Short-Term Outcomes of Three Consecutive Monthly Loading Administrations of Aflibercept 8 Mg for Treatment-Naïve Exudative Age-Related Macular Degeneration
Abstract
1. Introduction
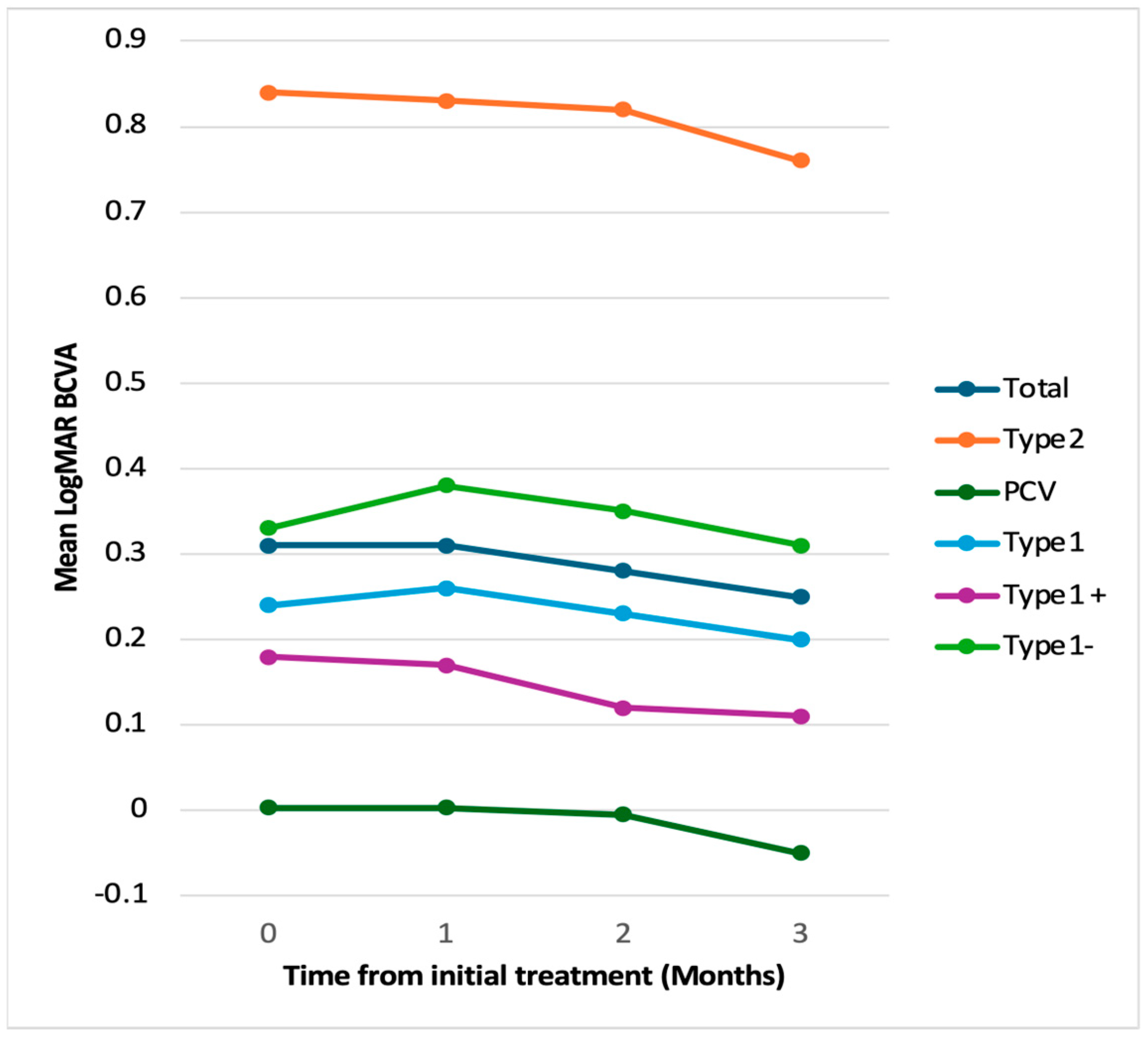
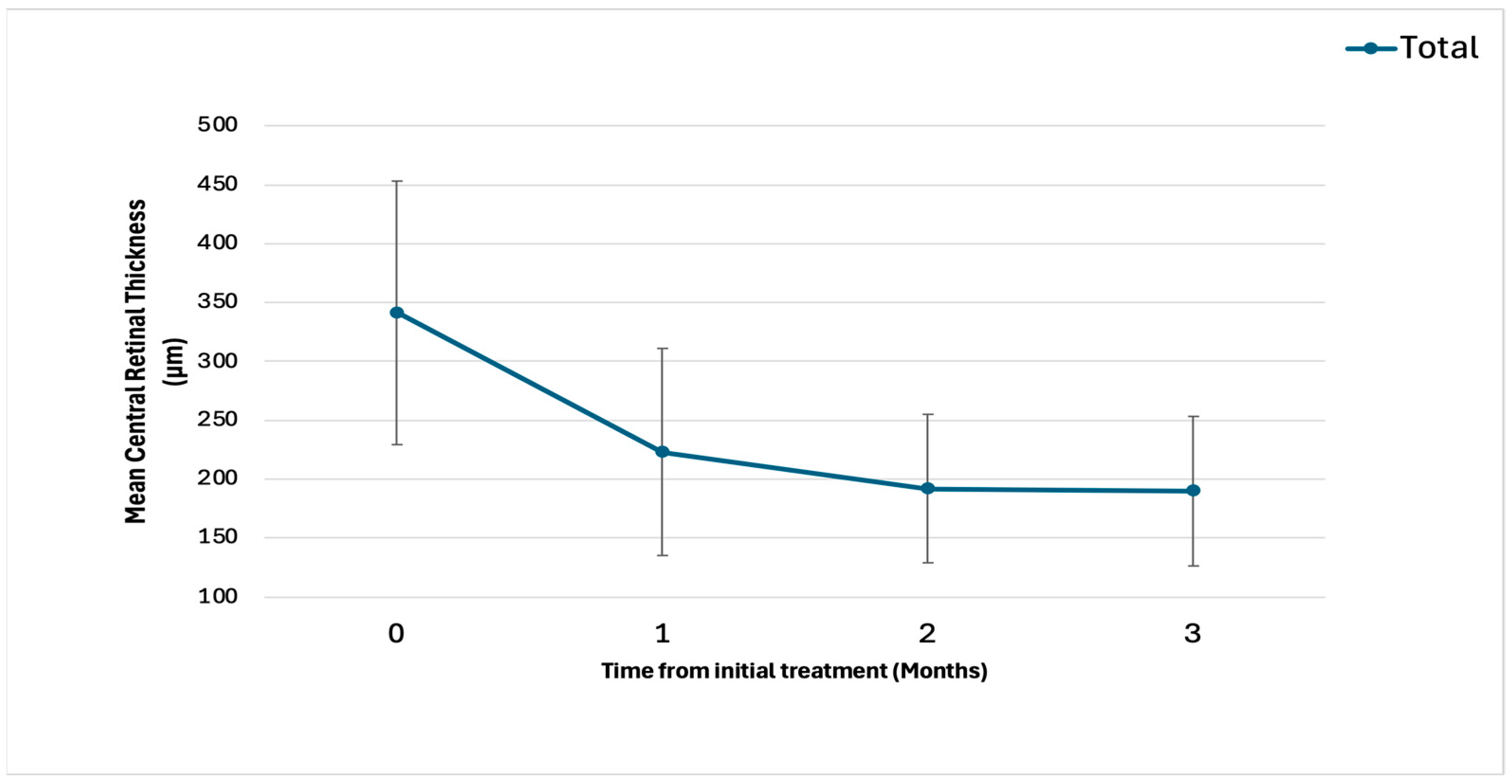
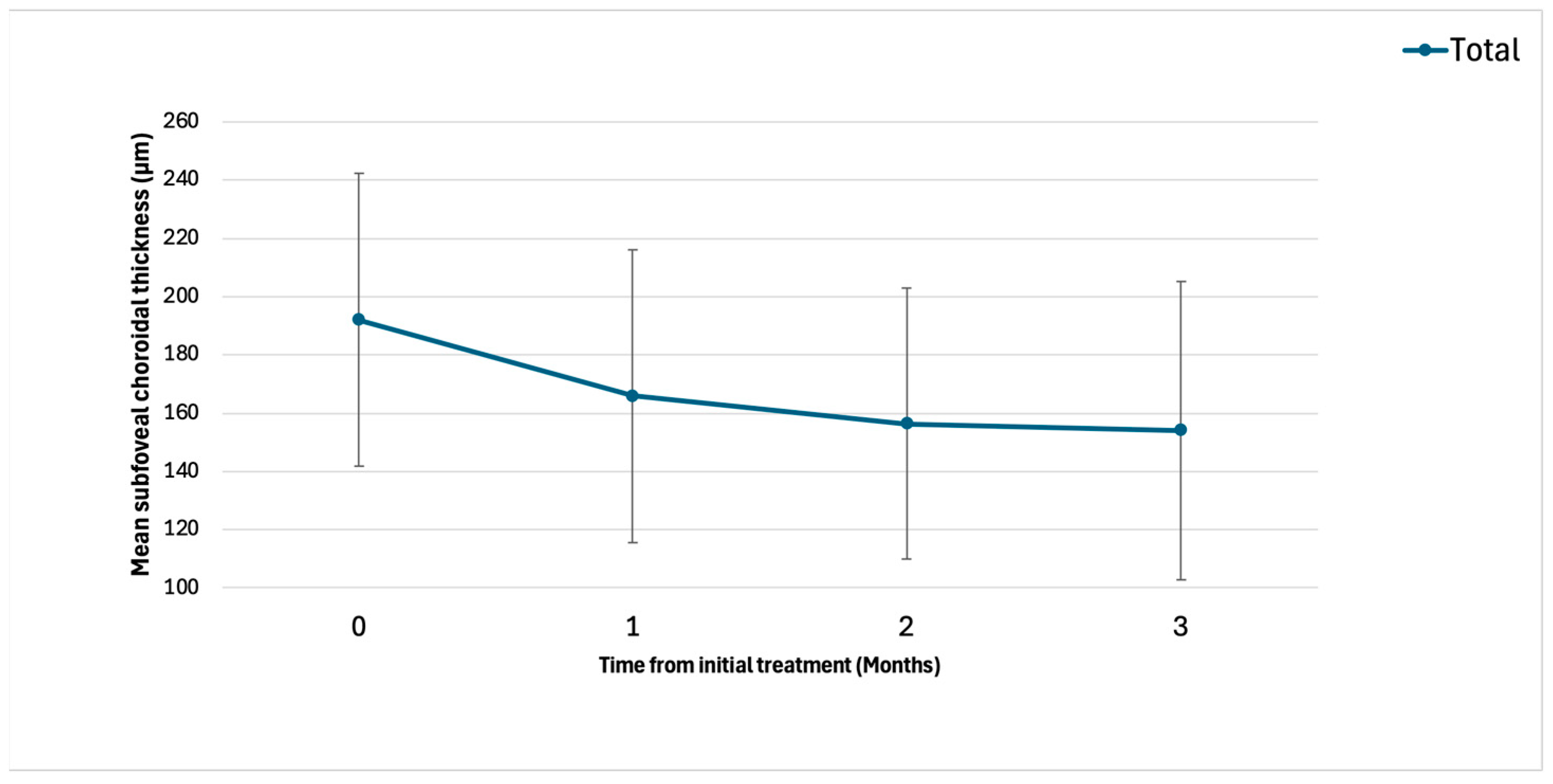
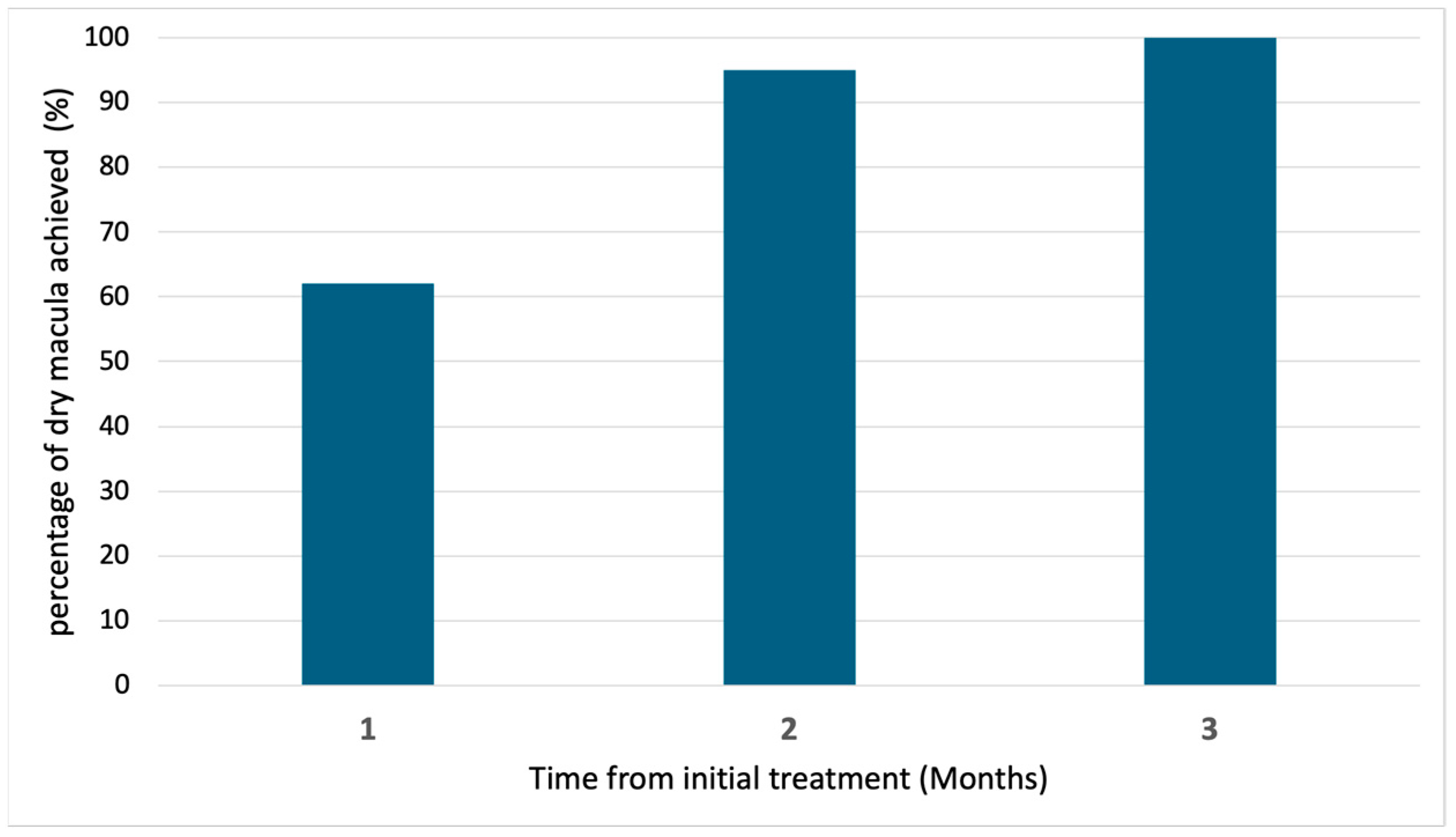
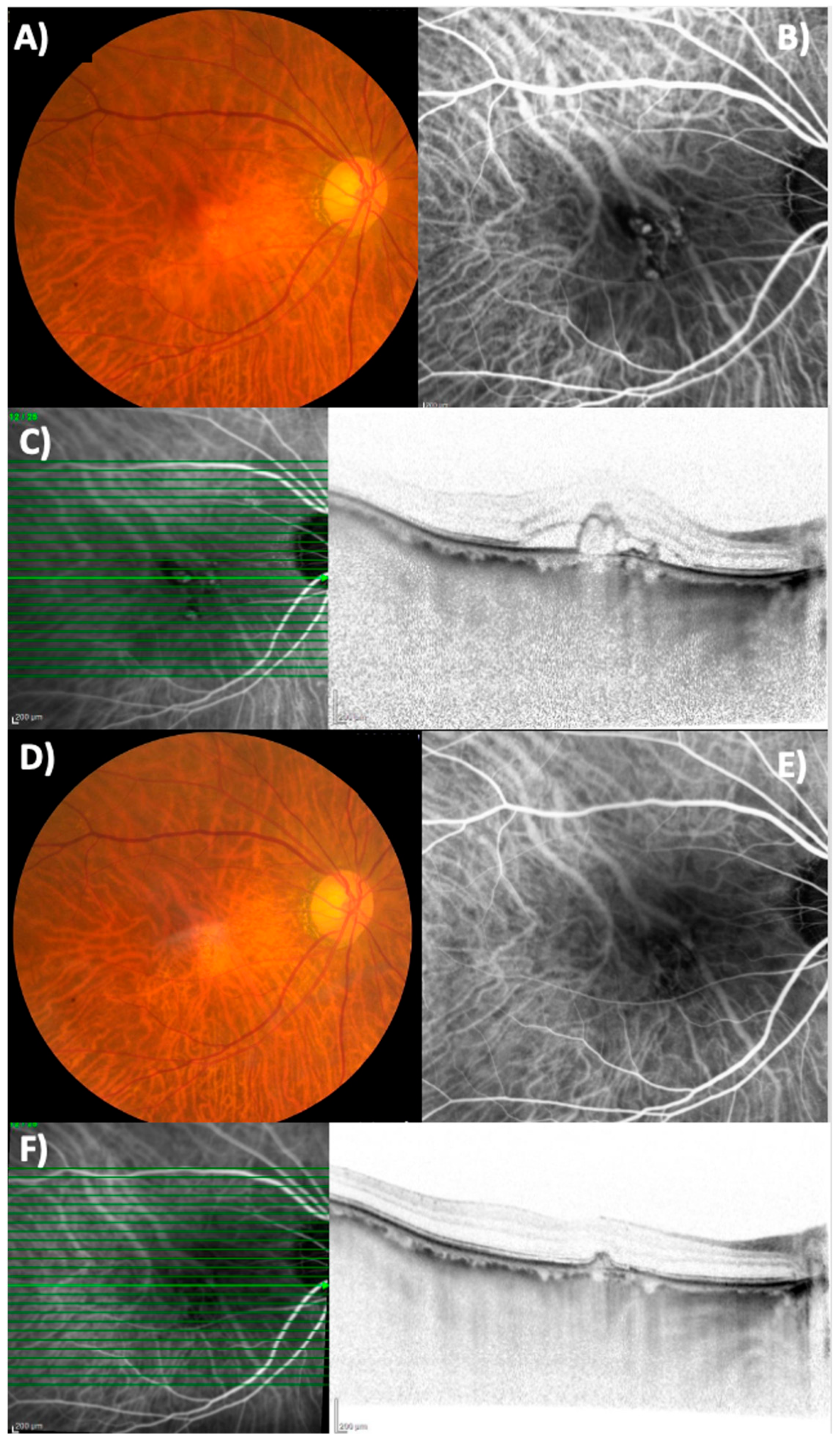
2. Results
3. Discussion
4. Methods
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Wong, W.L.; Su, X.; Li, X.; Cheung, C.M.G.; Klein, R.; Cheng, C.-Y.; Wong, T.Y. Global prevalence of age-related macular degeneration and disease burden projection for 2020 and 2040: A systematic review and meta-analysis. Lancet Glob. Health 2014, 2, e106–e116. [Google Scholar] [CrossRef] [PubMed]
- Sakurada, Y.; Tanaka, K.; Fragiotta, S. Differentiating drusen and drusenoid deposits subtypes on multimodal imaging and risk of advanced age-related macular degeneration. Jpn. J. Ophthalmol. 2023, 67, 1–13. [Google Scholar] [PubMed]
- Sasaki, M.; Kawasaki, R.; Yanagi, Y. Early Stages of Age-Related Macular Degeneration: Racial/Ethnic Differences and Proposal of a New Classification Incorporating Emerging Concept of Choroidal Pathology. J. Clin. Med. 2022, 11, 6274. [Google Scholar] [CrossRef] [PubMed]
- Sadda, S.R.; Guymer, R.; Holz, F.G.; Schmitz-Valckenberg, S.; Curcio, C.A.; Bird, A.C.; Blodi, B.A.; Bottoni, F.; Chakravarthy, U.; Chew, E.Y.; et al. Consensus Definition for Atrophy Associated with Age-Related Macular Degeneration on OCT: Classification of Atrophy Report 3. Ophthalmology 2018, 125, 537–548. [Google Scholar] [CrossRef]
- Spaide, R.F.; Jaffe, G.J.; Sarraf, D.; Freund, K.B.; Sadda, S.R.; Staurenghi, G.; Waheed, N.K.; Chakravarthy, U.; Rosenfeld, P.J.; Holz, F.G.; et al. Consensus Nomenclature for Reporting Neovascular Age-Related Macular Degeneration Data: Consensus on Neovascular Age-Related Macular Degeneration Nomenclature Study Group. Ophthalmology 2020, 127, 616–636. [Google Scholar]
- Photodynamic therapy of subfoveal choroidal neovascularization in age-related macular degeneration with verteporfin: One-year results of 2 randomized clinical trials—TAP report. Treatment of age-related macular degeneration with photodynamic therapy (TAP) Study Group. Arch. Ophthalmol. 1999, 117, 1329–1345. [Google Scholar]
- Gragoudas, E.S.; Adamis, A.P.; Cunningham, E.T., Jr.; Feinsod, M.; Guyer, D.R.; VEGF Inhibition Study in Ocular Neovascularization Clinical Trial Group. Pegaptanib for neovascular age-related macular degeneration. N. Engl. J. Med. 2004, 351, 2805–2816. [Google Scholar] [CrossRef]
- Rosenfeld, P.J.; Brown, D.M.; Heier, J.S.; Boyer, D.S.; Kaiser, P.K.; Chung, C.Y.; MARINA Study Group. Ranibizumab for neovascular age-related macular degeneration. N. Engl. J. Med. 2006, 355, 1419–1431. [Google Scholar]
- Heier, J.S.; Brown, D.M.; Chong, V.; Korobelnik, J.-F.; Kaiser, P.K.; Nguyen, Q.D.; Kirchhof, B.; Ho, A.; Ogura, Y.; Yancopoulos, G.D.; et al. Intravitreal aflibercept (VEGF trap-eye) in wet age-related macular degeneration. Ophthalmology 2012, 119, 2537–2548. [Google Scholar]
- Azuma, K.; Okubo, A.; Nomura, Y.; Zhou, H.; Terao, R.; Hashimoto, Y.; Asano, K.S.; Azuma, K.; Inoue, T.; Obata, R. Association between pachychoroid and long-term treatment outcomes of photodynamic therapy with intravitreal ranibizumab for polypoidal choroidal vasculopathy. Sci. Rep. 2020, 10, 8337. [Google Scholar]
- Hashimoto, Y.; Okada, A.; Matsui, H.; Yasunaga, H.; Aihara, M.; Obata, R. Recent trends in anti-vascular endothelial growth factor intravitreal injections: A large claims database study in Japan. Jpn. J. Ophthalmol. 2023, 67, 109–118. [Google Scholar]
- Kume, A.; Ohshiro, T.; Sakurada, Y.; Kikushima, W.; Yoneyama, S.; Kashiwagi, K. Treatment Patterns and Health Care Costs for Age-Related Macular Degeneration in Japan: An Analysis of National Insurance Claims Data. Ophthalmology 2016, 123, 1263–1268. [Google Scholar] [CrossRef]
- Nguyen, Q.D.; Das, A.; Do, D.V.; Dugel, P.U.; Gomes, A.; Holz, F.G.; Koh, A.; Pan, C.K.; Sepah, Y.J.; Patel, N.; et al. Brolucizumab: Evolution through Preclinical and Clinical Studies and the Implications for the Management of Neovascular Age-Related Macular Degeneration. Ophthalmology 2020, 127, 963–976. [Google Scholar]
- Dugel, P.U.; Singh, R.P.; Koh, A.; Ogura, Y.; Weissgerber, G.; Gedif, K.; Jaffe, G.J.; Tadayoni, R.; Schmidt-Erfurth, U.; Holz, F.G. HAWK and HARRIER: Ninety-Six-Week Outcomes from the Phase 3 Trials of Brolucizumab for Neovascular Age-Related Macular Degeneration. Ophthalmology 2021, 128, 89–99. [Google Scholar]
- Heier, J.S.; Khanani, A.M.; Ruiz, C.Q.; Basu, K.; Ferrone, P.J.; Brittain, C.; Figueroa, M.S.; Lin, H.; Holz, F.G.; Patel, V.; et al. Efficacy, durability, and safety of intravitreal faricimab up to every 16 weeks for neovascular age-related macular degeneration (TENAYA and LUCERNE): Two randomised, double-masked, phase 3, non-inferiority trials. Lancet 2022, 399, 729–740. [Google Scholar] [PubMed]
- Khanani, A.M.; Kotecha, A.; Chang, A.; Chen, S.-J.; Chen, Y.; Guymer, R.; Heier, J.S.; Holz, F.G.; Iida, T.; Ives, J.A.; et al. TENAYA and LUCERNE: Two-Year Results from the Phase 3 Neovascular Age-Related Macular Degeneration Trials of Faricimab with Treat-and-Extend Dosing in Year 2. Ophthalmology 2024, 131, 914–926. [Google Scholar] [CrossRef]
- Dugel, P.U.; Koh, A.; Ogura, Y.; Jaffe, G.J.; Schmidt-Erfurth, U.; Brown, D.M.; Gomes, A.V.; Warburton, J.; Weichselberger, A.; Holz, F.G.; et al. HAWK and HARRIER: Phase 3, Multicenter, Randomized, Double-Masked Trials of Brolucizumab for Neovascular Age-Related Macular Degeneration. Ophthalmology 2020, 127, 72–84. [Google Scholar] [PubMed]
- Lanzetta, P.; Korobelnik, J.-F.; Heier, J.S.; Leal, S.; Holz, F.G.; Clark, W.L.; Eichenbaum, D.; Iida, T.; Xiaodong, S.; Berliner, A.J.; et al. Intravitreal aflibercept 8 mg in neovascular age-related macular degeneration (PULSAR): 48-week results from a randomised, double-masked, non-inferiority, phase 3 trial. Lancet 2024, 403, 1141–1152. [Google Scholar] [CrossRef]
- Ghezala, I.B.; Gabrielle, P.-H.; Sibert, M.; Steinberg, L.-A.; Dautriche, A.; Arnould, L.; Creuzot-Garcher, C. Severe Intraocular Inflammation After Intravitreal Injection of Faricimab: A Single-Site Case Series of Six Patients. Am. J. Ophthalmol. 2025, 269, 11–19. [Google Scholar] [PubMed]
- Montesel, A.; Sen, S.; Preston, E.; Patel, P.J.; Huemer, J.; Hamilton, R.D.; Nicholson, L.; Papasavvas, I.; Tucker, W.R.; Yeung, I. Intraocular Inflammation (IOI) Associated with Faricimab Therapy: One-year Real World Outcomes. Retina 2025. ahead of print. [Google Scholar] [CrossRef]
- Bruening, W.; Kim, S.; Yeh, S.; Rishi, P.; Conrady, C.D. Inflammation and Occlusive Retinal Vasculitis Post Faricimab. JAMA Ophthalmol. 2025. ahead of print. [Google Scholar] [CrossRef]
- Baumal, C.R.; Bodaghi, B.; Singer, M.; Tanzer, D.J.; Seres, A.; Joshi, M.R.; Feltgen, N.; Gale, R. Expert Opinion on Management of Intraocular Inflammation, Retinal Vasculitis, and Vascular Occlusion after Brolucizumab Treatment. Ophthalmol. Retin. 2021, 5, 519–527. [Google Scholar]
- Fukuda, Y.; Sakurada, Y.; Matsubara, M.; Kotoda, Y.; Kasai, Y.; Sugiyama, A.; Kashiwagi, K. Comparison of one-year outcomes between as-needed brolucizumab and aflibercept for polypoidal choroidal vasculopathy. Jpn. J. Ophthalmol. 2023, 67, 402–409. [Google Scholar] [PubMed]
- Matsumoto, H.; Hoshino, J.; Nakamura, K.; Nagashima, T.; Akiyama, H. Short-term outcomes of intravitreal faricimab for treatment-naive neovascular age-related macular degeneration. Graefes Arch. Clin. Exp. Ophthalmol. 2023, 261, 2945–2952. [Google Scholar] [PubMed]
- Mukai, R.; Kataoka, K.; Tanaka, K.; Miyara, Y.; Maruko, I.; Nakayama, M.; Watanabe, Y.; Yamamoto, A.; Wakatsuki, Y.; Onoe, H.; et al. Three-month outcomes of faricimab loading therapy for wet age-related macular degeneration in Japan. Sci. Rep. 2023, 13, 8747. [Google Scholar]
- Allehyani, M.H.; Alsaeedi, A.K.; Alqthmi, R.O.; Saleh, R.E.; Alsamli, R.S.; Almalki, H.A.; Alshehri, A.F.; Felimban, S.A.; Kambiji, G.J.; Almatrafi, M.I.; et al. Comparative Efficacy of Brolucizumab and Aflibercept in Polypoidal Choroidal Vasculopathy: A Systematic Review and Meta-Analysis. Cureus 2025, 17, e77073. [Google Scholar]
- Kimura, M.; Sakurada, Y.; Fukuda, Y.; Matsubara, M.; Kotoda, Y.; Kasai, Y.; Sugiyama, A.; Kikushima, W.; Tsuru, D.V.; Kashiwagi, K. Association of Polyp Regression after Loading Phase with 12-Month Outcomes of Eyes with Polypoidal Choroidal Vasculopathy. Pharmaceuticals 2024, 17, 687. [Google Scholar] [CrossRef]
- Sayanagi, K.; Fujimoto, S.; Hara, C.; Fukushima, Y.; Maruyama, K.; Kawasaki, R.; Sato, S.; Nishida, K. Effect of polyp regression and reduction on treatment efficacy in polypoidal choroidal vasculopathy treated with aflibercept. Sci. Rep. 2024, 14, 1833. [Google Scholar]
- Ferrara, N.; Mass, R.D.; Campa, C.; Kim, R. Targeting VEGF-A to treat cancer and age-related macular degeneration. Annu. Rev. Med. 2007, 58, 491–504. [Google Scholar]
- Kikushima, W.; Sakurada, Y.; Fukuda, Y.; Matsubara, M.; Yoneyama, S.; Shijo, T.; Sugiyama, A.; Kotoda, Y.; Kashiwagi, K. Incidence And Characteristics Of Neovascular Age-Related Macular With Over A 12-Month Remission After Three Monthly Aflibercept Administration: 60 Months Results of a Pro Re Nata Regimen. Retina 2024, 44, 498–505. [Google Scholar]
| Characteristics (N = 21) | Values |
|---|---|
| Age (years) | 75 ± 9.9 |
| Sex Male/Female (%) | 11 (52)/10 (48) |
| R/L (%) | 7 (33)/14 (67) |
| Phakia/IOL (%) | 16 (76)/5 (24) |
| BCVA (logMAR) | 0.31 ± 0.38 |
| CRT (μm) | 341 ± 112 |
| SCT (μm) | 192 ± 50 |
| Type1 MNV/Type2 MNV/PCV (%) | 11 (52)/4 (19)/6 (29) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hosoda, S.; Sakurada, Y.; Fukuda, Y.; Kotoda, Y.; Kikushima, W.; Kashiwagi, K. Short-Term Outcomes of Three Consecutive Monthly Loading Administrations of Aflibercept 8 Mg for Treatment-Naïve Exudative Age-Related Macular Degeneration. Pharmaceuticals 2025, 18, 438. https://doi.org/10.3390/ph18030438
Hosoda S, Sakurada Y, Fukuda Y, Kotoda Y, Kikushima W, Kashiwagi K. Short-Term Outcomes of Three Consecutive Monthly Loading Administrations of Aflibercept 8 Mg for Treatment-Naïve Exudative Age-Related Macular Degeneration. Pharmaceuticals. 2025; 18(3):438. https://doi.org/10.3390/ph18030438
Chicago/Turabian StyleHosoda, Shuhei, Yoichi Sakurada, Yoshiko Fukuda, Yumi Kotoda, Wataru Kikushima, and Kenji Kashiwagi. 2025. "Short-Term Outcomes of Three Consecutive Monthly Loading Administrations of Aflibercept 8 Mg for Treatment-Naïve Exudative Age-Related Macular Degeneration" Pharmaceuticals 18, no. 3: 438. https://doi.org/10.3390/ph18030438
APA StyleHosoda, S., Sakurada, Y., Fukuda, Y., Kotoda, Y., Kikushima, W., & Kashiwagi, K. (2025). Short-Term Outcomes of Three Consecutive Monthly Loading Administrations of Aflibercept 8 Mg for Treatment-Naïve Exudative Age-Related Macular Degeneration. Pharmaceuticals, 18(3), 438. https://doi.org/10.3390/ph18030438







