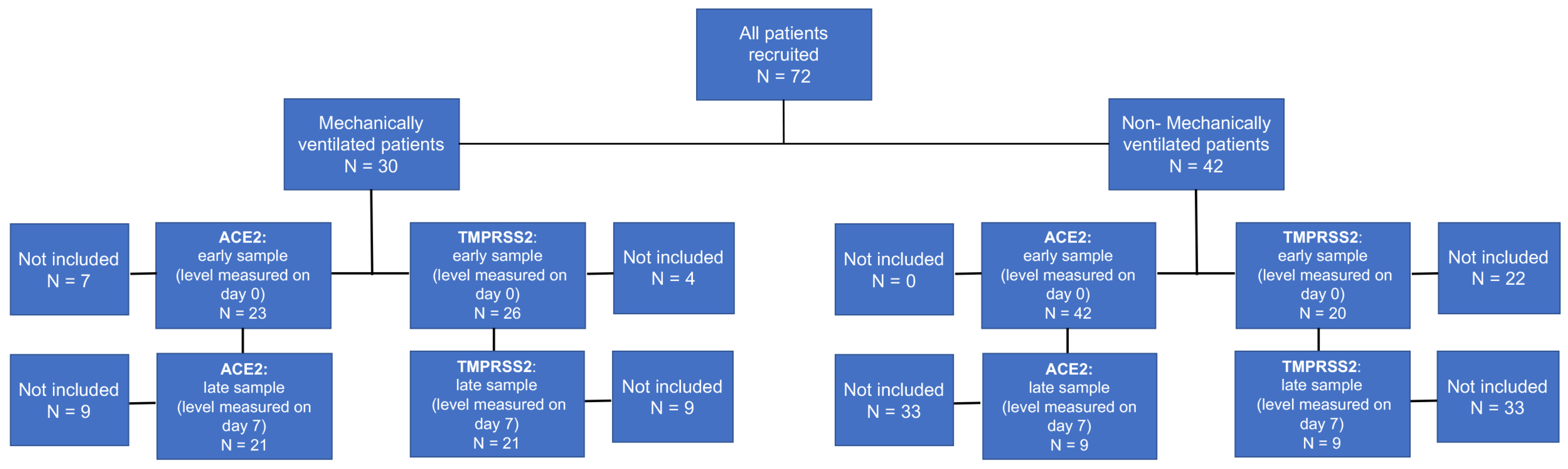
2.1. Patient Enrollment
2.2. Sample Collection and Handling
2.3. Data Collection
2.4. Outcomes
2.5. Statistical Analysis
3. Results
3.1. Patient Characteristics
3.2. Increased Circulatory ACE2 Levels in COVID-19 Patients at Early Disease Stages Correlate with an Increased Risk for Intubation and Mechanical Ventilation
3.3. Elevated Early Sample ACE2 Expression Is Significantly Associated with Biomarkers for Severe Disease Course in COVID-19 Patients
3.4. Increased Circulatory TMPRSS2 Levels in COVID-19 Patients at Admission Do Not Significantly Correlate the Risk for Intubation and Mechanical Ventilation
3.5. ACE2/TMPRSS2 Ratio Is Not Significantly Associated with the Risk for Intubation and Mechanical Ventilation
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Wynants, L.; Van Calster, B.; Collins, G.S.; Riley, R.D.; Heinze, G.; Schuit, E.; Bonten, M.M.J.; Dahly, D.L.; Damen, J.A.; Debray, T.P.A.; et al. Prediction models for diagnosis and prognosis of COVID-19: Systematic review and critical appraisal. BMJ 2020, 369, m1328. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tjendra, Y.; Al Mana, A.F.; Espejo, A.P.; Akgun, Y.; Millan, N.C.; Gomez-Fernandez, C.; Cray, C. Predicting Disease Severity and Outcome in COVID-19 Patients: A Review of Multiple Biomarkers. Arch. Pathol. Lab. Med. 2020, 144, 1465–1474. [Google Scholar] [CrossRef] [PubMed]
- Marin, B.G.; Aghagoli, G.; Lavine, K.; Yang, L.; Siff, E.J.; Chiang, S.S.; Salazar-Mather, T.P.; Dumenco, L.; Savaria, M.C.; Aung, S.N.; et al. Predictors of COVID-19 severity: A literature review. Rev. Med. Virol. 2021, 31, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Malik, P.; Patel, U.; Mehta, D.; Patel, N.; Kelkar, R.; Akrmah, M.; Gabrilove, J.L.; Sacks, H. Biomarkers and outcomes of COVID-19 hospitalisations: Systematic review and meta-analysis. BMJ Evid. Based Med. 2021, 26, 107–108. [Google Scholar] [CrossRef] [PubMed]
- Aloisio, E.; Chibireva, M.; Serafini, L.; Pasqualetti, S.; Falvella, F.S.; Dolci, A.; Panteghini, M. A Comprehensive Appraisal of Laboratory Biochemistry Tests as Major Predictors of COVID-19 Severity. Arch. Pathol. Lab. Med. 2020, 144, 1457–1464. [Google Scholar] [CrossRef]
- Alamin, A.A.; Yahia, A.I.O. Hematological Parameters Predict Disease Severity and Progression in Patients with COVID-19: A Review Article. Clin. Lab. 2021, 67, 9–13. [Google Scholar] [CrossRef]
- Bottcher, E.; Matrosovich, T.; Beyerle, M.; Klenk, H.-D.; Garten, W.; Matrosovich, M. Proteolytic activation of influenza viruses by serine proteases TMPRSS2 and HAT from human airway epithelium. J. Virol. 2006, 80, 9896–9898. [Google Scholar] [CrossRef] [Green Version]
- Chaipan, C.; Kobasa, D.; Bertram, S.; Glowacka, I.; Steffen, I.; Tsegaye, T.S.; Takeda, M.; Bugge, T.H.; Kim, S.; Park, Y.; et al. Proteolytic activation of the 1918 influenza virus hemagglutinin. J. Virol. 2009, 83, 3200–3211. [Google Scholar] [CrossRef] [Green Version]
- Hatesuer, B.; Bertram, S.; Mehnert, N.; Bahgat, M.M.; Nelson, P.S.; Pöhlman, S.; Schughart, K. Tmprss2 is essential for influenza H1N1 virus pathogenesis in mice. PLoS Pathog. 2013, 9, e1003774. [Google Scholar] [CrossRef] [Green Version]
- Abe, M.; Tahara, M.; Sakai, K.; Yamaguchi, H.; Kanou, K.; Shirato, K.; Kawase, M.; Noda, M.; Kimura, H.; Matsuyama, S.; et al. TMPRSS2 is an activating protease for respiratory parainfluenza viruses. J. Virol. 2013, 87, 11930–11935. [Google Scholar] [CrossRef] [Green Version]
- Wettstein, L.; Kirchhoff, F.; Münch, J. The Transmembrane Protease TMPRSS2 as a Therapeutic Target for COVID-19 Treatment. Int. J. Mol. Sci. 2022, 23, 1351. [Google Scholar] [CrossRef] [PubMed]
- Hoffmann, M.; Kleine-Weber, H.; Pohlmann, S. A Multibasic Cleavage Site in the Spike Protein of SARS-CoV-2 Is Essential for Infection of Human Lung Cells. Mol. Cell 2020, 78, 779–784.e5. [Google Scholar] [CrossRef] [PubMed]
- Hoffmann, M.; Schroeder, S.; Kleine-Weber, H.; Müller, M.A.; Drosten, C.; Pöhlmann, S. Nafamostat Mesylate Blocks Activation of SARS-CoV-2: New Treatment Option for COVID-19. Antimicrob. Agents Chemother. 2020, 64, e00754-20. [Google Scholar] [CrossRef] [Green Version]
- Matsuyama, S.; Nao, N.; Shirato, K.; Takeda, M. Enhanced isolation of SARS-CoV-2 by TMPRSS2-expressing cells. Proc. Natl. Acad. Sci. USA 2020, 117, 7001–7003. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hamming, I.; Timens, W.; Bulthuis, M.L.C.; Lely, A.T.; Navis, G.J.; van Goor, H. Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus. A first step in understanding SARS pathogenesis. J. Pathol. 2004, 203, 631–637. [Google Scholar] [CrossRef] [PubMed]
- Sward, P.; Edsfeldt, A.; Reepalu, A.; Jehpsson, L.; Rosengren, B.E.; Karlsson, M.K. Age and sex differences in soluble ACE2 may give insights for COVID-19. Crit. Care 2020, 24, 221. [Google Scholar] [CrossRef] [PubMed]
- Sama, I.; Ravera, A.; Santema, B.T.; Van Goor, H.; Ter Maaten, J.M.; Cleland, J.G.F.; Rienstra, M.; Friedrich, A.W.; Samani, N.J.; Ng, L.L.; et al. Circulating plasma concentrations of angiotensin-converting enzyme 2 in men and women with heart failure and effects of renin-angiotensin-aldosterone inhibitors. Eur. Heart J. 2020, 41, 1810–1817. [Google Scholar] [CrossRef]
- Kornilov, S.A.; Lucas, I.; Jade, K.; Dai, C.; Lovejoy, J.C.; Magis, A. Plasma levels of soluble ACE2are associated with sex, Metabolic Syndrome, and its biomarkers in a large cohort, pointing to a possible mechanism for increased severity in COVID-19. Crit. Care 2020, 24, 452. [Google Scholar] [CrossRef]
- Ramchand, J.; Patel, S.K.; Srivastava, P.M.; Farouque, O.; Burrell, L.M. Elevated plasma angiotensin converting enzyme 2 activity is an independent predictor of major adverse cardiac events in patients with obstructive coronary artery disease. PLoS ONE 2018, 13, e0198144. [Google Scholar] [CrossRef]
- Ramchand, J.; Burrell, L.M. Circulating ACE2: A novel biomarker of cardiovascular risk. Lancet 2020, 396, 937–939. [Google Scholar] [CrossRef]
- Ramchand, J.; Patel, S.K.; Kearney, L.G.; Matalanis, G.; Farouque, O.; Srivastava, P.M.; Burrell, L.M. Plasma ACE2 Activity Predicts Mortality in Aortic Stenosis and Is Associated With Severe Myocardial Fibrosis. JACC Cardiovasc. Imaging 2020, 13, 655–664. [Google Scholar] [CrossRef]
- Yang, X.H.; Deng, W.; Tong, Z.; Liu, Y.X.; Zhang, L.F.; Zhu, H.; Gao, H.; Huang, L.; Liu, Y.L.; Ma, C.M.; et al. Mice transgenic for human angiotensin-converting enzyme 2 provide a model for SARS coronavirus infection. Comp. Med. 2007, 57, 450–459. [Google Scholar] [PubMed]
- Zang, R.; Castro, M.F.G.; McCune, B.T.; Zeng, Q.; Rothlauf, P.W.; Sonnek, N.M.; Liu, Z.; Brulois, K.F.; Wang, X.; Greenberg, H.B. TMPRSS2 and TMPRSS4 promote SARS-CoV-2 infection of human small intestinal enterocytes. Sci. Immunol. 2020, 5, eabc3582. [Google Scholar] [CrossRef] [PubMed]
- Hoffmann, M.; Kleine-Weber, H.; Schroeder, S.; Krüger, N.; Herrler, T.; Erichsen, S.; Schiergens, T.S.; Herrler, G.; Wu, N.H.; Nitsche, A.; et al. SARS-CoV-2 Cell Entry Depends on ACE2 and TMPRSS2 and Is Blocked by a Clinically Proven Protease Inhibitor. Cell 2020, 181, 271–280.e8. [Google Scholar] [CrossRef] [PubMed]
- Bilan, N.; Dastranji, A.; Behbahani, A.G. Comparison of the spo2/fio2 ratio and the pao2/fio2 ratio in patients with acute lung injury or acute respiratory distress syndrome. J. Cardiovasc. Thorac. Res. 2015, 7, 28–31. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rice, T.W.; Wheeler, A.P.; Bernard, G.R.; Hayden, D.L.; Schoenfeld, D.A.; Ware, L.B. Comparison of the SpO2/FIO2 ratio and the PaO2/FIO2 ratio in patients with acute lung injury or ARDS. Chest 2007, 132, 410–417. [Google Scholar] [CrossRef] [PubMed]
- Pisano, A.; Yavorovskiy, A.; Verniero, L.; Landoni, G. Indications for Tracheal Intubation in Patients with Coronavirus Disease 2019 (COVID-19). J. Cardiothorac. Vasc. Anesth. 2021, 35, 1276–1280. [Google Scholar] [CrossRef]
- Khwaja, A. KDIGO clinical practice guidelines for acute kidney injury. Nephron Clin. Pract. 2012, 120, c179–c184. [Google Scholar] [CrossRef]
- Reddy, R.; Asante, I.; Liu, S.; Parikh, P.; Liebler, J.; Borok, Z.; Rodgers, K.; Baydur, A.; Louie, S.G. Circulating angiotensin peptides levels in Acute Respiratory Distress Syndrome correlate with clinical outcomes: A pilot study. PLoS ONE 2019, 14, e0213096. [Google Scholar] [CrossRef]
- Henry, B.M.; Benoit, J.L.; Berger, B.A.; Pulvino, C.; Lavie, C.J.; Lippi, G.; Benoit, S.W. Coronavirus disease 2019 is associated with low circulating plasma levels of angiotensin 1 and angiotensin 1,7. J. Med. Virol. 2021, 93, 678–680. [Google Scholar] [CrossRef]
- Kragstrup, T.W.; Singh, H.S.; Grundberg, I.; Nielsen, A.L.-L.; Rivellese, F.; Mehta, A.; Goldberg, M.B.; Filbin, M.R.; Qvist, P.; Bibby, B.M. Plasma ACE2 predicts outcome of COVID-19 in hospitalized patients. PLoS ONE 2021, 16, e0252799. [Google Scholar] [CrossRef]
- Reindl-Schwaighofer, R.; Hödlmoser, S.; Eskandary, F.; Poglitsch, M.; Bonderman, D.; Strassl, R.; Aberle, J.H.; Oberbauer, R.; Zoufaly, A.; Hecking, M. ACE2 Elevation in Severe COVID-19. Am. J. Respir. Crit. Care Med. 2021, 203, 1191–1196. [Google Scholar] [CrossRef] [PubMed]
- Patel, S.K.; Juno, J.A.; Lee, W.S.; Wragg, K.M.; Hogarth, P.M.; Kent, S.J.; Burrell, L.M. Plasma ACE2 activity is persistently elevated following SARS-CoV-2 infection: Implications for COVID-19 pathogenesis and consequences. Eur. Respir. J. 2021, 57, 2003730. [Google Scholar] [CrossRef] [PubMed]
- Fagyas, M.; Fejes, Z.; Sütő, R.; Nagy, Z.; Székely, B.; Pócsi, M.; Ivády, G.; Bíró, E.; Bekő, G.; Nagy, A.; et al. Circulating ACE2 activity predicts mortality and disease severity in hospitalized COVID-19 patients. Int. J. Infect. Dis. 2021, 115, 8–16. [Google Scholar] [CrossRef] [PubMed]
- Rieder, M.; Wirth, L.; Pollmeier, L.; Jeserich, M.; Goller, I.; Baldus, N.; Schmid, B.; Busch, H.-J.; Hofmann, M.; Kern, W.; et al. Serum ACE2, Angiotensin II, and Aldosterone Levels Are Unchanged in Patients With COVID-19. Am. J. Hypertens. 2021, 34, 278–281. [Google Scholar] [CrossRef] [PubMed]
- Kolberg, E.S.; Wickstrøm, K.; Tonby, K.; Dyrhol-Riise, A.M.; Holten, A.R.; Amundsen, E.K. Serum ACE as a prognostic biomarker in COVID-19: A case series. APMIS 2021, 129, 237–238. [Google Scholar] [CrossRef]
- Imai, Y.; Kuba, K.; Rao, S.; Huan, Y.; Guo, F.; Guan, B.; Yang, P.; Sarao, R.; Wada, T.; Leong-Poi, H.; et al. Angiotensin-converting enzyme 2 protects from severe acute lung failure. Nature 2005, 436, 112–116. [Google Scholar] [CrossRef]
- Zoufaly, A.; Poglitsch, M.; Aberle, J.H.; Hoepler, W.; Seitz, T.; Traugott, M.; Grieb, A.; Pawelka, E.; Laferl, H.; Wenisch, C.; et al. Human recombinant soluble ACE2 in severe COVID-19. Lancet Respir. Med. 2020, 8, 1154–1158. [Google Scholar] [CrossRef]
- Narula, S.; Yusuf, S.; Chong, M.; Ramasundarahettige, C.; Rangarajan, S.; Bangdiwala, I.S.; van Eikels, M.; Leineweber, K.; Wu, A.; Pigeyre, M.; et al. Plasma ACE2 and risk of death or cardiometabolic diseases: A case-cohort analysis. Lancet 2020, 396, 968–976. [Google Scholar] [CrossRef]
- Emilsson, V.; Gudmundsson, E.F.; Aspelund, T.; Jonsson, B.G.; Gudjonsson, A.; Launer, L.J.; Lamb, J.R.; Gudmundsdottir, V.; Jennings, L.L.; Gudnason, V. Serum levels of ACE2 are higher in patients with obesity and diabetes. Obes. Sci. Pract. 2021, 7, 239–243. [Google Scholar] [CrossRef]
- Lei, Y.; Zhang, J.; Schiavon, C.R.; He, M.; Chen, L.; Shen, H.; Zhang, Y.; Yin, Q.; Cho, Y.; Andrade, L.; et al. SARS-CoV-2 Spike Protein Impairs Endothelial Function via Downregulation of ACE 2. Circ. Res. 2021, 128, 1323–1326. [Google Scholar] [CrossRef] [PubMed]
- Velavan, T.P.; Meyer, C.G. Mild versus severe COVID-19: Laboratory markers. Int. J. Infect. Dis. 2020, 95, 304–307. [Google Scholar] [CrossRef] [PubMed]
| Non-MV N = 42 | MV N = 30 | p Value | |
|---|---|---|---|
| Age * | 68.93 ± 13.90 | 58.67 ± 13.33 | 0.008 |
| Male | 30 (71.4%) | 23 (76.7%) | 0.619 |
| Weight * (N = 61) | 81.73 ± 16.92 | 86.03 ± 18.43 | 0.622 |
| Diabetes | 14 (33.3%) | 14 (46.7%) | 0.253 |
| HTN | 25 (59.5%) | 14 (46.7%) | 0.280 |
| Dyslipidemia | 13 (31.0%) | 14 (46.7%) | 0.175 |
| Lung disease ** | 3 (7.1%) | 2 (6.7%) | 0.938 |
| IHD | 9 (21.4%) | 3 (10.0%) | 0.200 |
| CRF | 8 (19.0%) | 0 (0.0%) | 0.011 |
| CVA | 2 (4.8%) | 1 (3.3%) | 0.765 |
| Anemia | 6 (14.3%) | 3 (10.0%) | 0.588 |
| Malignancy | 2 (4.8%) | 1 (3.3%) | 0.557 |
| ACE2-First Sample <7.8 ng/mL N = 42 | ACE2-First Sample >7.8 ng/mL N = 23 | p Value | |
|---|---|---|---|
| Mortality | 7 (16.7%) | 4 (17.4%) | 0.941 |
| Mechanical ventilation | 11 (26.2%) | 12 (52.2%) | 0.036 |
| Hospitalization > 7 days | 28 (66.7%) | 15 (65.2%) | 0.906 |
| Inotropic support | 10 (23.8%) | 12 (52.2%) | 0.021 |
| Acute renal failure * | 11 (26.2%) | 9 (39.1%) | 0.280 |
| RRT | 2 (4.8%) | 6 (26.1%) | 0.012 |
| ECMO | 4 (9.5%) | 3 (13%) | 0.662 |
| Blood products | 12 (28.6%) | 9 (39.1%) | 0.384 |
| DIC | 3 (7.1%) | 0 (0%) | 0.189 |
| PE/DVT | 2 (4.8%) | 4 (17.4%) | 0.093 |
| Bleeding | 6 (14.3%) | 9 (39.1%) | 0.023 |
| Pneumothorax | 1 (2.4%) | 1 (4.3%) | 0.661 |
| Sepsis | 12 (28.6%) | 10 (43.5%) | 0.225 |
| Variables | OR | 95% CI | p Value |
|---|---|---|---|
| ACE2 (above 7.8 vs. below 7.8) | 7.49 | 1.51–37.11 | 0.014 |
| Age | 0.89 | 0.83–0.95 | 0.001 |
| Sex (Female vs. Male) | 0.71 | 0.14–3.56 | 0.677 |
| Acute renal failure * | 17.68 | 3.13–99.86 | 0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kassif Lerner, R.; Stein Yeshurun, M.; Hemi, R.; Zada, N.; Asraf, K.; Doolman, R.; Benoit, S.W.; Santos de Oliveira, M.H.; Lippi, G.; Henry, B.M.; et al. The Predictive Value of Serum ACE2 and TMPRSS2 Concentrations in Patients with COVID-19—A Prospective Pilot Study. J. Pers. Med. 2022, 12, 622. https://doi.org/10.3390/jpm12040622
Kassif Lerner R, Stein Yeshurun M, Hemi R, Zada N, Asraf K, Doolman R, Benoit SW, Santos de Oliveira MH, Lippi G, Henry BM, et al. The Predictive Value of Serum ACE2 and TMPRSS2 Concentrations in Patients with COVID-19—A Prospective Pilot Study. Journal of Personalized Medicine. 2022; 12(4):622. https://doi.org/10.3390/jpm12040622
Chicago/Turabian StyleKassif Lerner, Reut, Michal Stein Yeshurun, Rina Hemi, Nahid Zada, Keren Asraf, Ram Doolman, Stefanie W. Benoit, Maria Helena Santos de Oliveira, Giuseppe Lippi, Brandon Michael Henry, and et al. 2022. "The Predictive Value of Serum ACE2 and TMPRSS2 Concentrations in Patients with COVID-19—A Prospective Pilot Study" Journal of Personalized Medicine 12, no. 4: 622. https://doi.org/10.3390/jpm12040622
APA StyleKassif Lerner, R., Stein Yeshurun, M., Hemi, R., Zada, N., Asraf, K., Doolman, R., Benoit, S. W., Santos de Oliveira, M. H., Lippi, G., Henry, B. M., Pessach, I. M., & Pode Shakked, N. (2022). The Predictive Value of Serum ACE2 and TMPRSS2 Concentrations in Patients with COVID-19—A Prospective Pilot Study. Journal of Personalized Medicine, 12(4), 622. https://doi.org/10.3390/jpm12040622








