Oritavancin a Therapeutic Option for Periprosthetic Joint Infections in Selected Cases: A Comprehensive Review
Abstract
1. Introduction
2. Results and Discissions
2.1. Pharmacokinetics
2.2. In Vitro Activity of Oritavancin Against Biofilms
2.3. The Use in the Field of Periprosthetic Joint Infections
2.4. Safety
2.4.1. Infusion-Related and Hypersensitivity Reactions
2.4.2. Hepatotoxicity and Other Safety Considerations
2.4.3. Drug Interactions and Laboratory Interferences
2.5. Limitations
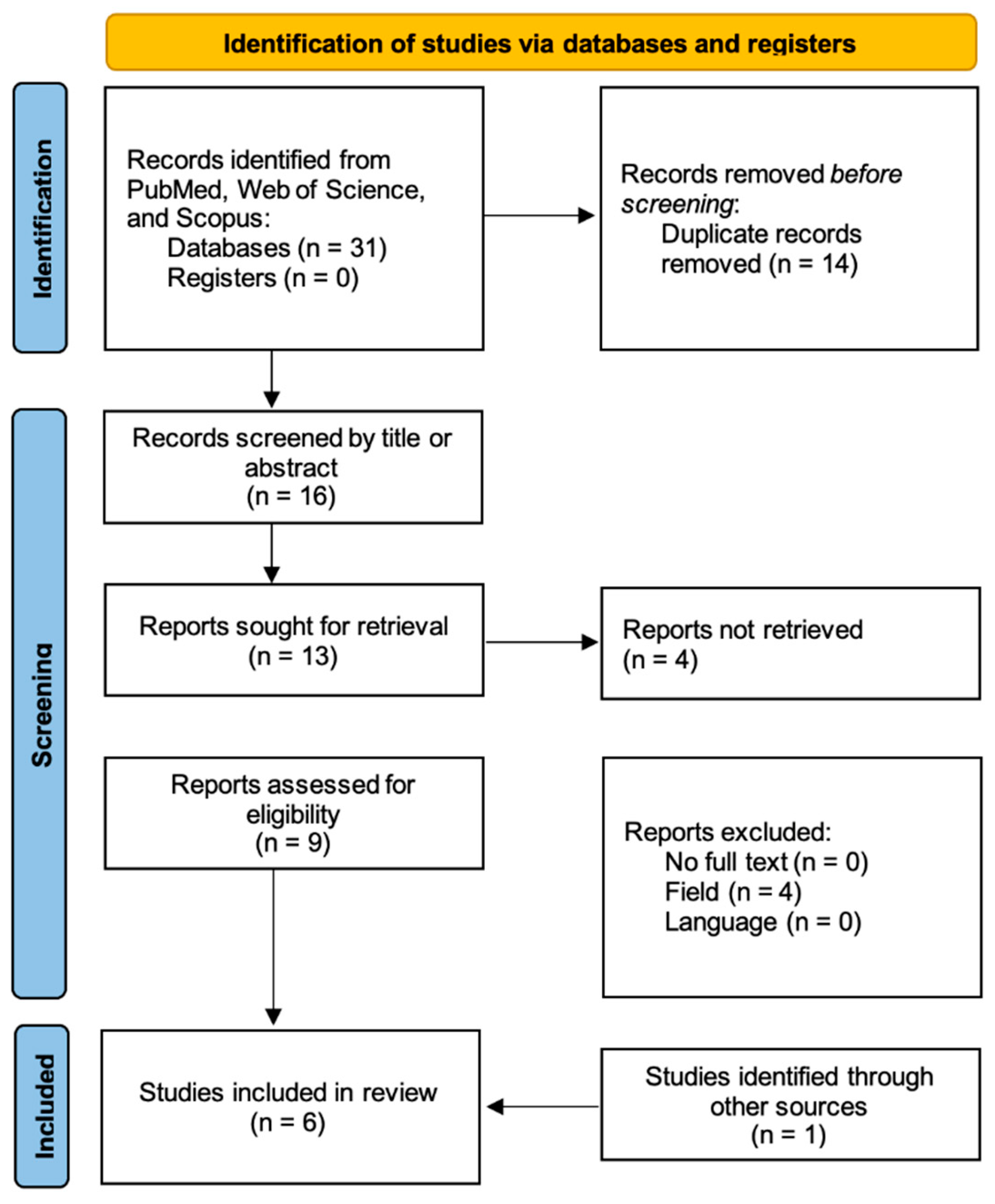
3. Materials and Methods
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| PJIs | periprosthetic joint infections |
| MRSE | methicillin-resistant Staphylococcus epidermidis |
| MRSA | methicillin-resistant Staphylococcus aureus |
| TDM | therapeutic drug monitoring |
References
- van Groesen, E.; Innocenti, P.; Martin, N.I. Recent Advances in the Development of Semisynthetic Glycopeptide Antibiotics: 2014–2022. ACS Infect. Dis. 2022, 8, 1381–1407. [Google Scholar] [CrossRef] [PubMed]
- Zhanel, G.G.; Schweizer, F.; Karlowsky, J.A. Oritavancin: Mechanism of Action. Clin. Infect. Dis. 2012, 54 (Suppl. 3), S214–S219. [Google Scholar] [CrossRef] [PubMed]
- Sigmund, I.K.; Ferry, T.; Sousa, R.; Soriano, A.; Metsemakers, W.-J.; Clauss, M.; Trebse, R.; Wouthuyzen-Bakker, M. Debridement, Antimicrobial Therapy, and Implant Retention (DAIR) as Curative Strategy for Acute Periprosthetic Hip and Knee Infections: A Position Paper of the European Bone & Joint Infection Society (EBJIS). J. Bone Jt. Infect. 2025, 10, 101–138. [Google Scholar] [CrossRef] [PubMed]
- Birlutiu, R.M.; Stoica, C.I.; Russu, O.; Cismasiu, R.S.; Birlutiu, V. Positivity Trends of Bacterial Cultures from Cases of Acute and Chronic Periprosthetic Joint Infections. J. Clin. Med. 2022, 11, 2238. [Google Scholar] [CrossRef]
- Birlutiu, R.M.; Birlutiu, V.; Cismasiu, R.S.; Mihalache, M. BbFISH-Ing in the Sonication Fluid. Medicine 2019, 98, e16501. [Google Scholar] [CrossRef]
- Aftab, M.H.S.; Joseph, T.; Almeida, R.; Sikhauli, N.; Pietrzak, J.R.T. Periprosthetic Joint Infection: A Multifaceted Burden Undermining Arthroplasty Success. Orthop. Rev. Pavia 2025, 17, 138205. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Mercurio, M.; Cofano, E.; Colace, S.; Piro, F.; Cerciello, S.; Galasso, O.; Gasparini, G. Outcomes, Complications, and Eradication Rates of Two-Stage Revision Surgery for Periprosthetic Shoulder, Elbow, Hip, and Knee Infections: A Systematic Review. Prosthesis 2024, 6, 1240–1258. [Google Scholar] [CrossRef]
- Goud, A.L.; Harlianto, N.I.; Ezzafzafi, S.; Veltman, E.S.; Bekkers, J.E.; Van der Wal, B.C. Reinfection rates after one- and two-stage revision surgery for hip and knee arthroplasty: A systematic review and meta-analysis. Arch. Orthop. Trauma. Surg. 2023, 143, 829–838. [Google Scholar] [CrossRef]
- Roman, M.D.; Bocea, B.-A.; Ion, N.-I.-C.; Vorovenci, A.E.; Dragomirescu, D.; Birlutiu, R.-M.; Birlutiu, V.; Fleaca, S.R. Are There Any Changes in the Causative Microorganisms Isolated in the Last Years from Hip and Knee Periprosthetic Joint Infections? Antimicrobial Susceptibility Test Results Analysis. Microorganisms 2023, 11, 116. [Google Scholar] [CrossRef]
- Birlutiu, R.M.; Mihalache, M.; Mihalache, P.; Cismasiu, R.S.; Birlutiu, V. Mid-Term Follow-up Results after Implementing a New Strategy for the Diagnosis and Management of Periprosthetic Joint Infections. BMC Infect. Dis. 2021, 21, 807. [Google Scholar] [CrossRef]
- Dragosloveanu, S.; Birlutiu, R.-M.; Neamtu, B.; Birlutiu, V. Microbiological Profiles, Antibiotic Susceptibility Patterns and the Role of Multidrug-Resistant Organisms in Patients Diagnosed with Periprosthetic Joint Infection over 8 Years: Results from a Single-Center Observational Cohort Study from Romania. Microorganisms 2025, 13, 1168. [Google Scholar] [CrossRef] [PubMed]
- Middleton, R.; Price, A.; Alvand, A. Contemporary outcomes of debridement, antibiotics and implant retention in knee arthroplasty. Ann. Jt. 2022, 7, 9. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Peel, T.N.; Cheng, A.C.; Choong, P.F.M.; Buising, K.L. Early Onset Prosthetic Hip and Knee Joint Infection: Treatment and Outcomes in Victoria, Australia. J. Hosp. Infect. 2012, 82, 248–253. [Google Scholar] [CrossRef] [PubMed]
- Leekha, S.; Terrell, C.L.; Edson, R.S. General Principles of Antimicrobial Therapy. Mayo Clin. Proc. 2011, 86, 156–167. [Google Scholar] [CrossRef]
- Zimmerli, W.; Sendi, P. Orthopaedic Biofilm Infections. APMIS 2017, 125, 353–364. [Google Scholar] [CrossRef]
- Kraus, K.; Mikziński, P.; Widelski, J.; Paluch, E. Prevention and Modern Strategies for Managing Methicillin-Resistant Staphylococcal Infections in Prosthetic Joint Infections (PJIs). Antibiotics 2024, 13, 1151. [Google Scholar] [CrossRef]
- Benito, N.; Franco, M.; Ribera, A.; Soriano, A.; Rodriguez-Pardo, D.; Sorlí, L.; Fresco, G.; Fernández-Sampedro, M.; Dolores del Toro, M.; Guío, L.; et al. Time trends in the aetiology of prosthetic joint infections: A multicentre cohort study. Clin. Microbiol. Infect. 2016, 22, 732.e1–732.e8. [Google Scholar] [CrossRef]
- Espíndola, R.; Vella, V.; Benito, N.; Mur, I.; Tedeschi, S.; Zamparini, E.; Hendriks, J.; Sorlí, L.; Murillo, O.; Soldevila, L.; et al. Incidence, associated disease burden and healthcare utilization due to Staphylococcus aureus prosthetic joint infection in European hospitals: The COMBACTE-NET ARTHR-IS multi-centre study. J. Hosp. Infect. 2023, 142, 9–17. [Google Scholar] [CrossRef]
- La, Y.J.; Kim, Y.C. Successful Treatment of Vancomycin-Resistant Enterococcus species Bone and Joint Infection with Daptomycin Plus Beta Lactam Agents. Infect. Chemother. 2022, 54, 797–802. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Renz, N.; Trebse, R.; Akgün, D.; Perka, C.; Trampuz, A. Enterococcal periprosthetic joint infection: Clinical and microbiological findings from an 8-year retrospective cohort study. BMC Infect. Dis. 2019, 19, 1083. [Google Scholar] [CrossRef]
- Lipoglycopeptides. In The Merck Manual Professional Version; Merck & Co., Inc.: Boston, MA, USA, 2024; Available online: https://www.merckmanuals.com/professional/infectious-diseases/bacteria-and-antibacterial-medications/lipoglycopeptides (accessed on 15 June 2025).
- Hoover, R.K.; Krsak, M.; Molina, K.C.; Shah, K.; Redell, M. Kimyrsa, An Oritavancin-Containing Product: Clinical Study and Review of Properties. Open Forum Infect. Dis. 2022, 9, ofac090. [Google Scholar] [CrossRef]
- Van Hise, N.W.; Chundi, V.; Didwania, V.; Anderson, M.; McKinsey, D.; Roig, I.; Sharma, A.; Petrak, R.M. Treatment of Acute Osteomyelitis with Once-Weekly Oritavancin: A Two-Year, Multicenter, Retrospective Study. Drugs Real World Outcomes 2020, 7, 41–45. [Google Scholar] [CrossRef]
- Bandaranayake, T.D.; Radcliffe, C.; Cvercko, M.; Golden, M.; Hao, R.M. Experience with Expanded Use of Oritavancin in a Tertiary Hospital: Indications, Tolerability and Outcomes. JAC Antimicrob. Resist. 2024, 6, dlae174. [Google Scholar] [CrossRef]
- Carcione, D.; Intra, J.; Andriani, L.; Campanile, F.; Gona, F.; Carletti, S.; Mancini, N.; Brigante, G.; Cattaneo, D.; Baldelli, S.; et al. New Antimicrobials for Gram-Positive Sustained Infections: A Comprehensive Guide for Clinicians. Pharmaceuticals 2023, 16, 1304. [Google Scholar] [CrossRef]
- Yan, Q.; Karau, M.J.; Patel, R. In Vitro Activity of Oritavancin against Biofilms of Staphylococci Isolated from Prosthetic Joint Infection. Diagn. Microbiol. Infect. Dis. 2018, 92, 155–157. [Google Scholar] [CrossRef]
- Yan, Q.; Karau, M.J.; Raval, Y.S.; Patel, R. Evaluation of Oritavancin Combinations with Rifampin, Gentamicin, or Linezolid against Prosthetic Joint Infection-Associated Methicillin-Resistant Staphylococcus Aureus Biofilms by Time-Kill Assays. Antimicrob. Agents Chemother. 2018, 62, 10-1128. [Google Scholar] [CrossRef] [PubMed]
- Krsak, M.; Morrisette, T.; Damioli, L.; Flues, B.; Liu, E.W.; Zhou, A.Y.; Msdi, A.S.; McLeod, C.; Akundi, S.; Redell, M.; et al. Can Oritavancin Be Used for Treatment and/or Suppressive Antimicrobial Therapy of Bone and Joint Infections Caused by Vancomycin-Resistant Enterococcus Faecium? Clin Orthop Relat Res 2025, 483, 1225–1233. [Google Scholar] [CrossRef] [PubMed]
- Buonomo, A.R.; Cattaneo, L.; Viceconte, G.; Calabria, F.; Di Troia, G.; Di Fusco, A.; Mula, J.; Cozzolino, A.; Ametrano, L.; D’Avolio, A.; et al. Long-Term Oritavancin Therapy for Shoulder Prosthetic Joint Infection: A Case Guided by Therapeutic Drug Monitoring (TDM). IDCases 2024, 38, e02105. [Google Scholar] [CrossRef] [PubMed]
- Redell, M.; Sierra-Hoffman, M.; Assi, M.; Bochan, M.; Chansolme, D.; Gandhi, A.; Sheridan, K.; Soosaipillai, I.; Walsh, T.; Massey, J. The CHROME Study, a Real-World Experience of Single- and Multiple-Dose Oritavancin for Treatment of Gram-Positive Infections. Open Forum Infect. Dis. 2019, 6, ofz479. [Google Scholar] [CrossRef]
- Nguyen, J.P.; Contreras, B.X.; Sierra-Hoffman, M.; Saddler, K.; Stevens, M.L.; Castro-Lainez, M.T.; Knox, B.; Deliz, R.J. Successful Treatment of a Prosthetic Hip Infection Due to Enterococcus Faecalis with Sequential Dosing of Oritavancin and Prosthesis Preservation without Prosthetic Joint Surgical Manipulation. IDCases 2020, 22, e00949. [Google Scholar] [CrossRef]
- Antony, S.J.; Cooper, L.G. Use of Oritavancin (Novel New Lipoglycopeptide) in the Treatment of Prosthetic Joint Infections (PJI): A Possible Alternative Novel Approach to a Difficult Problem. Infect. Disord. Drug Targets 2017, 17, 77–80. [Google Scholar] [CrossRef]
- Corey, G.R.; Good, S.; Jiang, H.; Moeck, G.; Wikler, M.; Green, S.; Manos, P.; Keech, R.; Singh, R.; Heller, B.; et al. Single-dose oritavancin versus 7-10 days of vancomycin in the treatment of gram-positive acute bacterial skin and skin structure infections: The SOLO II noninferiority study. Clin. Infect. Dis. 2015, 60, 254–262. [Google Scholar] [CrossRef]
- NICE. Oritavancin for Acute Bacterial Skin and Skin Structure Infections. Evidence Summary [ES39]; National Institute for Health and Care Excellence: London, UK, 2015; Available online: https://www.nice.org.uk/advice/es39/evidence/evidence-review-pdf-11072040301 (accessed on 10 August 2025).
- Medscape. Kimyrsa, Orbactiv (Oritavancin) Dosing, Indications, Interactions, Adverse Effects, and More. Medscape Drug Reference. Available online: https://reference.medscape.com/drug/kimyrsa-orbactiv-oritavancin-999944#3 (accessed on 10 August 2025).
- Melinta Therapeutics, LLC. Orbactiv (oritavancin) Prescribing Information. In Highlights of Prescribing Information and Full Product Details; Melinta Therapeutics: Parsippany, NJ, USA, February 2025; Available online: https://www.orbactiv.com/pdfs/orbactiv-prescribing-information.pdf (accessed on 10 August 2025).
- Saravolatz, L.D.; Stein, G.E. Oritavancin: A Long-Half-Life Lipoglycopeptide. Clin. Infect. Dis. 2015, 61, 627–632. [Google Scholar] [CrossRef]
- U.S. Food and Drug Administration (FDA). Orbactiv (Oritavancin Diphosphate): Warnings and Precautions Updated—Infusion-Related Reactions; FDA Drug Safety Update; FDA: Silver Spring, MD, USA, July–September 2019. Available online: https://www.fda.gov/drugs/fdas-adverse-event-reporting-system-faers/july-september-2019-potential-signals-serious-risksnew-safety-information-identified-fda-adverse (accessed on 10 August 2025).
- U.S. Food and Drug Administration (FDA). Clinical Review: Oritavancin Diphosphate (Orbactiv). In Center for Drug Evaluation and Research: Medical Review NDA 206334 (Original Submission); FDA: Silver Spring, MD, USA, 23 April 2014. Available online: https://www.accessdata.fda.gov/drugsatfda_docs/nda/2014/206334Orig1s000MedR.pdf#:~:text=match%20at%20L682%202xULN,meet%20the%20Hy’s%20law%20criteria (accessed on 10 August 2025).
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, 71. [Google Scholar] [CrossRef]
| Isolate of MRSA | MIC (μg/mL) of a: | MBBC (μg/mL) of a: | ||||||
|---|---|---|---|---|---|---|---|---|
| ORI | RIF | GEN | LZD | ORI | RIF | GEN | LZD | |
| 1 | 0.03 | 0.004 | 0.25 | 2 | 4 | 4 | 1 | >128 |
| 2 | 0.03 | 0.008 | 0.25 | 4 | 4 | 16 | 0.5 | >128 |
| 3 | 0.06 | 0.008 | 0.25 | 2 | 16 | 4 | 2 | >128 |
| 4 | 0.06 | 0.008 | 0.25 | 2 | 4 | 16 | 0.5 | >128 |
| 5 | 0.015 | 0.008 | 0.25 | 2 | 8 | 4 | 2 | >128 |
| 6 | 0.12 | 0.008 | 0.25 | 2 | 16 | 8 | 16 | >128 |
| 7 | 0.06 | 0.004 | 0.25 | 2 | 4 | 0.03 | 0.25 | >128 |
| 8 | 0.015 | 0.008 | 0.12 | 4 | 8 | 16 | 2 | >128 |
| 9 | 0.12 | 0.008 | 1 | 4 | 4 | 8 | 2 | >128 |
| 10 | 0.015 | 0.008 | 0.25 | 4 | 4 | 8 | 4 | >128 |
| Ref. | Study Design | No. of Enrolled Patients | Oritavancin Treatment Protocol | Treatment Outcomes | Follow-Up Duration | Safety Profile of Oritavancin for PJI Cases |
|---|---|---|---|---|---|---|
| [31] | Case report | 1 | 1200 mg intravenous every 7 days ×6 (sole therapy) | Patient mobility/functional status: The patient was ambulating independently without symptoms. | 10 months | Not mentioned |
| [24] | Retrospective cohort, single-center | 5 | 1200 mg intravenous | Specific outcomes for the individual PJI cases were not detailed | - Total duration of patient follow-up: 1 year after the last dose of oritavancin | Three experienced adverse reactions: a 56-year-old female developed itching, hives, and throat swelling during her first infusion, which required cessation of therapy; a 60-year-old female had a rash after her third dose, which appeared post-infusion; and a 46-year-old female experienced shaking, chills, vomiting, and back pain during her third infusion, necessitating immediate discontinuation. |
| [32] | Case series (single center) | 2 | 1200 mg intravenous, multidose | Both patients successfully treated | Insufficient follow-up information | Not mentioned |
| [29] | Case report | 1 | 1200 mg of oritavancin, 10 doses until the report was published, the patient is under long-lasting suppressive antimicrobial therapy with 1 dose every 28 days. | No pain with completely recovered joint mobility, complete healing of the fistula and the disappearance of the underlying abscess. | 28 weeks | None |
| [28] | Retrospective cohort, Case series, Multicenter (number of centers not specified) | 2 | 1st case 1200 mg of oritavancin, 8 doses 2nd case 1200 mg/month for 22 months | 1st case—recurrence of knee stiffness and persistent VRE infection. 2nd case—sustained symptom-free status | 195 days/22 months | None |
| [30] | Retrospective cohort study; Multicenter study | 3 | 2 patients 1200 mg single dose, 1 patient 1200 mg 2 doses | 2 cured patients | Not specifically mentioned | None |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Birlutiu, R.-M.; Birlutiu, V. Oritavancin a Therapeutic Option for Periprosthetic Joint Infections in Selected Cases: A Comprehensive Review. Pharmaceuticals 2025, 18, 1217. https://doi.org/10.3390/ph18081217
Birlutiu R-M, Birlutiu V. Oritavancin a Therapeutic Option for Periprosthetic Joint Infections in Selected Cases: A Comprehensive Review. Pharmaceuticals. 2025; 18(8):1217. https://doi.org/10.3390/ph18081217
Chicago/Turabian StyleBirlutiu, Rares-Mircea, and Victoria Birlutiu. 2025. "Oritavancin a Therapeutic Option for Periprosthetic Joint Infections in Selected Cases: A Comprehensive Review" Pharmaceuticals 18, no. 8: 1217. https://doi.org/10.3390/ph18081217
APA StyleBirlutiu, R.-M., & Birlutiu, V. (2025). Oritavancin a Therapeutic Option for Periprosthetic Joint Infections in Selected Cases: A Comprehensive Review. Pharmaceuticals, 18(8), 1217. https://doi.org/10.3390/ph18081217








