In Silico Design of Dual-Binding Site Anti-Cholinesterase Phytochemical Heterodimers as Treatment Options for Alzheimer’s Disease
Abstract
:1. Introduction
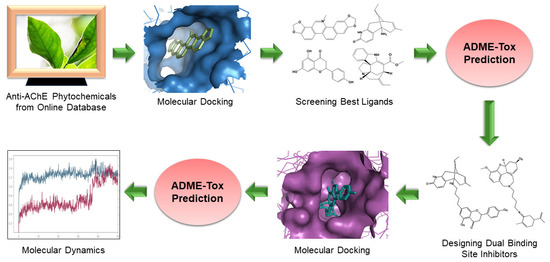
2. Materials and Methods
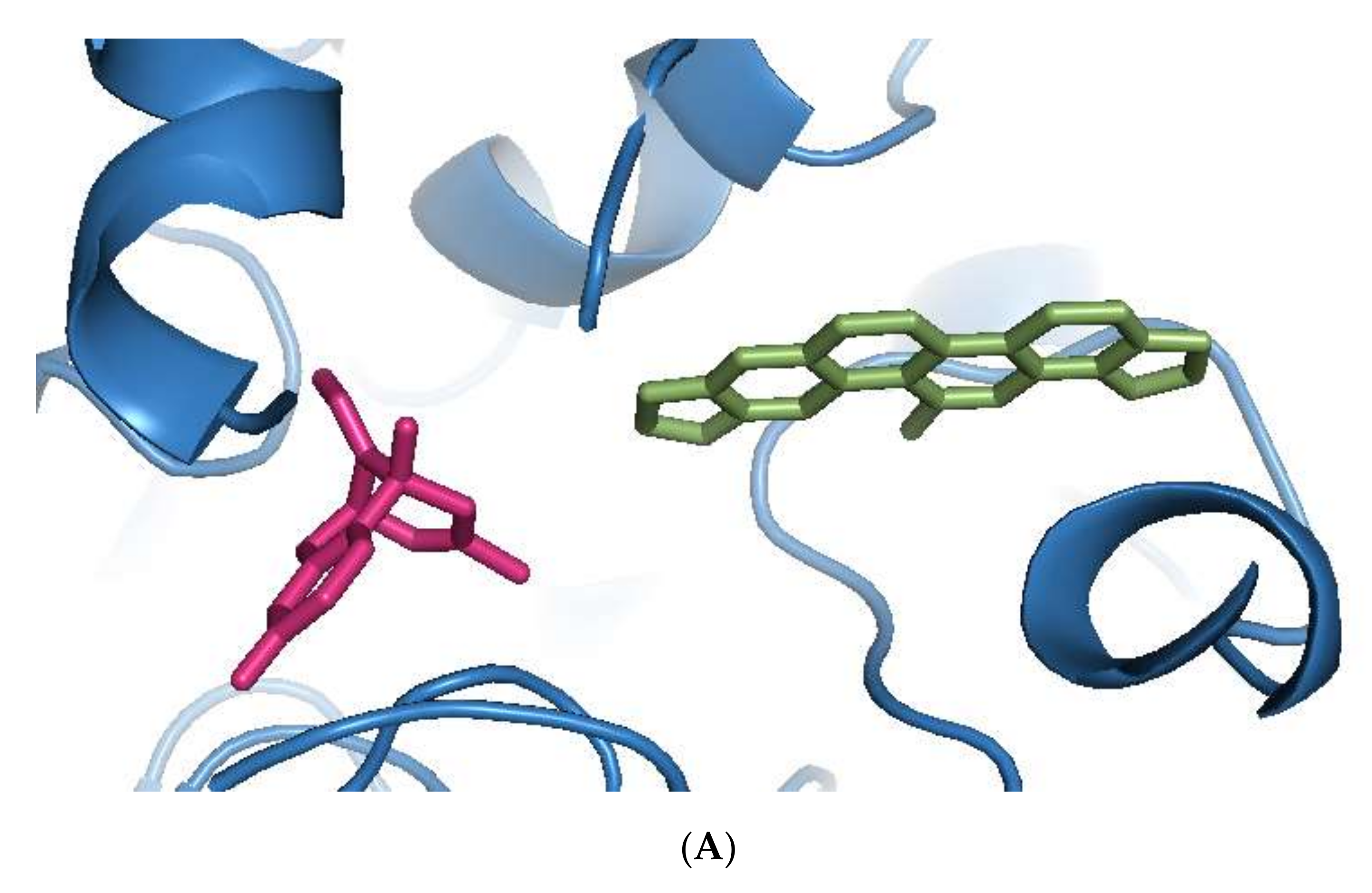
2.1. Screening and Molecular Docking of Phytochemicals
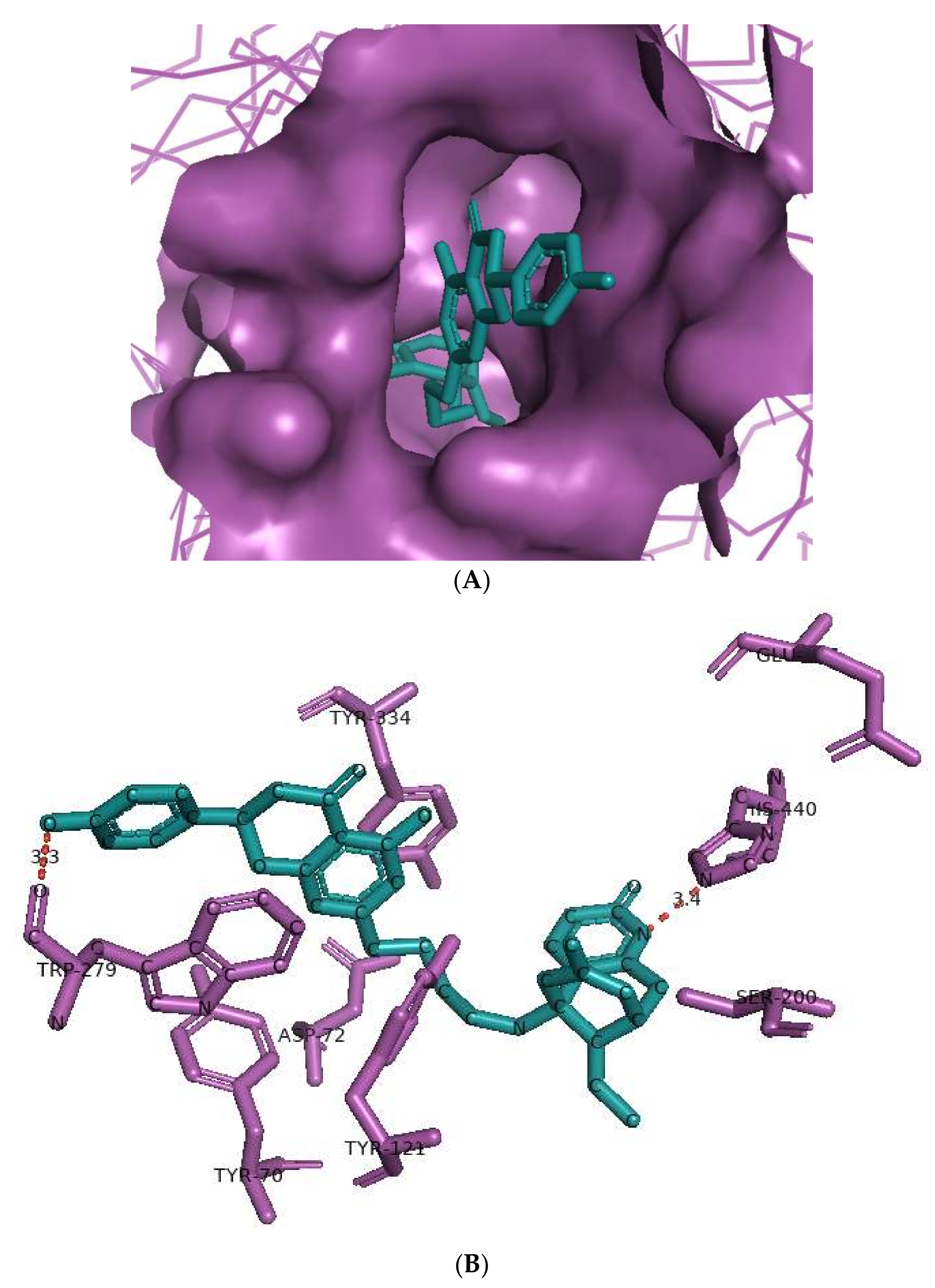
2.2. Design and Molecular Docking of Heterodimeric Ligands
2.3. Pharmacokinetic Predictions
2.4. Pharmacodynamic Predictions
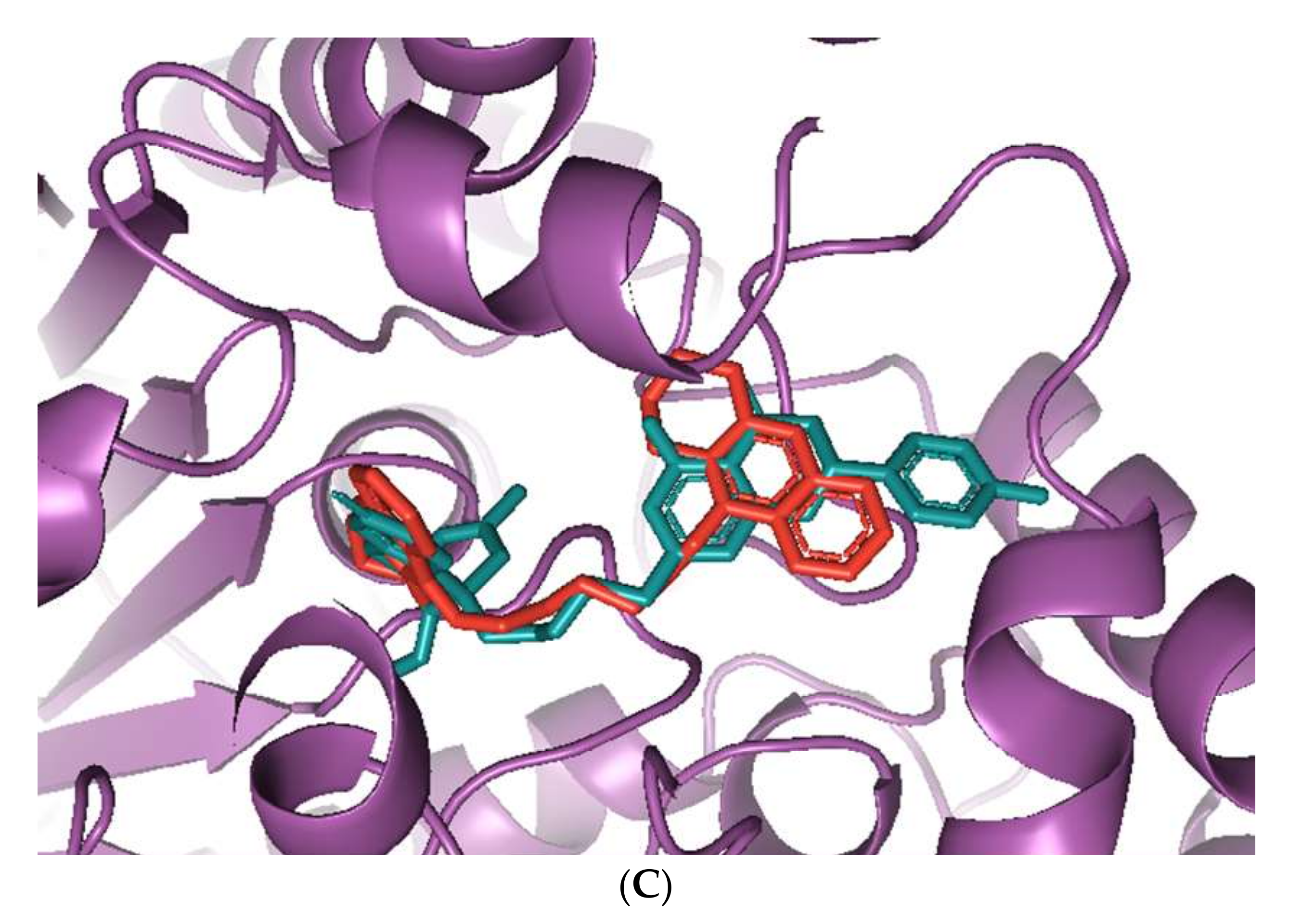
2.5. Molecular Dynamics Simulations
3. Results
3.1. Screening of Anti-AChE Phytochemical Ligands
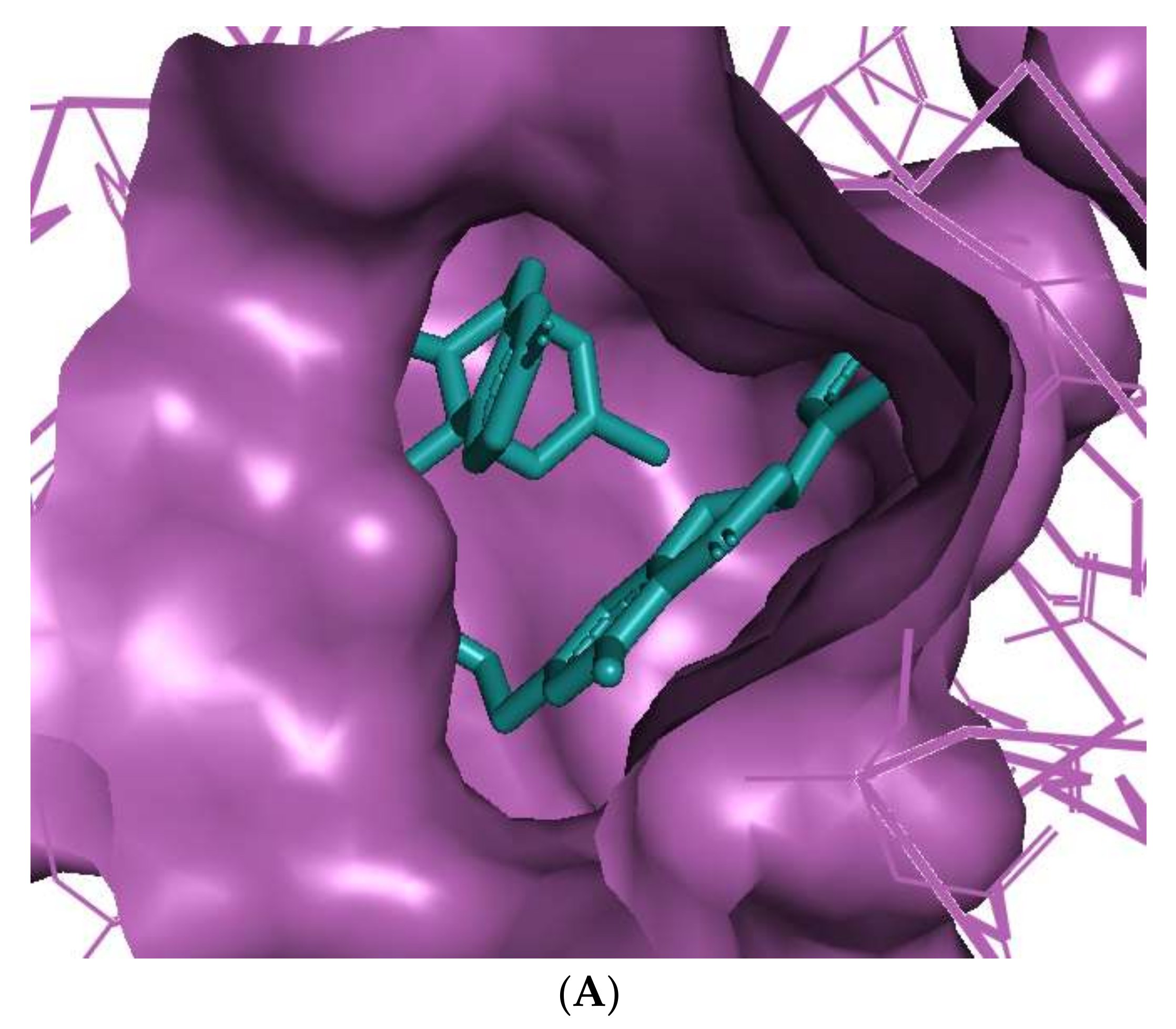
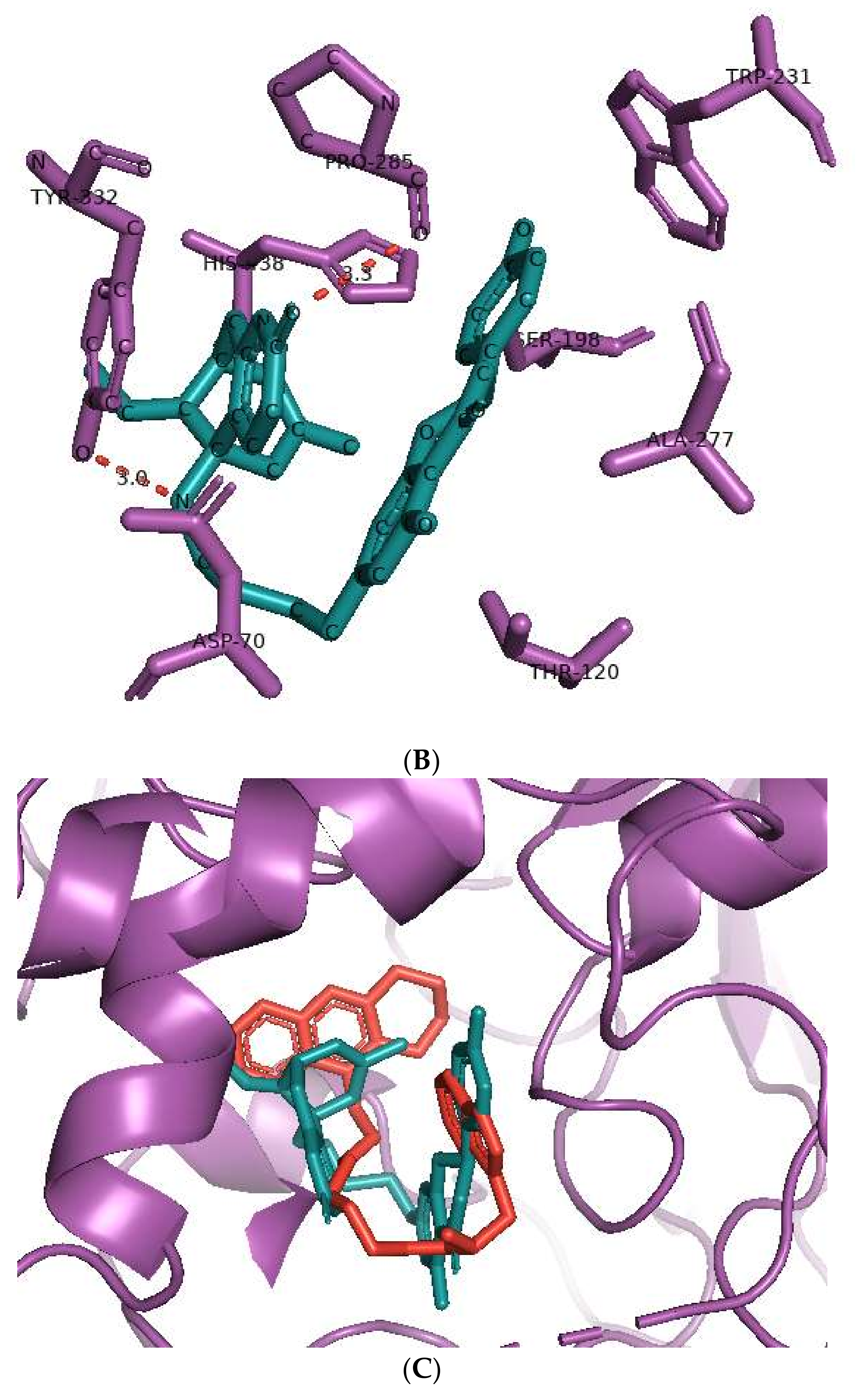
3.2. Molecular Docking of Heterodimeric Ligands
3.3. ADME Prediction
3.4. Toxicity Prediction
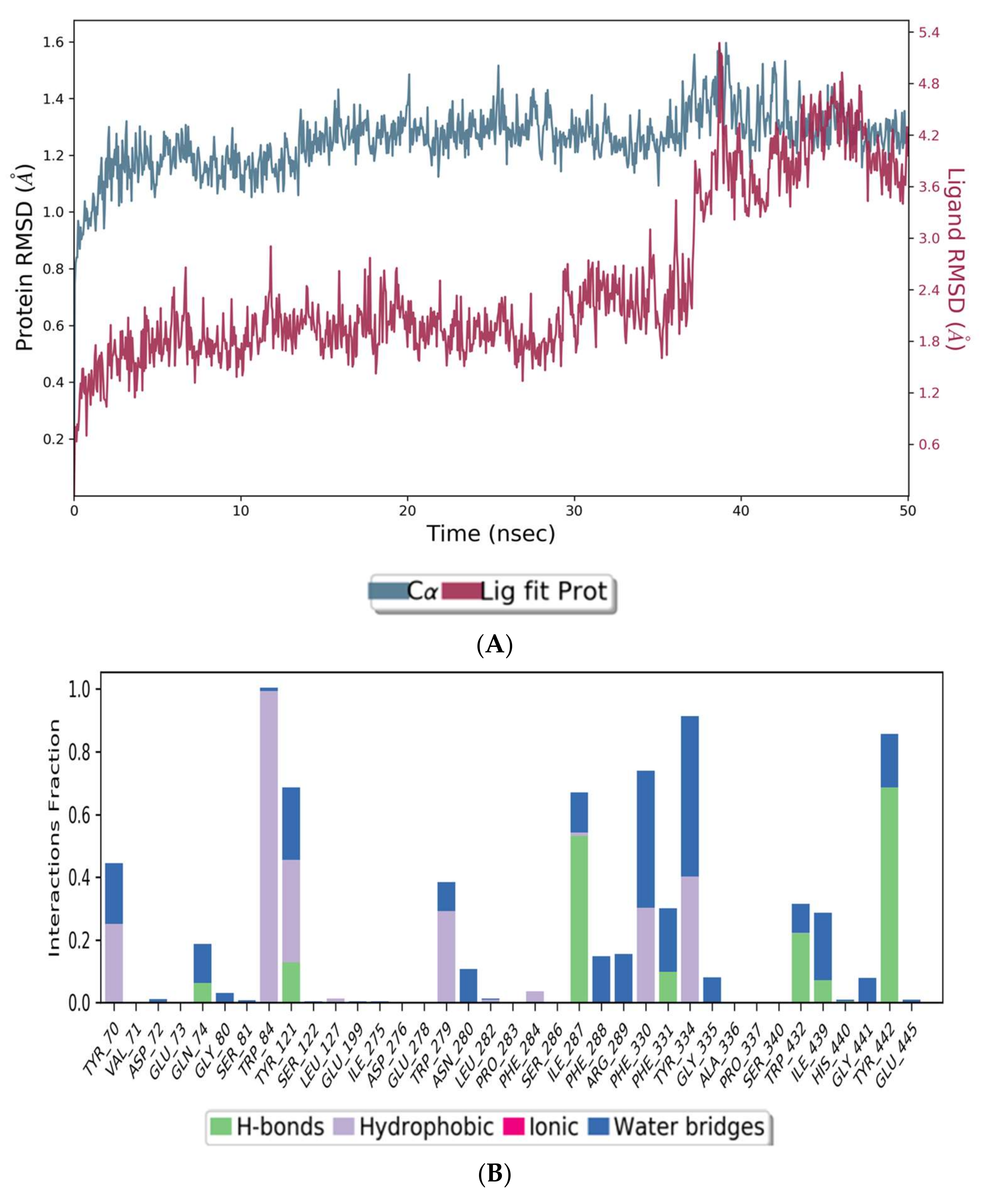
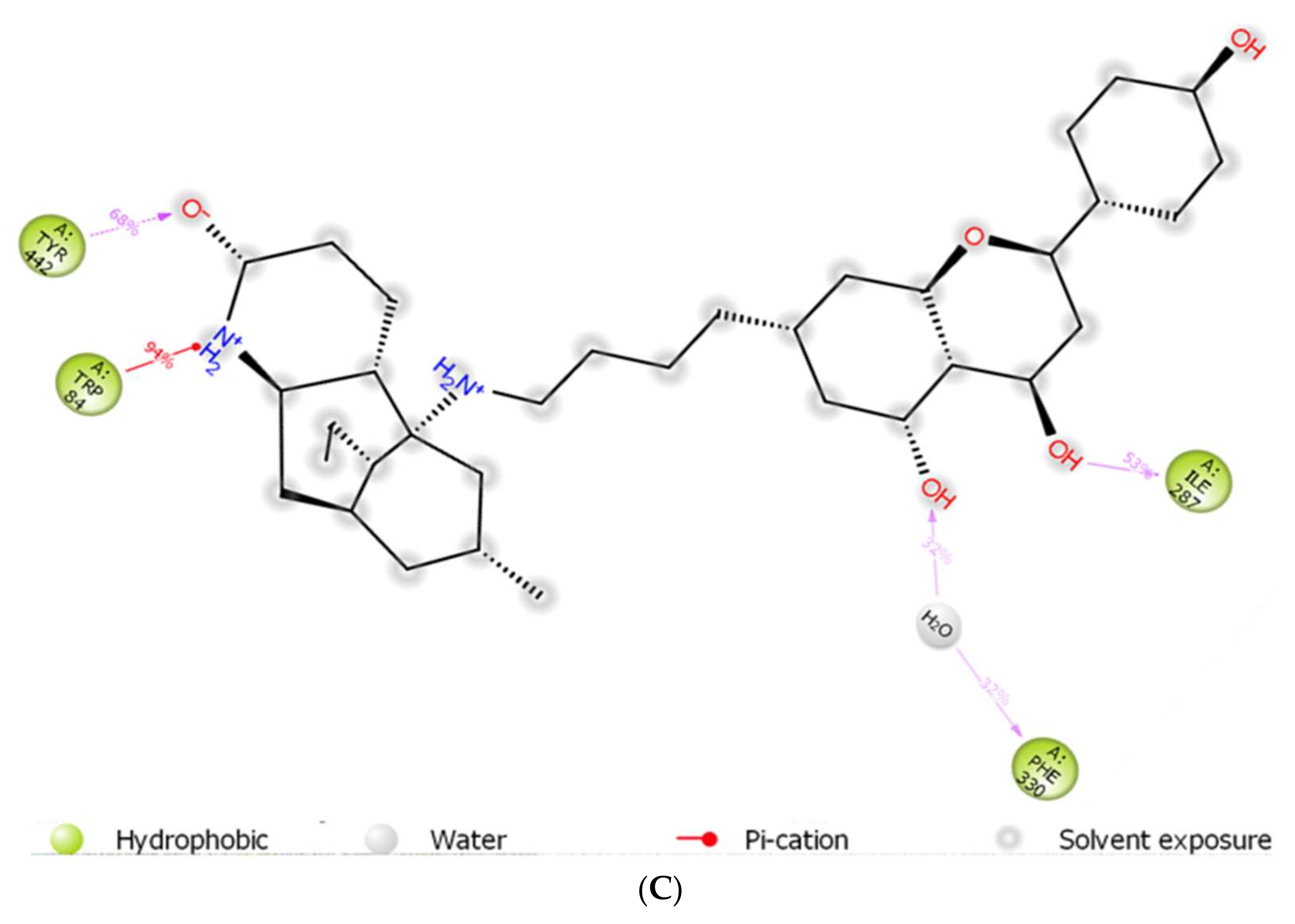
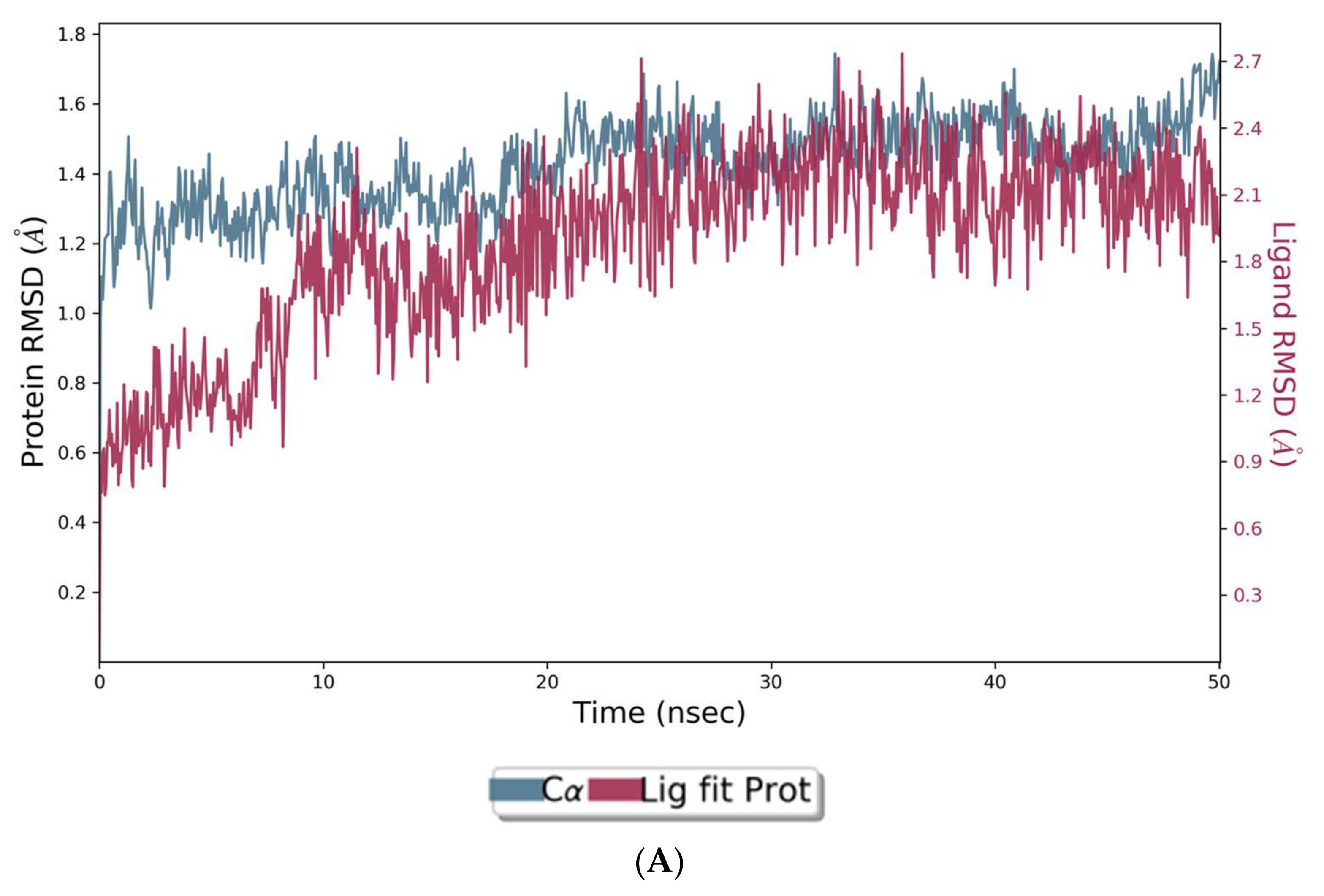
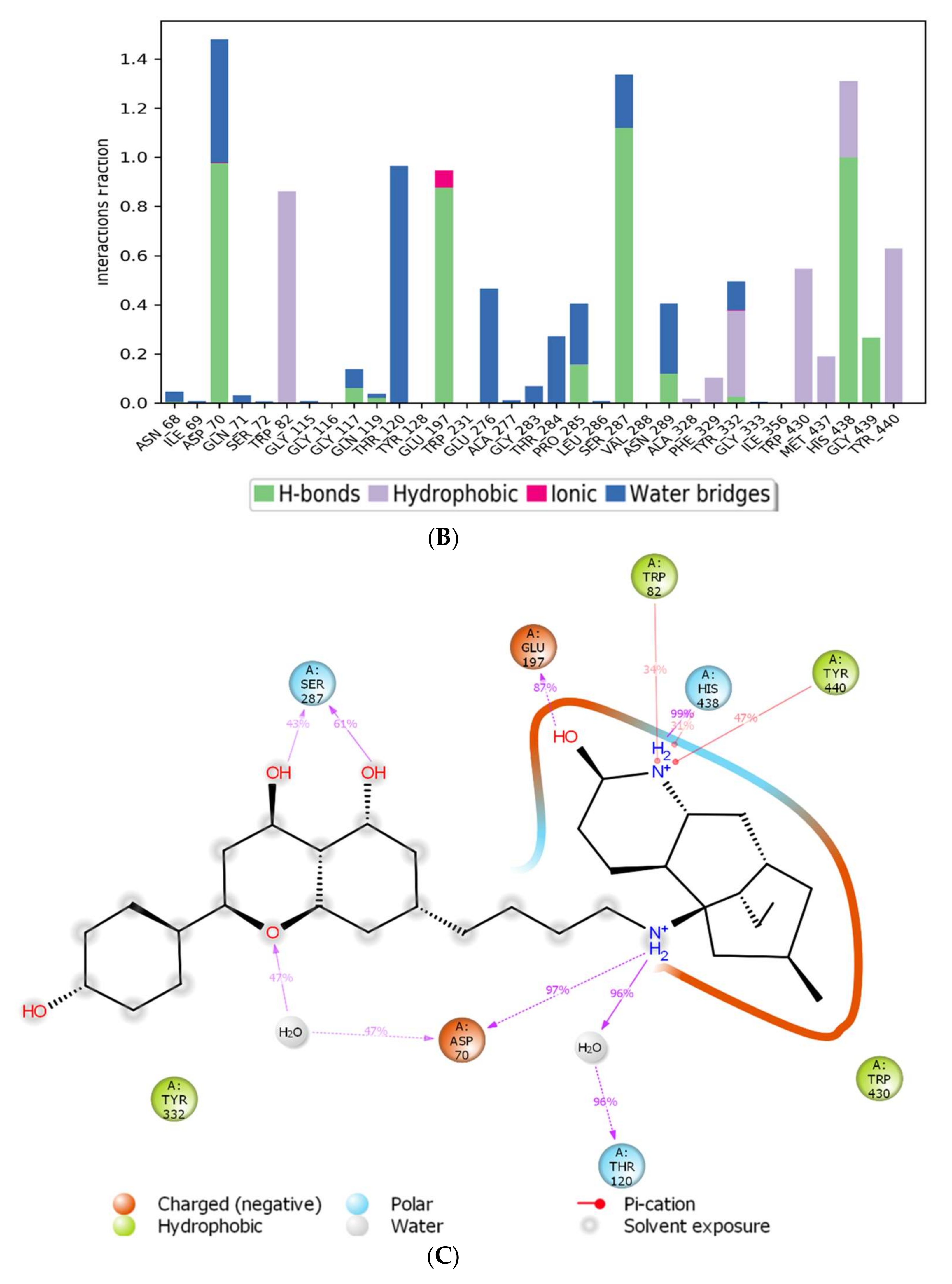
3.5. Molecular Dynamic Simulations
4. Discussion
Summary and Study Limitations
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- World Health Organization (WHO). Global Action Plan on the Public Health Response to Dementia 2017–2025. Available online: https://www.who.int/news-room/fact-sheets/detail/dementia (accessed on 28 November 2021).
- Kumfor, F.; Halliday, G.M.; Piguet, O. Clinical Aspects of Alzheimer’s Disease. In Neurodegenerative Diseases. Advances in Neurobiology; Beart, P., Robinson, M., Rattray, M., Maragakis, N., Eds.; Springer: Cham, Switzerland, 2017; Volume 15. [Google Scholar] [CrossRef]
- Grossberg, G.T. Cholinesterase Inhibitors for the Treatment of Alzheimer’s Disease: Getting On and Staying On. Curr. Ther. Res. 2003, 64, 216–235. [Google Scholar] [CrossRef] [Green Version]
- Birks, J.S. Cholinesterase inhibitors for Alzheimer’s disease. Cochrane Database Syst. Rev. 2006, 1, CD005593. [Google Scholar] [CrossRef]
- Du, X.; Wang, X.; Geng, M. Alzheimer’s disease hypothesis and related therapies. Transl. Neurodegener. 2018, 7, 1–7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mesulama, M.; Guillozetb, A.; Shaw, P.; Quinnc, B. Widely Spread Butyrylcholinesterase Can Hydrolyze Acetylcholine in the Normal and Alzheimer Brain. Neurobiol. Dis. 2002, 9, 88–93. [Google Scholar] [CrossRef] [PubMed]
- Arendt, T.; Brückner, M.K.; Lange, M.; Bigl, V. Changes in acetylcholinesterase and butyrylcholinesterase in Alzheimer’s disease resemble embryonic development—A study of molecular forms. Neurochem. Int. 1992, 21, 381–396. [Google Scholar] [CrossRef]
- Reinikainen, K.J.; Riekkinen, P.J.; Soininen, H.; Helkala, E.-L.; Jolkkonen, J.; Laakso, M. Cholinergic deficit in Alzheimer’s disease: A study based on CSF and autopsy data. Neurochem. Res. 1988, 13, 135–146. [Google Scholar] [CrossRef]
- Mushtaq, G.; Greig, N.H.; Khan, J.; Kamal, M.A. Status of Acetylcholinesterase and Butyrylcholinesterase in Alzheimer’s Disease and Type 2 Diabetes Mellitus. CNS Neurol. Disord. Drug Targets 2014, 13, 1432–1439. [Google Scholar] [CrossRef]
- Giacobini, E. Selective Inhibitors of Butyrylcholinesterase. Drugs Aging 2001, 18, 891–898. [Google Scholar] [CrossRef] [PubMed]
- Nordberg, A.; Ballard, C.; Bullock, R.; Darreh-Shori, T.; Somogyi, M. A Review of Butyrylcholinesterase as a Therapeutic Target in the Treatment of Alzheimer’s Disease. Prim. Care Companion CNS Disord. 2013, 15, 12r01412. [Google Scholar] [CrossRef]
- Green, C.; Picot, J.; Loveman, E.; Takeda, A.; Kirby, J.; Clegg, A. Modelling the cost effectiveness of cholinesterase inhibitors in the management of mild to moderately severe Alzheimer’s disease. Pharmacoeconomics 2005, 23, 1271–1282. [Google Scholar] [CrossRef]
- Xu, H.; Garcia-Ptacek, S.; Jönsson, L.; Wimo, A.; Nordström, P.; Eriksdotter, M. Long-term Effects of Cholinesterase Inhibitors on Cognitive Decline and Mortality. Neurology 2021, 96, e2220–e2230. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, F.; Ghalib, R.; Sasikala, P.; Ahmed, K.M. Cholinesterase inhibitors from botanicals. Pharmacogn. Rev. 2013, 7, 121–130. [Google Scholar] [CrossRef] [Green Version]
- Nwidu, L.L.; Elmorsy, E.; Thornton, J.; Wijamunige, B.; Wijesekara, A.; Tarbox, R.; Warren, A.; Carter, W.G. Anti-acetylcholinesterase activity and antioxidant properties of extracts and fractions of Carpolobia lutea. Pharm. Biol. 2017, 55, 1875–1883. [Google Scholar] [CrossRef] [Green Version]
- Nwidu, L.L.; Elmorsy, E.; Aprioku, J.S.; Siminialayi, I.; Carter, W.G. In Vitro Anti-Cholinesterase and Antioxidant Activity of Extracts of Moringa oleifera Plants from Rivers State, Niger Delta, Nigeria. Medicines 2018, 5, 71. [Google Scholar] [CrossRef] [Green Version]
- Jabir, N.R.; Khan, F.; Tabrez, S. Cholinesterase targeting by polyphenols: A therapeutic approach for the treatment of Alzheimer’s disease. CNS Neurosci. Ther. 2018, 24, 753–762. [Google Scholar] [CrossRef]
- Amat-Ur-Rasool, H.; Symes, F.; Tooth, D.; Schaffert, L.-N.; Elmorsy, E.; Ahmed, M.; Hasnain, S.; Carter, W.G. Potential Nutraceutical Properties of Leaves from Several Commonly Cultivated Plants. Biomolecules 2020, 10, 1556. [Google Scholar] [CrossRef] [PubMed]
- Tang, X.C.; Han, Y.F. Pharmacological Profile of Huperzine A, a Novel Acetylcholinesterase Inhibitor from Chinese Herb. CNS Drug Rev. 2006, 5, 281–300. [Google Scholar] [CrossRef] [Green Version]
- Wang, B.-S.; Wang, H.; Wei, Z.-H.; Song, Y.-Y.; Zhang, L.; Chen, H.-Z. Efficacy and safety of natural acetylcholinesterase inhibitor huperzine A in the treatment of Alzheimer’s disease: An updated meta-analysis. J. Neural Transm. 2009, 116, 457–465. [Google Scholar] [CrossRef] [PubMed]
- Yang, G.; Wang, Y.; Tian, J.; Liu, J.-P. Huperzine A for Alzheimer’s Disease: A Systematic Review and Meta-Analysis of Randomized Clinical Trials. PLoS ONE 2013, 8, e74916. [Google Scholar] [CrossRef] [Green Version]
- Neergheen-Bhujun, V.S. Underestimating the Toxicological Challenges Associated with the Use of Herbal Medicinal Products in Developing Countries. BioMed Res. Int. 2013, 2013, 804086. [Google Scholar] [CrossRef] [Green Version]
- Dvir, H.; Silman, I.; Harel, M.; Rosenberry, T.L.; Sussman, J.L. Acetylcholinesterase: From 3D structure to function. Chem. Interact. 2010, 187, 10–22. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rosenberry, T.L. Strategies to Resolve the Catalytic Mechanism of Acetylcholinesterase. J. Mol. Neurosci. 2009, 40, 32–39. [Google Scholar] [CrossRef]
- Bajda, M.; Więckowska, A.; Hebda, M.; Guzior, N.; Sotriffer, C.A.; Malawska, B. Structure-Based Search for New Inhibitors of Cholinesterases. Int. J. Mol. Sci. 2013, 14, 5608–5632. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Silva, M.A.; Kiametis, A.S.; Treptow, W. Donepezil Inhibits Acetylcholinesterase via Multiple Binding Modes at Room Temperature. J. Chem. Inf. Model. 2020, 60, 3463–3471. [Google Scholar] [CrossRef]
- Castro, A. Peripheral and Dual Binding Site Acetylcholinesterase Inhibitors: Implications in treatment of Alzheimer’s Disease. Mini-Rev. Med. Chem. 2001, 1, 267–272. [Google Scholar] [CrossRef]
- Camps, P.; Formosa, X.; Galdeano, C.; Gómez, T.; Muñoz-Torrero, D.; Scarpellini, M.; Viayna, E.; Badia, A.; Clos, M.V.; Camins, A.; et al. Novel Donepezil-Based Inhibitors of Acetyl- and Butyrylcholinesterase and Acetylcholinesterase-Induced β-Amyloid Aggregation. J. Med. Chem. 2008, 51, 3588–3598. [Google Scholar] [CrossRef] [PubMed]
- Amat-Ur-Rasool, H.; Ahmed, M. Designing Second Generation Anti-Alzheimer Compounds as Inhibitors of Human Acetylcholinesterase: Computational Screening of Synthetic Molecules and Dietary Phytochemicals. PLoS ONE 2015, 10, e0136509. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, S.; Iftikhar, F.; Ullah, F.; Sadiq, A.; Rashid, U. Rational design and synthesis of dihydropyrimidine based dual binding site acetylcholinesterase inhibitors. Bioorgan. Chem. 2016, 69, 91–101. [Google Scholar] [CrossRef]
- Tanoli, S.T.; Ramzan, M.; Hassan, A.; Sadiq, A.; Jan, M.S.; Khan, F.A.; Ullah, F.; Ahmad, H.; Bibi, M.; Mahmood, T.; et al. Design, synthesis and bioevaluation of tricyclic fused ring system as dual binding site acetylcholinesterase inhibitors. Bioorgan. Chem. 2018, 83, 336–347. [Google Scholar] [CrossRef]
- Zueva, I.; Dias, J.; Lushchekina, S.; Semenov, V.; Mukhamedyarov, M.; Pashirova, T.; Babaev, V.; Nachon, F.; Petrova, N.; Nurullin, L.; et al. New evidence for dual binding site inhibitors of acetylcholinesterase as improved drugs for treatment of Alzheimer’s disease. Neuropharmacology 2019, 155, 131–141. [Google Scholar] [CrossRef]
- Mak, S.; Li, W.; Fu, H.; Luo, J.; Cui, W.; Hu, S.; Pang, Y.; Carlier, P.R.; Tsim, K.W.; Pi, R.; et al. Promising tacrine/huperzine Abased dimeric acetylcholinesterase inhibitors for neurodegenerative disorders: From relieving symptoms to modifying diseases through multitarget. J. Neurochem. 2021, 158, 1381–1393. [Google Scholar] [CrossRef] [PubMed]
- Shan, W.-J.; Huang, L.; Zhou, Q.; Meng, F.-C.; Li, X.-S. Synthesis, biological evaluation of 9-N-substituted berberine derivatives as multi-functional agents of antioxidant, inhibitors of acetylcholinesterase, butyrylcholinesterase and amyloid-β aggregation. Eur. J. Med. Chem. 2011, 46, 5885–5893. [Google Scholar] [CrossRef] [PubMed]
- Viayna, E.; Sabate, R.; Muñoz-Torrero, D. Dual Inhibitors of β-Amyloid Aggregation and Acetylcholinesterase as Multi-Target Anti-Alzheimer Drug Candidates. Curr. Top. Med. Chem. 2013, 13, 1820–1842. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schaffert, L.-N.; Carter, W.G. Do Post-Translational Modifications Influence Protein Aggregation in Neurodegenerative Diseases: A Systematic Review. Brain Sci. 2020, 10, 232. [Google Scholar] [CrossRef] [PubMed]
- Brunhofer, G.; Fallarero, A.; Karlsson, D.; Batista-Gonzalez, A.; Shinde, P.; Mohan, C.G.; Vuorela, P. Exploration of natural compounds as sources of new bifunctional scaffolds targeting cholinesterases and beta amyloid aggregation: The case of chelerythrine. Bioorgan. Med. Chem. 2012, 20, 6669–6679. [Google Scholar] [CrossRef]
- Sharma, K. Cholinesterase inhibitors as Alzheimer’s therapeutics (Review). Mol. Med. Rep. 2019, 20, 1479–1487. [Google Scholar] [CrossRef] [Green Version]
- U.S. Department of Agriculture. Agricultural Research Service. 1992–2016. Dr. Duke’s Phytochemical and Ethnobotanical Databases. Available online: http://phytochem.nal.usda.gov/ (accessed on 25 September 2021).
- Mendelsohn, L.D. ChemDraw 8 Ultra, Windows and Macintosh Versions. J. Chem. Inf. Comput. Sci. 2004, 44, 2225–2226. [Google Scholar] [CrossRef]
- Daina, A.; Michielin, O.; Zoete, V. SwissADME: A free web tool to evaluate pharmacokinetics, drug-likeness and medicinal chemistry friendliness of small molecules. Sci. Rep. 2017, 7, 42717. [Google Scholar] [CrossRef] [Green Version]
- Banerjee, P.; Eckert, A.O.; Schrey, A.K.; Preissner, R. ProTox-II: A webserver for the prediction of toxicity of chemicals. Nucleic Acids Res. 2018, 46, W257–W263. [Google Scholar] [CrossRef] [Green Version]
- Desmond Molecular Dynamics System. D.E. Shaw Research. In Maestro-Desmond Interoperability Tools; Schrödinger: New York, NY, USA, 2021; Available online: https://www.schrodinger.com/products/desmond (accessed on 10 December 2021).
- Cheung, J.; Rudolph, M.J.; Burshteyn, F.; Cassidy, M.S.; Gary, E.N.; Love, J.; Franklin, M.C.; Height, J.J. Structures of Human Acetylcholinesterase in Complex with Pharmacologically Important Ligands. J. Med. Chem. 2012, 55, 10282–10286. [Google Scholar] [CrossRef]
- Pajouhesh, H.; Lenz, G.R. Medicinal chemical properties of successful central nervous system drugs. NeuroRX 2005, 2, 541–553. [Google Scholar] [CrossRef] [Green Version]
- Rydberg, E.H.; Brumshtein, B.; Greenblatt, H.M.; Wong, D.M.; Shaya, D.; Williams, L.D.; Carlier, P.R.; Pang, Y.-P.; Silman, I.; Sussman, J.L. Complexes of Alkylene-linked Tacrine dimers with Torpedo californica acetylcholinesterase: Binding of Bis (5)-tacrine produces a dramatic rearrangement in the active-site gorge. J. Med. Chem. 2006, 49, 5491–5500. [Google Scholar] [CrossRef]
- Chalupova, K.; Korabecny, J.; Bartolini, M.; Monti, B.; Lamba, D.; Caliandro, R.; Pesaresi, A.; Brazzolotto, X.; Gastellier, A.-J.; Nachon, F.; et al. Novel tacrine-tryptophan hybrids: Multi-target directed ligands as potential treatment for Alzheimer’s disease. Eur. J. Med. Chem. 2019, 168, 491–514. [Google Scholar] [CrossRef]
- Shultz, M.D. Two Decades under the Influence of the Rule of Five and the Changing Properties of Approved Oral Drugs. J. Med. Chem. 2019, 62, 1701–1714. [Google Scholar] [CrossRef] [PubMed]
- Benek, O.; Korabecny, J.; Soukup, O. A Perspective on Multi-target Drugs for Alzheimer’s Disease. Trends Pharmacol. Sci. 2020, 41, 434–445. [Google Scholar] [CrossRef] [PubMed]
- Kabir, M.T.; Uddin, M.S.; Mamun, A.A.; Jeandet, P.; Aleya, L.; Mansouri, R.A.; Ashraf, G.M.; Mathew, B.; Bin-Jumah, M.N.; Abdel-Daim, M.M. Combination Drug Therapy for the Management of Alzheimer’s Disease. Int. J. Mol. Sci. 2020, 21, 3272. [Google Scholar] [CrossRef]
- Amat-Ur-Rasool, H.; Ahmed, M.; Hasnain, S.; Carter, W.G. Anti-Cholinesterase Combination Drug Therapy as a Potential Treatment for Alzheimer’s Disease. Brain Sci. 2021, 11, 184. [Google Scholar] [CrossRef] [PubMed]
- Cacabelos, R. Donepezil in Alzheimer’s disease: From conventional trials to pharmacogenetics. Neuropsychiatr. Dis. Treat. 2007, 3, 303–333. [Google Scholar]
- Wang, R.; Yan, H.; Tang, X.-C. Progress in studies of huperzine A, a natural cholinesterase inhibitor from Chinese herbal medicine. Acta Pharmacol. Sin. 2006, 27, 1–26. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ha, G.T.; Wong, R.K.; Zhang, Y. Huperzine A as Potential Treatment of Alzheimer’s Disease: An assessment on chemistry, pharmacology, and clinical studies. Chem. Biodivers. 2011, 8, 1189–1204. [Google Scholar] [CrossRef]
- Alam, M.A.; Subhan, N.; Rahman, M.M.; Uddin, S.J.; Reza, H.M.; Sarker, S.D. Effect of citrus flavonoids, naringin and naringenin, on metabolic syndrome and their mechanisms of action. Adv. Nutr. 2014, 5, 404–417. [Google Scholar] [CrossRef]
- Salehi, B.; Fokou, P.V.T.; Sharifi-Rad, M.; Zucca, P.; Pezzani, R.; Martins, N.; Sharifi-Rad, J. The Therapeutic Potential of Naringenin: A Review of Clinical Trials. Pharmaceuticals 2019, 12, 11. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Heo, H.J.; Kim, M.-J.; Lee, J.-M.; Choi, S.J.; Cho, H.-Y.; Hong, B.; Kim, H.-K.; Kim, E.; Shin, D.-H. Naringenin from Citrus junos Has an Inhibitory Effect on Acetylcholinesterase and a Mitigating Effect on Amnesia. Dement. Geriatr. Cogn. Disord. 2004, 17, 151–157. [Google Scholar] [CrossRef]
- Rahigude, A.; Bhutada, P.; Kaulaskar, S.; Aswar, M.; Otari, K. Participation of antioxidant and cholinergic system in protective effect of naringenin against type-2 diabetes-induced memory dysfunction in rats. Neuroscience 2012, 226, 62–72. [Google Scholar] [CrossRef] [PubMed]
- Umukoro, S.; Kalejaye, H.A.; Ben-Azu, B.; Ajayi, A.M. Naringenin attenuates behavioral derangements induced by social defeat stress in mice via inhibition of acetylcholinesterase activity, oxidative stress and release of pro-inflammatory cytokines. Biomed. Pharmacother. 2018, 105, 714–723. [Google Scholar] [CrossRef]
- Liu, M.-Y.; Zeng, F.; Shen, Y.; Wang, Y.-Y.; Zhang, N.; Geng, F. Bioguided isolation and structure identification of acetylcholinesterase enzyme inhibitors from Drynariae Rhizome. J. Anal. Methods Chem. 2020, 2020, 2971841–2971849. [Google Scholar] [CrossRef] [PubMed]
- Lopez, M.D.; Pascual-Villalobos, M.J. Are monoterpenoids and phenylpropanoids efficient inhibitors of acetylcholinesterase from stored product insect strains? Flavour Fragr. J. 2015, 30, 108–112. [Google Scholar] [CrossRef]
- Tam, S.W.; Worcel, M.; Wyllie, M. Yohimbine: A clinical review. Pharmacol. Ther. 2001, 91, 215–243. [Google Scholar] [CrossRef]
- Orhan, I.; Naz, Q.; Kartal, M.; Tosun, F.; Şener, B. In vitro anticholinesterase activity of various alkaloids. Z. Naturforsch. C. J. Biosci. 2007, 62, 684–688. [Google Scholar] [CrossRef] [PubMed]
- Fu, C.; Guan, G.; Wang, H. The Anticancer Effect of Sanguinarine: A Review. Curr. Pharm. Des. 2018, 24, 2760–2764. [Google Scholar] [CrossRef]
- Croaker, A.; King, G.J.; Pyne, J.H.; Anoopkumar-Dukie, S.; Simanek, V.; Liu, L. Carcinogenic potential of sanguinarine, a phytochemical used in ‘therapeutic’ black salve and mouthwash. Mutat. Res. Mutat. Res. 2017, 774, 46–56. [Google Scholar] [CrossRef] [PubMed]
- Tuzimski, T.; Petruczynik, A. Application of HPLC-DAD for In Vitro Investigation of Acetylcholinesterase Inhibition Activity of Selected Isoquinoline Alkaloids from Sanguinaria canadensis Extracts. Molecules 2021, 26, 230. [Google Scholar] [CrossRef]
- Kuznetsova, L.P.; Nikol’Skaya, E.B.; Sochilina, E.E.; Faddeeva, M.D. Inhibition of Human Blood Acetylcholinesterase and Butyrylcholinesterase by Some Alkaloids. J. Evol. Biochem. Physiol. 2002, 38, 35–39. [Google Scholar] [CrossRef]
- Singh, N.; Sharma, B. Toxicological Effects of Berberine and Sanguinarine. Front. Mol. Biosci. 2018, 5, 21. [Google Scholar] [CrossRef] [Green Version]
- Jung, H.A.; Min, B.-S.; Yokozawa, T.; Lee, J.-H.; Kim, Y.S.; Choi, J.S. Anti-Alzheimer and antioxidant activities of Coptidis Rhizoma alkaloids. Biol. Pharm. Bull. 2009, 32, 1433–1438. [Google Scholar] [CrossRef] [Green Version]
- Huang, L.; Luo, Z.; He, F.; Lu, J.; Li, X. Synthesis and biological evaluation of a new series of berberine derivatives as dual inhibitors of acetylcholinesterase and butyrylcholinesterase. Bioorgan. Med. Chem. 2010, 18, 4475–4484. [Google Scholar] [CrossRef] [PubMed]
- Fan, L.; Fan, Y.; Liu, L.; Tao, W.; Shan, X.; Dong, Y.; Li, L.; Zhang, S.; Wang, H. Chelerythrine Attenuates the Inflammation of Lipopolysaccharide-Induced Acute Lung Inflammation Through NF-κB Signaling Pathway Mediated by Nrf2. Front. Pharmacol. 2018, 9, 1047. [Google Scholar] [CrossRef]
- Zhang, J.; Liang, Y.; Ren, L.; Zhang, T. In vitro Anti-Inflammatory Potency of Sanguinarine and Chelerythrine via Interaction with Glucocorticoid Receptor. eFood 2020, 1, 392–398. [Google Scholar] [CrossRef]
- Omar, F.; Tareq, A.M.; Alqahtani, A.M.; Dhama, K.; Sayeed, M.A.; Emran, T.B.; Simal-Gandara, J. Plant-Based Indole Alkaloids: A Comprehensive Overview from a Pharmacological Perspective. Molecules 2021, 26, 2297. [Google Scholar] [CrossRef]
- Mroue, M.A.; Euler, K.L.; Ghuman, M.A.; Alam, M. Indole Alkaloids of Haplophyton crooksii. J. Nat. Prod. 1996, 59, 890–893. [Google Scholar] [CrossRef]
- Newby, D.; Freitas, A.; Ghafourian, T. Decision trees to characterise the roles of permeability and solubility on the prediction of oral absorption. Eur. J. Med. Chem. 2015, 90, 751–765. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Galantamine Hydrobromide. Available online: https://www.sigmaaldrich.com/GB/en/sds/sial/phr1623 (accessed on 10 December 2021).
- Donepezil Hydrochloride. Available online: https://www.sigmaaldrich.com/GB/en/sds/sigma/d6821 (accessed on 10 December 2021).
- Watkins, P.B.; Zimmerman, H.J.; Knapp, M.J.; Gracon, S.I.; Lewis, K.W. Hepatotoxic effects of tacrine administration in patients with Alzheimer’s disease. JAMA 1994, 271, 992–998. [Google Scholar] [CrossRef]
- Stavrakov, G.; Philipova, I.; Zheleva, D.; Atanasova, M.; Konstantinov, S.; Doytchinova, I. Docking-based Design of Galantamine Derivatives with Dual-site Binding to Acetylcholinesterase. Mol. Inform. 2016, 35, 278–285. [Google Scholar] [CrossRef]
- Najafi, Z.; Mahdavi, M.; Saeedi, M.; Karimpour-Razkenari, E.; Edraki, N.; Sharifzadeh, M.; Khanavi, M.; Akbarzadeh, T. Novel tacrine-coumarin hybrids linked to 1, 2, 3-triazole as anti-Alzheimer’s compounds: In vitro and in vivo biological evaluation and docking study. Bioorganic Chem. 2019, 83, 303–316. [Google Scholar] [CrossRef]
- Pandey, K.B.; Rizvi, S.I. Plant polyphenols as dietary antioxidants in human health and disease. Oxid. Med. Cell. Longev. 2009, 2, 270–278. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ogura, H.; Kosasa, T.; Kuriya, Y.; Yamanishi, Y. Comparison of inhibitory activities of donepezil and other cholinesterase inhibitors on acetylcholinesterase and butyrylcholinesterase in vitro. Methods Find. Exp. Clin. Pharmacol. 2000, 22, 609–613. [Google Scholar] [CrossRef]
- Rogers, S.L.; Friedhoff, L.T. Pharmacokinetic and pharmacodynamic profile of donepezil HCl following single oral doses. Br. J. Clin. Pharmacol. 1998, 46 (Suppl. S1), 392–398. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Seltzer, B. Donepezil: A review. Expert Opin. Drug Metab. Toxicol. 2005, 1, 527–536. [Google Scholar] [CrossRef]
- Bickel, U.; Thomsen, T.; Weber, W.; Fischer, J.P.; Bachus, R.; Nitz, M.; Kewitz, H. Pharmacokinetics of galanthamine in humans and corresponding cholinesterase inhibition. Clin. Pharmacol. Ther. 1991, 50, 420–428. [Google Scholar] [CrossRef] [PubMed]
- Polinsky, R.J. Clinical pharmacology of rivastigmine: A new-generation acetylcholinesterase inhibitor for the treatment of Alzheimer’s disease. Clin. Ther. 1998, 20, 634–647. [Google Scholar] [CrossRef]

| Ligand | PubChem ID | 2D Structures | Mol. Wt g/mol | Example Source Plants * | AChE Affinity (kcal/mol) |
|---|---|---|---|---|---|
| Sanguinarine | CID_5154 |  | 332.3 | S. canadensis, A. mexicana, B. frutescens, C. majus, Corydalis spp., E. californica, G. flavum, M. cordata | −10.4 |
| Huperzine A | CID_854026 | 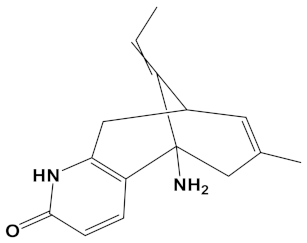 | 242.32 | Huperzia spp., L. selago, L. serratum | −9.9 |
| Chelerythrine | CID_2703 | 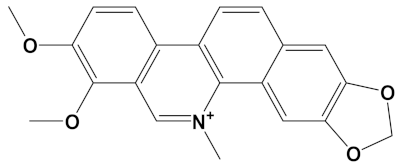 | 348.4 | A. mexicana, Bocconia spp., C. majus, E. californica, G. flavum, S. canadensis, Zanthoxylum spp. | −9.4 |
| Yohimbine | CID_8969 | 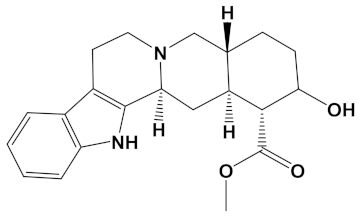 | 354.4 | A. floribunda, P. johimbe, Rauvolfia spp., Catharanthus spp., A. quebrachoblanco | −9.3 |
| Berberine | CID_2353 | 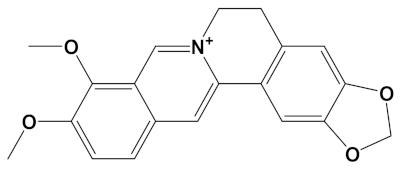 | 336.4 | B. vulgaris, Caulophyllum spp., Coptis spp., Corydalis spp., H. canadensis, Mahonia spp., Podophyllum spp., Zanthoxylum spp. | −9.2 |
| Berberastine | CID_442180 | 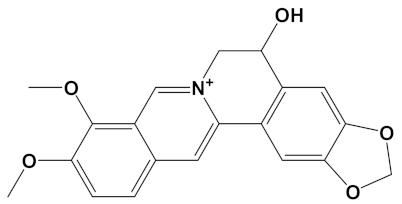 | 352.4 | Coptis spp., H. canadensis, Xanthorhiza simplicissima | −9.1 |
| Naringenin | CID_932 | 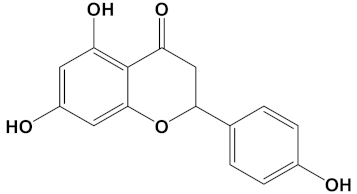 | 272.25 | Citrus spp., E. globulus, A. dracunculus, Glycyrrhiza spp., M. pomifera, Prunus spp., Salix sp., S. marianum | −8.5 |
| Akuammicine | CID_10314057 | 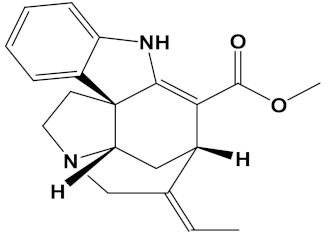 | 322.4 | A. quebrachoblanco, C. roseus, V minor | −8.1 |
| Carvone | CID_7439 |  | 150.22 | Citrus spp., Eucalyptus spp., Mentha spp., Origanum spp., Thymus spp., Teucrium spp., Pycnanthemum spp. | −7.7 |
| Galantamine | CID_9651 | 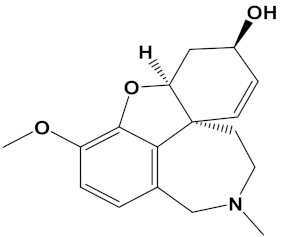 | 287.35 | G. nivalis, H. vittatum, L. radiata, L. squamigera, N. tazetta, P. maritimum | −7.7 |
| Ligand | Mol. Formula | 2D Structures | AChE Affinity (kcal/mol) | BuChE Affinity (kcal/mol) |
|---|---|---|---|---|
| Huperzine-4C-Naringenin | C34H36N2O5 |  | −14.1 | −12.3 |
| Naringenin-4C- Galantamine | C35H37NO7 |  | −14.0 | −11.9 |
| Huperzine-4C- Galantamine | C35H43N3O4 |  | −13.4 | −11.4 |
| Huperzine-5C- Carvone | C30H41N3O | 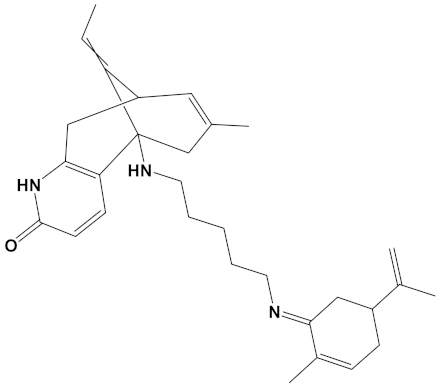 | −13.0 | −10.0 |
| Yohimbine-5C- Carvone | C35H48N4O2 | 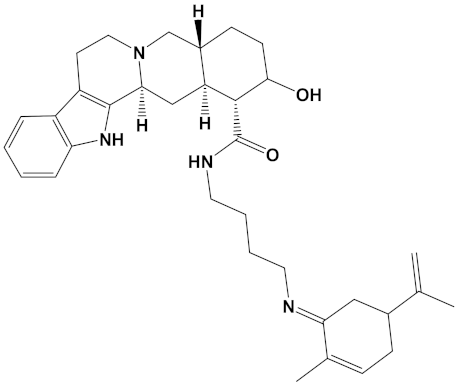 | −13.0 | −11.6 |
| Galantamine-4C- Carvone | C30H40N2O3 | 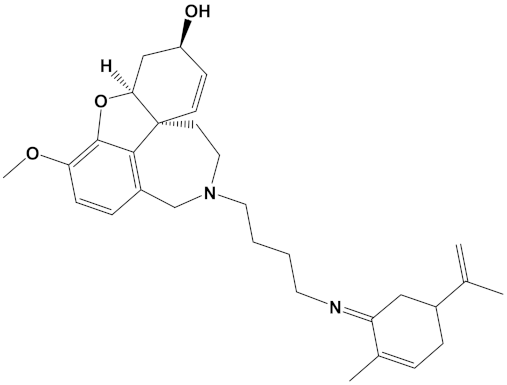 | −12.9 | −11.0 |
| Sanguinarine-4C- Carvone | C33H34N2O4 | 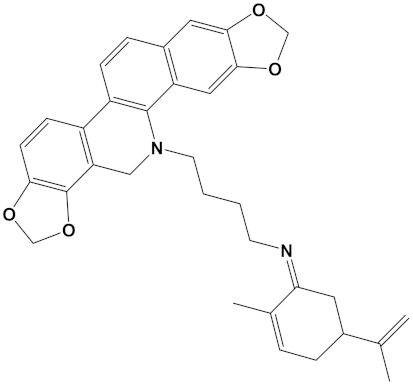 | −12.7 | −10.4 |
| Berberine-4C- Carvone | C34H39N2O4+ | 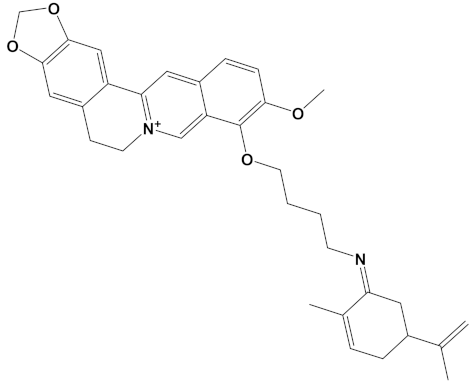 | −11.8 | −10.3 |
| Chelerythrine-4C-Carvone | C33H37N2O4 | 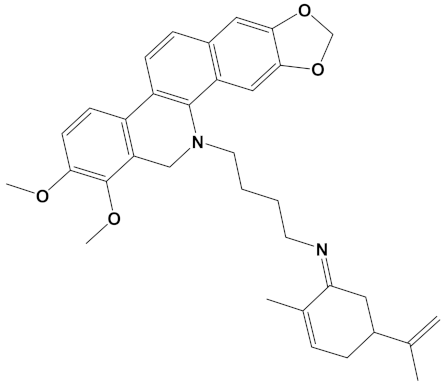 | −11.8 | −10.3 |
| Berberastine-4C- Carvone | C33H37N2O5+ | 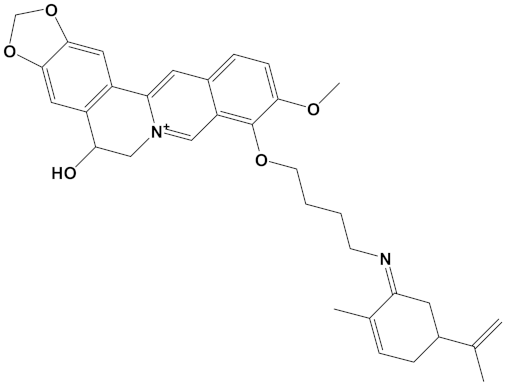 | −11.6 | −10.4 |
| Akuammicine-4C-Carvone | C32H41N3 | 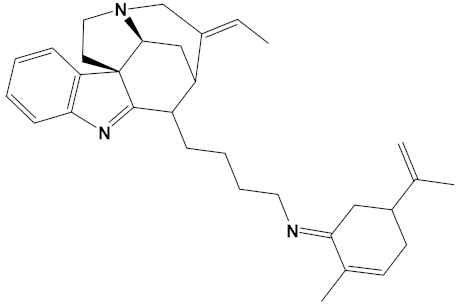 | −11.1 | −11.6 |
| Donepezil | C24H29NO3 | 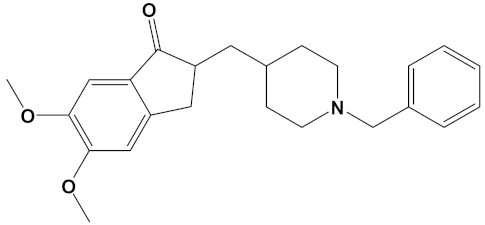 | −10.5 | −9.8 |
| Ligand | Mol. Wt. g/mol | Rotatable Bonds | H-Bond Acceptors | H-Bond Donors | Log Po/w | GI Absorption |
|---|---|---|---|---|---|---|
| Galantamine | 287.4 | 1 | 4 | 1 | 1.92 | High |
| Sanguinarine | 332.3 | 0 | 4 | 0 | 2.88 | High |
| Huperzine A | 242.3 | 1 | 2 | 2 | 1.88 | High |
| Chelerythrine | 348.4 | 2 | 4 | 0 | 3.02 | High |
| Yohimbine | 354.4 | 2 | 4 | 2 | 2.48 | High |
| Berberine | 336.4 | 2 | 4 | 0 | 2.53 | High |
| Berberastine | 352.4 | 2 | 5 | 1 | 1.72 | High |
| Naringenin | 272.3 | 1 | 5 | 3 | 1.84 | High |
| Akuammicine | 322.4 | 2 | 3 | 1 | 2.60 | High |
| Carvone | 150.2 | 1 | 1 | 0 | 2.44 | High |
| Donepezil | 379.5 | 6 | 4 | 0 | 4.00 | High |
| Huperzine-4C-Naringenin | 552.7 | 7 | 6 | 4 | 3.20 | Low |
| Naringenin-4C- Galantamine | 583.7 | 7 | 8 | 3 | 2.46 | High |
| Huperzine-4C- Galantamine | 569.7 | 7 | 6 | 3 | 3.33 | High |
| Huperzine-5C-Carvone | 459.7 | 8 | 3 | 2 | 4.38 | High |
| Yohimbine-5C-Carvone | 556.8 | 9 | 4 | 3 | 3.53 | High |
| Galantamine-4C- Carvone | 476.6 | 7 | 5 | 1 | 3.43 | High |
| Sanguinarine-4C- Carvone | 522.6 | 6 | 5 | 0 | 4.46 | Low |
| Berberine-4C-Carvone | 525.7 | 8 | 5 | 0 | 3.79 | High |
| Chelerythrine-4C- Carvone | 538.7 | 8 | 5 | 0 | 4.24 | Low |
| Berberastine-4C- Carvone | 541.7 | 8 | 6 | 1 | 2.99 | High |
| Akuammicine-4C- Carvone | 467.3 | 6 | 3 | 0 | 4.50 | High |
| Ligand | LD50 Predicted in Rodent (mg/kg) | Toxicity Class * | Hepatotoxicity |
|---|---|---|---|
| Galantamine | 85 | III | Inactive |
| Sanguinarine | 778 | IV | Inactive |
| Huperzine A | 5 | II | Inactive |
| Chelerythrine | 778 | IV | Inactive |
| Yohimbine | 300 | III | Inactive |
| Berberine | 200 | III | Inactive |
| Berberastine | 200 | III | Inactive |
| Naringenin | 2000 | IV | Inactive |
| Akuammicine | 28 | II | Inactive |
| Carvone | 1640 | IV | Inactive |
| Donepezil | 505 | IV | Inactive |
| Huperzine-4C-Naringenin | 280 | III | Inactive |
| Naringenin-4C-Galantamine | 100 | III | Inactive |
| Huperzine-4C-Galantamine | 100 | III | Inactive |
| Huperzine-5C-Carvone | 150 | III | Inactive |
| Yohimbine-5C-Carvone | 300 | III | Inactive |
| Galantamine-4C-Carvone | 100 | III | Inactive |
| Sanguinarine-4C-Carvone | 296 | III | Inactive |
| Berberine-4C-Carvone | 200 | III | Inactive |
| Chelerythrine-4C-Carvone | 296 | III | Inactive |
| Berberastine-4C-Carvone | 1000 | IV | Inactive |
| Akuammicine-4C-Carvone | 325 | IV | Inactive |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Amat-ur-Rasool, H.; Ahmed, M.; Hasnain, S.; Ahmed, A.; Carter, W.G. In Silico Design of Dual-Binding Site Anti-Cholinesterase Phytochemical Heterodimers as Treatment Options for Alzheimer’s Disease. Curr. Issues Mol. Biol. 2022, 44, 152-175. https://doi.org/10.3390/cimb44010012
Amat-ur-Rasool H, Ahmed M, Hasnain S, Ahmed A, Carter WG. In Silico Design of Dual-Binding Site Anti-Cholinesterase Phytochemical Heterodimers as Treatment Options for Alzheimer’s Disease. Current Issues in Molecular Biology. 2022; 44(1):152-175. https://doi.org/10.3390/cimb44010012
Chicago/Turabian StyleAmat-ur-Rasool, Hafsa, Mehboob Ahmed, Shahida Hasnain, Abrar Ahmed, and Wayne Grant Carter. 2022. "In Silico Design of Dual-Binding Site Anti-Cholinesterase Phytochemical Heterodimers as Treatment Options for Alzheimer’s Disease" Current Issues in Molecular Biology 44, no. 1: 152-175. https://doi.org/10.3390/cimb44010012
APA StyleAmat-ur-Rasool, H., Ahmed, M., Hasnain, S., Ahmed, A., & Carter, W. G. (2022). In Silico Design of Dual-Binding Site Anti-Cholinesterase Phytochemical Heterodimers as Treatment Options for Alzheimer’s Disease. Current Issues in Molecular Biology, 44(1), 152-175. https://doi.org/10.3390/cimb44010012