A Concise Review of Extraction and Characterization of Chondroitin Sulphate from Fish and Fish Wastes for Pharmacological Application
Abstract
:1. Introduction
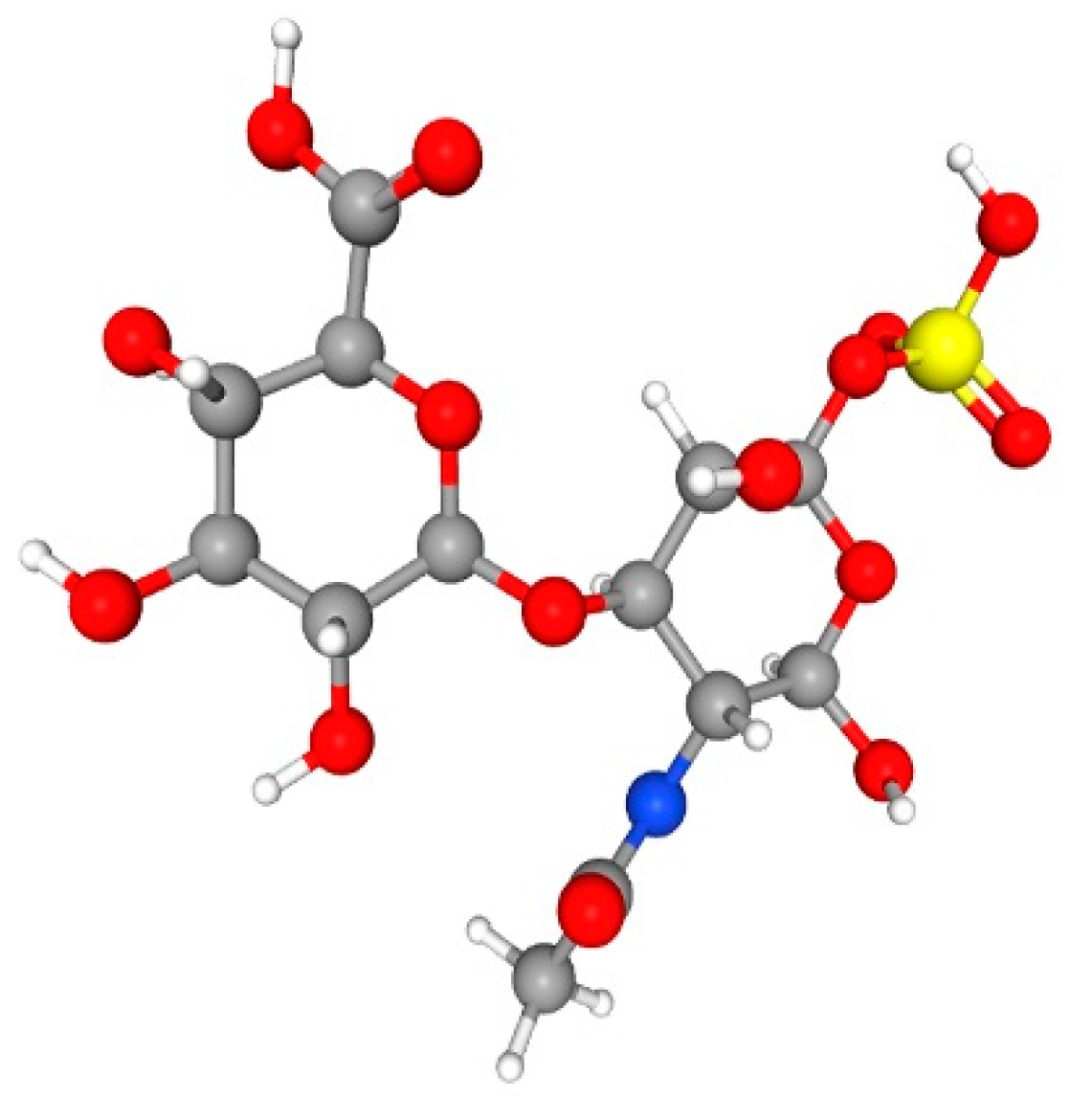
2. Chondroitin Sulphate
2.1. Biosynthesis of CS
2.2. Fish and Fish Wastes for CS Production
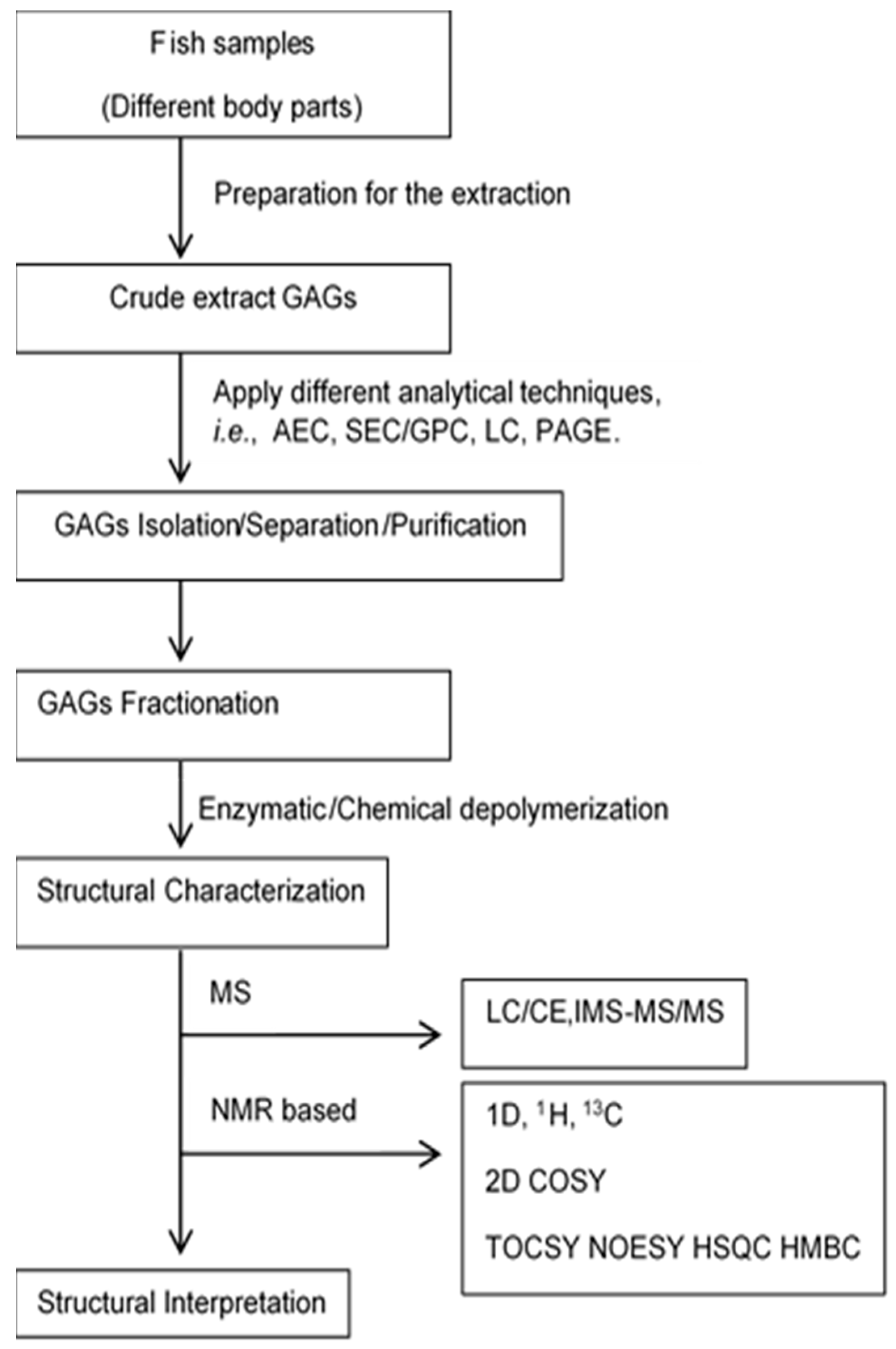
2.2.1. Extraction and Isolation Technique
2.2.2. Purification and Characterization
3. Prospective Pharmacological Application
4. Conclusions and Recommendations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Urbi, Z.; Azmi, N.S.; Hossain, M.S. Antimicrobial Role of Glycosaminoglycans: Beyond Bacterial Adhesion to Host Cell. In Proceedings of the 1st International Electronic Conference on Antibiotics, Basel, Switzerland, 8–17 May 2021; pp. 1–4. [Google Scholar]
- Idrus, N.H.; Azmi, N.S.; Palliah, J.V. Waste to wealth: Alternative source of glycosaminoglycans (GAGs) from sea food waste. IIOAB J. 2016, 7, 543–547. [Google Scholar]
- Sham, M.M.; Azmi, N.S.; Rahim, M.H.A. Glycosaminoglycans (GAGs) versus Cancer. J. Environ. Bioremediation Toxicol. 2014, 2, 58–61. [Google Scholar] [CrossRef]
- Lokwani, R.; Azmi, N.S.; Yusoff, M.M.; Ichwan, S.J.A. Beyond anticoagulant: Heparin as a potential anticancer agent. J. Biochem. Microbiol. Biotechnol. 2014, 2, 76–82. [Google Scholar] [CrossRef]
- Azmi, N.S. Reactive Oligosaccharides for Surface Derivatisation; The University of Liverpool: Liverpool, UK, 2013. [Google Scholar]
- Narayanaswamy, R.; Kanagesan, S.; Pandurangan, A.; Padmanabhan, P. Basics to different imaging techniques, different nanobiomaterials for image enhancement. In Nanobiomaterials in Medical Imaging; Elsevier: Amsterdam, The Netherlands, 2016; pp. 101–129. [Google Scholar]
- Tóth, G.; Vékey, K.; Sugár, S.; Kovalszky, I.; Drahos, L.; Turiák, L. Salt gradient chromatographic separation of chondroitin sulfate disaccharides. J. Chromatogr. A 2020, 1619, 460979. [Google Scholar] [CrossRef]
- Solakyildirim, K. Recent advances in glycosaminoglycan analysis by various mass spectrometry techniques. Anal. Bioanal. Chem. 2019, 411, 3731–3741. [Google Scholar] [CrossRef]
- Mende, M.; Bednarek, C.; Wawryszyn, M.; Sauter, P.; Biskup, M.B.; Schepers, U.; Bräse, S. Chemical synthesis of glycosaminoglycans. Chem. Rev. 2016, 116, 8193–8255. [Google Scholar] [CrossRef]
- Liu, Z.; Zhang, F.; Li, L.; Li, G.; He, W.; Linhardt, R.J. Compositional analysis and structural elucidation of glycosaminoglycans in chicken eggs. Glycoconj. J. 2014, 31, 593–602. [Google Scholar] [CrossRef]
- Place, L.W.; Kelly, S.M.; Kipper, M.J. Synthesis and characterization of proteoglycan-mimetic graft copolymers with tunable glycosaminoglycan density. Biomacromolecules 2014, 15, 3772–3780. [Google Scholar] [CrossRef]
- Lin, H.Y.; Lee, C.L.; Lo, Y.T.; Wang, T.J.; Huang, S.F.; Chen, T.L.; Wang, Y.S.; Niu, D.M.; Chuang, C.K.; Lin, S.P. The relationships between urinary glycosaminoglycan levels and phenotypes of mucopolysaccharidoses. Mol. Genet. Genom. Med. 2018, 6, 982–992. [Google Scholar] [CrossRef]
- Pomin, V.H. NMR structural determination of unique invertebrate glycosaminoglycans endowed with medical properties. Carbohydr. Res. 2015, 413, 41–50. [Google Scholar] [CrossRef]
- Datta, P.; Linhardt, R.J.; Sharfstein, S.T. Industrial production of glycosaminoglycans. Encycl. Microbiol. 2019, 681–690. [Google Scholar] [CrossRef]
- GlobeNewsWire. Chondroitin Sulfate Market Size Is Projected to Reach USD 1.70 Billion by 2030, Growing at a CAGR of 3.9%: Straits Research. Available online: https://www.globenewswire.com/en/news-release/2022/07/18/2481308/0/en/Chondroitin-Sulfate-Market-Size-is-projected-to-reach-USD-1-70-Billion-by-2030-growing-at-a-CAGR-of-3-9-Straits-Research.html (accessed on 20 August 2022).
- Valcarcel, J.; Novoa-Carballal, R.; Pérez-Martín, R.I.; Reis, R.L.; Vázquez, J.A. Glycosaminoglycans from marine sources as therapeutic agents. Biotechnol. Adv. 2017, 35, 711–725. [Google Scholar] [CrossRef]
- Gavva, C.; Patel, K.; Kudre, T.; Sharan, K.; Chilkunda, D.N. Glycosaminoglycans from fresh water fish processing discard-Isolation, structural characterization, and osteogenic activity. Int. J. Biol. Macromol. 2020, 145, 558–567. [Google Scholar] [CrossRef]
- Novoa-Carballal, R.; Perez-Martin, R.; Blanco, M.; Sotelo, C.G.; Fassini, D.; Nunes, C.; Coimbra, M.A.; Silva, T.H.; Reis, R.L.; Vazquez, J.A. By-products of Scyliorhinus canicula, Prionace glauca and Raja clavata: A valuable source of predominantly 6S sulfated chondroitin sulfate. Carbohydr. Polym. 2017, 157, 31–37. [Google Scholar] [CrossRef]
- Oliveira, C.; Ferreira, A.S.; Novoa-Carballal, R.; Nunes, C.; Pashkuleva, I.; Neves, N.M.; Coimbra, M.A.; Reis, R.L.; Martins, A.; Silva, T.H. The Key Role of Sulfation and Branching on Fucoidan Antitumor Activity. Macromol. Biosci. 2017, 17, 1600340. [Google Scholar] [CrossRef]
- Poh, Z.W.; Gan, C.H.; Lee, E.J.; Guo, S.; Yip, G.W.; Lam, Y. Divergent synthesis of chondroitin sulfate disaccharides and identification of sulfate motifs that inhibit triple negative breast cancer. Sci. Rep. 2015, 5, 14355. [Google Scholar] [CrossRef]
- Abdallah, M.M.; Fernandez, N.; Matias, A.A.; Bronze, M.D.R. Hyaluronic acid and Chondroitin sulfate from marine and terrestrial sources: Extraction and purification methods. Carbohydr. Polym. 2020, 243, 116441. [Google Scholar] [CrossRef]
- Bougatef, H.; Krichen, F.; Capitani, F.; Amor, I.B.; Maccari, F.; Mantovani, V.; Galeotti, F.; Volpi, N.; Bougatef, A.; Sila, A. Chondroitin sulfate/dermatan sulfate from corb (Sciaena umbra) skin: Purification, structural analysis and anticoagulant effect. Carbohydr. Polym. 2018, 196, 272–278. [Google Scholar] [CrossRef]
- Krichen, F.; Ghlissi, Z.; Amor, I.B.; Sayari, N.; Kallel, R.; Gargouri, J.; Sahnoun, Z.; Boudawara, T.; Bougatef, A. In vitro and in vivo anticoagulant activity and toxicological studies of marine sulfated glycosaminoglycans. Exp. Toxicol. Pathol. 2017, 69, 45–53. [Google Scholar] [CrossRef]
- Wang, W.; Shi, L.; Qin, Y.; Li, F. Research and Application of Chondroitin Sulfate/Dermatan Sulfate-Degrading Enzymes. Front. Cell Dev. Biol. 2020, 8, 560442. [Google Scholar] [CrossRef]
- Sugahara, K.; Mikami, T.; Uyama, T.; Mizuguchi, S.; Nomura, K.; Kitagawa, H. Recent advances in the structural biology of chondroitin sulfate and dermatan sulfate. Curr. Opin. Struct. Biol. 2003, 13, 612–620. [Google Scholar] [CrossRef] [PubMed]
- Sugahara, K.; Kitagawa, H. Recent advances in the study of the biosynthesis and functions of sulfated glycosaminoglycans. Curr. Opin. Struct. Biol. 2000, 10, 518–527. [Google Scholar] [CrossRef]
- Pacheco, B.; Malmström, A.; Maccarana, M. Two dermatan sulfate epimerases form iduronic acid domains in dermatan sulfate. J. Biol. Chem. 2009, 284, 9788–9795. [Google Scholar] [CrossRef] [PubMed]
- Maccarana, M.; Olander, B.; Malmström, J.; Tiedemann, K.; Aebersold, R.; Lindahl, U.; Li, J.-p.; Malmström, A. Biosynthesis of dermatan sulfate: Chondroitin-glucuronate C5-epimerase is identical to SART2. J. Biol. Chem. 2006, 281, 11560–11568. [Google Scholar] [CrossRef]
- Habuchi, O. Diversity and functions of glycosaminoglycan sulfotransferases. Biochim. Et Biophys. Acta (BBA)-Gen. Subj. 2000, 1474, 115–127. [Google Scholar] [CrossRef]
- de Moura, H.C.; Novello, C.R.; Balbinot-Alfaro, E.; Dusman, E.; Barddal, H.P.O.; Almeida, I.V.; Vicentini, V.E.P.; Prentice-Hernandez, C.; Alfaro, A.T. Obtaining glycosaminoglycans from tilapia (oreochromis niloticus) scales and evaluation of its anticoagulant and cytotoxic activities: Glycosaminoglycans from tilapia scales: Anticoagulant and cytotoxic activities. Food Res. Int. 2021, 140, 110012. [Google Scholar] [CrossRef]
- Kaczmarek, B.; Sionkowska, A.; Skopinska-Wisniewska, J. Influence of glycosaminoglycans on the properties of thin films based on chitosan/collagen blends. J. Mech. Behav. Biomed. Mater. 2018, 80, 189–193. [Google Scholar] [CrossRef]
- Maccari, F.; Galeotti, F.; Volpi, N. Isolation and structural characterization of chondroitin sulfate from bony fishes. Carbohydr. Polym. 2015, 129, 143–147. [Google Scholar] [CrossRef]
- Nogueira, A.V.; Rossi, G.R.; Iacomini, M.; Sassaki, G.L.; Trindade, E.S.; Cipriani, T.R. Viscera of fishes as raw material for extraction of glycosaminoglycans of pharmacological interest. Int. J. Biol. Macromol. 2019, 121, 239–248. [Google Scholar] [CrossRef]
- Rodrigues, J.A.G.; Quindere, A.L.G.; de Queiroz, I.N.L.; Coura, C.O.; Araujo, G.S.; Benevides, N.M.B. Purification, physical and chemical characterization, and anticoagulant activity of glycosaminoglycans isolated from the skin of Nile tilapia (Oreochromis niloticus)/Purificacao, caracterizacao fisico-quimica e atividade anticoagulante de glicosaminoglicanos isolados da pele de tilapia do Nilo (Oreochromis niloticus). Acta Scientiarum. Technol. 2011, 33, 233–242. [Google Scholar]
- Ticar, B.F.; Rohmah, Z.; Neri, T.A.N.; Pahila, I.G.; Vasconcelos, A.; Archer-Hartmann, S.A.; Reiter, C.E.N.; Dobruchowska, J.M.; Choi, B.D.; Heiss, C.; et al. Biocompatibility and structural characterization of glycosaminoglycans isolated from heads of silver-banded whiting (Sillago argentifasciata Martin & Montalban 1935). Int. J. Biol. Macromol. 2020, 151, 663–676. [Google Scholar] [CrossRef]
- Nakano, T.; Betti, M.; Pietrasik, Z. Extraction, isolation and analysis of chondroitin sulfate glycosaminoglycans. Recent Pat. Food Nutr. Agric. 2010, 2, 61–74. [Google Scholar] [CrossRef]
- Balbinot-Alfaro, E.; da Rocha, M.; da Trindade Alfaro, A.; Martins, V.G. Properties, bioactive potential and extraction processes of glycosaminoglycans: An overview. Ciência Rural 2021, 51, e20200821. [Google Scholar] [CrossRef]
- Rao, J.R.; Nair, B.U. Novel approach towards recovery of glycosaminoglycans from tannery wastewater. Bioresour. Technol. 2011, 102, 872–878. [Google Scholar] [CrossRef]
- Nakano, T.; Pietrasik, Z.; Ozimek, L.; Betti, M. Extraction, isolation and analysis of chondroitin sulfate from broiler chicken biomass. Process Biochem. 2012, 47, 1909–1918. [Google Scholar] [CrossRef]
- Bai, M.; Han, W.; Zhao, X.; Wang, Q.; Gao, Y.; Deng, S. Glycosaminoglycans from a Sea Snake (Lapemis curtus): Extraction, Structural Characterization and Antioxidant Activity. Mar. Drugs 2018, 16, 170. [Google Scholar] [CrossRef]
- Blanco, M.; Fraguas, J.; Sotelo, C.G.; Perez-Martin, R.I.; Vazquez, J.A. Production of Chondroitin Sulphate from Head, Skeleton and Fins of Scyliorhinus canicula By-Products by Combination of Enzymatic, Chemical Precipitation and Ultrafiltration Methodologies. Mar. Drugs 2015, 13, 3287–3308. [Google Scholar] [CrossRef]
- Song, S.; Yu, Q.; Zhang, B.; Ai, C.; Sun, Y.; Fu, Y.; Zhao, M.; Wen, C. Quantification and comparison of acidic polysaccharides in edible fish intestines and livers using HPLC-MS/MS. Glycoconj. J. 2017, 34, 625–632. [Google Scholar] [CrossRef]
- Kim, S.B.; Ji, C.I.; Woo, J.W.; Do, J.R.; Cho, S.M.; Lee, Y.B.; Kang, S.N.; Park, J.H. Simplified purification of chondroitin sulphate from scapular cartilage of shortfin mako shark (Isurus oxyrinchus). Int. J. Food Sci. Technol. 2012, 47, 91–99. [Google Scholar] [CrossRef]
- Talmoudi, N.; Ghariani, N.; Sadok, S. Glycosaminoglycans from Co-Products of «Scyliorhinus canicula»: Extraction and Purification in Reference to the European Pharmacopoeia Requirement. Biol. Proced. Online 2020, 22, 1. [Google Scholar] [CrossRef]
- Oliveira, A.P.V.; de Abreu Feitosa, V.; de Oliveira, J.M.; Coelho, A.L.; de Araújo P. Vieira, L.; de Assis Rocha da Silva, F.; de Assis Avelino Figueredo Sobrinho, F.; Duarte, E.B.; de Souza, B.W.; de sá Moreira de Souza Filho, M. Characteristics of Chondroitin Sulfate Extracted of Tilapia (Oreochromis niloticus) Processing. Procedia Eng. 2017, 200, 193–199. [Google Scholar] [CrossRef]
- Gargiulo, V.; Lanzetta, R.; Parrilli, M.; De Castro, C. Structural analysis of chondroitin sulfate from Scyliorhinus canicula: A useful source of this polysaccharide. Glycobiology 2009, 19, 1485–1491. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Amado, I.R.; Vazquez, J.A.; Pastrana, L.; Teixeira, J.A. Cheese whey: A cost-effective alternative for hyaluronic acid production by Streptococcus zooepidemicus. Food Chem. 2016, 198, 54–61. [Google Scholar] [CrossRef]
- Nakano, T.; Nakano, K.; Sim, J.S. Extraction of Glycosaminoglycan Peptide from Bovine Nasal Cartilage with 0.1 M Sodium Acetate. J. Agric. Food Chem. 1998, 46, 772–778. [Google Scholar] [CrossRef] [PubMed]
- Song, Y.; Zhang, F.; Linhardt, R.J. Analysis of the Glycosaminoglycan Chains of Proteoglycans. J. Histochem. Cytochem. 2021, 69, 121–135. [Google Scholar] [CrossRef] [PubMed]
- Paulsen, B.S.; Olafsdóttir, E.S.; Ingólfsdóttir, K. Chromatography and electrophoresis in separation and characterization of polysaccharides from lichens. J. Chromatogr. A 2002, 967, 163–171. [Google Scholar] [CrossRef]
- Volpi, N. Quality of different chondroitin sulfate preparations in relation to their therapeutic activity. J. Pharm. Pharmacol. 2009, 61, 1271–1280. [Google Scholar] [CrossRef]
- Opdensteinen, P.; Clodt, J.I.; Müschen, C.R.; Filiz, V.; Buyel, J.F. A Combined Ultrafiltration/Diafiltration Step Facilitates the Purification of Cyanovirin-N From Transgenic Tobacco Extracts. Front. Bioeng. Biotechnol. 2019, 6, 206. [Google Scholar] [CrossRef]
- Lignot, B.; Lahogue, V.; Bourseau, P. Enzymatic extraction of chondroitin sulfate from skate cartilage and concentration-desalting by ultrafiltration. J. Biotechnol. 2003, 103, 281–284. [Google Scholar] [CrossRef]
- Choi, S.; Choi, W.; Kim, S.; Lee, S.-Y.; Noh, I.; Kim, C.-W. Purification and biocompatibility of fermented hyaluronic acid for its applications to biomaterials. Biomater. Res. 2014, 18, 6. [Google Scholar] [CrossRef]
- Liu, H.F.; Ma, J.; Winter, C.; Bayer, R. Recovery and purification process development for monoclonal antibody production. MAbs 2010, 2, 480–499. [Google Scholar] [CrossRef]
- Vázquez, J.A.; Blanco, M.; Fraguas, J.; Pastrana, L.; Pérez-Martín, R. Optimisation of the extraction and purification of chondroitin sulphate from head by-products of Prionace glauca by environmental friendly processes. Food Chem. 2016, 198, 28–35. [Google Scholar] [CrossRef] [Green Version]
- Li, A.; Xiong, S. Preparation and Structure Analysis of Chondroitin Sulfate from Pig Laryngeal Cartilage. In Proceedings of the 2010 4th International Conference on Bioinformatics and Biomedical Engineering, Chengdu, China, 18–20 June 2010; pp. 1–5. [Google Scholar] [CrossRef]
- Sundaresan, G.; Abraham, R.J.J.; Appa Rao, V.; Narendra Babu, R.; Govind, V.; Meti, M.F. Established method of chondroitin sulphate extraction from buffalo (Bubalus bubalis) cartilages and its identification by FTIR. J. Food Sci. Technol. 2018, 55, 3439–3445. [Google Scholar] [CrossRef]
- Melrose, J.; Ghosh, P. Determination of the average molecular size of glycosaminoglycans by fast protein liquid chromatography. J. Chromatogr. A 1993, 637, 91–95. [Google Scholar] [CrossRef]
- Liu, J.; Zhou, L.; He, Z.; Gao, N.; Shang, F.; Xu, J.; Li, Z.; Yang, Z.; Wu, M.; Zhao, J. Structural analysis and biological activity of a highly regular glycosaminoglycan from Achatina fulica. Carbohydr. Polym. 2018, 181, 433–441. [Google Scholar] [CrossRef]
- Jeong, K.-S. Development of High Purity Purification Method of Chondroitin Sulfate Extracted from Skate Cartilage. J. Korea Acad.-Ind. Coop. Soc. 2016, 17, 9–17. [Google Scholar]
- Khare, A.; Houliston, S.; Black, T. Isolating chondroitin sulfate. U.S. Patent Application 10/704,866, 29 July 2004. [Google Scholar]
- Mizumoto, S.; Sugahara, K. Glycosaminoglycan chain analysis and characterization (glycosylation/epimerization). Methods Mol. Biol. 2012, 836, 99–115. [Google Scholar] [CrossRef]
- van Kuppevelt, T.H.; Oosterhof, A.; Versteeg, E.M.M.; Podhumljak, E.; van de Westerlo, E.M.A.; Daamen, W.F. Sequencing of glycosaminoglycans with potential to interrogate sequence-specific interactions. Sci. Rep. 2017, 7, 14785. [Google Scholar] [CrossRef]
- McClellan, J.E.; Costello, C.E.; O’Connor, P.B.; Zaia, J. Influence of charge state on product ion mass spectra and the determination of 4S/6S sulfation sequence of chondroitin sulfate oligosaccharides. Anal. Chem. 2002, 74, 3760–3771. [Google Scholar] [CrossRef]
- Shi, X.; Huang, Y.; Mao, Y.; Naimy, H.; Zaia, J. Tandem mass spectrometry of heparan sulfate negative ions: Sulfate loss patterns and chemical modification methods for improvement of product ion profiles. J. Am. Soc. Mass Spectrom. 2012, 23, 1498–1511. [Google Scholar] [CrossRef]
- Leach, F.E., III; Riley, N.M.; Westphall, M.S.; Coon, J.J.; Amster, I.J. Negative Electron Transfer Dissociation Sequencing of Increasingly Sulfated Glycosaminoglycan Oligosaccharides on an Orbitrap Mass Spectrometer. J. Am. Soc. Mass Spectrom. 2017, 28, 1844–1854. [Google Scholar] [CrossRef]
- Mainreck, N.; Brézillon, S.; Sockalingum, G.D.; Maquart, F.-X.; Manfait, M.; Wegrowski, Y. Rapid Characterization of Glycosaminoglycans Using a Combined Approach by Infrared and Raman Microspectroscopies. J. Pharm. Sci. 2011, 100, 441–450. [Google Scholar] [CrossRef]
- Beni, S.; Limtiaco, J.F.K.; Larive, C.K. Analysis and characterization of heparin impurities. Anal. Bioanal. Chem. 2011, 399, 527–539. [Google Scholar] [CrossRef]
- Mikšík, I.; Kubinová, Š.; Morvan, M.; Výborný, K.; Tatar, A.; Král, V.; Záruba, K.; Sýkora, D. Analysis of Chondroitin/Dermatan Sulphate Disaccharides Using High-Performance Liquid Chromatography. Separations 2020, 7, 49. [Google Scholar] [CrossRef]
- Mizumoto, S.; Yamada, S. Congenital Disorders of Deficiency in Glycosaminoglycan Biosynthesis. Front. Genet. 2021, 12, 717535. [Google Scholar] [CrossRef]
- Ghosh, P.; Smith, M.; Wells, C. Second line agents in osteoarthritis. In Second Line Agents in the Treatment of Rheumatic Diseases; Dixon, J.S., Furst, D.E., Eds.; Marcel Dekker: New York, NY, USA, 1992; pp. 363–427. [Google Scholar]
- Jurkiewicz, E.; Panse, P.; Jentsch, K.-D.; Hartmann, H.; Hunsmann, G. In vitro anti-HIV-1 activity of chondroitin polysulphate. AIDS 1989, 3, 423–427. [Google Scholar] [CrossRef]
- Kato, D.; Era, S.; Watanabe, I.; Arihara, M.; Sugiura, N.; Kimata, K.; Suzuki, Y.; Morita, K.; Hidari, K.I.P.J.; Suzuki, T. Antiviral activity of chondroitin sulphate E targeting dengue virus envelope protein. Antivir. Res. 2010, 88, 236–243. [Google Scholar] [CrossRef]
- Newburg, D.S.; Linhardt, R.J.; Ampofo, S.A.; Yolken, R.H. Human milk glycosaminoglycans inhibit HIV glycoprotein gp120 binding to its host cell CD4 receptor. J. Nutr. 1995, 125, 419–424. [Google Scholar]
- Ornell, K.J.; Lozada, D.; Phan, N.V.; Coburn, J.M. Controlling methacryloyl substitution of chondroitin sulfate: Injectable hydrogels with tunable long-term drug release profiles. J. Mater. Chem. B 2019, 7, 2151–2161. [Google Scholar] [CrossRef]
- Geng, H.; Zhang, P.; Liu, L.; Shangguan, Y.; Cheng, X.; Liu, H.; Zhao, Y.; Hao, J.; Li, W.; Cui, J. Convergent architecting of multifunction-in-one hydrogels as wound dressings for surgical anti-infections. Mater. Today Chem. 2022, 25, 100968. [Google Scholar] [CrossRef]
- Alinejad, Y.; Adoungotchodo, A.; Hui, E.; Zehtabi, F.; Lerouge, S. An injectable chitosan/chondroitin sulfate hydrogel with tunable mechanical properties for cell therapy/tissue engineering. Int. J. Biol. Macromol. 2018, 113, 132–141. [Google Scholar] [CrossRef] [PubMed]
- Ma, Y.; Abdelnabi, R.; Delang, L.; Froeyen, M.; Luyten, W.; Neyts, J.; Mirabelli, C. New class of early-stage enterovirus inhibitors with a novel mechanism of action. Antivir. Res. 2017, 147, 67–74. [Google Scholar] [CrossRef] [PubMed]
- Ren, Q.; Wang, J.; Liu, C.; Meng, L.-x.; Qian, R.-k.; Gao, H.-j.; Qin, W.; Zhou, C.-j.; Qiao, S.; Wang, H.-y. Exploring the sulfate patterns of chondroitin sulfate/dermatan sulfate and keratan sulfate in human pancreatic cancer. J. Pharm. Biomed. Anal. 2021, 205, 114339. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.; Liao, Q.; Price, M.; Moriarity, B.; Wolf, N.; Felices, M.; Miller, J.S.; Geller, M.A.; Bendzick, L.; Hopps, R. Chondroitin sulfate proteoglycan 4, a targetable oncoantigen that promotes ovarian cancer growth, invasion, cisplatin resistance and spheroid formation. Transl. Oncol. 2022, 16, 101318. [Google Scholar] [CrossRef]
- Iida, J.; Dorchak, J.; Clancy, R.; Slavik, J.; Ellsworth, R.; Katagiri, Y.; Pugacheva, E.N.; van Kuppevelt, T.H.; Mural, R.J.; Cutler, M.L. Role for chondroitin sulfate glycosaminoglycan in NEDD9-mediated breast cancer cell growth. Exp. Cell Res. 2015, 330, 358–370. [Google Scholar] [CrossRef]
- Li, H.; Zhang, P.; Luo, J.; Hu, D.; Huang, Y.; Zhang, Z.-R.; Fu, Y.; Gong, T. Chondroitin sulfate-linked prodrug nanoparticles target the golgi apparatus for cancer metastasis treatment. Acs Nano 2019, 13, 9386–9396. [Google Scholar] [CrossRef]
- Wegrowski, Y.; Maquart, F.X. Chondroitin sulfate proteoglycans in tumor progression. Adv. Pharmacol. 2006, 53, 297–321. [Google Scholar]
- Pudełko, A.; Wisowski, G.; Olczyk, K.; Koźma, E.M. The dual role of the glycosaminoglycan chondroitin-6-sulfate in the development, progression and metastasis of cancer. FEBS J. 2019, 286, 1815–1837. [Google Scholar] [CrossRef]
- Svensson, K.J.; Christianson, H.C.; Kucharzewska, P.; Fagerström, V.; Lundstedt, L.; Borgquist, S.; Jirström, K.; Belting, M. Chondroitin sulfate expression predicts poor outcome in breast cancer. Int. J. Oncol. 2011, 39, 1421–1428. [Google Scholar]
- Wu, R.; Li, P.; Wang, Y.; Su, N.; Xiao, M.; Li, X.; Shang, N. Structural analysis and anticancer activity of low-molecular-weight chondroitin sulfate from hybrid sturgeon cartilage. Carbohydr. Polym. 2022, 275, 118700. [Google Scholar] [CrossRef]
- Khan, A.R.; Yang, X.; Du, X.; Yang, H.; Liu, Y.; Khan, A.Q.; Zhai, G. Chondroitin sulfate derived theranostic and therapeutic nanocarriers for tumor-targeted drug delivery. Carbohydr. Polym. 2020, 233, 115837. [Google Scholar] [CrossRef]
- Asimakopoulou, A.P.; Theocharis, A.D.; Tzanakakis, G.N.; Karamanos, N.K. The biological role of chondroitin sulfate in cancer and chondroitin-based anticancer agents. Vivo 2008, 22, 385–389. [Google Scholar]
- Theocharis, A.D.; Tsolakis, I.; Tzanakakis, G.N.; Karamanos, N.K. Chondroitin sulfate as a key molecule in the development of atherosclerosis and cancer progression. Adv. Pharmacol. 2006, 53, 281–295. [Google Scholar]
- Silver, D.J.; Silver, J. Contributions of chondroitin sulfate proteoglycans to neurodevelopment, injury, and cancer. Curr. Opin. Neurobiol. 2014, 27, 171–178. [Google Scholar] [CrossRef]
- Li, H.; Cheng, F.; Wei, X.; Yi, X.; Tang, S.; Wang, Z.; Zhang, Y.S.; He, J.; Huang, Y. Injectable, self-healing, antibacterial, and hemostatic N, O-carboxymethyl chitosan/oxidized chondroitin sulfate composite hydrogel for wound dressing. Mater. Sci. Eng. C 2021, 118, 111324. [Google Scholar] [CrossRef]
- Anisha, B.S.; Sankar, D.; Mohandas, A.; Chennazhi, K.P.; Nair, S.V.; Jayakumar, R. Chitosan–hyaluronan/nano chondroitin sulfate ternary composite sponges for medical use. Carbohydr. Polym. 2013, 92, 1470–1476. [Google Scholar] [CrossRef]
- Lemons, M.L.; Howland, D.R.; Anderson, D.K. Chondroitin sulfate proteoglycan immunoreactivity increases following spinal cord injury and transplantation. Exp. Neurol. 1999, 160, 51–65. [Google Scholar] [CrossRef]
- Xu, K.; Wang, Z.; Copland, J.A.; Chakrabarti, R.; Florczyk, S.J. 3D porous chitosan-chondroitin sulfate scaffolds promote epithelial to mesenchymal transition in prostate cancer cells. Biomaterials 2020, 254, 120126. [Google Scholar] [CrossRef]
- Khan, A.A.; Mannan, V.; Pervaiz, M.A.; Akram, A.; Momin, E.S.; Sanusi, M.; Kashyap, T.; Elshaikh, A.O. The Role of Glucosamine and Chondroitin Sulfate in the Prevention of Colorectal Cancer: A Systematic Review. Cureus 2022, 14, e25401. [Google Scholar] [CrossRef]
- Avouac, B. Slow acting drugs in osteoarthritis: A step towards disease modification. Rev. Esp. Reumatol. 1993, 20, 221–222. [Google Scholar]
- Lequesne, M.; Brandt, K.; Bellamy, N.; Moskowitz, R.; Menkes, C.J.; Pelletier, J.P. Guidelines for testing slow acting drugs in osteoarthritis. J. Rheumatol. 1994, 41, 65–71. [Google Scholar]
- Ghosh, P.; Wells, C.; Smith, M.; Hutadilok, N. Chondroprotection, myth or reality: An experimental approach. Semin. Arthritis Rheum. 1990, 19, 3–9. [Google Scholar] [CrossRef]
- Baici, A.; Wagenhäuser, F.J. Reply ot the letter by P. Lualdi. Rheumatol. Int. 1993, 13, 41–43. [Google Scholar] [CrossRef]
- Lualdi, P. Bioavailability of oral chondroitin sulfate. Rheumatol. Int. 1993, 13, 39–40. [Google Scholar] [CrossRef] [PubMed]
- Thomas, J.V.; Smina, T.P.; Khanna, A.; Kunnumakkara, A.B.; Maliakel, B.; Mohanan, R.; Krishnakumar, I.M. Influence of a low-dose supplementation of curcumagalactomannoside complex (CurQfen) in knee osteoarthritis: A randomized, open-labeled, active-controlled clinical trial. Phytother. Res. 2021, 35, 1443–1455. [Google Scholar] [CrossRef]
- Bernetti, A.; Mangone, M.; Villani, C.; Alviti, F.; Valeo, M.; Grassi, M.C.; Migliore, A.; Viora, U.; Adriani, E.; Quirino, N. Appropriateness of clinical criteria for the use of SYmptomatic Slow-Acting Drug for OsteoArthritis (SYSADOA). A Delphi Method Consensus initiative among experts in Italy. Eur. J. Phys. Rehabil. Med. 2019, 55, 658–664. [Google Scholar] [CrossRef]
- Sarvilina, I.V.; Galustyan, A.N.; Hadzhidis, A.K.; Sardaryan, I.S.; Lavrov, N.V.; Gromova, O.A.; Prokofieva, Y.S. Comparative clinical and economic analysis of using SYSADOA drugs containing chondroitin sulphate or influencing its biosynthesis in the treatment of patients with stage II knee osteoarthritis. FARMAKOEKONOMIKA Mod. Pharm. Pharmacoepidemiol. 2020, 12, 255–266. [Google Scholar] [CrossRef]
- Volpi, N. Chondroitin sulphate for the treatment of osteoarthritis. Curr. Med. Chem.-Anti-Inflamm. Anti-Allergy Agents 2005, 4, 221–234. [Google Scholar] [CrossRef]
- Monfort, J.; Pelletier, J.-P.; Garcia-Giralt, N.; Martel-Pelletier, J. Biochemical basis of the effect of chondroitin sulphate on osteoarthritis articular tissues. Ann. Rheum. Dis. 2008, 67, 735–740. [Google Scholar] [CrossRef] [PubMed]
- Bishnoi, M.; Jain, A.; Hurkat, P.; Jain, S.K. Chondroitin sulphate: A focus on osteoarthritis. Glycoconj. J. 2016, 33, 693–705. [Google Scholar] [CrossRef] [PubMed]
- Uebelhart, D.; Thonar, E.J.M.A.; Zhang, J.; Williams, J.M. Protective effect of exogenous chondroitin 4,6-sulfate in the acute degradation of articular cartilage in the rabbit. Osteoarthr. Cartil. 1998, 6, 6–13. [Google Scholar] [CrossRef]
- Gibson, R.G.; Gibson, S.L.M.; Conway, V.; Chappell, D. Perna canaliculus in the treatment of arthritis. Practitioner 1980, 224, 955–960. [Google Scholar]
- Uebelhart, D.; Thonar, E.J.M.A.; Delmas, P.D.; Chantraine, A.; Vignon, E. Effects of oral chondroitin sulfate on the progression of knee osteoarthritis: A pilot study. Osteoarthr. Cartil. 1998, 6, 39–46. [Google Scholar] [CrossRef]
- Bucsi, L.; Poór, G. Efficacy and tolerability of oral chondroitin sulfate as a symptomatic slow-acting drug for osteoarthritis (SYSADOA) in the treatment of knee osteoarthritis. Osteoarthr. Cartil. 1998, 6, 31–36. [Google Scholar] [CrossRef]
- Bourgeois, P.; Chales, G.; Dehais, J.; Delcambre, B.; Kuntz, J.-L.; Rozenberg, S. Efficacy and tolerability of chondroitin sulfate 1200 mg/day vs chondroitin sulfate 3×400 mg/day vs placebo. Osteoarthr. Cartil. 1998, 6, 25–30. [Google Scholar] [CrossRef]
- Morreale, P.; Manopulo, R.; Galati, M.; Boccanera, L.; Saponati, G.; Bocchi, L. Comparison of the antiinflammatory efficacy of chondroitin sulfate and diclofenac sodium in patients with knee osteoarthritis. J. Rheumatol. 1996, 23, 1385–1391. [Google Scholar]
- Volpi, N. Chondroitin Sulfate Safety and Quality. Molecules 2019, 24, 1447. [Google Scholar] [CrossRef]
- Li, W.; Ura, K.; Takagi, Y. Industrial application of fish cartilaginous tissues. Curr. Res. Food Sci. 2022, 5, 698–709. [Google Scholar] [CrossRef]
- Medeiros, L.H.C.; Vasconcelos, B.M.F.; Silva, M.B.; Souza-Junior, A.A.; Chavante, S.F.; Andrade, G.P.V. Chondroitin sulfate from fish waste exhibits strong intracellular antioxidant potential. Braz. J. Med. Biol. Res. 2021, 54, e10730. [Google Scholar] [CrossRef]
- Krichen, F.; Volpi, N.; Sila, A.; Maccari, F.; Mantovani, V.; Galeotti, F.; Ellouz-Chaabouni, S.; Bougatef, A. Purification, structural characterization and antiproliferative properties of chondroitin sulfate/dermatan sulfate from tunisian fish skins. Int. J. Biol. Macromol. 2017, 95, 32–39. [Google Scholar] [CrossRef]
- Ajisaka, K.; Oyanagi, Y.; Miyazaki, T.; Suzuki, Y. Effect of the chelation of metal cation on the antioxidant activity of chondroitin sulfates. Biosci. Biotechnol. Biochem. 2016, 80, 1179–1185. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hashiguchi, T.; Kobayashi, T.; Fongmoon, D.; Shetty, A.K.; Mizumoto, S.; Miyamoto, N.; Nakamura, T.; Yamada, S.; Sugahara, K. Demonstration of the hepatocyte growth factor signaling pathway in the in vitro neuritogenic activity of chondroitin sulfate from ray fish cartilage. Biochim. Et Biophys. Acta (BBA) -Gen. Subj. 2011, 1810, 406–413. [Google Scholar] [CrossRef]
- Li, W.; Kobayashi, T.; Moroi, S.; Kotake, H.; Ikoma, T.; Saeki, H.; Ura, K.; Takagi, Y. Anti-obesity effects of chondroitin sulfate oligosaccharides from the skate Raja pulchra. Carbohydr. Polym. 2019, 214, 303–310. [Google Scholar] [CrossRef] [PubMed]
- Song, Y.O.; Kim, M.; Woo, M.; Baek, J.-M.; Kang, K.-H.; Kim, S.-H.; Roh, S.-S.; Park, C.H.; Jeong, K.-S.; Noh, J.-S. Chondroitin Sulfate-Rich Extract of Skate Cartilage Attenuates Lipopolysaccharide-Induced Liver Damage in Mice. Mar. Drugs 2017, 15, 178. [Google Scholar] [CrossRef] [PubMed]
- Im, A.R.; Park, Y.; Kim, Y.S. Isolation and Characterization of Chondroitin Sulfates from Sturgeon (Acipenser sinensis) and Their Effects on Growth of Fibroblasts. Biol. Pharm. Bull. 2010, 33, 1268–1273. [Google Scholar] [CrossRef] [PubMed]
- Gui, M.; Song, J.; Zhang, L.; Wang, S.; Wu, R.; Ma, C.; Li, P. Chemical characteristics and antithrombotic effect of chondroitin sulfates from sturgeon skull and sturgeon backbone. Carbohydr. Polym. 2015, 123, 454–460. [Google Scholar] [CrossRef]
- Zhang, Q.; Li, J.; Liu, C.; Song, C.; Li, P.; Yin, F.; Xiao, Y.; Li, J.; Jiang, W.; Zong, A.; et al. Protective effects of low molecular weight chondroitin sulfate on amyloid beta (Aβ)-induced damage in vitro and in vivo. Neuroscience 2015, 305, 169–182. [Google Scholar] [CrossRef] [PubMed]
- Olariu, L.; Dumitriu, B.; Craciun, L.; Buse, E.; Rosoiu, N.; Bojinca, M.; Papacocea, T. The in Vitro Influence of a Pharmaceutically Active Small Sea Fish Extract on Apoptosis and Proliferation Mechanisms Amplified by Inflammatory Conditions. Farmacia 2018, 66, 524–529. [Google Scholar] [CrossRef]

| Stages | Enzyme Involved | Specific Function in CS Biosynthesis |
|---|---|---|
| Initiation | Glycosyltransferase | Catalyzed linkage region in the tetra-saccharide structure |
| Disaccharide unit formation | Xylosyltransferase | Catalyzed linkage between xylose and serine residue |
| β1,4-galactosyltransferase I and β1,3-galactosyltransferase II | Catalyzed linkage between galactose and serine residues, in turn | |
| β1,3-glucuronyltransferase I | Catalyzed the formation of tetrasaccharide linkage region by adding GlcUA residue | |
| GalNAc transferase I | Catalyzed transfer of GalNAc residue to the nonreducing terminal GlcA residue and Chondroitin skeleton by adding GlcA and GalNAc residues in turn | |
| Polymerization | GalNAc transferase II and GlcA transferase II | Form repeating disaccharide GlcA-GlaNAc in Chondroitin skeleton by alternative catalysis |
| Source Name | Body Part | Enzyme | Extraction a | Analytical Methods | Yield | CS | Other GAGs | Reference |
|---|---|---|---|---|---|---|---|---|
| Nile tilapia | Skin | Alcalase | Acetone, chloroform, methanol, TCA, NaCl, ethanol | AEC, NMR, AGE | 0.15% DW | √ | DS, HS | [33] |
| Pacu fish | 0.18% DW | |||||||
| Nile tilapia | Scale | Crude papain | Acetone, TCA, ethanol | IEC, AGE, NMR | 0.86% DW | √ | - | [30] |
| Nile tilapia | Bone residues (spine) | Papain | Ethanol, NaCl | TGA, DSC, FTIR, SEM | 80% (residue: ethanol) | √ | - | [45] |
| Nile tilapia | Skin | Papain | Sodium acetate, CPC, ethanol | IEC, AGE | 10% | √ | DS | [34] |
| Grey triggerfish | Skin | Alcalase | Sodium acetate, CPC, NaCl, ethanol | CAE | 8.6% | √ | DS, HS | [23] |
| Smooth dogfish | 9.3% | |||||||
| Monkfish Codfish Spiny Dogfish and Tuna | Bones | Papain (ED) | Acetone, Sodium acetate, NaCl, ethanol | AEC, AGE | Monkfish 0.34% Codfish 0.011% Dogfish 0.28%Tuna 0.023% (% w/w of bones) | √ | - | [32] |
| Silver-banded whiting | Head | Lyase | Ethanol, NaCl, NaOH, | SEC, HPLC, NMR | 70:20% and 50:30%, | √ | HA | [35] |
| Salmo salar fish | Collagen-based scaffolds | Papain | Acetone, Sodium acetate, ethanol | Spectrophotometry | 5% | √ | - | [31] |
| Labeo rohita Piaractus brachypomus | Head | Papain | Acetone, TCA, ethanol, K-acetate | reverse-phase HPLC. | √ | DS | [17] |
| Fish Species | Char. of CS | Exp. Type (Model) | Dose and Admin. | Exp. Cond. | Pharmacology | Key Results | Ref. |
|---|---|---|---|---|---|---|---|
| Tilapia (Oreochromis niloticus) viscera | 4-sulfated CS (59.6%); 6-sulfated CS (36.6%); Non-sulfated CS (3.4%) | In vitro (chemical analysis) | 20, 40, 100, and 200 µg/mL | 37 °C; 24 h | Antioxidant | ↓ ROS (p < 0.01) highest level at 40 µg/mL | [116] |
| Nile tilapia (Oreochromis niloticus) viscera | CS-rich GAGs; Yield (0.15% of the freeze-dried sample) | In vitro (aPTT) | 0.25 mg/mL | 37 °C; 1 min | Anticoagulant | The Nile tilapia increased normal clotting time (2.3–2.8). The Pacu increased normal coagulation time (1.5–2.4) | [33] |
| Pacu (Piaractus mesopotamicus) viscera | CS-rich GAGs; Yield (0.158 of the dry sample) | ||||||
| Grey triggerfish skins (GTCS) | Purity (99.2%); 41.72 kDa; 4-sulfated CS (59%); 6-sulfated CS (18.2%); Non-sulfated CS (3.5%) | In vitro (HCT116 cells) | 10–200 µg/mL | 1 × 107 cells/mL; 37 °C; 24 h | Anticancer | ↓ 70.6% for GTCS and 72.65% for SHCS (p < 0.05) at 200 µg/mL; No hemolysis; No cytotoxicity against the normal lymphocytes | [117] |
| Smooth hound skins (SHCS) | Purity (95.4%); 23.8 kDa; 4-sulfated CS (47%); 6-sulfated CS (14.6%); Non-sulfated CS (5.5%) | ||||||
| Salmon cartilage | 4-sulfated CS (30–40%); 6-sulfated CS (50–60%) | In vitro (Chemical analysis) | 1, 2, 5, 10, 20 mg/mL | Chelating with divalent metal ions, Ca2+, Mg2+, Mn2+, or Zn2+ | Antioxidant | Sulfated CS has significant antioxidant potency; CS chelation with Ca2+ or Mg2+ remarkably increased SOD radical scavenging; and CS chelation with Ca2+, Mg2+, Mn2+, or Zn2+ increased hydroxyl radical scavenging | [118] |
| Shark cartilage | 4-sulfated CS (30%); 6-sulfated CS (40%) | ||||||
| Ray cartilage | HMWCS; 6-sulfated CS (61.9%); 4-sulfated CS (27.0%); 2-sulfated CS-6-sulfated CS (8.5%); 142 kDa | In vitro (Hippocampal cells from E16 mice) | 2 μg/well | 2 × 104 cells/cm2; 37 °C; 24 h | Neuritogenic activity | ↑ Neurite outgrowth through the HGF signaling pathway; Specific binding of HGF to the CS | [119] |
| Skate (Raja pulchra) | HMWCS | In vitro and | 5 or 50 mg/ml | 37 °C; 10 or 30 min | Anti-obesity | Ø Pancreatic lipase activity; Ø Proliferation and lipid accumulation in mature adipocytes; HMWCS has greater lipase inhibitory activity than LMWCS; | [120] |
| In vitro (mouse 3T3-L1) | Various concentrations and time points | 37 °C; 15 min | |||||
| In vivo (C57B/6 J mice; male; 4w) | 50 mg/5 mL/kg/day; orally | 8 w | |||||
| Skate cartilage | CSE, CS | In vivo (Mice) | 200, 400 mg/kg; orally | 3 consecutive days | Antiinflammation, hepatic dyslipidemia | ↑ Hepatic antioxidant enzyme expression levels; Ø Inflammatory factors; ↓ Serum lipid; ↓ hepatic sterol regulatory element-binding proteins expression; ↓ MAPK; and ↓ Apoptopic factors | [121] |
| Sturgeon cartilage | AMWCS; 4-sulfated CS (88.8%); 8 kDa | In vitro (Fibroblast) | 100 µg/ml | 1 × 103 cells/well; 37 °C; 24 h | Wound healing | ↑ cell adhesion; ↑ Proliferation and migration on fibroblasts; and ↑ MAPK signaling pathways | [122] |
| Sturgeon backbone | AMWCS; 6-sulfated CS (60%); 43 kDa | ||||||
| Sturgeon skull | AMWCS; non-sulfated CS (74.2%); 38.5 kDa | In vitro (Rabbit blood) | 1, 3, 5 mg/ml | 360 µL of platelet-poor plasma; 15 min | Anticoagulant, anti-platelet, and thrombolysis | ↑ aPTT; ↑ TT; Ø Platelet aggregation; Dissolved platelet plasma clots; Sturgeon backbone CS was stronger than sturgeon skull CS | [123] |
| Sturgeon backbone | AMWCS; 4-sulfated CS (37.8%); 6-sulfated CS (59.6%); 49.2 kDa | ||||||
| Shark cartilage | LMWCS (75.7%); 3.9 kDa | In vitro (PC12; SH-SY5Y) | 50, 100, 200 µg/ml | 0.5 × 104 cells/well; 24 h | Neuroprotection | × Cell viability loss and apoptosis; ↓ Intracellular Ca; ↓ ROS levels; ↓ MMP depolarization; and ↓ Protein expression of Caspase-3 | [124] |
| Shark cartilage | LMWCS (75.7%); 3.9 kDa | In vivo (Male Balb/c mice; 8 w) | 50, 150, 450 mg/kg; perorally (p.o.) | Daily; 31 days | Neuroprotection | Improved the cognitive impairment; ↑ ChAT level; ↑ SOD; and ↑ GSH-Px; ↓ MDA level; and ↓ AChE level; ↓ Pyramidal cells of CA1 regions; Ø Protein expression of Bax/Bcl-2 and Caspase3, -9. | [124] |
| Small sea fish | CS Extracts (CP) | In vitro (CHON-001) | CP 0.2%, 0.3% (v/v in culture medium); CS 3, 200 µg/mL | 48, 72 h | Osteoarthritis | × Chondrocytes decline; Ø Osteo-articular inflammation Ø Apoptosis; and ↑ Proliferation rate | [125] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Urbi, Z.; Azmi, N.S.; Ming, L.C.; Hossain, M.S. A Concise Review of Extraction and Characterization of Chondroitin Sulphate from Fish and Fish Wastes for Pharmacological Application. Curr. Issues Mol. Biol. 2022, 44, 3905-3922. https://doi.org/10.3390/cimb44090268
Urbi Z, Azmi NS, Ming LC, Hossain MS. A Concise Review of Extraction and Characterization of Chondroitin Sulphate from Fish and Fish Wastes for Pharmacological Application. Current Issues in Molecular Biology. 2022; 44(9):3905-3922. https://doi.org/10.3390/cimb44090268
Chicago/Turabian StyleUrbi, Zannat, Nina Suhaity Azmi, Long Chiau Ming, and Md. Sanower Hossain. 2022. "A Concise Review of Extraction and Characterization of Chondroitin Sulphate from Fish and Fish Wastes for Pharmacological Application" Current Issues in Molecular Biology 44, no. 9: 3905-3922. https://doi.org/10.3390/cimb44090268
APA StyleUrbi, Z., Azmi, N. S., Ming, L. C., & Hossain, M. S. (2022). A Concise Review of Extraction and Characterization of Chondroitin Sulphate from Fish and Fish Wastes for Pharmacological Application. Current Issues in Molecular Biology, 44(9), 3905-3922. https://doi.org/10.3390/cimb44090268








