Clomiphene Citrate Treatment as an Alternative Therapeutic Approach for Male Hypogonadism: Mechanisms and Clinical Implications
Abstract
1. Introduction
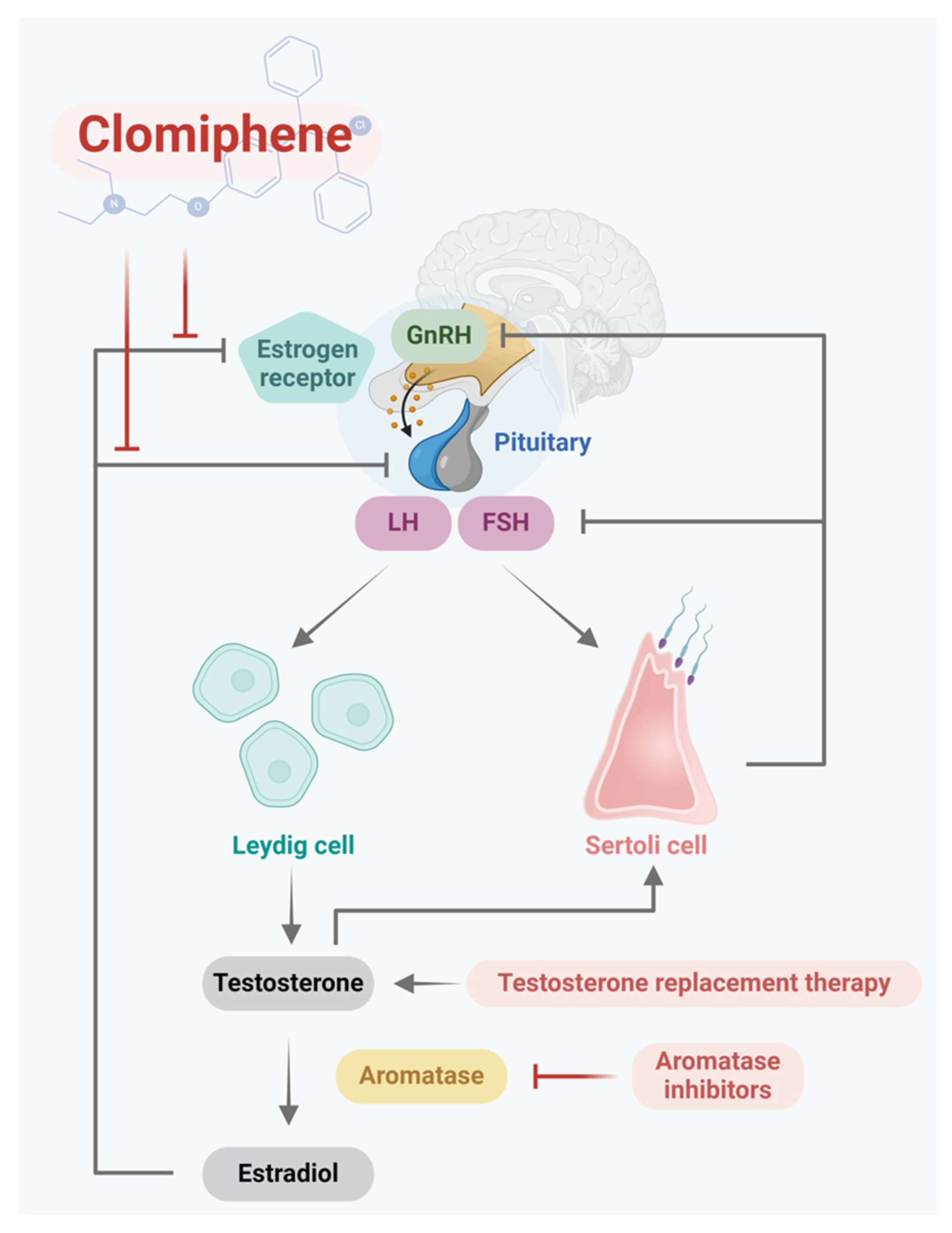
2. HPG Axis in Men
3. Testosterone Synthesis
4. Biological Function of Testosterone
5. Male Hypogonadism
6. Male Infertility
7. Treatment Options for Male Hypogonadism
8. Clomiphene
9. Hormonal Measurement
10. Treatment of Hypogonadism Symptoms
11. Treatment of Infertility
12. Safety
13. Population Variability in Treatment Response
14. Combination Therapy
15. Treatment Cost
16. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Mulhall, J.P.; Trost, L.W.; Brannigan, R.E.; Kurtz, E.G.; Redmon, J.B.; Chiles, K.A.; Lightner, D.J.; Miner, M.M.; Murad, M.H.; Nelson, C.J.; et al. Evaluation and Management of Testosterone Deficiency: AUA Guideline. J. Urol. 2018, 200, 423–432. [Google Scholar] [PubMed]
- Bhasin, S.; Cunningham, G.R.; Hayes, F.J.; Matsumoto, A.M.; Snyder, P.J.; Swerdloff, R.S.; Montori, V.M. Testosterone Therapy in Men with Androgen Deficiency Syndromes: An Endocrine Society Clinical Practice Guideline. J. Clin. Endocrinol. Metab. 2010, 95, 2536–2559. [Google Scholar] [PubMed]
- Wu, F.C.; Tajar, A.; Beynon, J.M.; Pye, S.R.; Silman, A.J.; Finn, J.D.; O’Neill, T.W.; Bartfai, G.; Casanueva, F.F.; Forti, G.; et al. Identification of Late-Onset Hypogonadism in Middle-Aged and Elderly Men. N. Engl. J. Med. 2010, 363, 123–135. [Google Scholar] [PubMed]
- Basaria, S. Male hypogonadism. Lancet 2014, 383, 1250–1263. [Google Scholar] [PubMed]
- Araujo, A.B.; O’donnell, A.B.; Brambilla, D.J.; Simpson, W.B.; Longcope, C.; Matsumoto, A.M.; McKinlay, J.B. Prevalence and Incidence of Androgen Deficiency in Middle-Aged and Older Men: Estimates from the Massachusetts Male Aging Study. J. Clin. Endocrinol. Metab. 2004, 89, 5920–5926. [Google Scholar]
- Salonia, A.; Bettocchi, C.; Capogrosso, P.; Carvalho, J.; Corona, G.; Hatzichristodoulou, G.; Jones, T.H.; Kadioglu, A.; Martinez-Salamanca, J.I.; Minhas, S.; et al. EAU Guidelines. In The EAU Annual Congress Milan; EAU Guidelines Office: Arnhem, The Netherlands, 2023. [Google Scholar]
- Salonia, A.; Rastrelli, G.; Hackett, G.; Seminara, S.B.; Huhtaniemi, I.T.; Rey, R.A.; Hellstrom, W.J.G.; Palmert, M.R.; Corona, G.; Dohle, G.R.; et al. Paediatric and adult-onset male hypogonadism. Nat. Rev. Dis. Primers 2019, 5, 38. [Google Scholar]
- Araujo, A.B.; Esche, G.R.; Kupelian, V.; O’donnell, A.B.; Travison, T.G.; Williams, R.E.; Clark, R.V.; McKinlay, J.B. Prevalence of Symptomatic Androgen Deficiency in Men. J. Clin. Endocrinol. Metab. 2007, 92, 4241–4247. [Google Scholar]
- Zarotsky, V.; Huang, M.; Carman, W.; Morgentaler, A.; Singhal, P.K.; Coffin, D.; Jones, T.H. Systematic literature review of the risk factors, comorbidities, and consequences of hypogonadism in men. Andrology 2014, 2, 819–834. [Google Scholar]
- Svartberg, J.; von Mühlen, D.; Mathiesen, E.; Joakimsen, O.; Bønaa, K.H.; Stensland-Bugge, E. Low testosterone levels are associated with carotid atherosclerosis in men. J. Intern. Med. 2006, 259, 576–582. [Google Scholar] [CrossRef]
- Kelly, D.M.; Jones, T.H. Testosterone and obesity. Obes. Rev. 2015, 16, 581–606. [Google Scholar]
- Dhindsa, S.; Prabhakar, S.; Sethi, M.; Bandyopadhyay, A.; Chaudhuri, A.; Dandona, P. Frequent Occurrence of Hypogonadotropic Hypogonadism in Type 2 Diabetes. J. Clin. Endocrinol. Metab. 2004, 89, 5462–5468. [Google Scholar] [CrossRef] [PubMed]
- Cunningham, G.R.; Stephens-Shields, A.J.; Rosen, R.C.; Wang, C.; Bhasin, S.; Matsumoto, A.M.; Parsons, J.K.; Gill, T.M.; Molitch, M.E.; Farrar, J.T.; et al. Testosterone Treatment and Sexual Function in Older Men with Low Testosterone Levels. J. Clin. Endocrinol. Metab. 2016, 101, 3096–3104. [Google Scholar] [CrossRef] [PubMed]
- Corona, G.; Rastrelli, G.; Morgentaler, A.; Sforza, A.; Mannucci, E.; Maggi, M. Meta-analysis of Results of Testosterone Therapy on Sexual Function Based on International Index of Erectile Function Scores. Eur. Urol. 2017, 72, 1000–1011. [Google Scholar] [CrossRef] [PubMed]
- Zitzmann, M. Testosterone, mood, behaviour and quality of life. Andrology 2020, 8, 1598–1605. [Google Scholar] [CrossRef]
- Spitzer, M.; Huang, G.; Basaria, S.; Travison, T.G.; Bhasin, S. Risks and benefits of testosterone therapy in older men. Nat. Rev. Endocrinol. 2013, 9, 414–424. [Google Scholar] [CrossRef]
- Wang, C.; Alexander, G.; Berman, N.; Salehian, B.; Davidson, T.; McDonald, V.; Steiner, B.; Hull, L.; Callegari, C.; Swerdloff, R.S. Testosterone replacement therapy improves mood in hypogonadal men—A clinical research center study. J. Clin. Endocrinol. Metab. 1996, 81, 3578–3583. [Google Scholar]
- Crosnoe, L.E.; Grober, E.; Ohl, D.; Kim, E.D. Exogenous testosterone: A preventable cause of male infertility. Transl. Androl. Urol. 2013, 2, 106–113. [Google Scholar] [PubMed]
- Cunningham, G.R.; Hirshkowitz, M.; Korenman, S.G.; Karacan, I. Testosterone Replacement Therapy and Sleep-Related Erections in Hypogonadal Men. J. Clin. Endocrinol. Metab. 1990, 70, 792–797. [Google Scholar] [CrossRef]
- Wheeler, K.M.; Smith, R.P.; Kumar, R.A.; Setia, S.; Costabile, R.A.; Kavoussi, P.K. A Comparison of Secondary Polycythemia in Hypogonadal Men Treated with Clomiphene Citrate versus Testosterone Replacement: A Multi-Institutional Study. J. Urol. 2017, 197, 1127–1131. [Google Scholar] [CrossRef]
- Xu, L.; Freeman, G.; Cowling, B.J.; Schooling, C.M. Testosterone therapy and cardiovascular events among men: A systematic review and meta-analysis of placebo-controlled randomized trials. BMC Med. 2013, 11, 108. [Google Scholar] [CrossRef]
- Vigen, R.; O’donnell, C.I.; Barón, A.E.; Grunwald, G.K.; Maddox, T.M.; Bradley, S.M.; Barqawi, A.; Woning, G.; Wierman, M.E.; Plomondon, M.E.; et al. Association of Testosterone Therapy With Mortality, Myocardial Infarction, and Stroke in Men With Low Testosterone Levels. JAMA 2013, 310, 1829–1836. [Google Scholar] [CrossRef]
- Finkle, W.D.; Greenland, S.; Ridgeway, G.K.; Adams, J.L.; Frasco, M.A.; Cook, M.B.; Fraumeni, J.F., Jr.; Hoover, R.N. Increased risk of non-fatal myocardial infarction following testosterone therapy prescription in men. PLoS ONE 2014, 9, e85805. [Google Scholar] [CrossRef] [PubMed]
- Seftel, A.D. Re: Testosterone Products: Drug Safety Communication—FDA Cautions about Using Testosterone Products for Low Testosterone due to Aging; Requires Labeling Change to Inform of Possible Increased Risk of Heart Attack and Stroke. J. Urol. 2015, 194, 759–760. [Google Scholar] [CrossRef]
- Schlegel, P.N. Aromatase inhibitors for male infertility. Fertil. Steril. 2012, 98, 1359–1362. [Google Scholar] [CrossRef] [PubMed]
- Kotoulas, I.-G.; Cardamakis, E.; Michopoulos, J.; Mitropoulos, D.; Dounis, A. Tamoxifen treatment in male infertility. I. Effect on spermatozoa. Fertil. Steril. 1994, 61, 911–914. [Google Scholar] [CrossRef]
- Dickey, R.; Holtkamp, D. Development, pharmacology and clinical experience with clomiphene citrate. Hum. Reprod. Update 1996, 2, 483–506. [Google Scholar] [CrossRef]
- Scovell, J.M.; Khera, M. Testosterone Replacement Therapy Versus Clomiphene Citrate in the Young Hypogonadal Male. Eur. Urol. Focus. 2018, 4, 321–323. [Google Scholar] [CrossRef] [PubMed]
- Wiehle, R.D.; Fontenot, G.K.; Wike, J.; Hsu, K.; Nydell, J.; Lipshultz, L. Enclomiphene citrate stimulates testosterone production while preventing oligospermia: A randomized phase II clinical trial comparing topical testosterone. Fertil. Steril. 2014, 102, 720–727. [Google Scholar] [CrossRef] [PubMed]
- Huijben, M.; Huijsmans, R.L.N.; Lock, M.T.W.T.; de Kemp, V.F.; de Kort, L.M.O.; van Breda, J.H.M.K. Clomiphene citrate for male infertility: A systematic review and meta-analysis. Andrology 2023, 11, 987–996. [Google Scholar] [CrossRef]
- Jarow, J.P.; Zirkin, B.R. The Androgen Microenvironment of the Human Testis and Hormonal Control of Spermatogenesis. Ann. N. Y. Acad. Sci. 2005, 1061, 208–220. [Google Scholar]
- Krzastek, S.C.; Sharma, D.; Abdullah, N.; Sultan, M.; Machen, G.L.; Wenzel, J.L.; Ells, A.; Chen, X.; Kavoussi, M.; Costabile, R.A.; et al. Long-Term Safety and Efficacy of Clomiphene Citrate for the Treatment of Hypogonadism. J. Urol. 2019, 202, 1029–1035. [Google Scholar] [CrossRef]
- Taylor, F.; Levine, L. Clomiphene Citrate and Testosterone Gel Replacement Therapy for Male Hypogonadism: Efficacy and Treatment Cost. J. Sex. Med. 2010, 7, 269–276. [Google Scholar] [CrossRef]
- Corradi, P.F.; Corradi, R.B.; Greene, L.W. Physiology of the Hypothalamic Pituitary Gonadal Axis in the Male. Urol. Clin. N. Am. 2016, 43, 151–162. [Google Scholar]
- Jin, J.-M.; Yang, W.-X. Molecular regulation of hypothalamus–pituitary–gonads axis in males. Gene 2014, 551, 15–25. [Google Scholar]
- Ellis, G.B.; Desjardins, C.; Fraser, H.M. Control of pulsatile LH release in male rats. Neuroendocrinology 1983, 37, 177–183. [Google Scholar]
- Ascoli, M.; Fanelli, F.; Segaloff, D.L. The lutropin/choriogonadotropin receptor, a 2002 perspective. Endocr. Rev. 2002, 23, 141–174. [Google Scholar]
- Midzak, A.S.; Chen, H.; Papadopoulos, V.; Zirkin, B.R. Leydig cell aging and the mechanisms of reduced testosterone synthesis. Mol. Cell. Endocrinol. 2009, 299, 23–31. [Google Scholar]
- Payne, A.H.; Hales, D.B. Overview of steroidogenic enzymes in the pathway from cholesterol to active steroid hormones. Endocr. Rev. 2004, 25, 947–970. [Google Scholar] [CrossRef]
- Young, J.; Couzinet, B.; Nahoul, K.; Brailly, S.; Chanson, P.; Baulieu, E.E.; Schaison, G. Panhypopituitarism as a model to study the metabolism of dehydroepiandrosterone (DHEA) in humans. J. Clin. Endocrinol. Metab. 1997, 82, 2578–2585. [Google Scholar]
- Sofikitis, N.; Giotitsas, N.; Tsounapi, P.; Baltogiannis, D.; Giannakis, D.; Pardalidis, N. Hormonal regulation of spermatogenesis and spermiogenesis. J. Steroid Biochem. Mol. Biol. 2008, 109, 323–330. [Google Scholar]
- Griswold, M.D. The central role of Sertoli cells in spermatogenesis. Semin. Cell Dev. Biol. 1998, 9, 411–416. [Google Scholar] [CrossRef] [PubMed]
- Kathrins, M.; Niederberger, C. Diagnosis and treatment of infertility-related male hormonal dysfunction. Nat. Rev. Urol. 2016, 13, 309–323. [Google Scholar] [CrossRef] [PubMed]
- Erkkilä, K.; Henriksén, K.; Hirvonen, V.; Rannikko, S.; Salo, J.; Parvinen, M.; Dunkel, L. Testosterone regulates apoptosis in adult human seminiferous tubules in vitro. J. Clin. Endocrinol. Metab. 1997, 82, 2314–2321. [Google Scholar] [CrossRef] [PubMed]
- Tesarik, J.; Greco, E.; Mendoza, C. Assisted reproduction with in-vitro-cultured testicular spermatozoa in cases of severe germ cell apoptosis: A pilot study. Hum. Reprod. 2001, 16, 2640–2645. [Google Scholar]
- Corona, G.; Maggi, M. The role of testosterone in erectile dysfunction. Nat. Rev. Urol. 2010, 7, 46–56. [Google Scholar]
- Lotti, F.; Maggi, M. Sexual dysfunction and male infertility. Nat. Rev. Urol. 2018, 15, 287–307. [Google Scholar] [CrossRef]
- Muraleedharan, V.; Jones, T.H. Testosterone and the metabolic syndrome. Ther. Adv. Endocrinol. Metab. 2010, 1, 207–223. [Google Scholar]
- Haffner, S.M.; Mykkänen, L.; Valdez, R.A.; Katz, M.S. Relationship of sex hormones to lipids and lipoproteins in nondiabetic men. J. Clin. Endocrinol. Metab. 1993, 77, 1610–1615. [Google Scholar]
- Kapoor, D.; Malkin, C.J.; Channer, K.S.; Jones, T.H. Androgens, insulin resistance and vascular disease in men. Clin. Endocrinol. 2005, 63, 239–250. [Google Scholar]
- Isidori, A.M.; Caprio, M.; Strollo, F.; Moretti, C.; Frajese, G.; Isidori, A.; Fabbri, A. Leptin and androgens in male obesity: Evidence for leptin contribution to reduced androgen levels. J. Clin. Endocrinol. Metab. 1999, 84, 3673–3680. [Google Scholar]
- Zumoff, B.; Strain, G.W.; Miller, L.K.; Rosner, W.; Senie, R.; Seres, D.S.; Rosenfeld, R.S. Plasma Free and Non-Sex-Hormone-Binding-Globulin Bound Testosterone Are Decreased in Obese Men in Proportion to Their Degree of Obesity. J. Clin. Endocrinol. Metab. 1990, 71, 929–931. [Google Scholar] [CrossRef] [PubMed]
- Dandona, P.; Dhindsa, S. Update: Hypogonadotropic Hypogonadism in Type 2 Diabetes and Obesity. J. Clin. Endocrinol. Metab. 2011, 96, 2643–2651. [Google Scholar] [PubMed]
- Russell, S.H.; Small, C.J.; Stanley, S.A.; Franks, S.; Ghatei, M.A.; Bloom, S.R. The In Vitro Role of Tumour Necrosis Factor-Alpha and Interleukin-6 in the Hypothalamic-Pituitary Gonadal Axis. J. Neuroendocrinol. 2001, 13, 296–301. [Google Scholar] [PubMed]
- Watanobe, H.; Hayakawa, Y. Hypothalamic Interleukin-1β and Tumor Necrosis Factor-α, But Not Interleukin-6, Mediate the Endotoxin-Induced Suppression of the Reproductive Axis in Rats. Endocrinology 2003, 144, 4868–4875. [Google Scholar]
- Dandona, P.; Rosenberg, M.T. A practical guide to male hypogonadism in the primary care setting. Int. J. Clin. Pract. 2010, 64, 682–696. [Google Scholar] [PubMed]
- Dhindsa, S.; Ghanim, H.; Batra, M.; Kuhadiya, N.D.; Abuaysheh, S.; Sandhu, S.; Green, K.; Makdissi, A.; Hejna, J.; Chaudhuri, A.; et al. Insulin Resistance and Inflammation in Hypogonadotropic Hypogonadism and Their Reduction After Testosterone Replacement in Men With Type 2 Diabetes. Diabetes Care 2015, 39, 82–91. [Google Scholar]
- Elliott, J.; Kelly, S.E.; Millar, A.C.; Peterson, J.; Chen, L.; Johnston, A.; Kotb, A.; Skidmore, B.; Bai, Z.; Mamdani, M.; et al. Testosterone therapy in hypogonadal men: A systematic review and network meta-analysis. BMJ Open 2017, 7, e015284. [Google Scholar] [PubMed]
- Pantalone, K.M.; Faiman, C. Male hypogonadism: More than just a low testosterone. Cleve Clin. J. Med. 2012, 79, 717–725. [Google Scholar]
- Carnegie, C. Diagnosis of hypogonadism: Clinical assessments and laboratory tests. Rev. Urol. 2004, 6 (Suppl. 6), S3–S8. [Google Scholar]
- Kumar, P.; Kumar, N.; Thakur, D.S.; Patidar, A. Male hypogonadism: Symptoms and treatment. J. Adv. Pharm. Technol. Res. 2010, 1, 297–301. [Google Scholar]
- Ross, A.; Bhasin, S. Hypogonadism: Its Prevalence and Diagnosis. Urol. Clin. N. Am. 2016, 43, 163–176. [Google Scholar]
- Carrageta, D.F.; Oliveira, P.F.; Alves, M.G.; Monteiro, M.P. Obesity and male hypogonadism: Tales of a vicious cycle. Obes. Rev. 2019, 20, 1148–1158. [Google Scholar] [PubMed]
- Practice Committee of the American Society for Reproductive Medicine. Definitions of infertility and recurrent pregnancy loss: A committee opinion. Fertil. Steril. 2013, 99, 63. [Google Scholar]
- Krausz, C. Male infertility: Pathogenesis and clinical diagnosis. Best. Pract. Res. Clin. Endocrinol. Metab. 2011, 25, 271–285. [Google Scholar] [PubMed]
- Sharlip, I.D.; Jarow, J.P.; Belker, A.M.; Lipshultz, L.I.; Sigman, M.; Thomas, A.J.; Schlegel, P.N.; Howards, S.S.; Nehra, A.; Damewood, M.D.; et al. Best practice policies for male infertility. Fertil. Steril. 2002, 77, 873–882. [Google Scholar]
- Sharma, A.; Minhas, S.; Dhillo, W.S.; Jayasena, C.N. Male infertility due to testicular disorders. J. Clin. Endocrinol. Metab. 2021, 106, e442–e459. [Google Scholar]
- Rastrelli, G.; Guaraldi, F.; Reismann, Y.; Sforza, A.; Isidori, A.M.; Maggi, M.; Corona, G. Testosterone Replacement Therapy for Sexual Symptoms. Sex. Med. Rev. 2019, 7, 464–475. [Google Scholar]
- Snyder, P.J.; Bhasin, S.; Cunningham, G.R.; Matsumoto, A.M.; Stephens-Shields, A.J.; A Cauley, J.; Gill, T.M.; Barrett-Connor, E.; Swerdloff, R.S.; Wang, C.; et al. Lessons From the Testosterone Trials. Endocr. Rev. 2018, 39, 369–386. [Google Scholar]
- Shores, M.M.; Smith, N.L.; Forsberg, C.W.; Anawalt, B.D.; Matsumoto, A.M. Testosterone Treatment and Mortality in Men with Low Testosterone Levels. J. Clin. Endocrinol. Metab. 2012, 97, 2050–2058. [Google Scholar]
- Yang, C.; Li, P.; Li, Z. Clinical application of aromatase inhibitors to treat male infertility. Hum. Reprod. Update 2021, 28, 30–50. [Google Scholar]
- Dias, J.P.; Melvin, D.; Simonsick, E.M.; Carlson, O.; Shardell, M.D.; Ferrucci, L.; Chia, C.W.; Basaria, S.; Egan, J.M. Effects of aromatase inhibition vs. testosterone in older men with low testosterone: Randomized-controlled trial. Andrology 2016, 4, 33–40. [Google Scholar] [CrossRef] [PubMed]
- Maier, U.; Hienert, G. Tamoxifen and kallikrein in therapy of oligoasthenozoospermia: Results of a randomized study. Eur. Urol. 1990, 17, 223–225. [Google Scholar] [CrossRef] [PubMed]
- Maier, U.; Hienert, G. Tamoxifen and testolactone in therapy of oligozoospermia: Results of a randomized study. Eur. Urol. 1988, 14, 447–449. [Google Scholar] [CrossRef] [PubMed]
- AinMelk, Y.; Belisle, S.; Carmel, M.; Jean-Pierre, T. Tamoxifen citrate therapy in male infertility. Fertil. Steril. 1987, 48, 113–117. [Google Scholar] [CrossRef]
- Thaker, H.; Ko, E.Y.; Sabanegh, E.S.; Brannigan, R.E.; Alukal, J.P.; Samplaski, M.K. Empirical medical therapy for idiopathic male infertility. F S Rep. 2020, 1, 15–20. [Google Scholar] [CrossRef]
- Wallach, E.E.; Adashi, E.Y. Clomiphene citrate: Mechanism(s) and site(s) of action—A hypothesis revisited*. Fertil. Steril. 1984, 42, 331–344. [Google Scholar] [CrossRef] [PubMed]
- Kousta, E.; White, D.M.; Franks, S. Modern use of clomiphene citrate in induction of ovulation. Hum. Reprod. Update 1997, 3, 359–365. [Google Scholar]
- Gonen, Y.; Casper, R.F. Sonographic determination of a possible adverse effect of clomiphene citrate on endometrial growth. Hum. Reprod. 1990, 5, 670–674. [Google Scholar] [CrossRef]
- Shabsigh, A.; Kang, Y.; Shabsign, R.; Gonzalez, M.; Liberson, G.; Fisch, H.; Goluboff, E. Clomiphene Citrate Effects on Testosterone/Estrogen Ratio in Male Hypogonadism. J. Sex. Med. 2005, 2, 716–721. [Google Scholar]
- Ramasamy, R.; Scovell, J.M.; Kovac, J.R.; Lipshultz, L.I. Testosterone Supplementation Versus Clomiphene Citrate for Hypogonadism: An Age Matched Comparison of Satisfaction and Efficacy. J. Urol. 2014, 192, 875–879. [Google Scholar] [CrossRef]
- Helo, S.; Ellen, J.; Mechlin, C.; Feustel, P.; Grossman, M.; Ditkoff, E.; McCullough, A. A Randomized Prospective Double-Blind Comparison Trial of Clomiphene Citrate and Anastrozole in Raising Testosterone in Hypogonadal Infertile Men. J. Sex. Med. 2015, 12, 1761–1769. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Chan, C.-W.; Wong, K.-K.; Yeung, K.-K. Comparison of the effectiveness of placebo, clomiphene citrate, mesterolone, pentoxifylline, and testosterone rebound therapy for the treatment of idiopathic oligospermia. Fertil. Steril. 1983, 40, 358–365. [Google Scholar] [CrossRef] [PubMed]
- Goldstein, S.R.; Siddhanti, S.; Ciaccia, A.V.; Plouffe, L. A pharmacological review of selective oestrogen receptor modulators. Hum. Reprod. Update 2000, 6, 212–224. [Google Scholar] [CrossRef] [PubMed]
- Samplaski, M.K.; Loai, Y.; Wong, K.; Lo, K.C.; Grober, E.D.; Jarvi, K.A. Testosterone use in the male infertility population: Prescribing patterns and effects on semen and hormonal parameters. Fertil. Steril. 2014, 101, 64–69. [Google Scholar] [CrossRef]
- Bagatell, C.J.; Dahl, K.D.; Bremner, W.J. The direct pituitary effect of testosterone to inhibit gonadotropin secretion in men is partially mediated by aromatization to estradiol. J. Androl. 1994, 15, 15–21. [Google Scholar] [CrossRef]
- Vigersky, R.A.; Glass, A.R. Effects of delta 1-testolactone on the pituitary-testicular axis in oligospermic men. J. Clin. Endocrinol. Metab. 1981, 52, 897–902. [Google Scholar] [CrossRef]
- Dony, J.M.J.; Smals, A.G.H.; Rolland, R.; Fauser, B.C.J.M.; Thomas, C.M.G. Effect of chronic aromatase inhibition by delta 1-testolactone on pituitary-gonadal function in oligozoospermic men. Andrologia 1986, 18, 69–78. [Google Scholar] [CrossRef] [PubMed]
- Clark, R.V.; Sherins, R.J. Treatment of men with idiopathic oligozoospermic infertility using the aromatase inhibitor, testolactone. Results of a double-blinded, randomized, placebo-controlled trial with crossover. J. Androl. 1989, 10, 240–247. [Google Scholar] [CrossRef]
- Pavlovich, C.P.; King, P.; Goldstein, M.; Schlegel, P.N. Evidence of a treatable endocrinopathy in infertile men. J. Urol. 2001, 165, 837–841. [Google Scholar]
- Saylam, B.; Efesoy, O.; Çayan, S. The effect of aromatase inhibitor letrozole on body mass index, serum hormones, and sperm parameters in infertile men. Fertil. Steril. 2011, 95, 809–811. [Google Scholar] [CrossRef]
- Morley, J.E.; Charlton, E.; Patrick, P.; Kaiser, F.E.; Cadeau, P.; McCready, D.; Perry, H.M., 3rd. Validation of a screening questionnaire for androgen deficiency in aging males. Metabolism 2000, 49, 1239–1242. [Google Scholar] [CrossRef] [PubMed]
- Morley, J.E.; Perry, H.; Kevorkian, R.; Patrick, P. Comparison of screening questionnaires for the diagnosis of hypogonadism. Maturitas 2006, 53, 424–429. [Google Scholar] [CrossRef] [PubMed]
- Mohamed, O.; E Freundlich, R.; Dakik, H.K.; Grober, E.D.; Najari, B.; I Lipshultz, L.; Khera, M. The quantitative ADAM questionnaire: A new tool in quantifying the severity of hypogonadism. Int. J. Impot. Res. 2010, 22, 20–24. [Google Scholar] [CrossRef] [PubMed]
- Katz, D.J.; Nabulsi, O.; Tal, R.; Mulhall, J.P. Outcomes of clomiphene citrate treatment in young hypogonadal men. BJU Int. 2012, 110, 573–578. [Google Scholar] [CrossRef] [PubMed]
- Chandrapal, J.C.; Nielson, S.; Patel, D.P.; Zhang, C.; Presson, A.P.; Brant, W.O.; Myers, J.B.; Hotaling, J.M. Characterising the safety of clomiphene citrate in male patients through prostate-specific antigen, haematocrit, and testosterone levels. BJU Int. 2016, 118, 994–1000. [Google Scholar] [CrossRef] [PubMed]
- Moskovic, D.J.; Katz, D.J.; Akhavan, A.; Park, K.; Mulhall, J.P. Clomiphene citrate is safe and effective for long-term management of hypogonadism. BJU Int. 2012, 110, 1524–1528. [Google Scholar] [CrossRef]
- Habous, M.; Giona, S.; Tealab, A.; Aziz, M.; Williamson, B.; Nassar, M.; Abdelrahman, Z.; Remeah, A.; Abdelkader, M.; Binsaleh, S.; et al. Clomiphene citrate and human chorionic gonadotropin are both effective in restoring testosterone in hypogonadism: A short-course randomized study. BJU Int. 2018, 122, 889–897. [Google Scholar]
- Soares, A.H.; Horie, N.C.; Chiang, L.A.P.; Caramelli, B.; Matheus, M.G.; Campos, A.H.; Marti, L.C.; Rocha, F.A.; Mancini, M.C.; Costa, E.M.F.; et al. Effects of clomiphene citrate on male obesity-associated hypogonadism: A randomized, double-blind, placebo-controlled study. Int. J. Obes. 2018, 42, 953–963. [Google Scholar] [CrossRef]
- Guay, A.T.; Bansal, S.; Heatley, G.J. Effect of raising endogenous testosterone levels in impotent men with secondary hypogonadism: Double blind placebo-controlled trial with clomiphene citrate. J. Clin. Endocrinol. Metab. 1995, 80, 3546–3552. [Google Scholar]
- Guay, A.T.; Jacobson, J.; Perez, J.B.; Hodge, M.B.; Velasquez, E. Clomiphene increases free testosterone levels in men with both secondary hypogonadism and erectile dysfunction: Who does and does not benefit? Int. J. Impot. Res. 2003, 15, 156–165. [Google Scholar]
- Giagulli, V.A.; Silvestrini, A.; Bruno, C.; Triggiani, V.; Mordente, A.; Mancini, A. Is There Room for SERMs or SARMs as Alternative Therapies for Adult Male Hypogonadism? Int. J. Endocrinol. 2020, 2020, 9649838. [Google Scholar] [PubMed]
- Ide, V.; Vanderschueren, D.; Antonio, L. Treatment of Men with Central Hypogonadism: Alternatives for Testosterone Replacement Therapy. Int. J. Mol. Sci. 2020, 22, 21. [Google Scholar] [CrossRef] [PubMed]
- Holdcraft, R.W.; Braun, R.E. Hormonal regulation of spermatogenesis. Int. J. Androl. 2004, 27, 335–342. [Google Scholar] [PubMed]
- Rönnberg, L. The effect of clomiphene citrate on different sperm parameters and serum hormone levels in preselected infertile men: A controlled double-blind cross-over study. Int. J. Androl. 1980, 3, 479–486. [Google Scholar] [PubMed]
- Surbone, A.; Vaucher, L.; Primi, M.-P.; Leyvraz, C.; Pitteloud, N.; Ballabeni, P.; Mathevet, P.; Vulliemoz, N. Clomiphene citrate effect on testosterone level and semen parameters in 18 infertile men with low testosterone level and normal/low gonadotropines level. Eur. J. Obstet. Gynecol. Reprod. Biol. 2019, 238, 104–109. [Google Scholar]
- Mićić, S.; Dotlić, R. Evaluation of sperm parameters in clinical trial with clomiphene citrate of oligospermic men. J. Urol. 1985, 133, 221–222. [Google Scholar]
- Moradi, M.; Moradi, A.; Alemi, M.; Ahmadnia, H.; Abdi, H.; Ahmadi, A.; Bazargan-Hejazi, S. Safety and efficacy of clomiphene citrate and L-carnitine in idiopathic male infertility: A comparative study. Urol. J. 2010, 7, 188–193. [Google Scholar]
- Rowe, P.J.; Comhaire, F.; World Health Organization. A double-blind trial of clomiphene citrate for the treatment of idiopathic male infertility. Int. J. Androl. 1992, 15, 299–307. [Google Scholar]
- Chua, M.E.; Escusa, K.G.; Luna, S.; Tapia, L.C.; Dofitas, B.; Morales, M. Revisiting oestrogen antagonists (clomiphene or tamoxifen) as medical empiric therapy for idiopathic male infertility: A meta-analysis. Andrology 2013, 1, 749–757. [Google Scholar]
- Sokol, R.Z.; Steiner, B.S.; Bustillo, M.; Petersen, G.; Swerdloff, R.S. A controlled comparison of the efficacy of clomiphene citrate in male infertility. Fertil. Steril. 1988, 49, 865–870. [Google Scholar] [CrossRef]
- Huijben, M.; Lock, M.T.W.; de Kemp, V.F.; de Kort, L.M.; van Breda, H. Clomiphene citrate for men with hypogonadism: A systematic review and meta-analysis. Andrology 2022, 10, 451–469. [Google Scholar] [CrossRef]
- Wheeler, K.M.; Sharma, D.; Kavoussi, P.K.; Smith, R.P.; Costabile, R. Clomiphene Citrate for the Treatment of Hypogonadism. Sex. Med. Rev. 2019, 7, 272–276. [Google Scholar] [CrossRef] [PubMed]
- Yaşar, H.Y.; Ertuğrul, O. Clomiphene citrate-induced severe hypertriglyceridemia. Fertil. Steril. 2009, 92, e7–e8. [Google Scholar] [CrossRef] [PubMed]
- Castro, M.R.; Nguyen, T.T.; O’Brien, T. Clomiphene-induced severe hypertriglyceridemia and pancreatitis. Mayo Clin. Proc. 1999, 74, 1125–1128. [Google Scholar] [CrossRef] [PubMed]
- Da Ros, C.T.; Averbeck, M.A. Twenty-five milligrams of clomiphene citrate presents positive effect on treatment of male testosterone deficiency—A prospective study. Int. Braz. J. Urol. 2012, 38, 512–518. [Google Scholar] [CrossRef] [PubMed]
- Bendre, S.V.; Murray, P.J.; Basaria, S. Clomiphene Citrate Effectively Increases Testosterone in Obese, Young, Hypogonadal Men. Reprod. Syst. Sex. Disord. 2015, 4, 155. [Google Scholar]
- Ory, J.; Nackeeran, S.; Balaji, N.C.; Hare, J.M.; Ramasamy, R. Secondary Polycythemia in Men Receiving Testosterone Therapy Increases Risk of Major Adverse Cardiovascular Events and Venous Thromboembolism in the First Year of Therapy. J. Urol. 2022, 207, 1295–1301. [Google Scholar] [CrossRef]
- Drinka, P.J.; Jochen, A.L.; Cuisinier, M.; Bloom, R.; Rudman, I.; Rudman, D. Polycythemia as a complication of testosterone replacement therapy in nursing home men with low testosterone levels. J. Am. Geriatr. Soc. 1995, 43, 899–901. [Google Scholar]
- Fernández-Balsells, M.M.; Murad, M.H.; Lane, M.; Lampropulos, J.F.; Albuquerque, F.; Mullan, R.J.; Agrwal, N.; Elamin, M.B.; Gallegos-Orozco, J.F.; Wang, A.T.; et al. Adverse Effects of Testosterone Therapy in Adult Men: A Systematic Review and Meta-Analysis. J. Clin. Endocrinol. Metab. 2010, 95, 2560–2575. [Google Scholar] [CrossRef]
- Calof, O.M.; Singh, A.B.; Lee, M.L.; Kenny, A.M.; Urban, R.J.; Tenover, J.L.; Bhasin, S. Adverse Events Associated With Testosterone Replacement in Middle-Aged and Older Men: A Meta-Analysis of Randomized, Placebo-Controlled Trials. J. Gerontol. Ser. A 2005, 60, 1451–1457. [Google Scholar] [CrossRef]
- Pasqualotto, F.F.; Fonseca, G.P.; Pasqualotto, E.B. Azoospermia after treatment with clomiphene citrate in patients with oligospermia. Fertil. Steril. 2008, 90, 2014.e11–2014.e12. [Google Scholar] [CrossRef] [PubMed]
- Aftab, S.A.S.; Kumar, S.; Barber, T.M. The role of obesity and type 2 diabetes mellitus in the development of male obesity-associated secondary hypogonadism. Clin. Endocrinol. 2013, 78, 330–337. [Google Scholar] [CrossRef] [PubMed]
- Tienforti, D.; Castellini, C.; Di Giulio, F.; Totaro, M.; Dalmazio, G.; Spagnolo, L.; Muselli, M.; Corona, G.; Baroni, M.G.; Barbonetti, A. Selective modulation of estrogen receptor in obese men with androgen deficiency: A systematic review and meta-analysis. Andrology 2023, 11, 1067–1076. [Google Scholar] [CrossRef]
- Selvam, M.K.P.; Baskaran, S.; Tannenbaum, J.; Greenberg, J.; Shalaby, H.Y.; Hellstrom, W.J.G.; Sikka, S.C. Clomiphene Citrate in the Management of Infertility in Oligospermic Obese Men with Hypogonadism: Retrospective Pilot Study. Medicina 2023, 59, 1902. [Google Scholar] [CrossRef]
- Kim, E.D.; McCullough, A.; Kaminetsky, J. Oral enclomiphene citrate raises testosterone and preserves sperm counts in obese hypogonadal men, unlike topical testosterone: Restoration instead of replacement. BJU Int. 2016, 117, 677–685. [Google Scholar] [CrossRef]
- Dutta, D.; Mohindra, R.; Kumar, M.; Sharma, M. Role of Aromatase Inhibitors in Managing Hypogonadism in Adult Males Related to Obesity and Aging: A Systematic Review and Meta-Analysis. Indian J. Endocrinol. Metab. 2022, 26, 501–509. [Google Scholar] [CrossRef]
- Colleluori, G.; Chen, R.; Turin, C.G.; Vigevano, F.; Qualls, C.; Johnson, B.; Mediwala, S.; Villareal, D.T.; Armamento-Villareal, R. Aromatase Inhibitors Plus Weight Loss Improves the Hormonal Profile of Obese Hypogonadal Men Without Causing Major Side Effects. Front. Endocrinol. 2020, 11, 277. [Google Scholar] [CrossRef] [PubMed]
- Shah, T.; Nyirenda, T.; Shin, D. Efficacy of anastrozole in the treatment of hypogonadal, subfertile men with body mass index ≥25 kg/m2. Transl. Androl. Urol. 2021, 10, 1222–1228. [Google Scholar] [CrossRef]
- Lašaitė, L.; Čeponis, J.; Preikša, R.T.; Žilaitienė, B. Effects of two-year testosterone replacement therapy on cognition, emotions and quality of life in young and middle-aged hypogonadal men. Andrologia 2017, 49, e12633. [Google Scholar] [CrossRef]
- Alder, N.J.; Keihani, S.; Stoddard, G.J.; Myers, J.B.; Hotaling, J.M. Combination therapy with clomiphene citrate and anastrozole is a safe and effective alternative for hypoandrogenic subfertile men. BJU Int. 2018, 122, 688–694. [Google Scholar] [CrossRef]
- Taşkapu, H.H.; Sönmez, M.G.; Kılınç, M.T.; Altınkaya, N.; Aydın, A.; Balasar, M. Efficiency of intracavernosal alprostadil and oral clomiphene citrate combination treatment in penile vasculogenic erectile dysfunction patients accompanied by late-onset hypogonadism. Andrologia 2020, 52, e13759. [Google Scholar] [CrossRef] [PubMed]
- Ghanem, H.; Shaeer, O.; El-Segini, A. Combination clomiphene citrate and antioxidant therapy for idiopathic male infertility: A randomized controlled trial. Fertil. Steril. 2010, 93, 2232–2235. [Google Scholar] [CrossRef] [PubMed]
| Therapy | Mechanism of Action | Side Effects | Benefits | Risks |
|---|---|---|---|---|
| Testosterone Replacement Therapy | Administers exogenous testosterone through various formulations (oral, intramuscular, transdermal, subdermal, buccal, and nasal). | Associated with potential risks, including cardiovascular events, impaired fertility, obstructive sleep apnea, and erythrocytosis. | Supported by substantial long-term RCT evidence; FDA-approved to treat men with hypogonadism. | Risk of significant adverse effects, particularly erythrocytosis and infertility. |
| Aromatase Inhibitors | Inhibit the enzymatic conversion of testosterone to estradiol, reducing negative feedback on the HPG axis. | Common side effects include nausea, headache, and hot flashes. Less frequent effects include libido changes and elevated liver enzymes. Decreased bone mineral density has been reported. | Improves hypogonadal symptoms and fertility outcomes without causing major side effects. | Potential risk of decreased estradiol interfering with bone metabolism and associated symptoms; lack of long-term RCT data. |
| Tamoxifen | Blocks estrogen’s negative feedback on the hypothalamus and pituitary gland, leading to increased GnRH production, which subsequently boosts endogenous testosterone secretion. | Potential adverse effects include weight gain, sexual dysfunction, hot flashes, and neurocognitive impairment; rare reports of infertility and idiopathic gynecomastia. | Improves hypogonadal symptoms and fertility outcomes without significant side effects or suppression of estradiol. | Requires a functional HPG axis; lacks robust RCT evidence. |
| Clomiphene | Reported side effects include headaches, visual disturbances, dizziness, gynecomastia, and testicular enlargement; rare instances of azoospermia have been documented. | Improves hypogonadal symptoms and fertility outcomes without significant side effects or suppression of estradiol; particularly promising for men with obesity-related hypogonadism or those prioritizing fertility preservation; cost-effective compared to TRT. | Requires a functional HPG axis; high-quality RCTs and long-term follow-up data are needed to fully establish its safety and efficacy. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wu, Y.-C.; Sung, W.-W. Clomiphene Citrate Treatment as an Alternative Therapeutic Approach for Male Hypogonadism: Mechanisms and Clinical Implications. Pharmaceuticals 2024, 17, 1233. https://doi.org/10.3390/ph17091233
Wu Y-C, Sung W-W. Clomiphene Citrate Treatment as an Alternative Therapeutic Approach for Male Hypogonadism: Mechanisms and Clinical Implications. Pharmaceuticals. 2024; 17(9):1233. https://doi.org/10.3390/ph17091233
Chicago/Turabian StyleWu, Yao-Cheng, and Wen-Wei Sung. 2024. "Clomiphene Citrate Treatment as an Alternative Therapeutic Approach for Male Hypogonadism: Mechanisms and Clinical Implications" Pharmaceuticals 17, no. 9: 1233. https://doi.org/10.3390/ph17091233
APA StyleWu, Y.-C., & Sung, W.-W. (2024). Clomiphene Citrate Treatment as an Alternative Therapeutic Approach for Male Hypogonadism: Mechanisms and Clinical Implications. Pharmaceuticals, 17(9), 1233. https://doi.org/10.3390/ph17091233







