Specific Features of Focal Cortical Dysplasia in Tuberous Sclerosis Complex
Abstract
1. Introduction
2. Structural Features of Cortical Tubers
3. Molecular Genetics
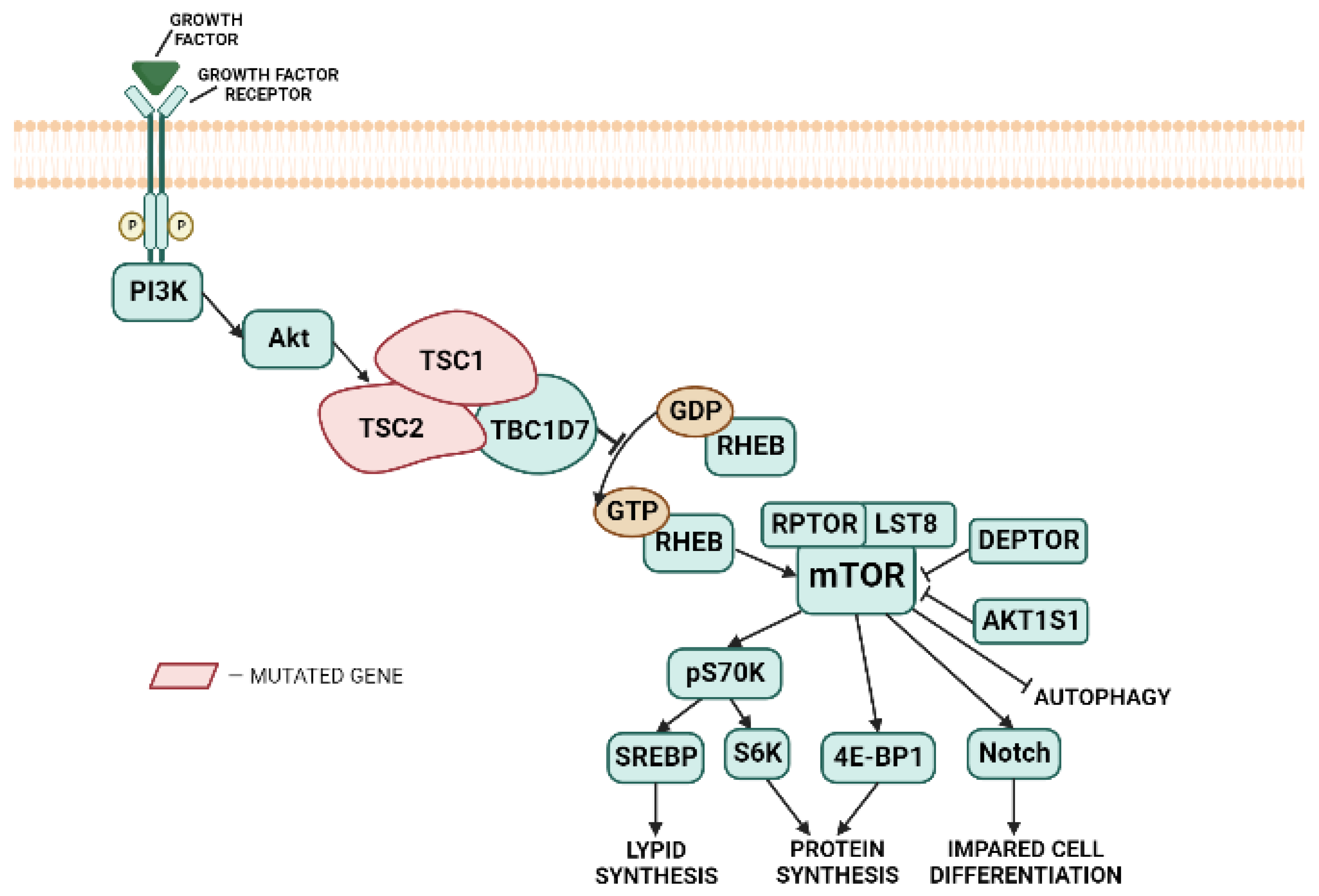
3.1. Impaired Inhibition of the mTOR Pathway by the TSC Complex
3.2. Alternative Mechanisms for Brain Pathlogy in TSC
3.3. Biallelic Mutations in the TSC1 or TSC2 Genes Are Rarely Detected in Cortical Tubers
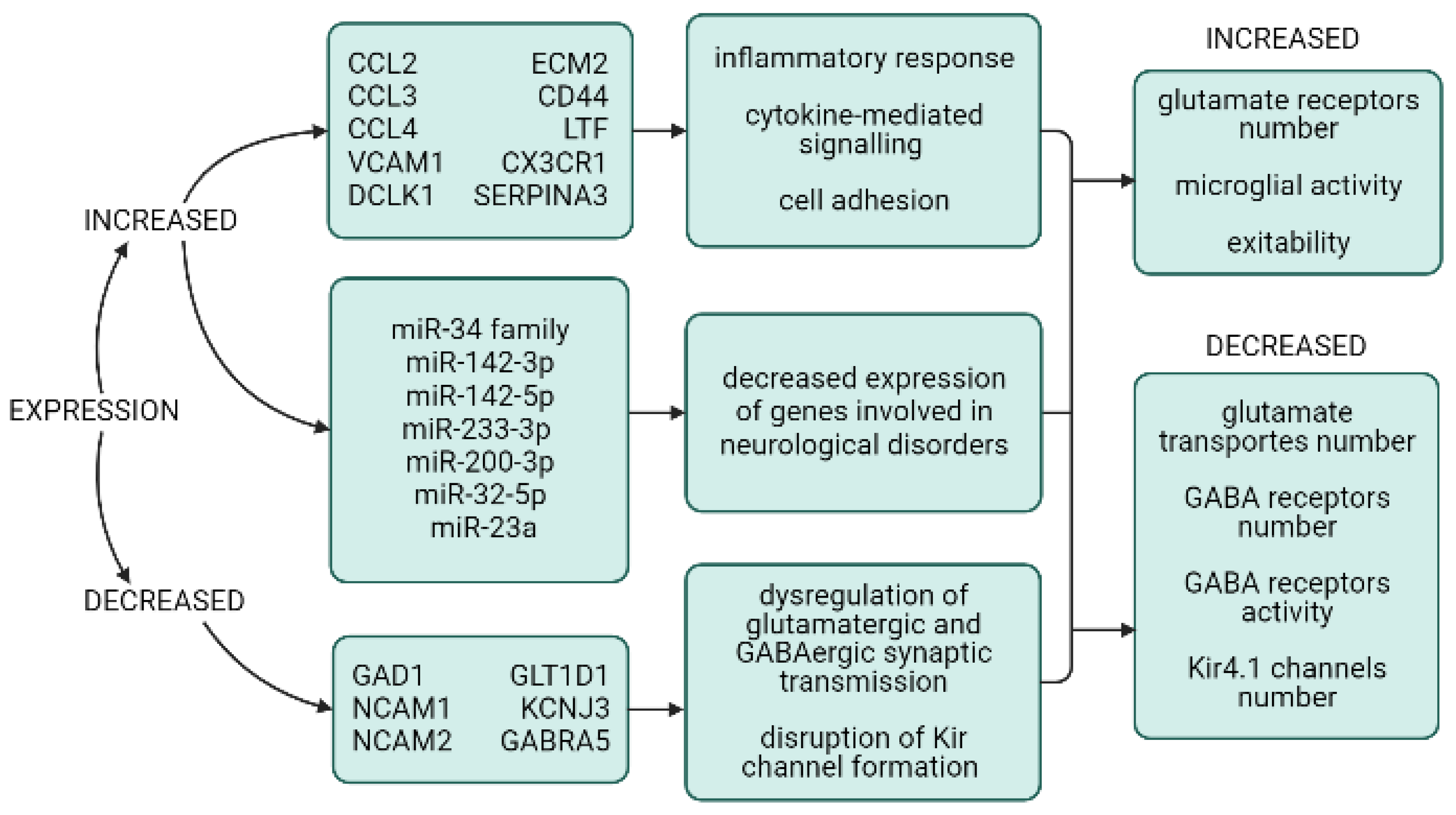
3.4. Transcriptome and miRNA Expression in Cortical Tubers
4. The Origin of Cortical Tubers
4.1. Normal Cortical Development and Tuberogenesis
4.2. Models for Studying the Development of Cortical Tubers
5. Epileptogenicity of Cortical Tubers and Its Treatment
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Henske, E.P.; Jóźwiak, S.; Kingswood, J.C.; Sampson, J.R.; Thiele, E.A. Tuberous sclerosis complex. Nat. Rev. Dis. Primers 2016, 2, 16035. [Google Scholar] [CrossRef]
- Curatolo, P.; Moavero, R.; de Vries, P.J. Neurological and neuropsychiatric aspects of tuberous sclerosis complex. Lancet Neurol. 2015, 14, 733–745. [Google Scholar] [CrossRef]
- Randle, S.C. Tuberous sclerosis complex: A review. Pediatr. Ann. 2017, 46, e166–e171. [Google Scholar] [CrossRef]
- Saxton, R.A.; Sabatini, D.M. mTOR Signaling in Growth, Metabolism, and Disease. Cell 2017, 168, 960–976. [Google Scholar] [CrossRef]
- Feliciano, D.M. The neurodevelopmental pathogenesis of tuberous sclerosis complex (TSC). Front. Neuroanat. 2020, 14, 39. [Google Scholar] [CrossRef]
- Sancak, O.; Nellist, M.; Goedbloed, M.; Elfferich, P.; Wouters, C.; Maat-Kievit, A.; Zonnenberg, B.; Verhoef, S.; Halley, D.; van den Ouweland, A. Mutational analysis of the TSC1 and TSC2 genes in a diagnostic setting: Genotype–phenotype correlations and comparison of diagnostic DNA techniques in Tuberous Sclerosis Complex. Eur. J. Hum. Genet. 2005, 13, 731–741. [Google Scholar] [CrossRef]
- Moavero, R.; Mühlebner, A.; Luinenburg, M.J.; Craiu, D.; Aronica, E.; Curatolo, P. Genetic pathogenesis of the epileptogenic lesions in Tuberous Sclerosis Complex: Therapeutic targeting of the mTOR pathway. Epilepsy Behav. 2022, 131, 107713. [Google Scholar] [CrossRef]
- Mühlebner, A.; Iyer, A.M.; van Scheppingen, J.; Anink, J.J.; Jansen, F.E.; Veersema, T.J.; Braun, K.P.; Spliet, W.G.M.; van Hecke, W.; Söylemezoğlu, F.; et al. Specific pattern of maturation and differentiation in the formation of cortical tubers in tuberous sclerosis complex (TSC): Evidence from layer-specific marker expression. J. Neurodev. Disord. 2016, 8, 9. [Google Scholar] [CrossRef]
- Mizuguchi, M. Abnormal giant cells in the cerebral lesions of tuberous sclerosis complex. Congenit. Anom. 2007, 47, 2–8. [Google Scholar] [CrossRef]
- Wong, M.; Crino, P.B. Tuberous sclerosis and epilepsy: Role of astrocytes. Glia 2012, 60, 1244–1250. [Google Scholar] [CrossRef]
- Mühlebner, A.; van Scheppingen, J.; Hulshof, H.M.; Scholl, T.; Iyer, A.M.; Anink, J.J.; van den Ouweland, A.M.W.; Nellist, M.D.; Jansen, F.E.; Spliet, W.G.M.; et al. Novel Histopathological Patterns in Cortical Tubers of Epilepsy Surgery Patients with Tuberous Sclerosis Complex. PLoS ONE 2016, 11, e0157396. [Google Scholar] [CrossRef]
- Boer, K.; Jansen, F.; Nellist, M.; Redeker, S.; van den Ouweland, A.M.W.; Spliet, W.G.M.; van Nieuwenhuizen, O.; Troost, D.; Crino, P.B.; Aronica, E. Inflammatory processes in cortical tubers and subependymal giant cell tumors of tuberous sclerosis complex. Epilepsy Res. 2008, 78, 7–21. [Google Scholar] [CrossRef]
- Veersema, T.J.; de Neef, A.; van Scheppingen, J.; Ferrier, C.H.; van Eijsden, P.; Gosselaar, P.H.; van Rijen, P.C.; Spliet, W.G.M.; Braun, K.P.J.; Mühlebner, A.; et al. Changes in vascular density in resected tissue of 97 patients with mild malformation of cortical development, focal cortical dysplasia or TSC-related cortical tubers. Int. J. Dev. Neurosci. 2019, 79, 96–104. [Google Scholar] [CrossRef]
- Chu-Shore, C.J.; Frosch, M.P.; Grant, P.E.; Thiele, E.A. Progressive multifocal cystlike cortical tubers in tuberous sclerosis complex: Clinical and neuropathologic findings. Epilepsia 2009, 50, 2648–2651. [Google Scholar] [CrossRef]
- Kalantari, B.N.; Salamon, N. Neuroimaging of tuberous sclerosis: Spectrum of pathologic findings and frontiers in imaging. AJR Am. J. Roentgenol. 2008, 190, W304–W309. [Google Scholar] [CrossRef]
- Marcotte, L.; Aronica, E.; Baybis, M.; Crino, P.B. Cytoarchitectural alterations are widespread in cerebral cortex in tuberous sclerosis complex. Acta Neuropathol. 2012, 123, 685–693. [Google Scholar] [CrossRef]
- Doherty, C.; Goh, S.; Young Poussaint, T.; Erdag, N.; Thiele, E.A. Prognostic significance of tuber count and location in tuberous sclerosis complex. J. Child Neurol. 2005, 20, 837–841. [Google Scholar] [CrossRef]
- Chu-Shore, C.J.; Major, P.; Montenegro, M.; Thiele, E. Cyst-like tubers are associated with TSC2 and epilepsy in tuberous sclerosis complex. Neurology 2009, 72, 1165–1169. [Google Scholar] [CrossRef]
- Qin, W.; Chan, J.A.; Vinters, H.V.; Mathern, G.W.; Franz, D.N.; Taillon, B.E.; Bouffard, P.; Kwiatkowski, D.J. Analysis of TSC cortical tubers by deep sequencing of TSC1, TSC2 and KRAS demonstrates that small second-hit mutations in these genes are rare events. Brain Pathol. 2010, 20, 1096–1105. [Google Scholar] [CrossRef]
- Martin, K.R.; Zhou, W.; Bowman, M.J.; Shih, J.; Au, K.S.; Dittenhafer-Reed, K.E.; Sisson, K.A.; Koeman, J.; Weisenberger, D.J.; Cottingham, S.L.; et al. The genomic landscape of tuberous sclerosis complex. Nat. Commun. 2017, 8, 15816. [Google Scholar] [CrossRef]
- Sosunov, A.A.; McGovern, R.A.; Mikell, C.B.; Wu, X.; Coughlin, D.G.; Crino, P.B.; Weiner, H.L.; Ghatan, S.; Goldman, J.E.; McKhann, G.M. Epileptogenic but MRI-normal perituberal tissue in Tuberous Sclerosis Complex contains tuber-specific abnormalities. Acta Neuropathol. Commun. 2015, 3, 17. [Google Scholar] [CrossRef] [PubMed]
- Prabowo, A.S.; Anink, J.J.; Lammens, M.; Nellist, M.; van den Ouweland, A.M.W.; Adle-Biassette, H.; Sarnat, H.B.; Flores-Sarnat, L.; Crino, P.B.; Aronica, E. Fetal brain lesions in tuberous sclerosis complex: TORC1 activation and inflammation. Brain Pathol. 2013, 23, 45–59. [Google Scholar] [CrossRef] [PubMed]
- Najm, I.M.; Sarnat, H.B.; Blümcke, I. Review: The international consensus classification of Focal Cortical Dysplasia—A critical update 2018. Neuropathol. Appl. Neurobiol. 2018, 44, 18–31. [Google Scholar] [CrossRef] [PubMed]
- Crino, P.B. mTOR signaling in epilepsy: Insights from malformations of cortical development. Cold Spring Harb. Perspect. Med. 2015, 5, a022442. [Google Scholar] [CrossRef]
- Russo, C.; Nastro, A.; Cicala, D.; De Liso, M.; Covelli, E.M.; Cinalli, G. Neuroimaging in tuberous sclerosis complex. Childs Nerv. Syst. 2020, 36, 2497–2509. [Google Scholar] [CrossRef]
- Gallagher, A.; Grant, E.P.; Madan, N.; Jarrett, D.Y.; Lyczkowski, D.A.; Thiele, E.A. MRI findings reveal three different types of tubers in patients with tuberous sclerosis complex. J. Neurol. 2010, 257, 1373–1381. [Google Scholar] [CrossRef]
- Zhang, M.-N.; Zou, L.-P.; Wang, Y.-Y.; Pang, L.-Y.; Ma, S.-F.; Huang, L.-L.; Gao, Y.; Lu, Q.; Franz, D.N. Calcification in cerebral parenchyma affects pharmacoresistant epilepsy in tuberous sclerosis. Seizure 2018, 60, 86–90. [Google Scholar] [CrossRef]
- Boer, K.; Troost, D.; Jansen, F.; Nellist, M.; van den Ouweland, A.M.W.; Geurts, J.J.G.; Spliet, W.G.M.; Crino, P.; Aronica, E. Clinicopathological and immunohistochemical findings in an autopsy case of tuberous sclerosis complex. Neuropathology 2008, 28, 577–590. [Google Scholar] [CrossRef]
- Talos, D.M.; Kwiatkowski, D.J.; Cordero, K.; Black, P.M.; Jensen, F.E. Cell-specific alterations of glutamate receptor expression in tuberous sclerosis complex cortical tubers. Ann. Neurol. 2008, 63, 454–465. [Google Scholar] [CrossRef]
- Gelot, A.B.; Represa, A. Progression of fetal brain lesions in tuberous sclerosis complex. Front. Neurosci. 2020, 14, 899. [Google Scholar] [CrossRef]
- Aronica, E.; Crino, P.B. Epilepsy related to developmental tumors and malformations of cortical development. Neurotherapeutics 2014, 11, 251–268. [Google Scholar] [CrossRef] [PubMed]
- Zimmer, T.S.; Broekaart, D.W.M.; Gruber, V.-E.; van Vliet, E.A.; Mühlebner, A.; Aronica, E. Tuberous Sclerosis Complex as Disease Model for Investigating mTOR-Related Gliopathy during Epileptogenesis. Front. Neurol. 2020, 11, 1028. [Google Scholar] [CrossRef] [PubMed]
- Arena, A.; Zimmer, T.S.; van Scheppingen, J.; Korotkov, A.; Anink, J.J.; Mühlebner, A.; Jansen, F.E.; van Hecke, W.; Spliet, W.G.; van Rijen, P.C.; et al. Oxidative stress and inflammation in a spectrum of epileptogenic cortical malformations: Molecular insights into their interdependence. Brain Pathol. 2019, 29, 351–365. [Google Scholar] [CrossRef]
- Mühlebner, A.; van Scheppingen, J.; de Neef, A.; Bongaarts, A.; Zimmer, T.S.; Mills, J.D.; Jansen, F.E.; Spliet, W.G.M.; Krsek, P.; Zamecnik, J.; et al. Myelin pathology beyond white matter in tuberous sclerosis complex (TSC) cortical tubers. J. Neuropathol. Exp. Neurol. 2020, 79, 1054–1064. [Google Scholar] [CrossRef] [PubMed]
- Feliciano, D.M.; Lin, T.V.; Hartman, N.W.; Bartley, C.M.; Kubera, C.; Hsieh, L.; Lafourcade, C.; O’Keefe, R.A.; Bordey, A. A circuitry and biochemical basis for tuberous sclerosis symptoms: From epilepsy to neurocognitive deficits. Int. J. Dev. Neurosci. 2013, 31, 667–678. [Google Scholar] [CrossRef]
- Meikle, L.; Talos, D.M.; Onda, H.; Pollizzi, K.; Rotenberg, A.; Sahin, M.; Jensen, F.E.; Kwiatkowski, D.J. A mouse model of tuberous sclerosis: Neuronal loss of TSC1 causes dysplastic and ectopic neurons, reduced myelination, seizure activity, and limited survival. J. Neurosci. 2007, 27, 5546–5558. [Google Scholar] [CrossRef]
- Zhang, B.; Zou, J.; Han, L.; Rensing, N.; Wong, M. Microglial activation during epileptogenesis in a mouse model of tuberous sclerosis complex. Epilepsia 2016, 57, 1317–1325. [Google Scholar] [CrossRef]
- Zimmer, T.S.; Korotkov, A.; Zwakenberg, S.; Jansen, F.E.; Zwartkruis, F.J.T.; Rensing, N.R.; Wong, M.; Mühlebner, A.; van Vliet, E.A.; Aronica, E.; et al. Upregulation of the pathogenic transcription factor SPI1/PU.1 in tuberous sclerosis complex and focal cortical dysplasia by oxidative stress. Brain Pathol. 2021, 31, e12949. [Google Scholar] [CrossRef]
- Yang, H.; Yu, Z.; Chen, X.; Li, J.; Li, N.; Cheng, J.; Gao, N.; Yuan, H.-X.; Ye, D.; Guan, K.-L.; et al. Structural insights into TSC complex assembly and GAP activity on Rheb. Nat. Commun. 2021, 12, 339. [Google Scholar] [CrossRef]
- Hoogeveen-Westerveld, M.; Wentink, M.; van den Heuvel, D.; Mozaffari, M.; Ekong, R.; Povey, S.; den Dunnen, J.T.; Metcalfe, K.; Vallee, S.; Krueger, S.; et al. Functional assessment of variants in the TSC1 and TSC2 genes identified in individuals with Tuberous Sclerosis Complex. Hum. Mutat. 2011, 32, 424–435. [Google Scholar] [CrossRef]
- Hoogeveen-Westerveld, M.; Ekong, R.; Povey, S.; Mayer, K.; Lannoy, N.; Elmslie, F.; Bebin, M.; Dies, K.; Thompson, C.; Sparagana, S.P.; et al. Functional assessment of TSC2 variants identified in individuals with tuberous sclerosis complex. Hum. Mutat. 2013, 34, 167–175. [Google Scholar] [CrossRef]
- Dibble, C.C.; Elis, W.; Menon, S.; Qin, W.; Klekota, J.; Asara, J.M.; Finan, P.M.; Kwiatkowski, D.J.; Murphy, L.O.; Manning, B.D. TBC1D7 is a third subunit of the TSC1-TSC2 complex upstream of mTORC1. Mol. Cell 2012, 47, 535–546. [Google Scholar] [CrossRef] [PubMed]
- Qin, J.; Wang, Z.; Hoogeveen-Westerveld, M.; Shen, G.; Gong, W.; Nellist, M.; Xu, W. Structural Basis of the Interaction between Tuberous Sclerosis Complex 1 (TSC1) and Tre2-Bub2-Cdc16 Domain Family Member 7 (TBC1D7). J. Biol. Chem. 2016, 291, 8591–8601. [Google Scholar] [CrossRef] [PubMed]
- Tee, A.R.; Sampson, J.R.; Pal, D.K.; Bateman, J.M. The role of mTOR signalling in neurogenesis, insights from tuberous sclerosis complex. Semin. Cell Dev. Biol. 2016, 52, 12–20. [Google Scholar] [CrossRef] [PubMed]
- Crino, P.B. The mTOR signalling cascade: Paving new roads to cure neurological disease. Nat. Rev. Neurol. 2016, 12, 379–392. [Google Scholar] [CrossRef]
- Salussolia, C.L.; Klonowska, K.; Kwiatkowski, D.J.; Sahin, M. Genetic etiologies, diagnosis, and treatment of tuberous sclerosis complex. Annu. Rev. Genomics Hum. Genet. 2019, 20, 217–240. [Google Scholar] [CrossRef]
- Ogórek, B.; Hamieh, L.; Hulshof, H.M.; Lasseter, K.; Klonowska, K.; Kuijf, H.; Moavero, R.; Hertzberg, C.; Weschke, B.; Riney, K.; et al. TSC2 pathogenic variants are predictive of severe clinical manifestations in TSC infants: Results of the EPISTOP study. Genet. Med. 2020, 22, 1489–1497. [Google Scholar] [CrossRef]
- Jansen, F.E.; Vincken, K.L.; Algra, A.; Anbeek, P.; Braams, O.; Nellist, M.; Zonnenberg, B.A.; Jennekens-Schinkel, A.; van den Ouweland, A.; Halley, D.; et al. Cognitive impairment in tuberous sclerosis complex is a multifactorial condition. Neurology 2008, 70, 916–923. [Google Scholar] [CrossRef]
- Overwater, I.E.; Swenker, R.; van der Ende, E.L.; Hanemaayer, K.B.; Hoogeveen-Westerveld, M.; van Eeghen, A.M.; Lequin, M.H.; van den Ouweland, A.M.; Moll, H.A.; Nellist, M.; et al. Genotype and brain pathology phenotype in children with tuberous sclerosis complex. Eur. J. Hum. Genet. 2016, 24, 1688–1695. [Google Scholar] [CrossRef]
- Ding, Y.; Wang, J.; Zhou, S.; Zhou, Y.; Zhang, L.; Yu, L.; Wang, Y. Genotype and phenotype analysis of chinese children with tuberous sclerosis complex: A pediatric cohort study. Front. Genet. 2020, 11, 204. [Google Scholar] [CrossRef]
- Farach, L.S.; Pearson, D.A.; Woodhouse, J.P.; Schraw, J.M.; Sahin, M.; Krueger, D.A.; Wu, J.Y.; Bebin, E.M.; Lupo, P.J.; Au, K.S.; et al. Tuberous sclerosis complex genotypes and developmental phenotype. Pediatr. Neurol. 2019, 96, 58–63. [Google Scholar] [CrossRef]
- He, J.; Zhou, W.J.; Shi, J.; Lin, J.L.; Zhang, B.Q.; Sun, Z.H. Analysis of genotypes, EEG and phenotypes of tuberous sclerosis complex patients. Zhonghua Yi Xue Za Zhi 2020, 100, 136–140. [Google Scholar] [CrossRef]
- Mietzsch, U.; McKenna, J.; Reith, R.M.; Way, S.W.; Gambello, M.J. Comparative analysis of TSC1 and TSC2 single and double radial glial cell mutants. J. Comp. Neurol. 2013, 521, 3817–3831. [Google Scholar] [CrossRef]
- D’Gama, A.M.; Walsh, C.A. Somatic mosaicism and neurodevelopmental disease. Nat. Neurosci. 2018, 21, 1504–1514. [Google Scholar] [CrossRef]
- Iffland, P.H.; Crino, P.B. The role of somatic mutational events in the pathogenesis of epilepsy. Curr. Opin. Neurol. 2019, 32, 191–197. [Google Scholar] [CrossRef] [PubMed]
- Rowitch, D.H.; Kriegstein, A.R. Developmental genetics of vertebrate glial-cell specification. Nature 2010, 468, 214–222. [Google Scholar] [CrossRef]
- Ma, J.; Meng, Y.; Kwiatkowski, D.J.; Chen, X.; Peng, H.; Sun, Q.; Zha, X.; Wang, F.; Wang, Y.; Jing, Y.; et al. Mammalian target of rapamycin regulates murine and human cell differentiation through STAT3/p63/Jagged/Notch cascade. J. Clin. Invest. 2010, 120, 103–114. [Google Scholar] [CrossRef] [PubMed]
- Blair, J.D.; Hockemeyer, D.; Bateup, H.S. Genetically engineered human cortical spheroid models of tuberous sclerosis. Nat. Med. 2018, 24, 1568–1578. [Google Scholar] [CrossRef] [PubMed]
- Lim, K.C.; Crino, P.B. Focal malformations of cortical development: New vistas for molecular pathogenesis. Neuroscience 2013, 252, 262–276. [Google Scholar] [CrossRef]
- Yasin, S.A.; Ali, A.M.; Tata, M.; Picker, S.R.; Anderson, G.W.; Latimer-Bowman, E.; Nicholson, S.L.; Harkness, W.; Cross, J.H.; Paine, S.M.L.; et al. mTOR-dependent abnormalities in autophagy characterize human malformations of cortical development: Evidence from focal cortical dysplasia and tuberous sclerosis. Acta Neuropathol. 2013, 126, 207–218. [Google Scholar] [CrossRef]
- Cukovic, D.; Bagla, S.; Ukasik, D.; Stemmer, P.M.; Jena, B.P.; Naik, A.R.; Sood, S.; Asano, E.; Luat, A.; Chugani, D.C.; et al. Exosomes in Epilepsy of Tuberous Sclerosis Complex: Carriers of Pro-Inflammatory MicroRNAs. Noncoding RNA 2021, 7, 40. [Google Scholar] [CrossRef]
- Zadjali, F.; Kumar, P.; Yao, Y.; Johnson, D.; Astrinidis, A.; Vogel, P.; Gross, K.W.; Bissler, J.J. Tuberous sclerosis complex axis controls renal extracellular vesicle production and protein content. Int. J. Mol. Sci. 2020, 21, 1729. [Google Scholar] [CrossRef] [PubMed]
- Bae, J.-H.; Kim, J.H. Exosome Release by Glucose Deprivation Is Important for the Viability of TSC-Null Cells. Cells 2022, 11, 2862. [Google Scholar] [CrossRef] [PubMed]
- Moon, U.Y.; Park, J.Y.; Park, R.; Cho, J.Y.; Hughes, L.J.; McKenna, J.; Goetzl, L.; Cho, S.-H.; Crino, P.B.; Gambello, M.J.; et al. Impaired Reelin-Dab1 Signaling Contributes to Neuronal Migration Deficits of Tuberous Sclerosis Complex. Cell Rep. 2015, 12, 965–978. [Google Scholar] [CrossRef]
- Rossini, L.; Moroni, R.F.; Tassi, L.; Watakabe, A.; Yamamori, T.; Spreafico, R.; Garbelli, R. Altered layer-specific gene expression in cortical samples from patients with temporal lobe epilepsy. Epilepsia 2011, 52, 1928–1937. [Google Scholar] [CrossRef]
- Iyer, A.; Prabowo, A.; Anink, J.; Spliet, W.G.M.; van Rijen, P.C.; Aronica, E. Cell injury and premature neurodegeneration in focal malformations of cortical development. Brain Pathol. 2014, 24, 1–17. [Google Scholar] [CrossRef]
- Alves, M.M.; Fuhler, G.M.; Queiroz, K.C.S.; Scholma, J.; Goorden, S.; Anink, J.; Spek, C.A.; Hoogeveen-Westerveld, M.; Bruno, M.J.; Nellist, M.; et al. PAK2 is an effector of TSC1/2 signaling independent of mTOR and a potential therapeutic target for Tuberous Sclerosis Complex. Sci. Rep. 2015, 5, 14534. [Google Scholar] [CrossRef]
- Choi, J.H.; Ro, J.Y. The 2020 WHO classification of tumors of soft tissue: Selected changes and new entities. Adv. Anat. Pathol. 2021, 28, 44–58. [Google Scholar] [CrossRef]
- Louis, D.N.; Ohgaki, H.; Wiestler, O.D.; Cavenee, W.K.; Burger, P.C.; Jouvet, A.; Scheithauer, B.W.; Kleihues, P. The 2007 WHO classification of tumours of the central nervous system. Acta Neuropathol. 2007, 114, 97–109. [Google Scholar] [CrossRef] [PubMed]
- Mocellin, S. Cutaneous Angiofibroma. In Soft Tissue Tumors: A Practical and Comprehensive Guide to Sarcomas and Benign Neoplasms; Springer International Publishing: Cham, Switzerland, 2021; pp. 189–192. ISBN 978-3-030-58709-3. [Google Scholar]
- Rodin, R.E.; Walsh, C.A. Somatic mutation in pediatric neurological diseases. Pediatr. Neurol. 2018, 87, 20–22. [Google Scholar] [CrossRef]
- Niida, Y.; Stemmer-Rachamimov, A.O.; Logrip, M.; Tapon, D.; Perez, R.; Kwiatkowski, D.J.; Sims, K.; MacCollin, M.; Louis, D.N.; Ramesh, V. Survey of somatic mutations in tuberous sclerosis complex (TSC) hamartomas suggests different genetic mechanisms for pathogenesis of TSC lesions. Am. J. Hum. Genet. 2001, 69, 493–503. [Google Scholar] [CrossRef] [PubMed]
- Kobow, K.; Ziemann, M.; Kaipananickal, H.; Khurana, I.; Mühlebner, A.; Feucht, M.; Hainfellner, J.A.; Czech, T.; Aronica, E.; Pieper, T.; et al. Genomic DNA methylation distinguishes subtypes of human focal cortical dysplasia. Epilepsia 2019, 60, 1091–1103. [Google Scholar] [CrossRef] [PubMed]
- Jeganathan, D.; Fox, M.F.; Young, J.M.; Yates, J.R.W.; Osborne, J.P.; Povey, S. Nonsense-mediated RNA decay in the TSC1 gene suggests a useful tool pre- and post-positional cloning. Hum. Genet. 2002, 111, 555–565. [Google Scholar] [CrossRef] [PubMed]
- Armstrong, L.C.; Westlake, G.; Snow, J.P.; Cawthon, B.; Armour, E.; Bowman, A.B.; Ess, K.C. Heterozygous loss of TSC2 alters p53 signaling and human stem cell reprogramming. Hum. Mol. Genet. 2017, 26, 4629–4641. [Google Scholar] [CrossRef] [PubMed]
- Hoogeveen-Westerveld, M.; Ekong, R.; Povey, S.; Karbassi, I.; Batish, S.D.; den Dunnen, J.T.; van Eeghen, A.; Thiele, E.; Mayer, K.; Dies, K.; et al. Functional assessment of TSC1 missense variants identified in individuals with tuberous sclerosis complex. Hum. Mutat. 2012, 33, 476–479. [Google Scholar] [CrossRef]
- Lim, J.S.; Gopalappa, R.; Kim, S.H.; Ramakrishna, S.; Lee, M.; Kim, W.-I.; Kim, J.; Park, S.M.; Lee, J.; Oh, J.-H.; et al. Somatic mutations in TSC1 and TSC2 cause focal cortical dysplasia. Am. J. Hum. Genet. 2017, 100, 454–472. [Google Scholar] [CrossRef]
- Nakashima, M.; Saitsu, H.; Takei, N.; Tohyama, J.; Kato, M.; Kitaura, H.; Shiina, M.; Shirozu, H.; Masuda, H.; Watanabe, K.; et al. Somatic Mutations in the MTOR gene cause focal cortical dysplasia type IIb. Ann. Neurol. 2015, 78, 375–386. [Google Scholar] [CrossRef]
- Crino, P.B.; Aronica, E.; Baltuch, G.; Nathanson, K.L. Biallelic TSC gene inactivation in tuberous sclerosis complex. Neurology 2010, 74, 1716–1723. [Google Scholar] [CrossRef]
- Winden, K.D.; Sundberg, M.; Yang, C.; Wafa, S.M.A.; Dwyer, S.; Chen, P.-F.; Buttermore, E.D.; Sahin, M. Biallelic Mutations in TSC2 Lead to Abnormalities Associated with Cortical Tubers in Human iPSC-Derived Neurons. J. Neurosci. 2019, 39, 9294–9305. [Google Scholar] [CrossRef]
- Eichmüller, O.L.; Corsini, N.S.; Vértesy, Á.; Morassut, I.; Scholl, T.; Gruber, V.-E.; Peer, A.M.; Chu, J.; Novatchkova, M.; Hainfellner, J.A.; et al. Amplification of human interneuron progenitors promotes brain tumors and neurological defects. Science 2022, 375, eabf5546. [Google Scholar] [CrossRef]
- Boer, K.; Crino, P.B.; Gorter, J.A.; Nellist, M.; Jansen, F.E.; Spliet, W.G.M.; van Rijen, P.C.; Wittink, F.R.A.; Breit, T.M.; Troost, D.; et al. Gene expression analysis of tuberous sclerosis complex cortical tubers reveals increased expression of adhesion and inflammatory factors. Brain Pathol. 2010, 20, 704–719. [Google Scholar] [CrossRef] [PubMed]
- Mills, J.D.; Iyer, A.M.; van Scheppingen, J.; Bongaarts, A.; Anink, J.J.; Janssen, B.; Zimmer, T.S.; Spliet, W.G.; van Rijen, P.C.; Jansen, F.E.; et al. Coding and small non-coding transcriptional landscape of tuberous sclerosis complex cortical tubers: Implications for pathophysiology and treatment. Sci. Rep. 2017, 7, 8089. [Google Scholar] [CrossRef] [PubMed]
- Korotkov, A.; Luinenburg, M.J.; Romagnolo, A.; Zimmer, T.S.; van Scheppingen, J.; Bongaarts, A.; Broekaart, D.W.M.; Anink, J.J.; Mijnsbergen, C.; Jansen, F.E.; et al. Down-regulation of the brain-specific cell-adhesion molecule contactin-3 in tuberous sclerosis complex during the early postnatal period. J. Neurodev. Disord. 2022, 14, 8. [Google Scholar] [CrossRef] [PubMed]
- van Scheppingen, J.; Iyer, A.M.; Prabowo, A.S.; Mühlebner, A.; Anink, J.J.; Scholl, T.; Feucht, M.; Jansen, F.E.; Spliet, W.G.; Krsek, P.; et al. Expression of microRNAs miR21, miR146a, and miR155 in tuberous sclerosis complex cortical tubers and their regulation in human astrocytes and SEGA-derived cell cultures. Glia 2016, 64, 1066–1082. [Google Scholar] [CrossRef]
- Bagla, S.; Cukovic, D.; Asano, E.; Sood, S.; Luat, A.; Chugani, H.T.; Chugani, D.C.; Dombkowski, A.A. A distinct microRNA expression profile is associated with α[11C]-methyl-L-tryptophan (AMT) PET uptake in epileptogenic cortical tubers resected from patients with tuberous sclerosis complex. Neurobiol. Dis. 2018, 109, 76–87. [Google Scholar] [CrossRef]
- Dombkowski, A.A.; Batista, C.E.; Cukovic, D.; Carruthers, N.J.; Ranganathan, R.; Shukla, U.; Stemmer, P.M.; Chugani, H.T.; Chugani, D.C. Cortical Tubers: Windows into Dysregulation of Epilepsy Risk and Synaptic Signaling Genes by MicroRNAs. Cereb. Cortex 2016, 26, 1059–1071. [Google Scholar] [CrossRef]
- Franco, S.J.; Müller, U. Shaping our minds: Stem and progenitor cell diversity in the mammalian neocortex. Neuron 2013, 77, 19–34. [Google Scholar] [CrossRef]
- Park, S.H.; Pepkowitz, S.H.; Kerfoot, C.; De Rosa, M.J.; Poukens, V.; Wienecke, R.; DeClue, J.E.; Vinters, H.V. Tuberous sclerosis in a 20-week gestation fetus: Immunohistochemical study. Acta Neuropathol. 1997, 94, 180–186. [Google Scholar] [CrossRef]
- Wei, J.; Li, P.; Chiriboga, L.; Mizuguchi, M.; Yee, H.; Miller, D.C.; Greco, M.A. Tuberous sclerosis in a 19-week fetus: Immunohistochemical and molecular study of hamartin and tuberin. Pediatr. Dev. Pathol. 2002, 5, 448–464. [Google Scholar] [CrossRef]
- Carson, R.P.; Van Nielen, D.L.; Winzenburger, P.A.; Ess, K.C. Neuronal and glia abnormalities in TSC1-deficient forebrain and partial rescue by rapamycin. Neurobiol. Dis. 2012, 45, 369–380. [Google Scholar] [CrossRef]
- Fu, C.; Ess, K.C. Conditional and domain-specific inactivation of the Tsc2 gene in neural progenitor cells. Genesis 2013, 51, 284–292. [Google Scholar] [CrossRef] [PubMed]
- Way, S.W.; McKenna, J.; Mietzsch, U.; Reith, R.M.; Wu, H.C.-J.; Gambello, M.J. Loss of Tsc2 in radial glia models the brain pathology of tuberous sclerosis complex in the mouse. Hum. Mol. Genet. 2009, 18, 1252–1265. [Google Scholar] [CrossRef] [PubMed]
- Goto, J.; Talos, D.M.; Klein, P.; Qin, W.; Chekaluk, Y.I.; Anderl, S.; Malinowska, I.A.; Di Nardo, A.; Bronson, R.T.; Chan, J.A.; et al. Regulable neural progenitor-specific Tsc1 loss yields giant cells with organellar dysfunction in a model of tuberous sclerosis complex. Proc. Natl. Acad. Sci. USA 2011, 108, E1070–E1079. [Google Scholar] [CrossRef] [PubMed]
- Zeng, L.-H.; Rensing, N.R.; Zhang, B.; Gutmann, D.H.; Gambello, M.J.; Wong, M. Tsc2 gene inactivation causes a more severe epilepsy phenotype than Tsc1 inactivation in a mouse model of tuberous sclerosis complex. Hum. Mol. Genet. 2011, 20, 445–454. [Google Scholar] [CrossRef]
- Kannan, L.; Vogrin, S.; Bailey, C.; Maixner, W.; Harvey, A.S. Centre of epileptogenic tubers generate and propagate seizures in tuberous sclerosis. Brain 2016, 139, 2653–2667. [Google Scholar] [CrossRef]
- Fong, C.Y.; Bleasel, A.; Dexter, M.A.; Lawson, J.A.; Wong, C.H. Successful epilepsy surgery for tuberous sclerosis complex evaluated by stereoelectroencephalography. Epileptic Disord. 2020, 22, 633–641. [Google Scholar] [CrossRef]
- Kumar, A.; Asano, E.; Chugani, H.T. α-[11C]-methyl-L-tryptophan PET for tracer localization of epileptogenic brain regions: Clinical studies. Biomark. Med. 2011, 5, 577–584. [Google Scholar] [CrossRef]
- Chandra, P.S.; Salamon, N.; Huang, J.; Wu, J.Y.; Koh, S.; Vinters, H.V.; Mathern, G.W. FDG-PET/MRI coregistration and diffusion-tensor imaging distinguish epileptogenic tubers and cortex in patients with tuberous sclerosis complex: A preliminary report. Epilepsia 2006, 47, 1543–1549. [Google Scholar] [CrossRef]
- von Oertzen, T.J. PET and ictal SPECT can be helpful for localizing epileptic foci. Curr. Opin. Neurol. 2018, 31, 184–191. [Google Scholar] [CrossRef]
- French, J.A.; Lawson, J.A.; Yapici, Z.; Ikeda, H.; Polster, T.; Nabbout, R.; Curatolo, P.; de Vries, P.J.; Dlugos, D.J.; Berkowitz, N.; et al. Adjunctive everolimus therapy for treatment-resistant focal-onset seizures associated with tuberous sclerosis (EXIST-3): A phase 3, randomised, double-blind, placebo-controlled study. Lancet 2016, 388, 2153–2163. [Google Scholar] [CrossRef]
- Lasarge, C.L.; Danzer, S.C. Mechanisms regulating neuronal excitability and seizure development following mTOR pathway hyperactivation. Front. Mol. Neurosci. 2014, 7, 18. [Google Scholar] [CrossRef]
- Zeng, L.-H.; Bero, A.W.; Zhang, B.; Holtzman, D.M.; Wong, M. Modulation of astrocyte glutamate transporters decreases seizures in a mouse model of Tuberous Sclerosis Complex. Neurobiol. Dis. 2010, 37, 764–771. [Google Scholar] [CrossRef] [PubMed]
- Crino, P.B. Molecular pathogenesis of tuber formation in tuberous sclerosis complex. J. Child Neurol. 2004, 19, 716–725. [Google Scholar] [CrossRef] [PubMed]
- Wong, M. The role of glia in epilepsy, intellectual disability, and other neurodevelopmental disorders in tuberous sclerosis complex. J. Neurodev. Disord. 2019, 11, 30. [Google Scholar] [CrossRef] [PubMed]
- Tye, C.; Mcewen, F.S.; Liang, H.; Underwood, L.; Woodhouse, E.; Barker, E.D.; Sheerin, F.; Yates, J.R.W.; Bolton, P.F.; Tuberous Sclerosis 2000 Study Group. Long-term cognitive outcomes in tuberous sclerosis complex. Dev. Med. Child Neurol. 2020, 62, 322–329. [Google Scholar] [CrossRef]
- Sadowski, K.; Kotulska-Jóźwiak, K.; Jóźwiak, S. Role of mTOR inhibitors in epilepsy treatment. Pharmacol. Rep. 2015, 67, 636–646. [Google Scholar] [CrossRef]
- Kotulska, K.; Kwiatkowski, D.J.; Curatolo, P.; Weschke, B.; Riney, K.; Jansen, F.; Feucht, M.; Krsek, P.; Nabbout, R.; Jansen, A.C.; et al. Prevention of Epilepsy in Infants with Tuberous Sclerosis Complex in the EPISTOP Trial. Ann. Neurol. 2021, 89, 304–314. [Google Scholar] [CrossRef]
- Sarbassov, D.D.; Ali, S.M.; Sengupta, S.; Sheen, J.-H.; Hsu, P.P.; Bagley, A.F.; Markhard, A.L.; Sabatini, D.M. Prolonged rapamycin treatment inhibits mTORC2 assembly and Akt/PKB. Mol. Cell 2006, 22, 159–168. [Google Scholar] [CrossRef]
- Lu, D.S.; Karas, P.J.; Krueger, D.A.; Weiner, H.L. Central nervous system manifestations of tuberous sclerosis complex. Am. J. Med. Genet. C Semin. Med. Genet. 2018, 178, 291–298. [Google Scholar] [CrossRef]
| Gene | Function of the Encoded Protein | Expression Level |
|---|---|---|
| CCL2 | Recruits monocytes, memory T-cells, and dendritic cells to the inflammation sites | Increased |
| CCL3 | Participates in acute inflammation, attraction, and activation of polymorphonuclear leukocytes | Increased |
| CCL4 | Chemoattractant for natural killer cells, monocytes, and other immune cells | Increased |
| SERPINA3 | Participates in the regulation of inflammation and the immune response | Increased |
| CX3CR1 | A receptor for the chemokine CX3CL1 involved in the adhesion and migration of lymphocytes | Increased |
| ECM2 | Participates in cell adhesion | Increased |
| VCAM1 | Participates in the adhesion of leukocytes and endothelial cells and signal transmission | Increased |
| CD44 | A hyaluronic acid receptor involved in the activation of lymphocytes and the recirculation and homing of hematopoietic cells | Increased |
| DCLK1 | Promotes neuronal migration during neurogenesis | Increased |
| LTF | Participates in iron ion binding and transport, has antibacterial, antiviral, antiparasitic, catalytic, anticancer, and antiallergic properties | Increased |
| GAD1 | Catalyzes the conversion of glutamate to GABA | Decreased |
| GLT1D1 | Promotes the elimination of glutamate from the synaptic gap | Decreased |
| GABRA5 | The GABA A receptor α5 subunit | Decreased |
| KCNJ3 | Participates in the reduction of resting membrane potential during hyperpolarization by conducting a weak potassium current inside the cell | Decreased |
| NCAM1, NCAM2 | Transmit a signal that induces neurite growth, participate in cell adhesion | Decreased |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bychkova, E.; Dorofeeva, M.; Levov, A.; Kislyakov, A.; Karandasheva, K.; Strelnikov, V.; Anoshkin, K. Specific Features of Focal Cortical Dysplasia in Tuberous Sclerosis Complex. Curr. Issues Mol. Biol. 2023, 45, 3977-3996. https://doi.org/10.3390/cimb45050254
Bychkova E, Dorofeeva M, Levov A, Kislyakov A, Karandasheva K, Strelnikov V, Anoshkin K. Specific Features of Focal Cortical Dysplasia in Tuberous Sclerosis Complex. Current Issues in Molecular Biology. 2023; 45(5):3977-3996. https://doi.org/10.3390/cimb45050254
Chicago/Turabian StyleBychkova, Ekaterina, Marina Dorofeeva, Aleksandr Levov, Alexey Kislyakov, Kristina Karandasheva, Vladimir Strelnikov, and Kirill Anoshkin. 2023. "Specific Features of Focal Cortical Dysplasia in Tuberous Sclerosis Complex" Current Issues in Molecular Biology 45, no. 5: 3977-3996. https://doi.org/10.3390/cimb45050254
APA StyleBychkova, E., Dorofeeva, M., Levov, A., Kislyakov, A., Karandasheva, K., Strelnikov, V., & Anoshkin, K. (2023). Specific Features of Focal Cortical Dysplasia in Tuberous Sclerosis Complex. Current Issues in Molecular Biology, 45(5), 3977-3996. https://doi.org/10.3390/cimb45050254






