N-Acetylcysteine Treatment Restores the Protective Effect of Heart Ischemic Postconditioning in a Murine Model in the Early Stages of Atherosclerosis
Abstract
1. Introduction
2. Results
3. Discussion
4. Materials and Methods
4.1. Animal Care
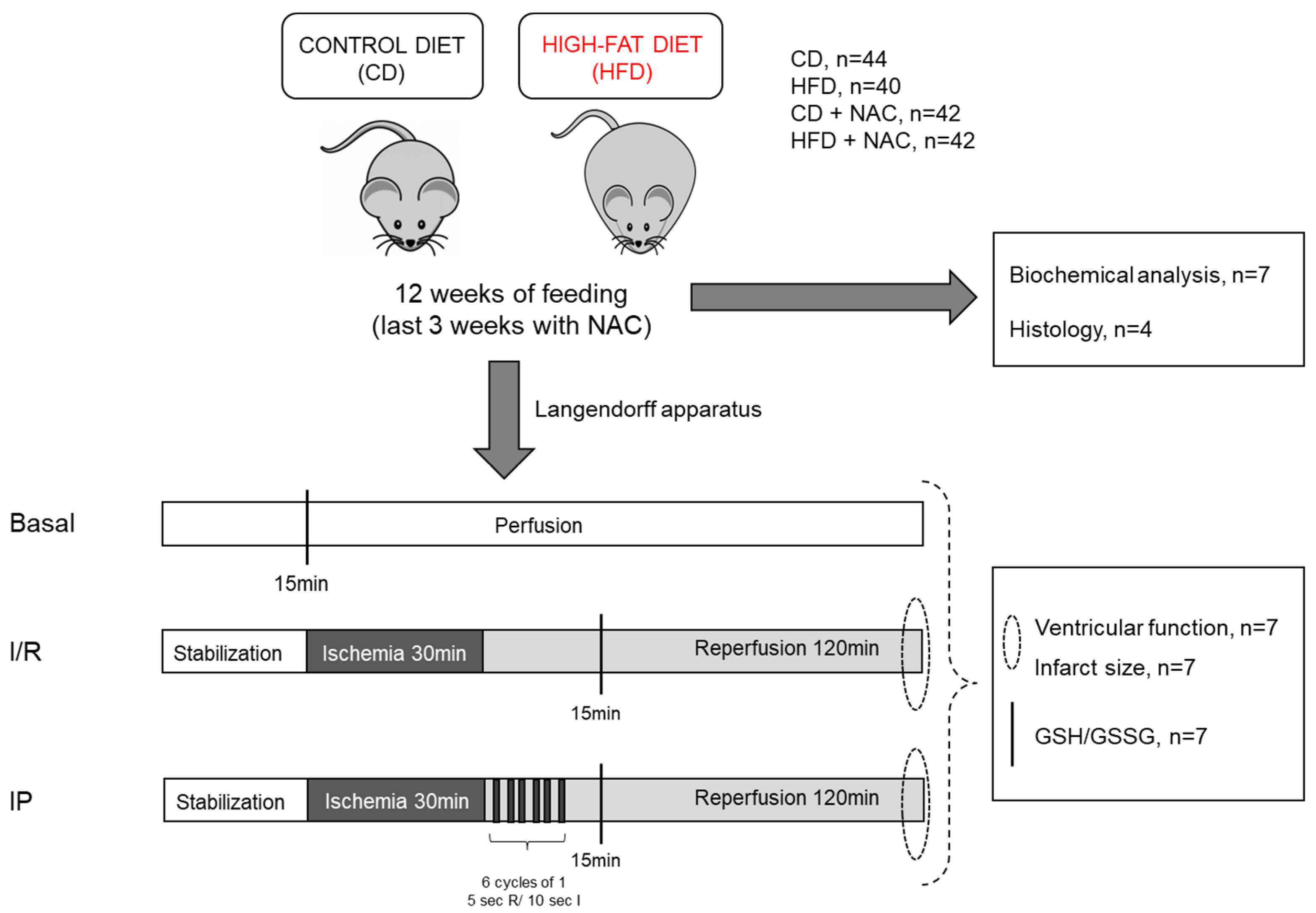
4.2. Experimental Protocols
4.3. Isolated Mouse Heart Perfusion Protocol
4.4. Ventricular Function
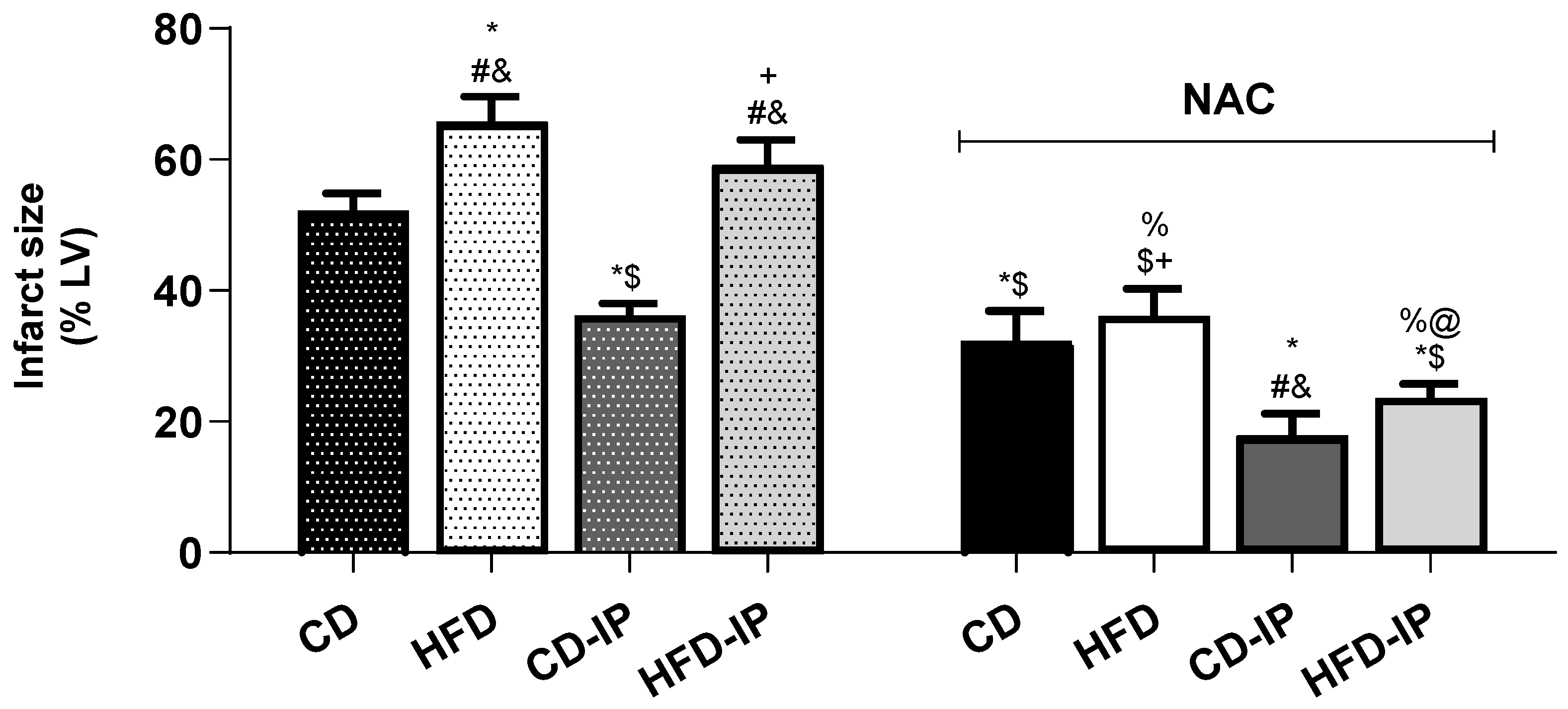
4.5. Infarct Size Measurement
4.6. Biochemical Analyses
4.7. Histological Analysis
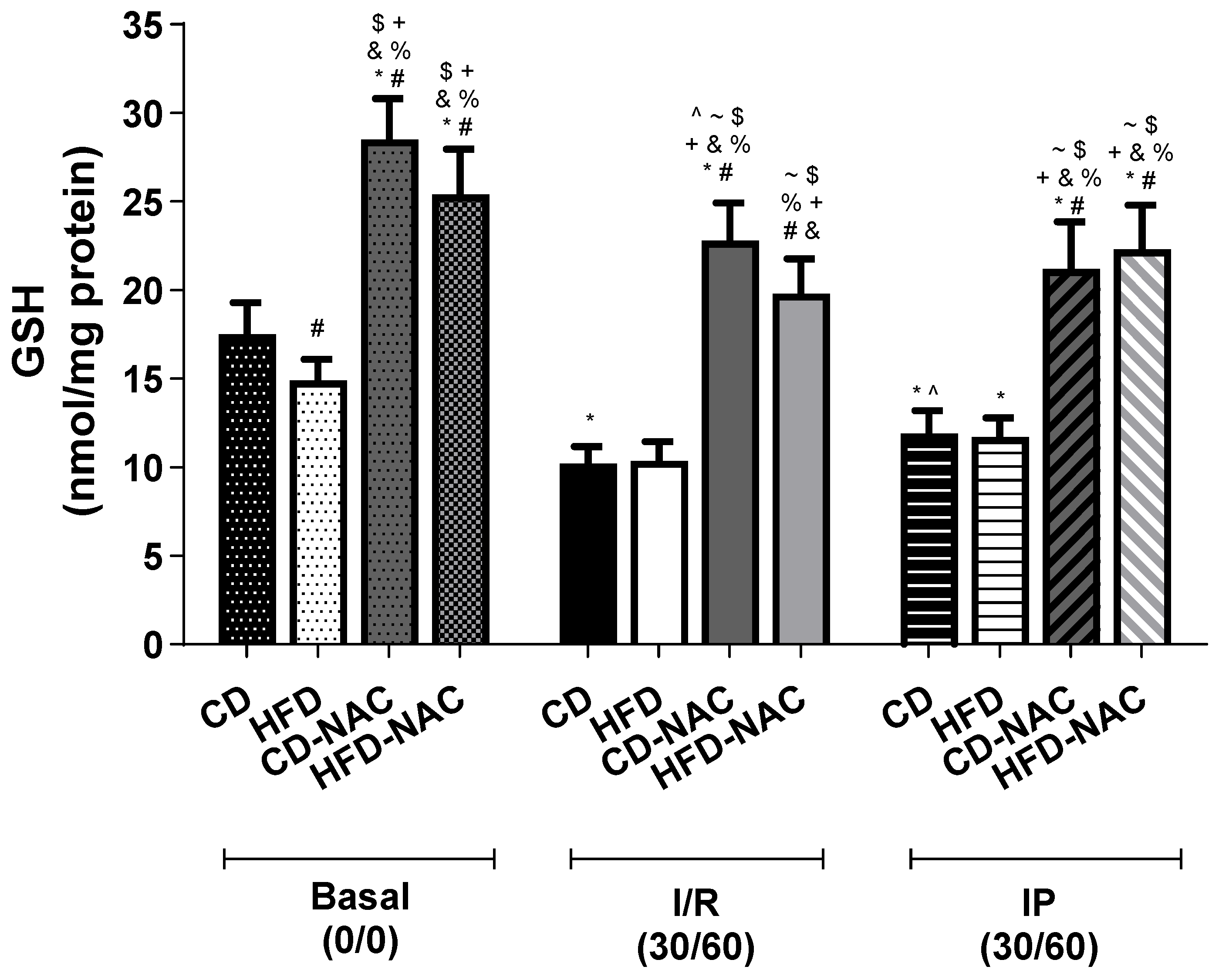
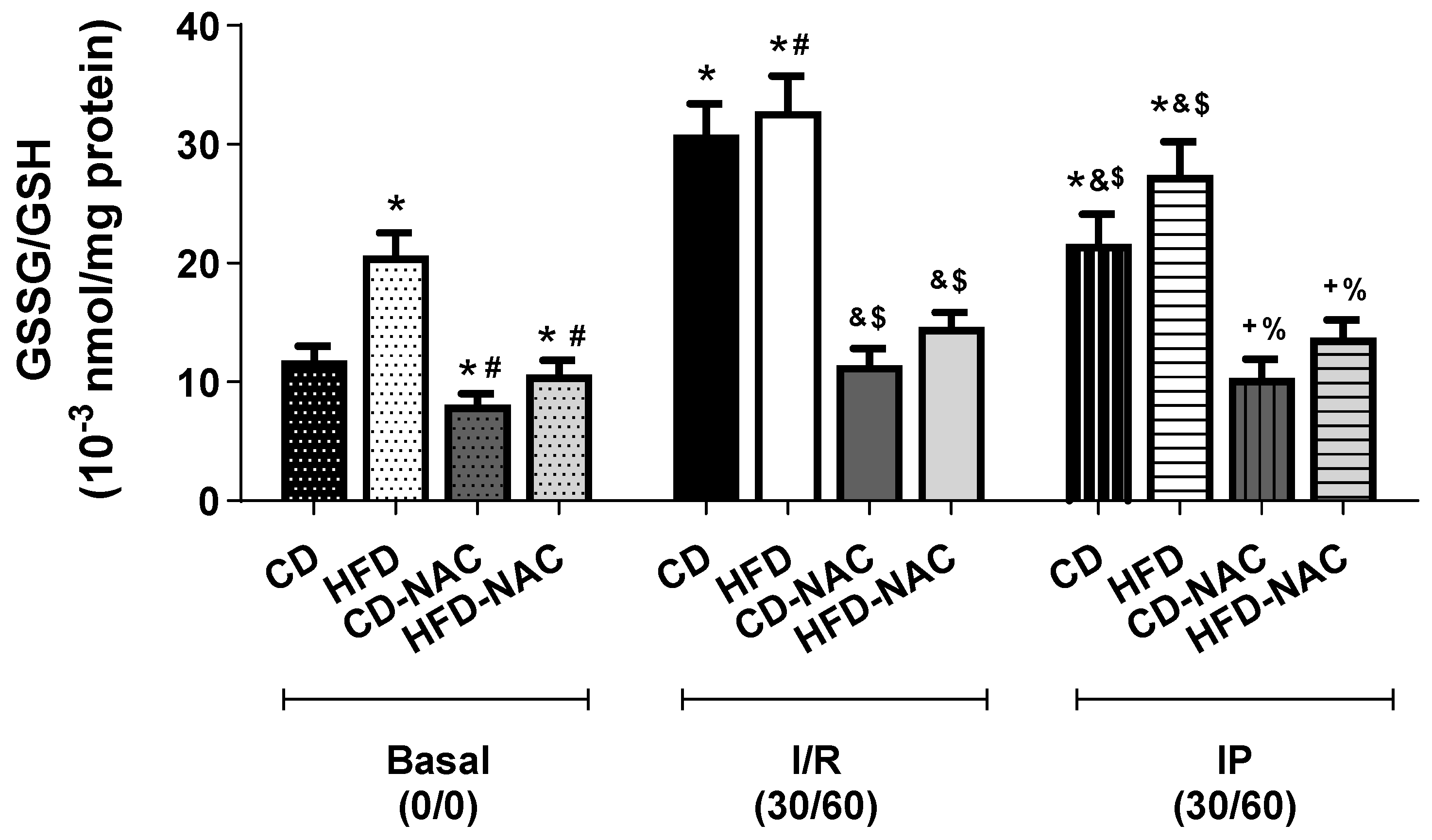
4.8. Reduced (GSH) and Oxidized (GSSG) Glutathione Levels
4.9. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| AMI | acute myocardial infarction |
| CD | control diet |
| HFD | high-fat diet |
| GSH | reduced glutathione |
| GSSG | oxidized glutathione |
| IP | ischemic postconditioning |
| I/R | ischemia/reperfusion |
| NAC | N-acetylcysteine |
| ROS | reactive oxygen species |
References
- Alpert, M.A.; Lavie, C.J.; Agrawal, H.; Aggarwal, K.B.; Kumar, S.A. Obesity and heart failure: Epidemiology, pathophysiology, clinical manifestations, and management. Transl. Res. 2014, 164, 345–356. [Google Scholar] [CrossRef]
- Yellon, D.M.; Hausenloy, D.J. Myocardial reperfusion injury. N. Engl. J. Med. 2007, 357, 1121–1135. [Google Scholar] [CrossRef] [PubMed]
- Ferdinandy, P.; Hausenloy, D.J.; Heusch, G.; Baxter, G.F.; Schulz, R. Interaction of risk factors, comorbidities, and comedications with ischemia/reperfusion injury and cardioprotection by preconditioning, postconditioning, and remote conditioning. Pharmacol. Rev. 2007, 66, 1142–1174. [Google Scholar] [CrossRef] [PubMed]
- Donato, M.; D’Annunzio, V.; Berg, G.; Gonzalez, G.; Schreier, L.; Morales, C.; Wikinski, R.L.; Gelpi, R.J. Ischemic postconditioning reduces infarct size by activation of A1 receptors and K+ATP channels in both normal and hypercholesterolemic rabbits. J. Cardiovasc. Pharmacol. 2007, 49, 287–292. [Google Scholar] [CrossRef] [PubMed]
- Mazo, T.; D’Annunzio, V.; Zaobornyj, T.; Perez, V.; Gomez, A.; Berg, G.; Barchuk, M.; Ossani, G.; Martinefski, M.; Tripodi, V.; et al. High-fat diet abolishes the cardioprotective effects of ischemic postconditioning in murine models despite increased thioredoxin-1 levels. Mol. Cell. Biochem. 2019, 452, 153–166. [Google Scholar] [CrossRef]
- Argentine FRICAS (Factores de Riesgo Coronario en America del Sur) Investigators; Ciruzzi, M.; Schargrodsky, H.; Rozlosnik, J.; Pramparo, P.; Delmonte, H.; Rudich, V.; Piskorz, D.; Negri Soifer, S.; La Vecchia, C. Frequency of family history of acute myocardial infarction in patients with acute E, myocardial infarction. Am. J. Cardiol. 1997, 80, 122–127. [Google Scholar] [CrossRef]
- Gao, S.; Zhao, D.; Wang, M.; Zhao, F.; Han, X.; Qi, Y.; Liu, J. Association Between Circulating Oxidized LDL and Atherosclerotic Cardiovascular Disease: A Meta-Analysis of Observational Studies. Can. J. Cardiol. 2017, 33, 1624–1632. [Google Scholar] [CrossRef]
- Schmitt, B.; Vicenzi, M.; Garrel, C.; Denis, F.M. Effects of Nacetylcysteine, oral glutathione (GSH) and a novel sublingual form of GSH on oxidative stress markers: A comparative crossover study. Redox Biol. 2015, 6, 198–205. [Google Scholar] [CrossRef]
- Atkuri, K.R.; Mantovani, J.J.; Herzenberg, L.A.; Herzenberg, L.A. N-Acetylcysteine—A safe antidote for cysteine/glutathione deficiency. Curr. Opin. Pharmacol. 2007, 7, 355–359. [Google Scholar] [CrossRef]
- Margaritelis, N.V.; Cobley, J.N.; Paschalis, V.; Veskoukis, A.S.; Theodorou, A.A.; Kyparos, A.; Nikolaidis, M.G. Principles for integrating reactive species into in vivo biological processes: Examples from exercise physiology. Cell. Signal. 2016, 28, 256–271. [Google Scholar] [CrossRef]
- Zhou, D.; Yang, Y.; Chen, J.; Zhou, J.; He, J.; Liu, D.; Zhang, A.; Yuan, B.; Jiang, Y.; Xia, W.; et al. N-acetylcysteine Protects Against Myocardial Ischemia-Reperfusion Injury Through Anti-ferroptosis in Type 1 Diabetic Mice. Cardiovasc. Toxicol. 2024, 24, 481–498. [Google Scholar] [CrossRef] [PubMed]
- San-Martín-Martínez, D.; Serrano-Lemus, D.; Cornejo, V.; Gajardo, A.I.J.; Rodrigo, R. Pharmacological Basis for Abrogating Myocardial Reperfusion Injury Through a Multi-Target Combined Antioxidant Therapy. Clin. Pharmacokinet. 2022, 61, 1203–1218. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Z.Q.; Corvera, J.S.; Halkos, M.E.; Kerendi, F.; Wang, N.P.; Guyton, R.A.; Vinten-Johansen, J. Inhibition of myocardial injury by ischemic postconditioning during reperfusion: Comparison with ischemic preconditioning. Am. J. Physiol. Heart Circ. Physiol. 2003, 285, H579–H588. [Google Scholar] [CrossRef] [PubMed]
- Donato, M.; Evelson, P.; Gelpi, R.J. Protecting the heart from ischemia/reperfusion injury: An update on remote ischemic preconditioning and postconditioning. Curr. Opin. Cardiol. 2017, 32, 784–790. [Google Scholar] [CrossRef]
- Ludmer, P.L.; Selwyn, A.P.; Shook, T.L.; Wayne, R.R.; Mudge, G.H.; Alexander, R.W.; Ganz, P. Paradoxical vasoconstriction induced by acetylcholine in atherosclerotic coronary arteries. N. Engl. J. Med. 1986, 315, 1046–1051. [Google Scholar] [CrossRef]
- Egashira, K.; Inou, T.; Hirooka, Y.; Yamada, A.; Maruoka, Y.; Kai, H.; Sugimachi, M.; Suzuki, S.; Takeshita, A. Impaired coronary blood flow response to acetylcholine in patients with coronary risk factors and proximal atherosclerotic lesions. J. Clin. Investig. 1993, 91, 29–37. [Google Scholar] [CrossRef]
- Paigen, B.; Morrow, A.; Brandon, C.; Mitchell, D.; Holmes, P. Variation in susceptibility to atherosclerosis among inbred strains of mice. Atherosclerosis 1985, 57, 65–73. [Google Scholar] [CrossRef]
- Montgomery, M.; Hallahan, N.; Brown, S.; Liu, M.; Mitchell, T.W.; Cooney, G.J.; Turner, N. Mouse strain-dependent variation in obesity and glucose homeostasis in response to high-fat feeding. Diabetologia 2013, 56, 1129–1139. [Google Scholar] [CrossRef]
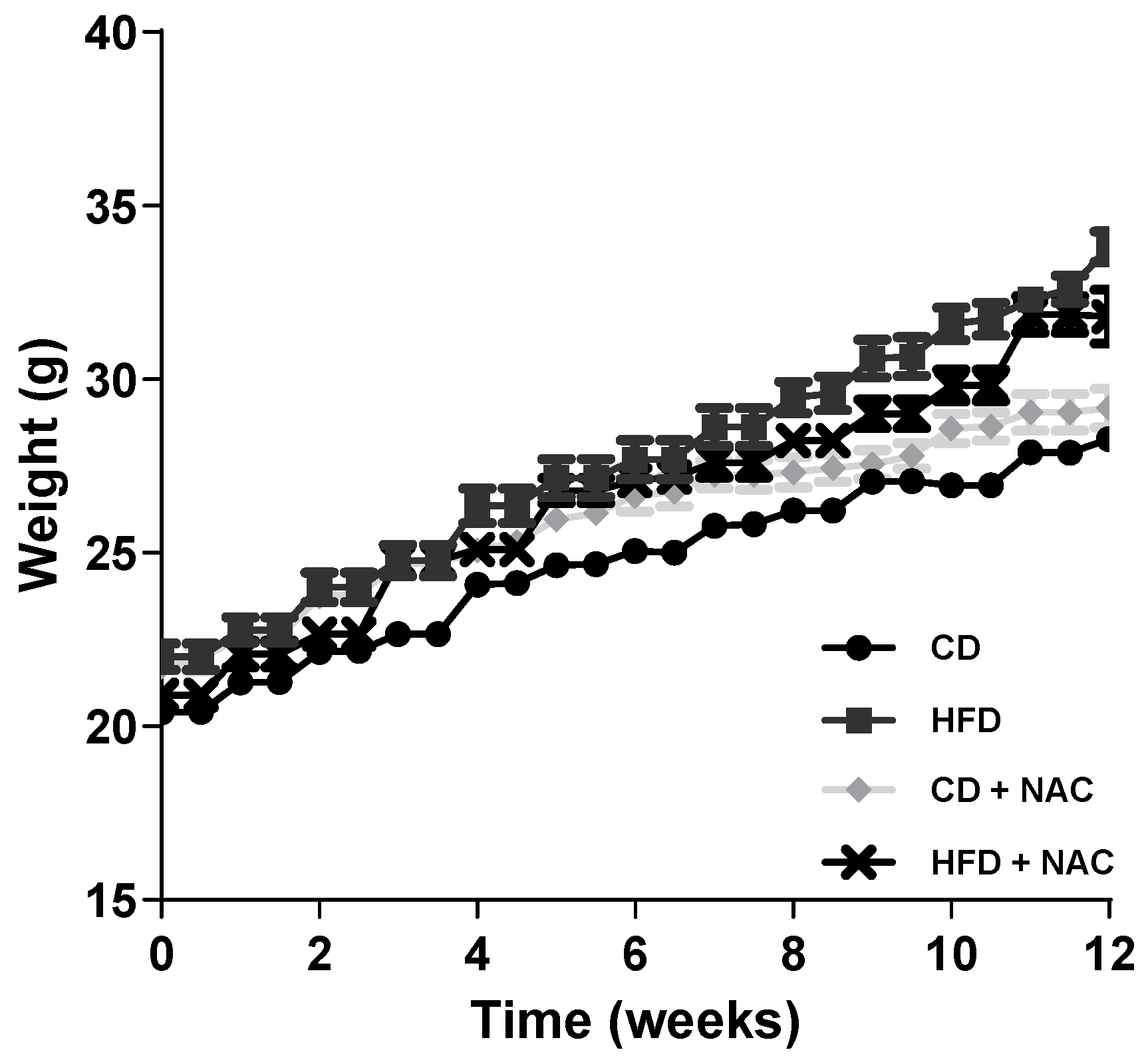
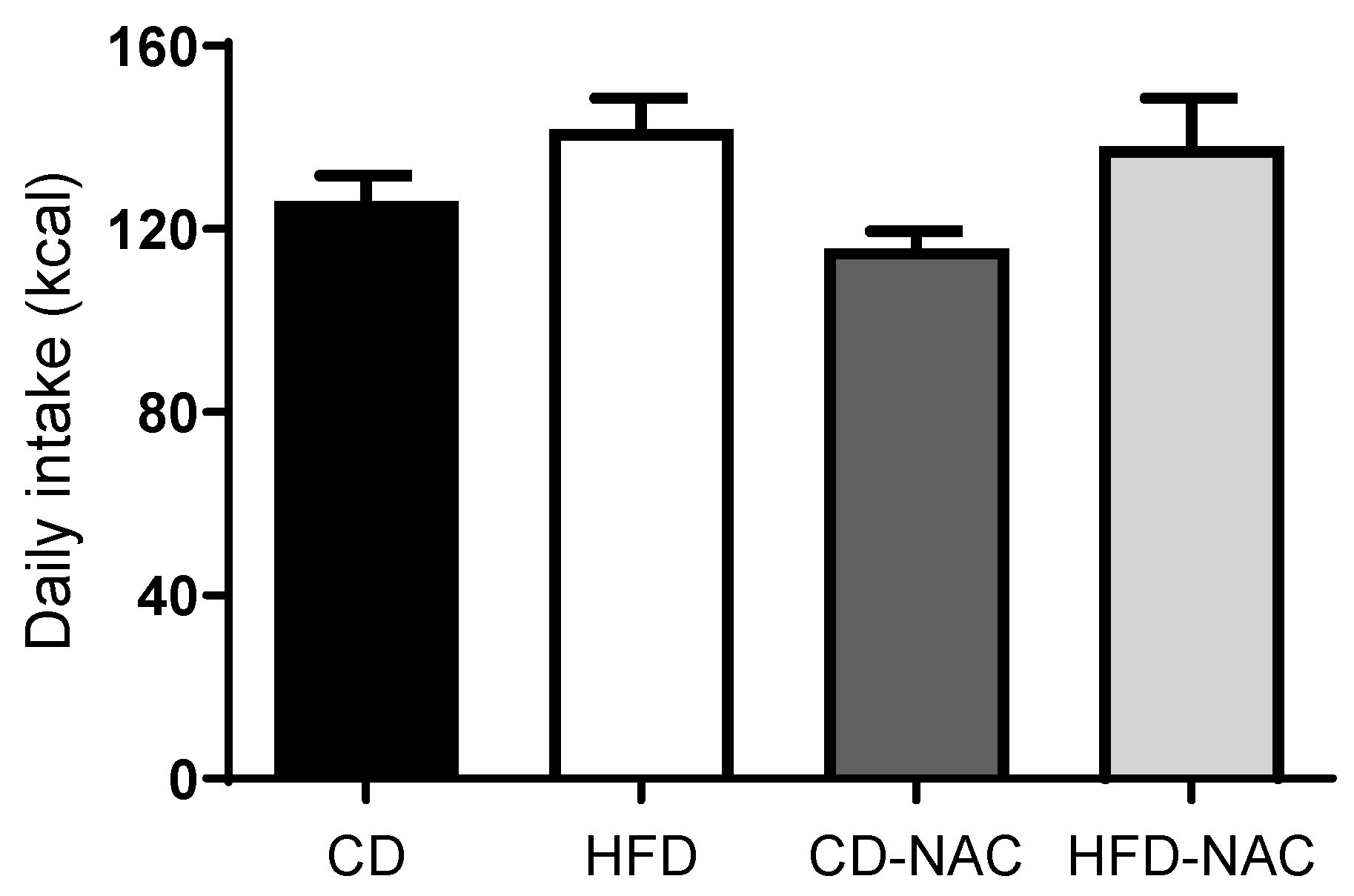
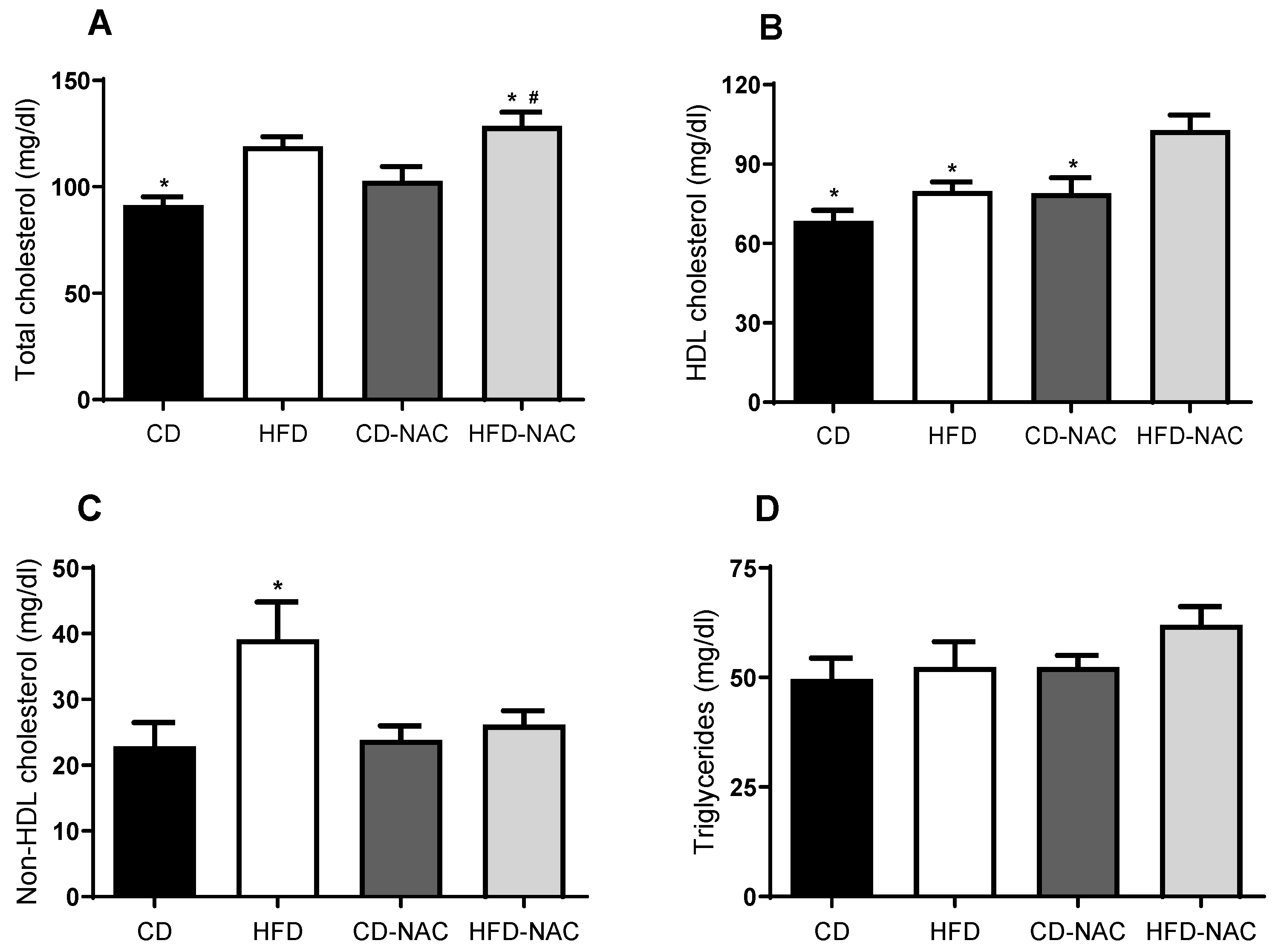
- Lin, C.C.; Yin, M.C. Effects of cysteine-containing compounds on biosynthesis of triacylglycerol and cholesterol and anti-oxidative protection in liver from mice consuming a high-fat diet. Br. J. Nutr. 2008, 99, 37–43. [Google Scholar] [CrossRef]
- Lin, C.C.; Yin, M.C.; Hsu, C.C.; Lin, M.P. Effect of five cysteine-containing compounds on three lipogenic enzymes in Balb/cA mice consuming a high saturated fat diet. Lipids 2004, 39, 843–848. [Google Scholar] [CrossRef]
- Nie, J.; Ngokana, L.D.; Kou, J.; Zhao, Y.; Tu, J.; Ji, H.; Tan, P.; Zhao, T.; Cao, Y.; Wu, Z.; et al. Low-dose ethanol intake prevents high-fat diet-induced adverse cardiovascular events in mice. Food Funct. 2020, 11, 3549–3562. [Google Scholar] [CrossRef] [PubMed]
- Korou, L.M.; Agrogiannis, G.; Pantopoulou, A.; Vlachos, I.S.; Iliopoulos, D.; Karatzas, T.; Perrea, D.N. Comparative antilipidemic effect of N-acetylcysteine and sesame oil administration in diet-induced hypercholesterolemic mice. Lipids Health Dis. 2010, 9, 23. [Google Scholar] [CrossRef] [PubMed]
- Diniz, Y.S.; Rocha, K.K.; Souza, G.A.; Galhardi, C.M.; Ebaid, G.M.; Rodrigues, H.G.; Novelli Filho, J.L.; Cicogna, A.C.; Novelli, E.L. Effects of N-acetylcysteine on sucrose-rich diet-induced hyperglycaemia, dyslipidemia and oxidative stress in rats. Eur. J. Pharmacol. 2006, 543, 151–157. [Google Scholar] [CrossRef] [PubMed]
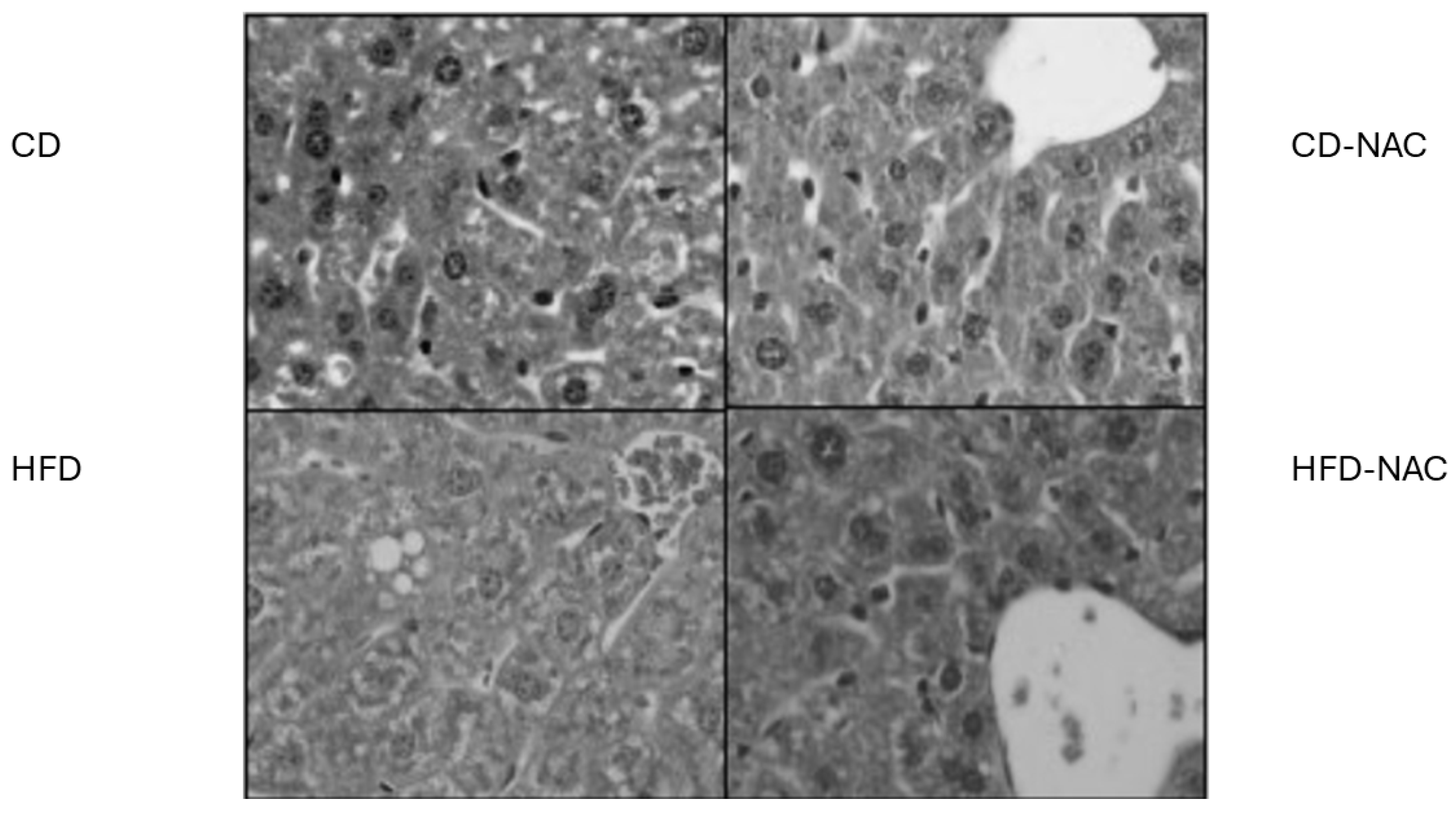
- El-Lakkany, N.M.; Seif El-Din, S.H.; Sabra, A.A.; Hammam, O.A.; Ebeid, F.A. Co-administration of metformin and N-acetylcysteine with dietary control improves the biochemical and histological manifestations in rats with non-alcoholic fatty liver. Res. Pharm. Sci. 2016, 11, 374–382. [Google Scholar] [CrossRef] [PubMed]
- Brizzi, P.; Tonolo, G.; Carusillo, F.; Malaguarnera, M.; Maioli, M.; Musumeci, S. Plasma lipid composition and LDL oxidation. Clin. Chem. Lab. Med. 2003, 41, 56–60. [Google Scholar] [CrossRef]
- van der Heijden, R.A.; Sheedfar, F.; Morrison, M.C.; Hommelberg, P.P.; Kor, D.; Kloosterhuis, N.J.; Gruben, N.; Youssef, S.A.; de Bruin, A.; Hofker, M.H.; et al. High-fat diet induced obesity primes inflammation in adipose tissue prior to liver in C57BL/6j mice. Aging 2015, 7, 256–268. [Google Scholar] [CrossRef] [PubMed]
- Ma, Y.; Gao, M.; Liu, D. N-acetylcysteine Protects Mice from High Fat Diet-induced Metabolic Disorders. Pharm. Res. 2016, 33, 2033–2042. [Google Scholar] [CrossRef]
- Korou, L.M.; Agrogiannis, G.; Koros, C.; Kitraki, E.; Vlachos, I.S.; Tzanetakou, I.; Karatzas, T.; Pergialiotis, V.; Dimitroulis, D.; Perrea, D.N. Impact of N-acetylcysteine and sesame oil on lipid metabolism and hypothalamic-pituitary-adrenal axis homeostasis in middle-aged hypercholesterolemic mice. Sci. Rep. 2014, 28, 6806. [Google Scholar] [CrossRef]
- Hang, W.; Shu, H.; Wen, Z.; Liu, J.; Jin, Z.; Shi, Z.; Chen, C.; Wang, D.W. N-Acetyl Cysteine Ameliorates High-Fat Diet-Induced Nonalcoholic Fatty Liver Disease and Intracellular Triglyceride Accumulation by Preserving Mitochondrial Function. Front. Pharmacol. 2021, 12, 636204. [Google Scholar] [CrossRef]
- Cohen, M.V.; Yang, X.M.; Neumann, T.; Heusch, G.; Downey, J.M. Favorable remodeling enhances recovery of regional myocardial function in the weeks after infarction in ischemically preconditioned hearts. Circulation 2000, 102, 579–583. [Google Scholar] [CrossRef]
- D’Annunzio, V.; Perez, V.; Boveris, A.; Gelpi, R.J.; Poderoso, J.J. Role of thioredoxin-1 in ischemic preconditioning, postconditioning and aged ischemic hearts. Pharmacol. Res. 2016, 109, 24–31. [Google Scholar] [CrossRef] [PubMed]
- D’Annunzio, V.; Donato, M.; Sabán, M.; Sanguinetti, S.M.; Wikinski, R.L.; Gelpi, R.J. Hypercholesterolemia attenuates postischemic ventricular dysfunction in the isolated rabbit heart. Mol. Cell. Biochem. 2005, 273, 137–143. [Google Scholar] [CrossRef] [PubMed]
- Perez, V.; D’Annunzio, V.; Valdez, L.B.; Zaobornyj, T.; Bombicino, S.; Mazo, T.; Carbajosa, N.L.; Gironacci, M.M.; Boveris, A.; Sadoshima, J.; et al. Thioredoxin-1 Attenuates Ventricular and Mitochondrial Postischemic Dysfunction in the Stunned Myocardium of Transgenic Mice. Antiox. Red. Signal. 2016, 25, 78–88. [Google Scholar] [CrossRef]
- Buchholz, B.; Kelly, J.; Muñoz, M.; Bernatené, E.A.; Méndez Diodati, N.; González Maglio, D.H.; Dominici, F.P.; Gelpi, R.J. Vagal stimulation mimics preconditioning and postconditioning of ischemic myocardium in mice by activating different protection mechanisms. Am. J. Physiol. Heart Circ. Physiol. 2018, 314, H1289–H1297. [Google Scholar] [CrossRef]
- Andreadou, I.; Iliodromitis, E.K.; Lazou, A.; Görbe, A.; Giricz, Z.; Schulz, R.; Ferdinandy, P. Effect of hypercholesterolaemia on myocardial function, ischaemia-reperfusion injury and cardioprotection by preconditioning, postconditioning and remote conditioning. Br. J. Pharmacol. 2017, 174, 1555–1569. [Google Scholar] [CrossRef]
- Kupai, K.; Csonka, C.; Fekete, V.; Odendaal, L.; van Rooyen, J.; Marais, D.W.; Csont, T.; Ferdinandy, P. Cholesterol diet-induced hyperlipidemia impairs the cardioprotective effect of postconditioning: Role of peroxynitrite. Am. J. Physiol. Heart Circ. Physiol. 2009, 297, H1729–H1735. [Google Scholar] [CrossRef]
- Ueda, Y.; Kitakaze, M.; Komamura, K.; Minamino, T.; Asanuma, H.; Sato, H.; Kuzuya, T.; Takeda, H.; Hori, M. Pravastatin restored the infarct size-limiting effect of ischemic preconditioning blunted by hypercholesterolemia in the rabbit model of myocardial infarction. J. Am. Coll. Cardiol. 1999, 34, 2120–2125. [Google Scholar] [CrossRef] [PubMed]
- Abe, M.; Takiguchi, Y.; Ichimaru, S.; Tsuchiya, K.; Wada, K. Comparison of the protective effect of N-acetylcysteine by different treatments on rat myocardial ischemia-reperfusion injury. J. Pharmacol. Sci. 2008, 106, 571–577. [Google Scholar] [CrossRef]
- Wang, T.; Mao, X.; Li, H.; Qiao, S.; Xu, A.; Wang, J.; Lei, S.; Liu, Z.; Ng, K.F.; Wong, G.T.; et al. N-Acetylcysteine and allopurinol up-regulated the Jak/STAT3 and PI3K/Akt pathways via adiponectin and attenuated myocardial postischemic injury in diabetes. Free Rad. Biol. Med. 2013, 63, 291–303. [Google Scholar] [CrossRef]
- Nagoor Meeran, M.F.; Stanely Mainzen Prince, P.; Hidhayath Basha, R. Preventive effects of N-acetyl cysteine on lipids, lipoproteins and myocardial infarct size in isoproterenol induced myocardial infarcted rats: An in vivo and in vitro study. Eur. J. Pharmacol. 2012, 677, 116–122. [Google Scholar] [CrossRef]
- Britto, R.M.; Silva-Neto, J.A.D.; Mesquita, T.R.R.; Vasconcelos, C.M.L.; de Almeida, G.K.M.; Jesus, I.C.G.; Santos, P.H.D.; Souza, D.S.; Miguel-Dos-Santos, R.; de Sá, L.A.; et al. Myrtenol protects against myocardial ischemia-reperfusion injury through antioxidant and anti-apoptotic dependent mechanisms. Food Chem. Toxicol. 2018, 111, 557–566. [Google Scholar] [CrossRef] [PubMed]
- Pasupathy, S.; Tavella, R.; Grover, S.; Raman, B.; Procter, N.E.K.; Du, Y.T.; Mahadavan, G.; Stafford, I.; Heresztyn, T.; Holmes, A.; et al. Early Use of N-acetylcysteine With Nitrate Therapy in Patients Undergoing Primary Percutaneous Coronary Intervention for ST-Segment-Elevation Myocardial Infarction Reduces Myocardial Infarct Size (the NACIAM Trial [N-acetylcysteine in Acute Myocardial Infarction]). Circulation 2017, 136, 894–903. [Google Scholar] [PubMed]
- Cadenas, S. ROS and redox signaling in myocardial ischemia-reperfusion injury and cardioprotection. Free Radic. Biol. Med. 2018, 117, 76–89. [Google Scholar] [CrossRef]
- Dhalla, N.S.; Ostadal, P.; Tappia, P.S. Involvement of Oxidative Stress and Antioxidants in Modification of Cardiac Dysfunction Due to Ischemia-Reperfusion Injury. Antioxidants 2025, 14, 340. [Google Scholar] [CrossRef]
- Ommati, M.M.; Amjadinia, A.; Mousavi, K.; Azarpira, N.; Jamshidzadeh, A.; Heidari, R. N-acetyl cysteine treatment mitigates biomarkers of oxidative stress in different tissues of bile duct ligated rats. Stress 2021, 24, 213–228. [Google Scholar] [CrossRef] [PubMed]
- Kumar, P.; Osahon, O.W.; Sekhar, R.V. GlyNAC (Glycine and N-Acetylcysteine) Supplementation in Mice Increases Length of Life by Correcting Glutathione Deficiency, Oxidative Stress, Mitochondrial Dysfunction, Abnormalities in Mitophagy and Nutrient Sensing, and Genomic Damage. Nutrients 2022, 14, 1114. [Google Scholar] [CrossRef]
- Aldini, G.; Altomare, A.; Baron, G.; Vistoli, G.; Carini, M.; Borsani, L. N-Acetylcysteine as an antioxidant and disulphide breaking agent: The reasons why. Free Radic. Res. 2018, 52, 751–762. [Google Scholar] [CrossRef]
- Grundy, S.M. Atherogenic dyslipidemia associated with metabolic syndrome and insulin resistance. Clin. Cornerstone 2006, 8, S21–S27. [Google Scholar] [CrossRef]
- Paschalis, V.; Theodorou, A.A.; Margaritelis, N.V.; Kyparos, A.; Nikolaidis, M.G. N-acetylcysteine supplementation increases exercise performance and reduces oxidative stress only in individuals with low levels of glutathione. Free Radic. Biol. Med. 2018, 115, 288–297. [Google Scholar] [CrossRef]
- Ait Abderrahim, L.; Taïbi, K.; Abderrahim, N.A.; Alomery, A.M.; Abdellah, F.; Alhazmi, A.S.; Aljassabi, S. Protective effects of melatonin and N-acetyl cysteine against oxidative stress induced by microcystin-LR on cardiac muscle tissue. Toxicon 2019, 169, 38–44. [Google Scholar] [CrossRef]
- Rodriguez, B.M.; Khouzami, L.; Decostre, V.; Varnous, S.; Pekovic-Vaughan, V.; Hutchison, C.J.; Pecker, F.; Bonne, G.; Muchir, A. N-acetyl cysteine alleviates oxidative stress and protects mice from dilated cardiomyopathy caused by mutations in nuclear A-type lamins gene. Hum. Mol. Genet. 2018, 27, 3353–3360. [Google Scholar] [CrossRef] [PubMed]
- Jones, D.P. Redefining oxidative stress. Antioxid. Redox Signal. 2006, 8, 1865–1879. [Google Scholar] [CrossRef]
- Perez, V.; Zaobornyj, T.; Vico, T.; Vanasco, V.; Marchini, T.; Godoy, E.; Alvarez, S.; Evelson, P.; Donato, M.; Gelpi, R.J.; et al. Middle-age abolishes cardioprotection conferred by thioredoxin-1 in mice. Arch. Biochem. Biophys. 2024, 753, 109880. [Google Scholar] [CrossRef]
- Hausenloy, D.J.; Yellon, D.M. Ischaemic conditioning and reperfusion injury. Nat. Rev. Cardiol. 2016, 13, 193–209. [Google Scholar] [CrossRef] [PubMed]
- Ong, S.B.; Dongworth, R.K.; Cabrera-Fuentes, H.A.; Hausenloy, D.J. Role of the MPTP in conditioning the heart—Translatability and mechanism. Br. J. Pharmacol. 2015, 172, 2074–2084. [Google Scholar] [CrossRef] [PubMed]
- Cohen, M.V.; Yang, X.M.; Downey, J.M. The pH hypothesis of postconditioning: Staccato reperfusion reintroduces oxygen and perpetuates myocardial acidosis. Circulation 2007, 115, 1895–1903. [Google Scholar] [CrossRef]
- D’Annunzio, V.; Perez, V.; Mazo, T.; Muñoz, M.C.; Dominici, F.P.; Carreras, M.C.; Poderoso, J.J.; Sadoshima, J.; Gelpi, R.J. Loss of myocardial protection against myocardial infarction in middle-aged transgenic mice overexpressing cardiac thioredoxin-1. Oncotarget 2016, 7, 11889–11898. [Google Scholar] [CrossRef]
- Zaobornyj, T.; Mazo, T.; Perez, V.; Gomez, A.; Contin, M.; Tripodi, V.; D’Annunzio, V.; Gelpi, R.J. Thioredoxin-1 is required for the cardioprotecive effect of sildenafil against ischaemia/reperfusion injury and mitochondrial dysfunction in mice. Free Radic. Res. 2019, 53, 993–1004. [Google Scholar] [CrossRef]

| Groups | Basal | 30 min R | |
|---|---|---|---|
| LVDP (mmHg) | CD-I/R | 96.3 ± 1.0 | 20.3 ± 3.4 * |
| CD-IP | 81.3 ± 5.9 | 19.9 ± 4.2 * | |
| HFD-/R | 98.3 ± 4.5 | 19.6 ± 2.8 * | |
| HFD-IP | 93.8 ± 11 | 20.2 ± 3.8 * | |
| CD-I/R-NAC | 97.3 ± 2.0 | 21.2 ± 4.3 * | |
| CD-IP-NAC | 98.3 ± 6.80 | 20.5 ± 5.4 * | |
| HFD-I/R-NAC | 76.2 ± 3.53 | 20.3 ± 3.2 * | |
| HFD-IP-NAC | 80.3 ± 7.78 | 19.9 ± 3.7 * | |
| LVEDP (mmHg) | CD-I/R | 7.3 ± 2.6 | 37.3 ± 6.8 * |
| CD-IP | 9.4 ± 1.9 | 41.9 ± 6.9 * | |
| HFD-I/R | 9.2 ± 6.2 | 46.4 ± 12.4 * | |
| HFD-IP | 7.7 ± 2.2 | 46.4 ± 3.1 * | |
| CD-I/R-NAC | 8.6 ± 4.6 | 42.6 ± 7.6 * | |
| CD-IP-NAC | 9.5 ± 1.6 | 40.8 ± 7.2 * | |
| HFD-I/R-NAC | 9.3 ± 5.5 | 47.2 ± 10.5 * | |
| HFD-IP-NAC | 7.9 ± 2.3 | 46.1 ± 8.9 * | |
| +dP/dtmax (mmHg/seg) | CD-I/R | 3831 ± 409 | 257 ± 89 * |
| CD-IP | 3485 ± 246 | 236 ± 67 * | |
| HFD-I/R | 3892 ± 324 | 268 ± 72 * | |
| HFD-IP | 3868 ± 508 | 365 ± 78 * | |
| CD-I/R-NAC | 3184 ± 301 | 354 ± 78 * | |
| CD-IP-NAC | 3896 ± 306 | 355 ± 57 * | |
| HFD-I/R-NAC | 3546 ± 327 | 297 ± 56 * | |
| HFD-IP-NAC | 3942 ± 541 | 372 ± 68 * | |
| CPP (mmHg) | CD-I/R | 67.1 ± 6.4 | 93.3 ± 10.7 * |
| CD-IP | 70.4 ± 3.8 | 87.13 ± 6.5 * | |
| HFD-I/R | 67.1 ± 5.8 | 111.7 ± 13.6 * | |
| HFD-IP | 68.0 ± 4.0 | 85.8 ± 6.2 * | |
| CD-I/R-NAC | 65.1 ± 5.4 | 102.4 ± 9.9 * | |
| CD-IP-NAC | 75.9 ± 4.1 | 99.0 ± 4.5 * | |
| HFD-I/R-NAC | 65.5 ± 6.9 | 100.7 ± 14.0 * | |
| HFD-IP-NAC | 64.8 ± 5.7 | 97.6 ± 6.3 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zaobornyj, T.; Perez, V.; Ossani, G.; Mazo, T.; Godoy, E.; Godoy, J.; Yanaje, Y.; Musci-Ferrari, C.; Contin, M.; Tripodi, V.; et al. N-Acetylcysteine Treatment Restores the Protective Effect of Heart Ischemic Postconditioning in a Murine Model in the Early Stages of Atherosclerosis. Pharmaceuticals 2025, 18, 1014. https://doi.org/10.3390/ph18071014
Zaobornyj T, Perez V, Ossani G, Mazo T, Godoy E, Godoy J, Yanaje Y, Musci-Ferrari C, Contin M, Tripodi V, et al. N-Acetylcysteine Treatment Restores the Protective Effect of Heart Ischemic Postconditioning in a Murine Model in the Early Stages of Atherosclerosis. Pharmaceuticals. 2025; 18(7):1014. https://doi.org/10.3390/ph18071014
Chicago/Turabian StyleZaobornyj, Tamara, Virginia Perez, Georgina Ossani, Tamara Mazo, Eugenia Godoy, Jorge Godoy, Yohana Yanaje, Camila Musci-Ferrari, Mario Contin, Valeria Tripodi, and et al. 2025. "N-Acetylcysteine Treatment Restores the Protective Effect of Heart Ischemic Postconditioning in a Murine Model in the Early Stages of Atherosclerosis" Pharmaceuticals 18, no. 7: 1014. https://doi.org/10.3390/ph18071014
APA StyleZaobornyj, T., Perez, V., Ossani, G., Mazo, T., Godoy, E., Godoy, J., Yanaje, Y., Musci-Ferrari, C., Contin, M., Tripodi, V., Barchuk, M., Berg, G., Gelpi, R. J., Donato, M., & D’Annunzio, V. (2025). N-Acetylcysteine Treatment Restores the Protective Effect of Heart Ischemic Postconditioning in a Murine Model in the Early Stages of Atherosclerosis. Pharmaceuticals, 18(7), 1014. https://doi.org/10.3390/ph18071014








