Pre- and Post-COVID-19 Antimicrobial Resistance Pattern of Pathogens in an Intensive Care Unit
Abstract
1. Introduction
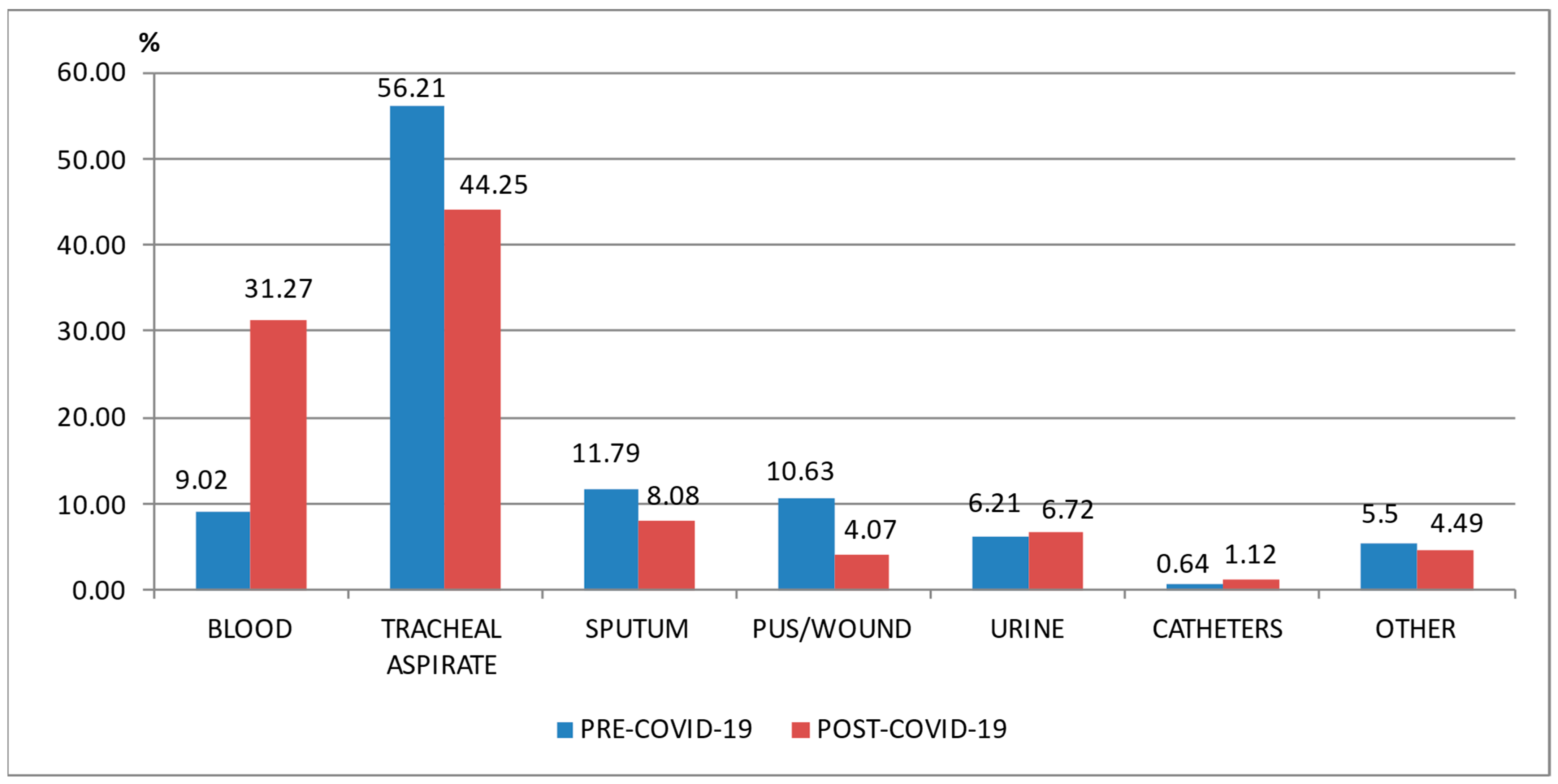
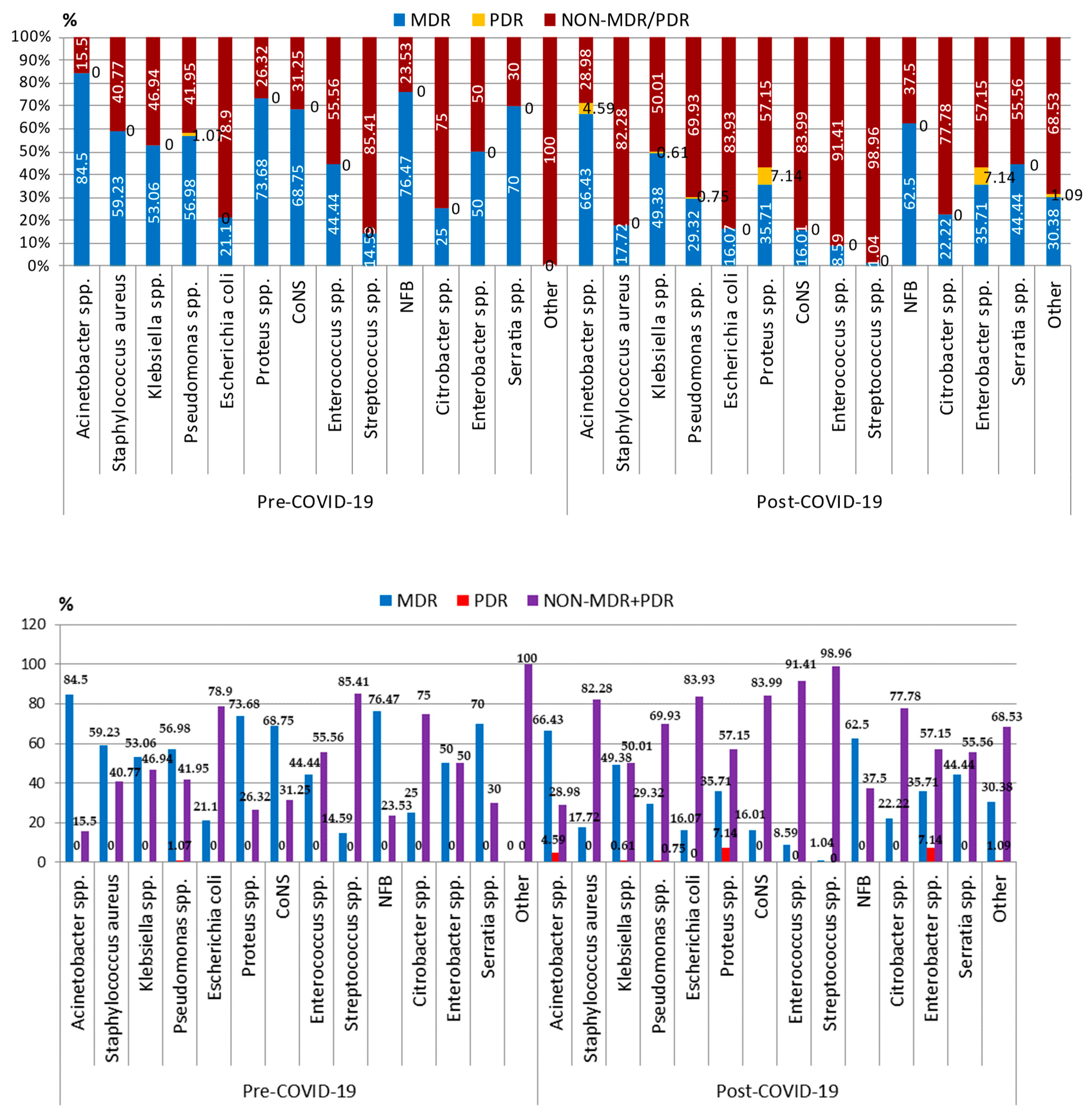
2. Results
3. Discussion
4. Materials and Methods
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- WHO. Antimicrobial Resistance. Available online: https://www.who.int/news-room/fact-sheets/detail/antimicrobial-resistance (accessed on 28 December 2021).
- ECDC. Antimicrobial Resistance in the EU/EEA: A One Health Response; ECDC: Stockholm, Sweden, 2021. [Google Scholar]
- Perez Jorge, G.; Rodrigues Dos Santos Goes, I.C.; Gontijo, M.T.P. Les miserables: A Parallel Between Antimicrobial Resistance and COVID-19 in Underdeveloped and Developing Countries. Curr. Infect. Dis. Rep. 2022, 24, 175–186. [Google Scholar] [CrossRef] [PubMed]
- Pidot, S.J.; Gao, W.; Buultjens, A.H.; Monk, I.R.; Guerillot, R.; Carter, G.P.; Lee, J.Y.H.; Lam, M.M.C.; Grayson, M.L.; Ballard, S.A.; et al. Increasing tolerance of hospital Enterococcus faecium to handwash alcohols. Sci. Transl. Med. 2018, 10, eaar6115. [Google Scholar] [CrossRef] [PubMed]
- Subramanya, S.H.; Czyz, D.M.; Acharya, K.P.; Humphreys, H. The potential impact of the COVID-19 pandemic on antimicrobial resistance and antibiotic stewardship. VirusDisease 2021, 32, 330–337. [Google Scholar] [CrossRef] [PubMed]
- ECDC. Antimicrobial Resistance in the EU/EEA (EARS-Net)—Annual Epidemiological Report 2022; ECDC: Stockholm, Sweden, 2023. [Google Scholar]
- INSP-CNSCBT. Analysis of the Evolution of Communicable Diseases under Surveillance—Report for 2020 and 2021; Institutul National de Sanatate Publica: Bucuresti, Romania, 2022; pp. 2394–2537. [Google Scholar]
- Rehman, S. A parallel and silent emerging pandemic: Antimicrobial resistance (AMR) amid COVID-19 pandemic. J. Infect. Public Health 2023, 16, 611–617. [Google Scholar] [CrossRef] [PubMed]
- WHO. Global Action Plan on Antimicrobial Resistance; WHO: Geneva, Switzerland, 2016. [Google Scholar]
- Chedid, M.; Waked, R.; Haddad, E.; Chetata, N.; Saliba, G.; Choucair, J. Antibiotics in treatment of COVID-19 complications: A review of frequency, indications, and efficacy. J. Infect. Public Health 2021, 14, 570–576. [Google Scholar] [CrossRef] [PubMed]
- Granata, G.; Schiavone, F.; Pipitone, G.; Taglietti, F.; Petrosillo, N. Antibiotics Use in COVID-19 Patients: A Systematic Literature Review. J. Clin. Med. 2022, 11, 7207. [Google Scholar] [CrossRef]
- Greco, R.; Panetta, V.; Della Rocca, M.T.; Durante, A.; Di Caprio, G.; Maggi, P. Profile of Co-Infection Prevalence and Antibiotics Use among COVID-19 Patients. Pathogens 2022, 11, 1250. [Google Scholar] [CrossRef]
- Malik, S.S.; Mundra, S. Increasing Consumption of Antibiotics during the COVID-19 Pandemic: Implications for Patient Health and Emerging Anti-Microbial Resistance. Antibiotics 2022, 12, 45. [Google Scholar] [CrossRef]
- Hosseini, M.; Ahmed Hamad, M.; Mohseni, G.; Salamy, S.; Dehghan Tarzjani, S.; Taati Moghadam, M. Prediction of tsunami of resistance to some antibiotics is not far-fetched which used during COVID-19 pandemic. J. Clin. Lab. Anal. 2023, 37, e24959. [Google Scholar] [CrossRef]
- INSP. CARMIAAM-ROM 2020 (Consumul de Antibiotice, Rezistența Microbiană și Infecții Asociate Asistenței Medicale în România—2020; INSP: Bucuresti, Romania, 2020. [Google Scholar]
- Mares, C.; Petca, R.C.; Petca, A.; Popescu, R.I.; Jinga, V. Does the COVID Pandemic Modify the Antibiotic Resistance of Uropathogens in Female Patients? A New Storm? Antibiotics 2022, 11, 376. [Google Scholar] [CrossRef]
- Mares, C.; Petca, R.C.; Popescu, R.I.; Petca, A.; Geavlete, B.F.; Jinga, V. Uropathogens’ Antibiotic Resistance Evolution in a Female Population: A Sequential Multi-Year Comparative Analysis. Antibiotics 2023, 12, 948. [Google Scholar] [CrossRef] [PubMed]
- Golli, A.-L.; Nițu, F.M.; Bălășoiu, M.; Rascu, S.; Lungu, M.A.; Dinescu, S.N.; Ciobanu-Mitrache, L.; Glodeanu, A.; Văcaru, M.; Olteanu, M. Microbiological profile and antibiotic resistance pattern of bacterial uropathogens among hospitalized patients. Farmacia 2019, 67, 167–173. [Google Scholar] [CrossRef]
- Das, S.; Gladston, J.; Silvanose, C. The Silent Pandemic by Super Pathogens during the COVID-19 Pandemic. Preprint 2023. [Google Scholar] [CrossRef]
- Kishk, R.M.; Abu Bakr, N.M.; Anani, M.; Nemr, N.; Salama, B.M.; Samahy, M.; Kishk, S.M.; Salem, N.E.; Mohamed, H.A. Pattern of antimicrobial resistance in the pre and during COVID-19 era: An observational study. Microbes Infect. Dis. 2023, 4, 1100–1113. [Google Scholar] [CrossRef]
- Hurtado, I.C.; Valencia, S.; Pinzon, E.M.; Lesmes, M.C.; Sanchez, M.; Rodriguez, J.; Ochoa, B.; Shewade, H.D.; Edwards, J.K.; Hann, K.; et al. Antibiotic resistance and consumption before and during the COVID-19 pandemic in Valle del Cauca, Colombia. Rev. Panam. Salud Publica 2023, 47, e10. [Google Scholar] [CrossRef] [PubMed]
- Iqbal, S.; Hussain, S.S. Impact of COVID-19 Pandemic on Antimicrobial Resistance Pattern; Transition from Resistivity to Susceptibility. Glob. J. Med. Pharm. Biomed. Update 2022, 17, 5–6. [Google Scholar] [CrossRef]
- Taleb, M.H.; Elmanama, A.A.; Taleb, A.H.; Tawfick, M.M. Pre- and post-COVID-19 antimicrobial resistance profile of bacterial pathogens, a comparative study in a tertiary hospital. J. Infect. Dev. Ctries. 2023, 17, 597–609. [Google Scholar] [CrossRef]
- Parisini, A.; Boni, S.; Vacca, E.B.; Bobbio, N.; Puente, F.D.; Feasi, M.; Prinapori, R.; Lattuada, M.; Sartini, M.; Cristina, M.L.; et al. Impact of the COVID-19 Pandemic on Epidemiology of Antibiotic Resistance in an Intensive Care Unit (ICU): The Experience of a North-West Italian Center. Antibiotics 2023, 12, 1278. [Google Scholar] [CrossRef]
- Raoofi, R.; Namavari, N.; Rahmanian, V.; Dousthaghi, M.H. Evaluation of antibiotics resistance in Southern Iran in light of COVID-19 pandemic: A retrospective observational study. Health Sci. Rep. 2023, 6, e1153. [Google Scholar] [CrossRef]
- Khaznadar, O.; Khaznadar, F.; Petrovic, A.; Kuna, L.; Loncar, A.; Omanovic Kolaric, T.; Mihaljevic, V.; Tabll, A.A.; Smolic, R.; Smolic, M. Antimicrobial Resistance and Antimicrobial Stewardship: Before, during and after the COVID-19 Pandemic. Microbiol. Res. 2023, 14, 727–740. [Google Scholar] [CrossRef]
- Petrakis, V.; Panopoulou, M.; Rafailidis, P.; Lemonakis, N.; Lazaridis, G.; Terzi, I.; Papazoglou, D.; Panagopoulos, P. The Impact of the COVID-19 Pandemic on Antimicrobial Resistance and Management of Bloodstream Infections. Pathogens 2023, 12, 780. [Google Scholar] [CrossRef]
- Golli, A.L.; Nitu, F.M.; Balasoiu, M.; Lungu, M.A.; Dragomirescu, C.C.; Olteanu, M.; Nemes, R.M.; Tantu, M.M.; Olteanu, M. The Characterization of Antibiotic Resistance of Bacterial Isolates from Intensive Care Unit Patient Samples in a University Affiliated Hospital in Romania. Rev. Chim. 2019, 70, 1778–1783. [Google Scholar] [CrossRef]
- Golli, A.L.; Nitu, F.M.; Balasoiu, M.; Lungu, M.A.; Olteanu, M.; Nemes, R.M.; Fortofoiu, M.; Rusu, E.; Olteanu, M. Antibiotic Resistance Pattern of Bacterial Pathogens in Elderly Patients Admitted in the Intensive Care Unit. Rev. Chim. 2018, 69, 3433–3438. [Google Scholar] [CrossRef]
- Golli, A.L.; Nitu, F.M.; Balasoiu, M.; Nemes, R.M.; Tudorache, S.I.; Mahler Boca, B.; Olteanu, M. Bacterial Isolates from Endotracheal Aspirates and their Antimicrobial Resistance Pattern in Patients from Intensive Care Unit. Rev. Chim. 2019, 70, 3299–3304. [Google Scholar] [CrossRef]
- Golli, A.L.; Cristea, O.M.; Zlatian, O.; Glodeanu, A.D.; Balasoiu, A.T.; Ionescu, M.; Popa, S. Prevalence of Multidrug-Resistant Pathogens Causing Bloodstream Infections in an Intensive Care Unit. Infect. Drug Resist. 2022, 15, 5981–5992. [Google Scholar] [CrossRef]
- Catalano, A.; Iacopetta, D.; Ceramella, J.; Pellegrino, M.; Giuzio, F.; Marra, M.; Rosano, C.; Saturnino, C.; Sinicropi, M.S.; Aquaro, S. Antibiotic-Resistant ESKAPE Pathogens and COVID-19: The Pandemic beyond the Pandemic. Viruses 2023, 15, 1843. [Google Scholar] [CrossRef] [PubMed]
- Meschiari, M.; Onorato, L.; Bacca, E.; Orlando, G.; Menozzi, M.; Franceschini, E.; Bedini, A.; Cervo, A.; Santoro, A.; Sarti, M.; et al. Long-Term Impact of the COVID-19 Pandemic on In-Hospital Antibiotic Consumption and Antibiotic Resistance: A Time Series Analysis (2015–2021). Antibiotics 2022, 11, 826. [Google Scholar] [CrossRef] [PubMed]
- Khoshbakht, R.; Kabiri, M.; Neshani, A.; Khaksari, M.N.; Sadrzadeh, S.M.; Mousavi, S.M.; Ghazvini, K.; Ghavidel, M. Assessment of antibiotic resistance changes during the COVID-19 pandemic in northeast of Iran during 2020-2022: An epidemiological study. Antimicrob. Resist. Infect. Control. 2022, 11, 121. [Google Scholar] [CrossRef] [PubMed]
- Cogliati Dezza, F.; Arcari, G.; Alessi, F.; Valeri, S.; Curtolo, A.; Sacco, F.; Ceccarelli, G.; Raponi, G.; Alessandri, F.; Mastroianni, C.M.; et al. Clinical Impact of COVID-19 on Multi-Drug-Resistant Gram-Negative Bacilli Bloodstream Infections in an Intensive Care Unit Setting: Two Pandemics Compared. Antibiotics 2022, 11, 926. [Google Scholar] [CrossRef] [PubMed]
- Magiorakos, A.P.; Srinivasan, A.; Carey, R.B.; Carmeli, Y.; Falagas, M.E.; Giske, C.G.; Harbarth, S.; Hindler, J.F.; Kahlmeter, G.; Olsson-Liljequist, B.; et al. Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: An international expert proposal for interim standard definitions for acquired resistance. Clin. Microbiol. Infect. 2012, 18, 268–281. [Google Scholar] [CrossRef] [PubMed]
- INSP-CNSCBT. Sentinel Surveillance Methodology for Healthcare Associated Infections and Antimicrobial Resistance; Institutul National de Sanatate Publica: Bucuresti, Romania, 2018. [Google Scholar]
- Zlatian, O.; Balasoiu, A.T.; Balasoiu, M.; Cristea, O.; Docea, A.O.; Mitrut, R.; Spandidos, D.A.; Tsatsakis, A.M.; Bancescu, G.; Calina, D. Antimicrobial resistance in bacterial pathogens among hospitalised patients with severe invasive infections. Exp. Ther. Med. 2018, 16, 4499–4510. [Google Scholar] [CrossRef] [PubMed]
- CLSI. Performance Standards for Antimicrobial Susceptibility Testing, 30th ed.; CLSI Supplement, M100; Clinical & Laboratory Standards Institute: Berwyn, PA, USA, 2020. [Google Scholar]
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gotzsche, P.C.; Vandenbroucke, J.P.; Initiative, S. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. BMJ 2007, 335, 806–808. [Google Scholar] [CrossRef] [PubMed]
| Patients | Pre-COVID-19 (No = 1267) | Post-COVID-19 (No = 1354) | |
|---|---|---|---|
| Gender | Male | 797 (62.90%) | 841 (62.11%) |
| Female | 470 (37.10%) | 513 (37.89%) | |
| Age (Mean ± SD) | 64 ± 18.60 | 64 ± 17.51 |
| Sample | Species | ||||||
|---|---|---|---|---|---|---|---|
| Total | Acinetobacter spp. | E. coli | Klebsiella spp. | Proteus spp. | Pseudomonas spp. | ||
| Blood | Pre-COVID-19 | 154 | 6 (3.90%) | 17 (11.04%) | 4 (2.59%) | 7 (4.54%) | 85 (55.2%) |
| Post-COVID-19 | 613 | 29 (4.73%) | 35 (5.71%) | 5 (0.81%) | 9 (1.47%) | 246 (40.13%) | |
| Tracheal aspirate/Sputum | Pre-COVID-19 | 1355 | 40 (2.95%) | 234 (17.27%) | 90 (6.64%) | 58 (4.28%) | 27 (1.99%) |
| Post-COVID-19 | 1294 | 72 (5.56%) | 226 (17.47%) | 90 (6.96%) | 94 (7.26%) | 2 (0.15%) | |
| Pus/wound swabs | Pre-COVID-19 | 215 | 23 (10.70%) | 32 (14.88%) | 27 (12.56%) | 19 (8.84%) | 10 (4.65%) |
| Post-COVID-19 | 124 | 13 (10.48%) | 25 (20.16%) | 16 (12.91%) | 10 (8.06%) | 6 (4.84%) | |
| Urine | Pre-COVID-19 | 108 | 31 (28.70%) | 33 (30.56%) | 4 (3.70%) | 2 (1.85%) | 0 (0%) |
| Post-COVID-19 | 115 | 38 (33.04%) | 16 (13.92%) | 10 (8.69%) | 5 (4.35%) | 0 (0%) | |
| Catheters | Pre-COVID-19 | 10 | 0 (0%) | 1 (10%) | 0 (0%) | 1 (10%) | 0 (0%) |
| Post-COVID-19 | 29 | 1 (3.44%) | 5 (17.24%) | 5 (17.24%) | 2 (6.90%) | 0 (0%) | |
| Other | Pre-COVID-19 | 98 | 9 (9.18%) | 26 (26.53%) | 8 (8.17%) | 6 (6.12%) | 6 (6.12%) |
| Post-COVID-19 | 106 | 15 (14.15%) | 19 (17.93%) | 12 (11.32%) | 13 (12.27%) | 2 (1.88%) | |
| Total | Pre-COVID-19 | 1940 | 109 (5.62%) | 343 (17.68%) | 133 (6.86%) | 93 (4.80%) | 128 (6.59%) |
| Post-COVID-19 | 2281 | 283 (12.41%) | 168 (7.36%) | 326 (14.92%) | 138 (6.05%) | 133 (5.83%) | |
| Sample | Species | ||||||
| CoNS | S. aureus | Streptococcus spp. | Enterococcus spp. | Other Species | |||
| Blood | Pre-COVID-19 | 85 (55.2%) | 9 (5.85%) | 10 (6.5%) | 5 (3.25%) | 4 (2.59%) | |
| Post-COVID-19 | 246 (40.13%) | 31 (5.05%) | 12 (1.96%) | 46 (7.5%) | 150 (24.47%) | ||
| Tracheal aspirate/Sputum | Pre-COVID-19 | 27 (1.99%) | 407 (30.04%) | 263 (19.41%) | 0 (0%) | 62 (4.58%) | |
| Post-COVID-19 | 2 (0.15%) | 364 (28.13%) | 173 (13.3%) | 38 (2.94%) | 34 (2.63%) | ||
| Pus/wound swabs | Pre-COVID-19 | 10 (4.65%) | 49 (22.79%) | 4 (1.86%) | 8 (3.72%) | 21 (9.77%) | |
| Post-COVID-19 | 6 (4.84%) | 16 (12.91%) | 5 (4.03%) | 5 (4.03%) | 12 (9.67%) | ||
| Urine | Pre-COVID-19 | 0 (0%) | 1 (0.93%) | 1 (0.93%) | 26 (24.07%) | 9 (8.33%) | |
| Post-COVID-19 | 0 (0%) | 0 (0%) | 0 (0%) | 34 (29.56%) | 12 (10.44%) | ||
| Catheters | Pre-COVID-19 | 0 (0%) | 5 (50%) | 0 (0%) | 0 (0%) | 2 (20%) | |
| Post-COVID-19 | 0 (0%) | 8 (27.59%) | 0 (0%) | 2 (6.90%) | 2 (6.90%) | ||
| Other | Pre-COVID-19 | 6 (6.12%) | 22 (22.54%) | 3 (3.06%) | 6 (6.12%) | 4 (4.08%) | |
| Post-COVID-19 | 2 (1.88%) | 21 (19.81%) | 2 (1.88%) | 3 (2.83%) | 7 (6.61%) | ||
| Total | Pre-COVID-19 | 128 (6.59%) | 493 (25.41%) | 281 (14.48%) | 45 (2.32%) | 102 (5.26%) | |
| Post-COVID-19 | 256 (11.22%) | 440 (19.29%) | 192 (8.42%) | 128 (5.61%) | 217 (9.52%) | ||
| Klebsiella spp. | Escherichia coli | Pseudomonas spp. | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Antimicrobial Agent | Pre-COVID-19 (n = 343) | Post-COVID-19 (n = 326) | p Value | Pre-COVID-19 (n = 109) | Post-COVID-19 (n = 168) | p Value | Pre-COVID-19 (n = 93) | Post-COVID-19 (n = 133) | p Value |
| Amoxicillin/ clavulanic acid | 217 (66.36%) | 194 (62.98%) | 0.15 | 31 (29.52%) | 60 (36.58%) | 0.23 | 18 (100%) | 7 (87.5%) | 0.12 |
| Ceftazidime | 209 (65.31%) | 223 (69.68%) | 0.23 | 32 (31.68%) | 64 (38.55%) | 0.25 | 53 (60.92%) | 86 (67.72%) | 0.30 |
| Ceftriaxone | 213 (65.34%) | 212 (67.30%) | 0.59 | 37 (35.58%) | 55 (33.95%) | 0.78 | 14 (82.35%) | 7 (70%) | 0.45 |
| Cefotaxime | 99 (65.56%) | 137 (65.55%) | <0.001 * | 7 (26.92%) | 40 33.78% | 0.31 | 9 (75%) | 9 (81.82%) | 0.69 |
| Cefazolin | 152 (77.16%) | 211 (79.32%) | 0.57 | 32 (57.14%) | 62 (51.24%) | 0.46 | 5 (100%) | 6 (100%) | - |
| Cefepime | 132 (61.68%) | 172 (55.30%) | 0.14 | 21 (33.33%) | 40 (25.97%) | 0.27 | 52 (76.47%) | 55 (58.51%) | 0.01 * |
| Imipenem | 108 (40.60%) | 113 (45.56%) | 0.25 | 16 (16.49%) | 7 (6.14%) | 0.01 * | 45 (58.44%) | 35 (47.30%) | 0.17 |
| Meropenem | 111 (45.68%) | 106 (44.35%) | 0.76 | 2 (2.60%) | 9 (9.57%) | 0.06 | 52 (65%) | 47 (57.32%) | 0.31 |
| Ciprofloxacin | 199 (59.76%) | 179 (61.30%) | 0.69 | 43 (39.82%) | 64 (43.54%) | 0.74 | 49 (55.68%) | 76 (62.29%) | 0.33 |
| Levofloxacin | 40 (55.56%) | 82 (59%) | 0.63 | 13 (52%) | 21 (28.76%) | 0.03 | 31 (60.78%) | 49 (56.98%) | 0.21 |
| Piperacillin/tazobactam | 35 (71.43%) | 119 (61.34%) | 0.19 | 0 (0%) | 24 (24%) | 0.14 | 28 (36.84%) | 39 (47.56%) | 0.36 |
| Colistin | 1 (0.38%) | 40 (20.51%) | <0.001 * | 3 (4.69%) | 25 (32.46%) | <0.001 * | 0 (0%) | 4 (4.88%) | 0.03 |
| Gentamicin | 112 (44.62%) | 203 (64.85%) | <0.001 * | 21 (36.94%) | 60 (37.73%) | 0.90 | 38 (61.29%) | 77 (60.63%) | 0.93 |
| Aztreonam | 182 (56.35%) | 180 (73.60%) | <0.001 * | 27 (27%) | 31 (27.43%) | 0.94 | 39 (50%) | 34 (39.08%) | 0.15 |
| Acinetobacter spp. | Proteus spp. | ||||||||
| Antimicrobial Agent | Pre-COVID-19 (n = 213) | Post-COVID-19 (n = 283) | p Value | Pre-COVID-19 (n = 133) | Post-COVID-19 (n = 138) | p Value | |||
| Amoxicillin/ clavulanic acid | 87 (94.57%) | 47 (100%) | 0.10 | 100 (78.13%) | 96 (73.85%) | 0.42 | |||
| Ceftazidime | 165 (93.75%) | 265 (96.01%) | 0.27 | 89 (72.95%) | 100 (73.53%) | 0.91 | |||
| Ceftriaxone | 189 (97.73%) | 270 (97.12%) | 0.84 | 99 (76.15%) | 91 (67.41%) | 0.11 | |||
| Cefotaxime | 159 (95.78%) | 230 (95.43%) | 0.86 | 45 (80.36%) | 71 (72.45%) | 0.27 | |||
| Cefazolin | 52 (100%) | 49 (100%) | - | 80 (94.12%) | 103 (84.43%) | 0.03 * | |||
| Cefepime | 132 (95.65%) | 141 (84.43%) | <0.001 * | 40 (54.80%) | 28 (21.37%) | <0.001 * | |||
| Imipenem | 77 (90.58%) | 156 (90.17%) | 0.91 | 49 (46.67%) | 33 (36.67%) | 0.15 | |||
| Meropenem | 150 (88.76%) | 192 (88.48%) | 0.93 | 19 (19.79%) | 10 (22.73%) | 0.69 | |||
| Ciprofloxacin | 190 (92.23%) | 165 (94.83%) | 0.30 | 82 (68.33%) | 93 (75%) | 0.24 | |||
| Levofloxacin | 47 (88.68%) | 104 (88.88%) | 0.96 | 20 (86.96%) | 41 (75.93%) | 0.27 | |||
| Piperacillin/ tazobactam | 118 (86.76%) | 186 (91.62%) | 0.14 | 0 (0%) | 20 (26.32%) | 0.06 | |||
| Colistin | 7 (3.37%) | 36 (18.09%) | <0.001 * | 95 (100%) | 56 (100%) | - | |||
| Gentamicin | 70 (86.42%) | 236 (85.19%) | 0.78 | 72 (76.59%) | 75 (55.97%) | 0.001 * | |||
| Aztreonam | 77 (96.25%) | 47 (81.03%) | 0.003 * | 34 (27.2%) | 24 (26.97%) | 0.96 | |||
| Staphylococcus aureus | CoNS | |||||
|---|---|---|---|---|---|---|
| Antimicrobial Agent | Pre- COVID-19 (n = 493) | Post-COVID-19 (n = 440) | p Value | Pre-COVID-19 (n = 128) | Post-COVID-19 (n = 256) | p Value |
| Ciprofloxacin | 296 (61.67%) | 259 (59.27%) | 0.45 | 90 (70.87%) | 149 (59.36%) | 0.18 |
| Clindamycin | 366 (76.25%) | 259 (77.72%) | 0.59 | 85 (66.93%) | 163 (68.20%) | 0.80 |
| Clarithromycin | 219 (56.74%) | 243 (60.90%) | 0.23 | 73 (67.60%) | 54 (73.97%) | 0.35 |
| Doxycycline | 190 (40.08%) | 135 (51.72%) | 0.002 * | 52 (54.74%) | 7 (43.75%) | 0.41 |
| Erythromycin | 359 (74.17%) | 239 (55.58%) | <0.001 * | 100 (80.65%) | 99 (68.27%) | 0.02 * |
| Linezolid | 1 (0.22%) | 8 (3.13%) | <0.001 * | 16 (23.88%) | 11 (9.65%) | 0.009 |
| Penicillin | 474 (98.34%) | 382 (87.01%) | <0.001 * | 112 (93.33%) | 231 (93.52%) | 0.94 |
| Rifampicin | 252 (53.16%) | 263 (64.93%) | <0.001 * | 57 (45.24%) | 157 (62.55%) | 0.001 * |
| Tetracycline | 224 (62.57%) | 25 (78.12%) | 0.07 | 85 (71.43%) | 81 (72.32%) | 0.88 |
| Oxacillin | 354 (72.99%) | 229 (73.40%) | 0.89 | 104 (81.89%) | 119 (76.28%) | 0.25 |
| Vancomycin | 2 (16.67%) | 1 (3.58%) | 0.14 | 12 (15.79%) | 1 (0.91%) | <0.001 * |
| Teicoplanin | 5 (26.31%) | 55 (53.40%) | 0.03 * | 16 (26.67%) | 96 (63.57%) | <0.001 * |
| Streptococcus spp. | Enterococcus spp. | |||||
| Antimicrobial Agent | Pre-COVID-19 (n = 281) | Post-COVID-19 (n = 192) | p Value | Pre-COVID-19(n = 45) | Post-COVID-19 (n = 128) | p Value |
| Ciprofloxacin | 5 (100%) | 3 (100%) | - | 37 (86.05%) | 91 (72.8%) | 0.07 |
| Clindamycin | 80 (29.31%) | 50 (27.03%) | 0.59 | 1 (100%) | 1 (50%) | - |
| Clarithromycin | 84 (49.12%) | 53 (27.03%) | <0.001 * | 4 (100%) | 5 (71.43%) | 0.23 |
| Doxycycline | 24 (10.57%) | 16 (19.75%) | 0.03 * | 25 (80.65%) | 19 (33.33%) | <0.001 * |
| Erythromycin | 144 (52.55%) | 46 (29.11%) | <0.001 * | 6 (100%) | 42 (75%) | 0.16 |
| Linezolid | 0 (0%) | 0 (0%) | - | 2 (4.54%) | 1 (1.20%) | 0.23 |
| Penicillin | 200 (85.11%) | 74 (62.18%) | <0.001 * | 16 (38.09%) | 60 (61.22%) | 0.01 * |
| Rifampicin | 4 (20%) | 3 (3.61%) | 0.008 | - | 19 (51.35%) | - |
| Tetracycline | 41 (35.04%) | 34 (32.69%) | 0.71 | 6 (75%) | 13 (41.93%) | 0.09 |
| Oxacillin | 170 (91.89%) | 37 (87.70%) | 0.73 | - | 24 (96%) | - |
| Vancomycin | 3 (1.11%) | 0 (0%) | 0.26 | 7 (29.17%) | 4 (5.33%) | 0.001 * |
| Teicoplanin | - | - | - | 12 (29.27%) | 27 (36.98%) | 0.40 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Golli, A.-L.; Zlatian, O.M.; Cara, M.L.; Olteanu, M. Pre- and Post-COVID-19 Antimicrobial Resistance Pattern of Pathogens in an Intensive Care Unit. Pharmaceuticals 2024, 17, 407. https://doi.org/10.3390/ph17040407
Golli A-L, Zlatian OM, Cara ML, Olteanu M. Pre- and Post-COVID-19 Antimicrobial Resistance Pattern of Pathogens in an Intensive Care Unit. Pharmaceuticals. 2024; 17(4):407. https://doi.org/10.3390/ph17040407
Chicago/Turabian StyleGolli, Andreea-Loredana, Ovidiu Mircea Zlatian, Monica Laura Cara, and Mădălina Olteanu. 2024. "Pre- and Post-COVID-19 Antimicrobial Resistance Pattern of Pathogens in an Intensive Care Unit" Pharmaceuticals 17, no. 4: 407. https://doi.org/10.3390/ph17040407
APA StyleGolli, A.-L., Zlatian, O. M., Cara, M. L., & Olteanu, M. (2024). Pre- and Post-COVID-19 Antimicrobial Resistance Pattern of Pathogens in an Intensive Care Unit. Pharmaceuticals, 17(4), 407. https://doi.org/10.3390/ph17040407






