The Special Features of Prenatal and Preimplantation Genetic Counseling in Arab Countries
Abstract
:1. Introduction
2. Consanguinity and the Need for Prenatal Counseling
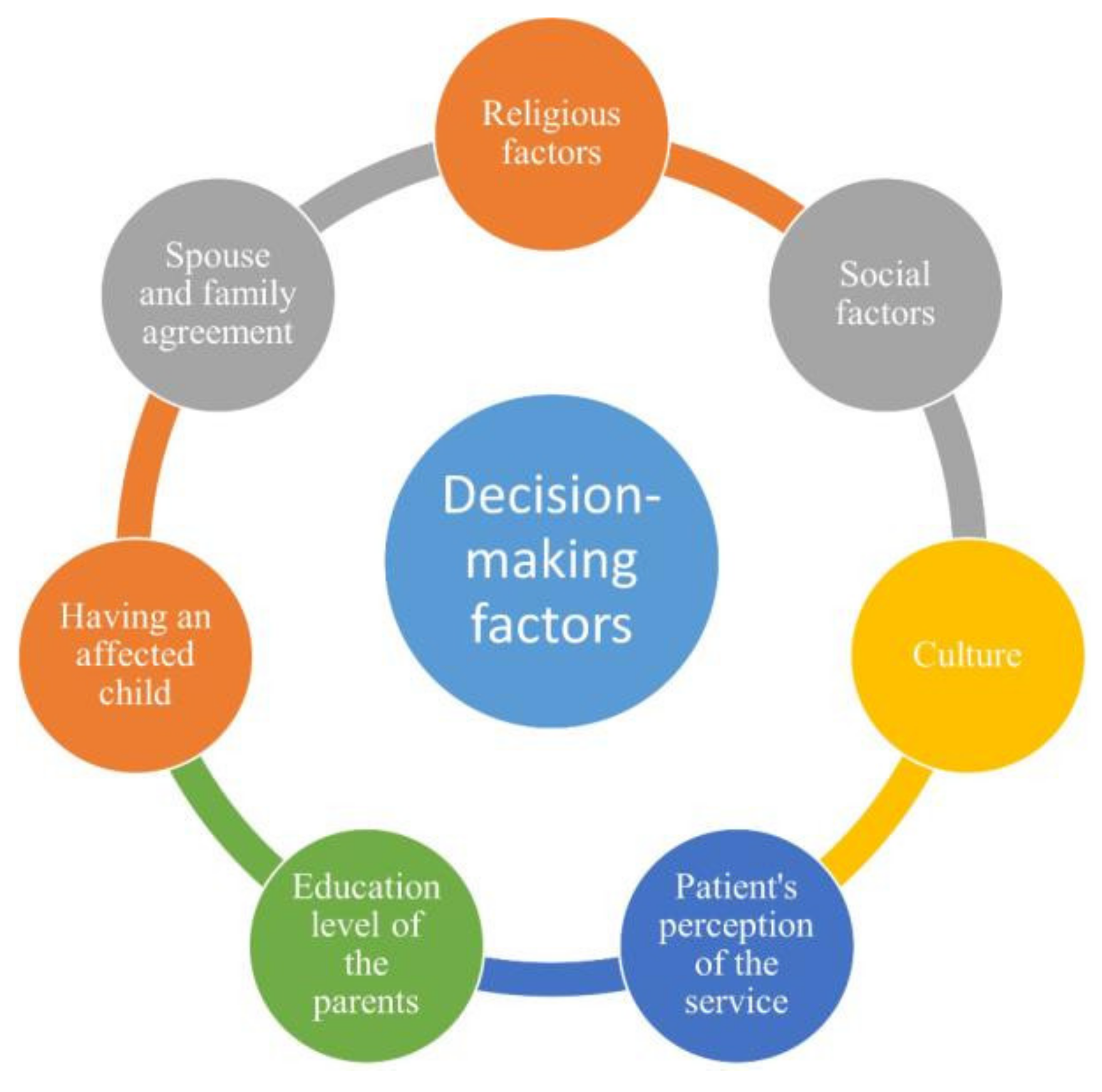
- There is abundant literature on the factors affecting decision making and the types of decisions made by parents accessing prenatal genetic counseling ser-vices around the world.
- Most of the 22 Arab countries still do not provide genetic counseling services, despite a significant need, given the elevated consanguinity rates in the region.
- It is known that social and cultural factors influence decision making around access to and uptake of prenatal genetic counseling services, although the fac-tors specific to the Arab world are less well documented.
- Utilization of genetic counseling services varies across different Arab countries.
- Many factors affect decision making and service utilization in the region, not least religion.
- Knowledge of these factors, especially religious drivers of acceptance of prena-tal genetic counseling services, can help to improve informed decision making in the Arab world and beyond.
3. The Decisions Faced in Prenatal Settings
4. Factors Affecting the Acceptance of Prenatal Genetic Counseling Services
4.1. Social Factors
4.2. Religious Factors
4.3. Cultural Factors
4.4. Miscellaneous Factors
5. Genetic Counseling Service in Qatar
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Zayed, H. The Arab genome: Health and wealth. Gene 2016, 592, 239–243. [Google Scholar] [CrossRef] [PubMed]
- Al-Gazali, L.; Hamamy, H. Consanguinity and dysmorphology in Arabs. Hum. Hered. 2014, 77, 93–107. [Google Scholar] [CrossRef]
- Yunis, K.; El Rafei, R.; Mumtaz, G. International perspectives: Consanguinity: Perinatal outcomes and prevention—A view from the Middle East. NeoReviews 2008, 9, e59–e65. [Google Scholar] [CrossRef]
- Uhlmann, W.R.; Schuette, J.L.; Yashar, B. A Guide to Genetic Counseling; John Wiley & Sons: Hoboken, NJ, USA, 2011; ISBN 1118210530. [Google Scholar]
- Albar, M.A. Ethical considerations in the prevention and management of genetic disorders with special emphasis on religious considerations. Saudi Med. J. 2002, 23, 627–632. [Google Scholar] [PubMed]
- Cuckle, H.; Maymon, R. Development of prenatal screening—A historical overview. Semin. Perinatol. 2016, 40, 12–22. [Google Scholar] [CrossRef]
- Krstic, N.; Obican, S.G. Current landscape of prenatal genetic screening and testing. Birth Defects Res. 2020, 112, 321–331. [Google Scholar] [CrossRef]
- Al-Herz, W.; Aldhekri, H.; Barbouche, M.R.; Rezaei, N. Consanguinity and primary immunodeficiencies. Hum. Hered. 2014, 77, 138–143. [Google Scholar] [CrossRef] [Green Version]
- Al-Gazali, L.I. Attitudes toward genetic counseling in the United Arab Emirates. Community Genet. 2005, 8, 48–51. [Google Scholar] [CrossRef]
- Balobaid, A.; Qari, A.; Al-Zaidan, H. Genetic counselors’ scope of practice and challenges in genetic counseling services in Saudi Arabia. Int. J. Pediatr. Adolesc. Med. 2016, 3, 1–6. [Google Scholar] [CrossRef] [Green Version]
- Bener, A.; Al-Mulla, M.; Clarke, A. Premarital screening and genetic counseling program: Studies from an endogamous population. Int. J. Appl. Basic Med. Res. 2019, 9, 20–26. [Google Scholar] [CrossRef]
- El Hawary, R.E.; Meshaal, S.S.; Abd Elaziz, D.S.; Elsharkawy, M.A.; Alkady, R.S.; Lotfy, S.; El-Sheikhah, A.; Hassan, A.; Galal, N.M.; Boutros, J.A.; et al. Genetic counseling in primary immunodeficiency disorders: An emerging experience in Egypt. Mol. Diagn. Ther. 2017, 21, 677–684. [Google Scholar] [CrossRef] [PubMed]
- Ahram, M.; Soubani, M.; Salem, L.A.; Saker, H.; Ahmad, M. Knowledge, attitudes, and practice regarding genetic testing and genetic counselors in Jordan: A population-based survey. J. Genet. Couns. 2015, 24, 1001–1010. [Google Scholar] [CrossRef]
- Abacan, M.; Alsubaie, L.; Barlow-Stewart, K.; Caanen, B.; Cordier, C.; Courtney, E.; Davoine, E.; Edwards, J.; Elackatt, N.J.; Gardiner, K.; et al. The global state of the genetic counseling profession. Eur. J. Hum. Genet. 2019, 27, 183–197. [Google Scholar] [CrossRef] [Green Version]
- Alshawish, E.; Yaseen, F. Knowledge and attitude toward genetic counseling and testing among parents of children with genetic disorder in the West Bank/Palestine. Palest. Med. Pharm. J. 2018, 3, 24–30. [Google Scholar]
- Chaabouni-Bouhamed, H. Tunisia: Communities and community genetics. Public Health Genom. 2008, 11, 313–323. [Google Scholar] [CrossRef]
- Alsaeed, E.S.; Farhat, G.N.; Assiri, A.M.; Memish, Z.; Ahmed, E.M.; Saeedi, M.Y.; Al-Dossary, M.F.; Bashawri, H. Distribution of hemoglobinopathy disorders in Saudi Arabia based on data from the premarital screening and genetic counseling program, 2011–2015. J. Epidemiol. Glob. Health 2018, 7 (Suppl. S1), S41–S47. [Google Scholar] [CrossRef] [PubMed]
- Ibrahim, N.K.; Bashawri, J.; Al Bar, H.; Al Ahmadi, J.; Al Bar, A.; Qadi, M.; Milaat, W.; Feda, H. Premarital screening and genetic counseling program: Knowledge, attitude, and satisfaction of attendees of governmental outpatient clinics in Jeddah. J. Infect. Public Health 2013, 6, 41–54. [Google Scholar] [CrossRef] [Green Version]
- Bawazeer, S.; AlSayed, M.; Kurdi, W.; Balobaid, A. Knowledge and attitudes regarding non-invasive prenatal testing among women in Saudi Arabia. Prenat. Diagn. 2021, 41, 1343–1350. [Google Scholar] [CrossRef] [PubMed]
- Bachir, S.; Aouar, A. Study of the impact of consanguinity on abortion and mortality in the population of Beni Abbes (Southwestern Algeria). Egypt. J. Med. Hum. Genet. 2019, 20, 1. [Google Scholar] [CrossRef] [Green Version]
- Hamamy, H.A.; Al-Hakkak, Z.S. Consanguinity and reproductive health in Iraq. Hum. Hered. 1989, 39, 271–275. [Google Scholar] [CrossRef]
- Al-Nood, H.; Al-Hadi, A. Proposed low-cost premarital screening program for prevention of sickle cell and thalassemia in Yemen. Qatar Med. J. 2013, 2013, 33–37. [Google Scholar] [CrossRef] [Green Version]
- Thong, M.K.; See-Toh, Y.; Hassan, J.; Ali, J. Medical genetics in developing countries in the Asia-Pacific region: Challenges and opportunities. Genet. Med. 2018, 20, 1114–1121. [Google Scholar] [CrossRef] [PubMed]
- Kimelman, D.; Pavone, M.E. Non-invasive prenatal testing in the context of IVF and PGT-A. Best Pract. Res. Clin. Obstet. Gynaecol. 2021, 70, 51–62. [Google Scholar] [CrossRef]
- Harper, J.C.; Wilton, L.; Traeger-Synodinos, J.; Goossens, V.; Moutou, C.; SenGupta, S.B.; Pehlivan Budak, T.; Renwick, P.; De Rycke, M.; Geraedts, J.P.; et al. The ESHRE PGD consortium: 10 years of data collection. Hum. Reprod. Update 2012, 18, 234–247. [Google Scholar] [CrossRef] [Green Version]
- Zuckerman, S.; Gooldin, S.; Zeevi, D.A.; Altarescu, G. The decision-making process, experience, and perceptions of preimplantation genetic testing (PGT) users. J. Assist. Reprod. Genet. 2020, 37, 1903–1912. [Google Scholar] [CrossRef]
- Buchanan, A.; Sachs, A.; Toler, T.; Tsipis, J. NIPT: Current utilization and implications for the future of prenatal genetic counseling. Prenat. Diagn. 2014, 34, 850–857. [Google Scholar] [CrossRef] [Green Version]
- Devers, P.L.; Cronister, A.; Ormond, K.E.; Facio, F.; Brasington, C.K.; Flodman, P. Noninvasive prenatal testing/noninvasive prenatal diagnosis: The position of the National Society of Genetic Counselors. J. Genet. Couns. 2013, 22, 291–295. [Google Scholar] [CrossRef]
- El-Hazmi, M.A.; al-Swailem, A.R.; Warsy, A.S.; al-Swailem, A.M.; Sulaimani, R.; al-Meshari, A.A. Consanguinity among the Saudi Arabian population. J. Med. Genet. 1995, 32, 623–626. [Google Scholar] [CrossRef] [PubMed]
- Al-Gazali, L.; Hamamy, H.; Al-Arrayad, S. Genetic disorders in the Arab world. BMJ 2006, 333, 831–834. [Google Scholar] [CrossRef] [Green Version]
- Oniya, O.; Neves, K.; Ahmed, B.; Konje, J.C. A Review of the reproductive consequences of consanguinity. Eur. J. Obstet. Gynecol. Reprod. Biol. 2019, 232, 87–96. [Google Scholar] [CrossRef] [PubMed]
- El Shanti, H.; Chouchane, L.; Badii, R.; Gallouzi, I.E.; Gasparini, P. Genetic testing and genomic analysis: A debate on ethical, social and legal issues in the Arab world with a focus on Qatar. J. Transl. Med. 2015, 13, 358. [Google Scholar] [CrossRef] [Green Version]
- Lai, S.; Zhang, X.; Feng, L.; He, M.; Wang, S. The prenatal diagnosis and genetic counseling of chromosomal micro-duplication on 10q24.3 in a fetus: A case report and a brief review of the literature. Medicine 2020, 99, e22533. [Google Scholar] [CrossRef]
- Raz, A.E.; Vizner, Y. Carrier matching and collective socialization in community genetics: Dor Yeshorim and the reinforcement of stigma. Soc. Sci. Med. 2008, 67, 1361–1369. [Google Scholar] [CrossRef] [PubMed]
- Al-Odaib, A.N.; Abu-Amero, K.K.; Ozand, P.T.; Al-Hellani, A.M. A New era for preventive genetic programs in the Arabian Peninsula. Saudi Med. J. 2003, 24, 1168–1175. [Google Scholar]
- Sulaiman, R.A.; Al-Owain, M. Inherited metabolic disorders in adults: A view from Saudi Arabia. Eur. J. Med. Genet. 2019, 62, 103562. [Google Scholar] [CrossRef]
- Richards, S.; Aziz, N.; Bale, S.; Bick, D.; Das, S.; Gastier-Foster, J.; Grody, W.W.; Hegde, M.; Lyon, E.; Spector, E.; et al. Standards and guidelines for the interpretation of sequence variants: A joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet. Med. 2015, 17, 405–424. [Google Scholar] [CrossRef]
- Zhytnik, L.; Simm, K.; Salumets, A.; Peters, M.; Märtson, A.; Maasalu, K. Reproductive options for families at risk of osteogenesis imperfecta: A review. Orphanet J. Rare Dis. 2020, 15, 128. [Google Scholar] [CrossRef]
- De Die-Smulders, C.E.; de Wert, G.M.; Liebaers, I.; Tibben, A.; Evers-Kiebooms, G. Reproductive options for prospective parents in families with Huntington’s disease: Clinical, psychological and ethical reflections. Hum. Reprod. Update 2013, 19, 304–315. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bach, G.; Zeigler, M.; Zlotogora, J. Prevention of lysosomal storage disorders in Israel. Mol. Genet. Metab. 2007, 90, 353–357. [Google Scholar] [CrossRef] [PubMed]
- Hewison, J.; Green, J.M.; Ahmed, S.; Cuckle, H.S.; Hirst, J.; Hucknall, C.; Thornton, J.G. Attitudes to prenatal testing and termination of pregnancy for fetal abnormality: A comparison of white and Pakistani women in the UK. Prenat. Diagn. 2007, 27, 419–430. [Google Scholar] [CrossRef]
- Bayon, J.C.; Orruno, E.; Portillo, M.I.; Asua, J. The consequences of implementing non-invasive prenatal testing with cell-free foetal DNA for the detection of down syndrome in the Spanish national health service: A cost-effectiveness analysis. Cost Eff. Resour. Alloc. 2019, 17, 6. [Google Scholar] [CrossRef] [PubMed]
- Cernat, A.; De Freitas, C.; Majid, U.; Higgins, C.; Vanstone, M. Facilitating informed choice about non-invasive prenatal testing (NIPT): A systematic review and qualitative meta-synthesis of women’s experiences. BMC Pregnancy Childbirth 2019, 19, 27. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stokowski, R.; Wang, E.; White, K.; Batey, A.; Jacobsson, B.; Brar, H.; Balanarasimha, M.; Hollemon, D.; Sparks, A.; Nicolaides, K. Clinical performance of non-invasive prenatal testing (NIPT) using targeted cell-free DNA analysis in maternal plasma with microarrays or next generation sequencing (NGS) is consistent across multiple controlled clinical studies. Prenat. Diagn. 2015, 35, 1243–1246. [Google Scholar] [CrossRef] [Green Version]
- Van Opstal, D.; Srebniak, M.I.; Polak, J.; de Vries, F.; Govaerts, L.C.; Joosten, M.; Go, A.T.; Knapen, M.F.; van den Berg, C.; Diderich, K.E.; et al. False negative NIPT results: Risk figures for chromosomes 13, 18 and 21 based on chorionic villi results in 5967 cases and literature review. PLoS ONE 2016, 11, e0146794. [Google Scholar] [CrossRef] [Green Version]
- Haidar, H.; Rispler-Chaim, V.; Hung, A.; Chandrasekharan, S.; Ravitsky, V. Noninvasive prenatal testing: Implications for Muslim communities. AJOB Empir. Bioeth. 2015, 6, 94–105. [Google Scholar] [CrossRef]
- Palomaki, G.E.; Kloza, E.M.; Lambert-Messerlian, G.M.; Haddow, J.E.; Neveux, L.M.; Ehrich, M.; van den Boom, D.; Bombard, A.T.; Deciu, C.; Grody, W.W.; et al. DNA sequencing of maternal plasma to detect down syndrome: An international clinical validation study. Genet. Med. 2011, 13, 913–920. [Google Scholar] [CrossRef]
- Verdonk, P.; Metselaar, S.; Storms, O.; Bartels, E. Reproductive choices: A qualitative study of Dutch Moroccan and Turkish consanguineously married women’s perspectives on preconception carrier screening. BMC Womens Health 2018, 18, 79. [Google Scholar] [CrossRef] [PubMed]
- Bittles, A.H.; Black, M.L. Consanguinity, human evolution, and complex diseases. Proc. Natl. Acad. Sci. USA 2010, 107, 1779–1786. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tomashov-Matar, R.; Biran, G.; Lagovsky, I.; Kotler, N.; Stein, A.; Fisch, B.; Sapir, O.; Shohat, M. Severe combined immunodeficiency (SCID): From the detection of a new mutation to preimplantation genetic diagnosis. J. Assist. Reprod. Genet. 2012, 29, 687–692. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Simonstein, F.; Mashiach-Eizenberg, M. Reprogenetics, genetic tools and reproductive risk: Attitudes and understanding among Ethnic groups in Israel. J. Genet. Couns. 2016, 25, 127–134. [Google Scholar] [CrossRef]
- Basel-Vanagaite, L.; Taub, E.; Halpern, G.J.; Drasinover, V.; Magal, N.; Davidov, B.; Zlotogora, J.; Shohat, M. Genetic screening for autosomal recessive nonsyndromic mental retardation in an isolated population in Israel. Eur. J. Hum. Genet. 2007, 15, 250–253. [Google Scholar] [CrossRef] [PubMed]
- Besser, A.G.; Blakemore, J.K.; Grifo, J.A.; Mounts, E.L. Transfer of embryos with positive results following preimplantation genetic testing for monogenic disorders (PGT-M): Experience of two high-volume fertility clinics. J. Assist. Reprod. Genet. 2019, 36, 1949–1955. [Google Scholar] [CrossRef] [PubMed]
- Abduljabbar, H.S.; Amin, R. Assisted reproductive technology in Saudi Arabia. Saudi Med. J. 2009, 30, 461–464. [Google Scholar] [PubMed]
- Mennie, M.E.; Gilfillan, A.; Compton, M.E.; Liston, W.A.; Brock, D.J. Prenatal cystic fibrosis carrier screening: Factors in a woman’s decision to decline testing. Prenat. Diagn. 1993, 13, 807–814. [Google Scholar] [CrossRef]
- Neter, E.; Wolowelsky, Y.; Borochowitz, Z.U. Attitudes of Israeli Muslims at risk of genetic disorders towards pregnancy termination. Public Health Genom. 2005, 8, 88–93. [Google Scholar] [CrossRef]
- Chaabouni, H.; Chaabouni, M.; Maazoul, F.; M’Rad, R.; Jemaa, L.B.; Smaoui, N.; Terras, K.; Kammoun, H.; Belghith, N.; Ridene, H.; et al. Prenatal Diagnosis of Chromosome Disorders in Tunisian Population. Ann. Genet. 2001, 44, 99–104. [Google Scholar] [CrossRef]
- Olwi, D.; Merdad, L.; Ramadan, E. Knowledge of genetics and attitudes toward genetic testing among college students in Saudi Arabia. Public Health Genom. 2016, 19, 260–268. [Google Scholar] [CrossRef] [PubMed]
- Alsulaiman, A.; Hewison, J. Attitudes to prenatal and preimplantation diagnosis in Saudi parents at genetic risk. Prenat. Diagn. 2006, 26, 1010–1014. [Google Scholar] [CrossRef] [PubMed]
- Alsulaiman, A.; Mousa, A.; Kondkar, A.A.; Abu-Amero, K.K. Attitudes of Saudi parents with a deaf child towards prenatal diagnosis and termination of pregnancy. Prenat. Diagn. 2014, 34, 153–158. [Google Scholar] [CrossRef]
- Kosaryan, M.; Rabiei, K. Prenatal diagnosis in Islamic countries: A narrative review in 2013. J. Pediatr. Rev. 2014, 2, 47–54. [Google Scholar]
- Koren, A.; Zalman, L.; Palmor, H.; Zamir, R.B.; Levin, C.; Openheim, A.; Daniel-Spiegel, E.; Shalev, S.; Filon, D. Sickle cell anemia in Northern Israel: Screening and prevention. Isr. Med. Assoc. J. 2009, 11, 229–234. [Google Scholar]
- Sheiner, E.; Shoham-Vardi, I.; Weitzman, D.; Gohar, J.; Carmi, R. Decisions regarding pregnancy termination among Bedouin couples referred to third level ultrasound clinic. Eur. J. Obstet. Gynecol. Reprod. Biol. 1998, 76, 141–146. [Google Scholar] [CrossRef]
- Al-Kharusi, K. The Experiences of Couples Undergoing Preimplantation Genetic Diagnosis (PGD) at the Genetic and Developmental Medicine Clinic, Sultan Qaboos University Hospital (SQUH) in Oman. Master’s Thesis, University of Cape Town, Cape Town, South Africa, 2016. Available online: https://open.uct.ac.za/handle/11427/23776 (accessed on 1 January 2022).
- Jaber, L.; Halpern, G.J.; Samara, S. Prenatal testing and termination of future pregnancies in Arab mothers of children with severe defects: Impact of Moslem cleric or physician on the decision making. OJGen 2011, 1, 54–59. [Google Scholar] [CrossRef] [Green Version]
- Al-Kharusi, K.; Bruwer, Z.; Wessels, T. The experience of preimplantation genetic testing (PGT) among Muslim couples in Oman in the Middle East. J. Genet. Couns. 2021, 30, 121–131. [Google Scholar] [CrossRef] [PubMed]
- Gesser-Edelsburg, A.; Shahbari, N.A. Decision-making on terminating pregnancy for Muslim Arab women pregnant with fetuses with congenital anomalies: Maternal affect and doctor-patient communication. Reprod. Health 2017, 14, 49. [Google Scholar] [CrossRef] [PubMed]
- Farra, C.; Nassar, A.H.; Usta, I.M.; Salameh, P.; Souaid, M.; Awwad, J. Acceptance of preimplantation genetic diagnosis for beta-thalassemia in Lebanese women with previously affected children. Prenat. Diagn. 2008, 28, 828–832. [Google Scholar] [CrossRef]
- AlHarthi, F.; Al Sayed, M.; Yaqinuddin, A.; Karbani, G.A.; Blobaid, A.S.; Wahi, M.M. Agreement within couples on choosing preimplantation genetic diagnosis versus pre-natal diagnosis: Perspective from Saudi population. J. Biochem. Clin. Genet. 2019, 2, 18–27. [Google Scholar]
- Abdo, N.; Ibraheem, N.; Obeidat, N.; Graboski-Bauer, A.; Batieha, A.; Altamimi, N.; Khatatbih, M. Knowledge, Attitudes, and Practices of Women Toward Prenatal Genetic Testing. Genet. Epigenet. 2018, 11, 2516865718813122. [Google Scholar] [CrossRef] [PubMed]
- Harris, S.; Gilmore, K.; Hardisty, E.; Lyerly, A.D.; Vora, N.L. Ethical and counseling challenges in prenatal exome sequencing. Prenat. Diagn. 2018, 38, 897–903. [Google Scholar] [CrossRef]
- Hadley, D.W.; Jenkins, J.; Dimond, E.; Nakahara, K.; Grogan, L.; Liewehr, D.J.; Steinberg, S.M.; Kirsch, I. Genetic counseling and testing in families with hereditary nonpolyposis colorectal cancer. Arch. Intern. Med. 2003, 163, 573–582. [Google Scholar] [CrossRef] [Green Version]
- Sharaf, R.N.; Myer, P.; Stave, C.D.; Diamond, L.C.; Ladabaum, U. Uptake of genetic testing by relatives of lynch syndrome probands: A systematic review. Clin. Gastroenterol. Hepatol. 2013, 11, 1093–1100. [Google Scholar] [CrossRef]
- Sussner, K.M.; Jandorf, L.; Thompson, H.S.; Valdimarsdottir, H.B. Barriers and facilitators to BRCA genetic counseling among at-risk Latinas in New York City. Psychooncology 2013, 22, 1594–1604. [Google Scholar] [CrossRef] [PubMed]
- Muhsen, K.; Na’amnah, W.; Lesser, Y.; Volovik, I.; Cohen, D.; Shohat, T. Determinates of underutilization of amniocentesis among Israeli Arab women. Prenat. Diagn. 2010, 30, 138–143. [Google Scholar] [CrossRef]
- Sharkia, R.; Tarabeia, J.; Zalan, A.; Atamany, E.; Athamna, M.; Allon-Shalev, S. Factors affecting the utilization of genetic counseling services among Israeli Arab women. Prenat. Diagn. 2015, 35, 370–375. [Google Scholar] [CrossRef] [PubMed]
- Altaany, Z.; Khabour, O.F.; Al-Taani, G. Knowledge, beliefs, and attitudes concerning genetic testing among young Jordanians. J. Multidiscip. Healthc. 2019, 12, 1043. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gaboon, N.E.; Bakur, K.H.; Edrees, A.Y.; Al-Aama, J.Y. Attitude toward prenatal testing and termination of pregnancy among health professionals and medical students in Saudi Arabia. J. Pediatr. Genet. 2017, 6, 149. [Google Scholar]
- Khan, M.A.Z.; Konje, J.C. Ethical and religious dilemmas of modern reproductive choices and the Islamic perspective. Eur. J. Obstet. Gynecol. Reprod. Biol. 2019, 232, 5–9. [Google Scholar] [CrossRef] [PubMed]
- Serour, G.I. Islamic perspectives in human reproduction. Reprod. Biomed. Online 2008, 17 (Suppl. S3), 34–38. [Google Scholar] [CrossRef]
- Schenker, J.G. Assisted reproduction practice: Religious perspectives. Reprod. Biomed. Online 2005, 10, 310–319. [Google Scholar] [CrossRef]
- Sultan, H.A. Legalization and Islamic Bioethical Perspectives on Prenatal Diagnosis and Advanced Uses of Pre Implantation Genetic Diagnosis in Saudi Arabia. J. Clin. Res. Bioeth. 2013, 4, S1. [Google Scholar] [CrossRef] [Green Version]
- Shabana, A. Islamic ethics and the legitimacy of scientific innovation: Reproductive genetic counseling within the Muslim context. Sociol. Islam 2020, 8, 265–289. [Google Scholar] [CrossRef]
- Alkuraya, F.S.; Kilani, R.A. Attitude of Saudi families affected with hemoglobinopathies towards prenatal screening and abortion and the influence of religious ruling (fatwa). Prenat. Diagn. 2001, 21, 448–451. [Google Scholar] [CrossRef]
- Chamsi-Pasha, H.; Albar, M.A. Assisted reproductive technology: Islamic Sunni perspective. Hum. Fertil. 2015, 18, 107–112. [Google Scholar] [CrossRef] [PubMed]
- Raz, A.E.; Atar, M. Nondirectiveness and its lay interpretations: The effect of counseling style, ethnicity and culture on attitudes towards genetic counseling among Jewish and Bedouin respondents in Israel. J. Genet. Couns. 2003, 12, 313–332. [Google Scholar] [CrossRef] [PubMed]
- El-Beshlawy, A.; El-Shekha, A.; Momtaz, M.; Said, F.; Hamdy, M.; Osman, O.; Meshaal, S.; Gafaar, T.; Petrou, M. Prenatal diagnosis for thalassaemia in Egypt: What changed parents’ attitude? Prenat. Diagn. 2012, 32, 777–782. [Google Scholar] [CrossRef]
- Awwad, R.; Veach, P.M.; Bartels, D.M.; LeRoy, B.S. Culture and acculturation influences on Palestinian perceptions of prenatal genetic counseling. J. Genet. Couns. 2008, 17, 101–116. [Google Scholar] [CrossRef]
- Bruwer, Z.; Achandira, U.; Al Kharousi, K.; Al-Kindy, A. Existing challenges associated with offering prenatal genetic diagnosis in an Arab Society in the Sultanate of Oman. J. Genet. Couns. 2014, 23, 928–932. [Google Scholar] [CrossRef] [PubMed]
- Saleem, R.; Gofin, R.; Ben-Neriah, Z.; Boneh, A. Variables influencing parental perception of inherited metabolic diseases before and after genetic counselling. J. Inherit. Metab. Dis. 1998, 21, 769–780. [Google Scholar] [CrossRef] [PubMed]
- Cohen-Kfir, N.; Bentwich, M.E.; Kent, A.; Dickman, N.; Tanus, M.; Higazi, B.; Kalfon, L.; Rudolf, M.; Falik-Zaccai, T.C. Challenges to effective and autonomous genetic testing and counseling for ethno-cultural minorities: A qualitative study. BMC Med. Ethics 2020, 21, 98. [Google Scholar] [CrossRef] [PubMed]
- Jaber, L.; Dolfin, T.; Shohat, T.; Halpern, G.J.; Reish, O.; Fejgin, M. Prenatal diagnosis for detecting congenital malformations: Acceptance among Israeli Arab women. Isr. Med. Assoc. J. 2000, 2, 346–350. [Google Scholar]
- Eskandarani, H.A. Ethical Concerns to the Use of Pre-Implantation Genetic Diagnosis in the Gulf Cooperative Council States; Citeseer: Princeton, NJ, USA, 2007; pp. 20–22. [Google Scholar]
- Eskandarani, H.A. Pre-implantation genetic diagnosis in the Gulf Cooperative Council countries: Utilization and ethical attitudes. Hum. Reprod. Genet. Ethics 2009, 15, 68–74. [Google Scholar] [CrossRef] [PubMed]
- Alsulaiman, A.; Al-Odaib, A.; Al-Rejjal, R.; Hewison, J. Preimplantation genetic diagnosis in Saudi Arabia: Parents’ experience and attitudes. Prenat. Diagn. 2010, 30, 753–757. [Google Scholar] [CrossRef] [PubMed]
- Padela, A.I.; Killawi, A.; Heisler, M.; Demonner, S.; Fetters, M.D. The role of imams in American Muslim health: Perspectives of Muslim community leaders in Southeast Michigan. J. Relig. Health 2011, 50, 359–373. [Google Scholar] [CrossRef] [PubMed]
- Bressler, T.; Popp, B. Orthodox Jewish thought leaders’ insights regarding BRCA mutations: A descriptive study. J. Oncol. Pract. 2017, 13, e303–e309. [Google Scholar] [CrossRef] [PubMed]
| Countries with Established Genetic Counseling Services | Countries Demonstrating a Need for Genetic Counseling Services | Countries with No Reported Genetic Counseling Services |
|---|---|---|
| Saudi Arabia | Algeria | Djibouti |
| Bahrain | Iraq | Libya |
| Egypt | Yemen | Mauritania |
| Jordan | Somalia | |
| Lebanon | Sudan | |
| Morocco | Comoros | |
| Oman | ||
| Qatar | ||
| Palestine | ||
| Tunisia | ||
| United Arab Emirates Kuwait |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Malik, S.D.; Al-Shafai, M.; Abdallah, A.M. The Special Features of Prenatal and Preimplantation Genetic Counseling in Arab Countries. Genes 2022, 13, 167. https://doi.org/10.3390/genes13020167
Malik SD, Al-Shafai M, Abdallah AM. The Special Features of Prenatal and Preimplantation Genetic Counseling in Arab Countries. Genes. 2022; 13(2):167. https://doi.org/10.3390/genes13020167
Chicago/Turabian StyleMalik, Shaza D., Mashael Al-Shafai, and Atiyeh M. Abdallah. 2022. "The Special Features of Prenatal and Preimplantation Genetic Counseling in Arab Countries" Genes 13, no. 2: 167. https://doi.org/10.3390/genes13020167
APA StyleMalik, S. D., Al-Shafai, M., & Abdallah, A. M. (2022). The Special Features of Prenatal and Preimplantation Genetic Counseling in Arab Countries. Genes, 13(2), 167. https://doi.org/10.3390/genes13020167






