Silk Fibroin Nanofibers: Advancements in Bioactive Dressings through Electrospinning Technology for Diabetic Wound Healing
Abstract
1. Introduction
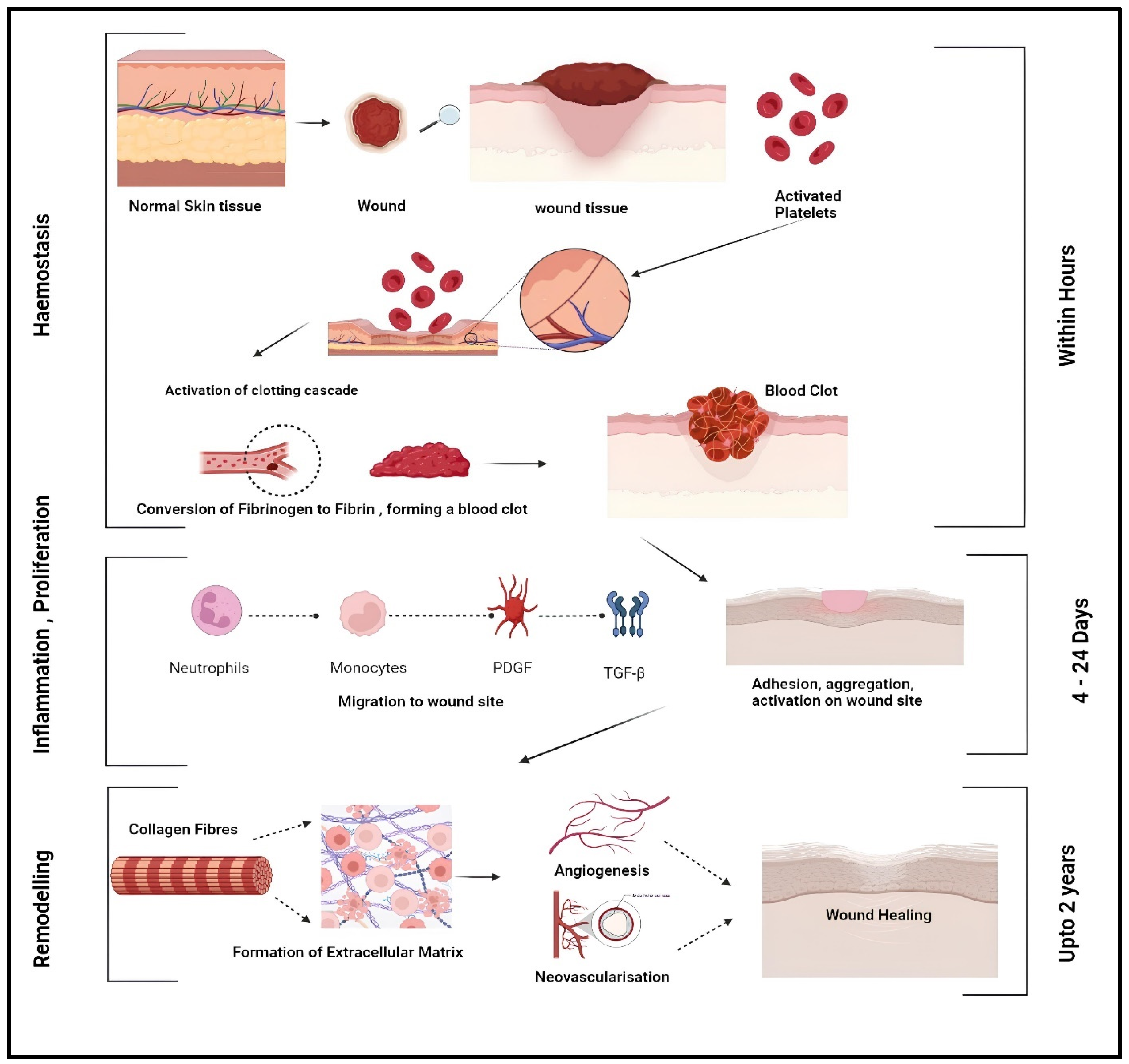
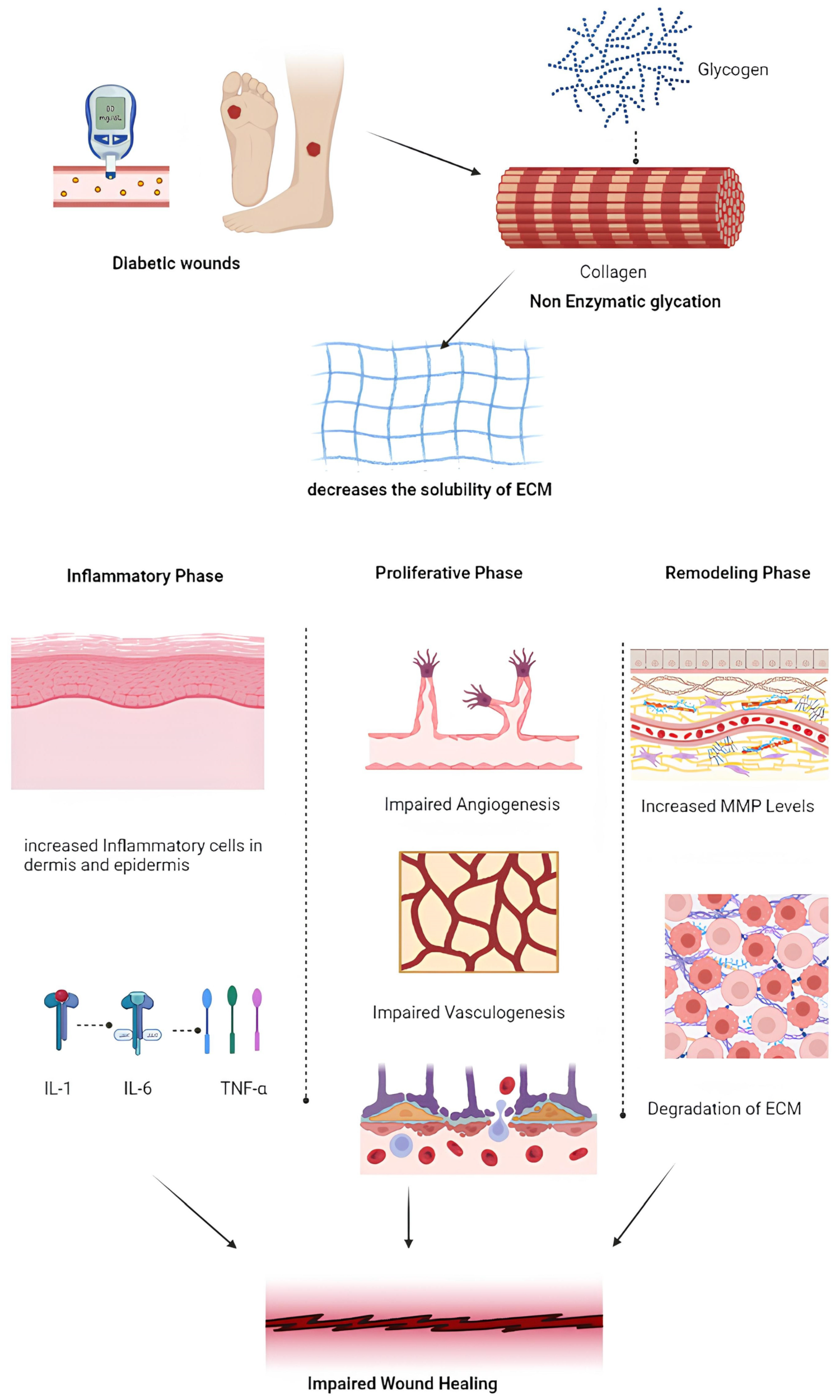
2. Pathogenesis and Intricate Mechanisms of Non-Healing Diabetic Wounds
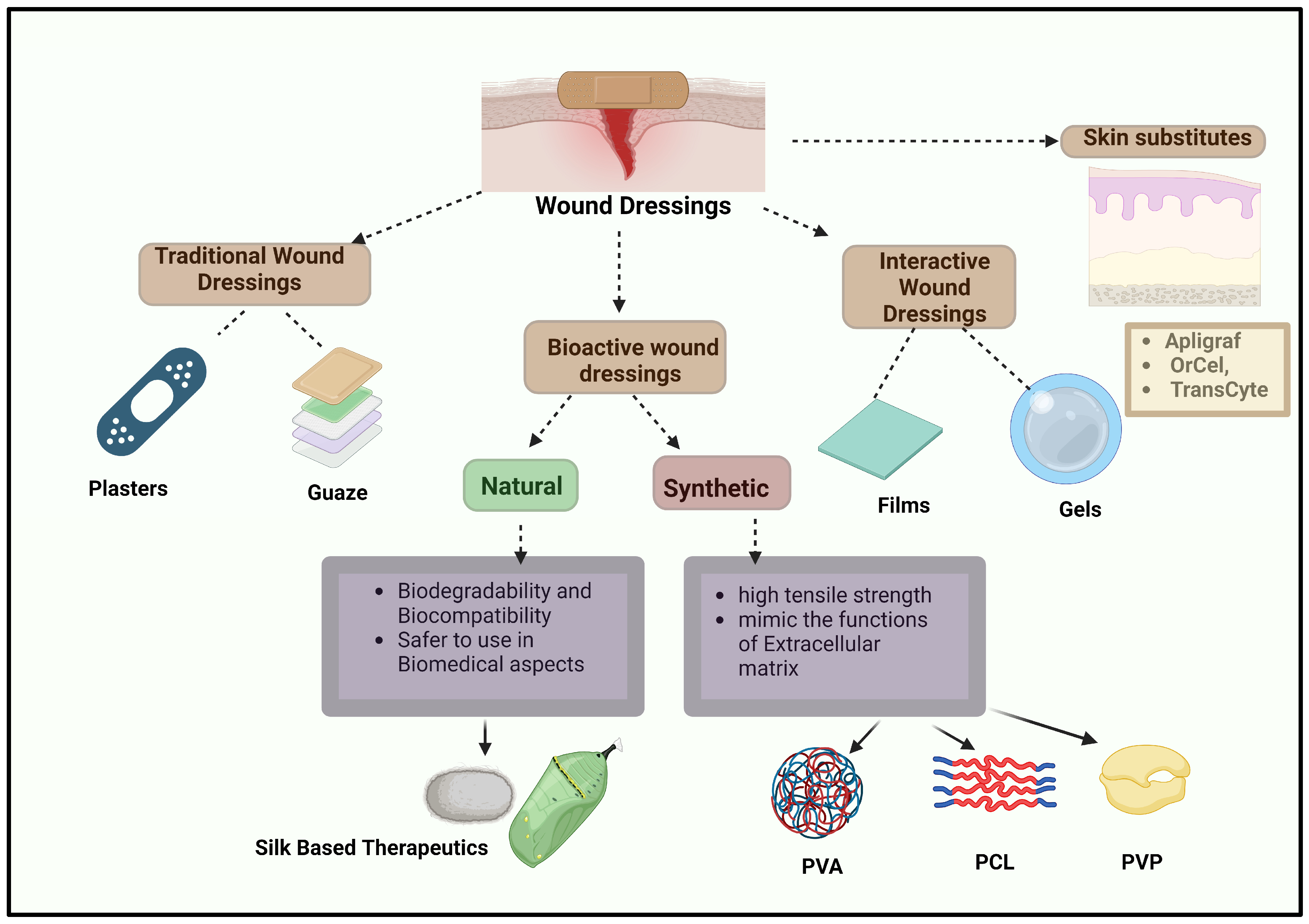
3. Role of Bioactive Wound Dressings and Its Types
4. Mechanical Properties and Biocompatibility in Wound Dressings
5. Polymeric Nanofibers Used in Wound Dressings
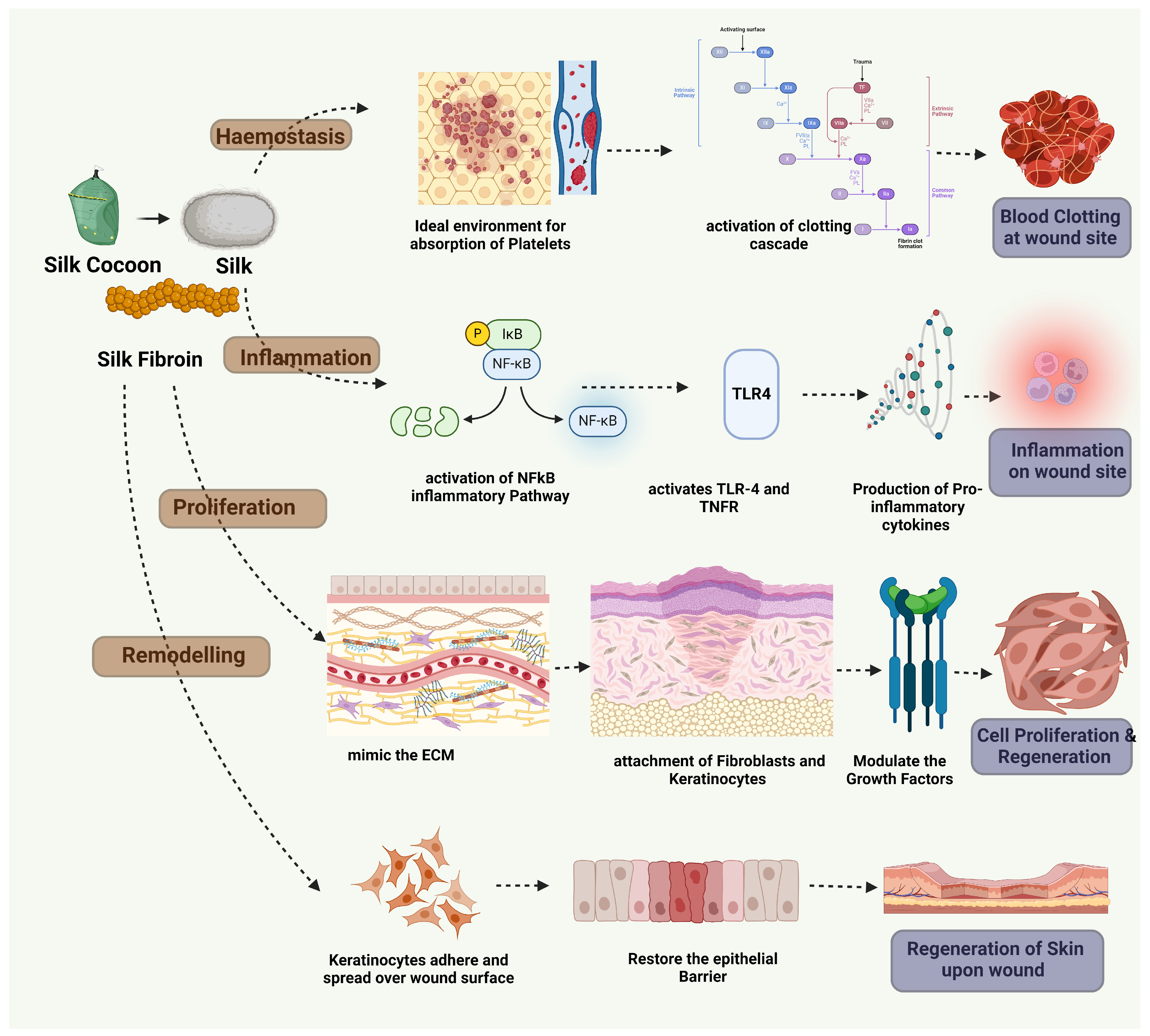
6. Silk Biomaterials and Silk Based Therapeutics in Diabetic Wound Healing
6.1. Silk Fibroin’s Structure and Properties
6.2. Wound Healing Mechanism of Silk Fibroin
7. Electrospinning—Fabrication Method of Silk Fibroin
7.1. Electrospinning
7.2. Types of Electrospinning
7.3. Mechanism of Wound Healing by Electrospun Fibers in the Various Phases of Wound Healing
7.4. Electrospun Silk Based Scaffolds from Bench to Bed Side
8. Conclusions and Future Perspectives
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| DM | Diabetes Mellitus |
| VEGF | Vascular Endothelial Growth Factor |
| TGF | Transforming Growth Factor |
| IL-4 | Interleukin-4 |
| IL-13 | Interleukin-13 |
| TNF | Tumor Necrosis Factor |
| FGF | Fibroblast Growth Factor |
| PLA | Polylactic Acid |
| PCL | Polycaprolactone |
| PLGA | Poly(lactic-co-glycolic acid) |
| PVA | Polyvinyl Alcohol |
| ECM | Extracellular Matrix |
| SF | Silk Fibroin |
| NFkB | Nuclear Factor-kappa B |
| ROS | Reactive Oxygen Species |
| TLR | Toll-Like Receptor |
| TNFR | Tumor Necrosis Factor Receptor |
| MAPK | Mitogen-Activated Protein Kinase |
| AKT | Protein Kinase B |
| IL-10 | Interleukin-10 |
| FGF | Fibroblast Growth Factor |
| IGF | Insulin Like Growth Factor |
| KGF | Keratinocyte Growth Factor |
| HGF | Hepatocyte Growth Factor |
References
- American Diabetes Association. Diagnosis and Classification of Diabetes Mellitus. Diabetes Care 2009, 32, S62–S67. [Google Scholar] [CrossRef] [PubMed]
- Burgess, J.L.; Wyant, W.A.; Abdo Abujamra, B.; Kirsner, R.S.; Jozic, I. Diabetic Wound-Healing Science. Medicina 2021, 57, 1072. [Google Scholar] [CrossRef]
- Frykberg, R.G.; Banks, J. Challenges in the Treatment of Chronic Wounds. Adv. Wound Care 2015, 4, 560–582. [Google Scholar] [CrossRef]
- Dasari, N.; Jiang, A.; Skochdopole, A.; Chung, J.; Reece, E.M.; Vorstenbosch, J.; Winocour, S. Updates in Diabetic Wound Healing, Inflammation, and Scarring. Semin. Plast. Surg. 2021, 35, 153–158. [Google Scholar] [CrossRef] [PubMed]
- Saeedi, P.; Petersohn, I.; Salpea, P.; Malanda, B.; Karuranga, S.; Unwin, N.; Colagiuri, S.; Guariguata, L.; Motala, A.A.; Ogurtsova, K.; et al. Global and Regional Diabetes Prevalence Estimates for 2019 and Projections for 2030 and 2045: Results from the International Diabetes Federation Diabetes Atlas, 9th Edition. Diabetes Res. Clin. Pract. 2019, 157, 107843. [Google Scholar] [CrossRef] [PubMed]
- Järbrink, K.; Ni, G.; Sönnergren, H.; Schmidtchen, A.; Pang, C.; Bajpai, R.; Car, J. The Humanistic and Economic Burden of Chronic Wounds: A Protocol for a Systematic Review. Syst. Rev. 2017, 6, 15. [Google Scholar] [CrossRef] [PubMed]
- Sharma, A.; Shankar, R.; Yadav, A.K.; Pratap, A.; Ansari, M.A.; Srivastava, V. Burden of Chronic Nonhealing Wounds: An Overview of the Worldwide Humanistic and Economic Burden to the Healthcare System. Int. J. Low Extrem. Wounds 2024. [Google Scholar] [CrossRef] [PubMed]
- Shi, C.; Wang, C.; Liu, H.; Li, Q.; Li, R.; Zhang, Y.; Liu, Y.; Shao, Y.; Wang, J. Selection of Appropriate Wound Dressing for Various Wounds. Front. Bioeng. Biotechnol. 2020, 8, 182. [Google Scholar] [CrossRef]
- Al-Abduljabbar, A.; Farooq, I. Electrospun Polymer Nanofibers: Processing, Properties, and Applications. Polymers 2022, 15, 65. [Google Scholar] [CrossRef]
- Yang, L.; Wang, X.; Xiong, M.; Liu, X.; Luo, S.; Luo, J.; Wang, Y. Electrospun Silk Fibroin/Fibrin Vascular Scaffold with Superior Mechanical Properties and Biocompatibility for Applications in Tissue Engineering. Sci. Rep. 2024, 14, 3942. [Google Scholar] [CrossRef] [PubMed]
- Moazzami Goudarzi, Z.; Zaszczyńska, A.; Kowalczyk, T.; Sajkiewicz, P. Electrospun Antimicrobial Drug Delivery Systems and Hydrogels Used for Wound Dressings. Pharmaceutics 2024, 16, 93. [Google Scholar] [CrossRef]
- Wilkinson, H.N.; Hardman, M.J. Wound Healing: Cellular Mechanisms and Pathological Outcomes. Open Biol. 2020, 10, 200223. [Google Scholar] [CrossRef] [PubMed]
- Choudhary, V.; Choudhary, M.; Bollag, W.B. Exploring Skin Wound Healing Models and the Impact of Natural Lipids on the Healing Process. Int. J. Mol. Sci. 2024, 25, 3790. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez, A.C.D.O.; Costa, T.F.; de Araújo Andrade, Z.; Medrado, A.R.A.P. Wound Healing—A Literature Review. Bras. Dermatol. 2016, 91, 614–620. [Google Scholar] [CrossRef] [PubMed]
- Tamilarasi, G.P.; Krishnan, M.; Sabarees, G.; Gouthaman, S.; Alagarsamy, V.; Solomon, V.R. Emerging Trends in Curcumin Embedded Electrospun Nanofibers for Impaired Diabetic Wound Healing. Appl. Nano 2022, 3, 202–232. [Google Scholar] [CrossRef]
- Fernández-Guarino, M.; Hernández-Bule, M.L.; Bacci, S. Cellular and Molecular Processes in Wound Healing. Biomedicines 2023, 11, 2526. [Google Scholar] [CrossRef]
- Cade, W.T. Diabetes-Related Microvascular and Macrovascular Diseases in the Physical Therapy Setting. Phys. Ther. 2008, 88, 1322–1335. [Google Scholar] [CrossRef]
- Mieczkowski, M.; Mrozikiewicz-Rakowska, B.; Kowara, M.; Kleibert, M.; Czupryniak, L. The Problem of Wound Healing in Diabetes—From Molecular Pathways to the Design of an Animal Model. Int. J. Mol. Sci. 2022, 23, 7930. [Google Scholar] [CrossRef] [PubMed]
- Maheshwari, P.; Nirenjen, S.; Bergin, R.V.B.; Pavithradevi, M.; Arun, S.; Shanmugasundaram, P. Improvement of Patient Compliance through Patient Counselling in Patients with Diabetic Foot Ulcer. Res. J. Pharm. Technol. 2018, 11, 2248. [Google Scholar] [CrossRef]
- Mansour, A.; Mousa, M.; Abdelmannan, D.; Tay, G.; Hassoun, A.; Alsafar, H. Microvascular and Macrovascular Complications of Type 2 Diabetes Mellitus: Exome Wide Association Analyses. Front. Endocrinol. 2023, 14, 1143067. [Google Scholar] [CrossRef] [PubMed]
- Lauri, C.; Leone, A.; Cavallini, M.; Signore, A.; Giurato, L.; Uccioli, L. Diabetic Foot Infections: The Diagnostic Challenges. J. Clin. Med. 2020, 9, 1779. [Google Scholar] [CrossRef]
- Eisenbud, D.E. Oxygen in Wound Healing. Clin. Plast. Surg. 2012, 39, 293–310. [Google Scholar] [CrossRef] [PubMed]
- Guan, Y.; Niu, H.; Liu, Z.; Dang, Y.; Shen, J.; Zayed, M.; Ma, L.; Guan, J. Sustained Oxygenation Accelerates Diabetic Wound Healing by Promoting Epithelialization and Angiogenesis and Decreasing Inflammation. Sci. Adv. 2021, 7, abj0153. [Google Scholar] [CrossRef] [PubMed]
- Berbudi, A.; Rahmadika, N.; Tjahjadi, A.I.; Ruslami, R. Type 2 Diabetes and Its Impact on the Immune System. Curr. Diabetes Rev. 2020, 16, 442–449. [Google Scholar] [CrossRef] [PubMed]
- Zheng, S.-Y.; Wan, X.-X.; Kambey, P.A.; Luo, Y.; Hu, X.-M.; Liu, Y.-F.; Shan, J.-Q.; Chen, Y.-W.; Xiong, K. Therapeutic Role of Growth Factors in Treating Diabetic Wound. World J. Diabetes 2023, 14, 364–395. [Google Scholar] [CrossRef]
- Nirenjen, S.; Narayanan, J.; Tamilanban, T.; Subramaniyan, V.; Chitra, V.; Fuloria, N.K.; Wong, L.S.; Ramachawolran, G.; Sekar, M.; Gupta, G.; et al. Exploring the Contribution of Pro-Inflammatory Cytokines to Impaired Wound Healing in Diabetes. Front. Immunol. 2023, 14, 1216321. [Google Scholar] [CrossRef]
- Sood, A.; Granick, M.S.; Tomaselli, N.L. Wound Dressings and Comparative Effectiveness Data. Adv. Wound Care 2014, 3, 511–529. [Google Scholar] [CrossRef] [PubMed]
- Su, L.; Jia, Y.; Fu, L.; Guo, K.; Xie, S. The Emerging Progress on Wound Dressings and Their Application in Clinic Wound Management. Heliyon 2023, 9, e22520. [Google Scholar] [CrossRef] [PubMed]
- Alven, S.; Peter, S.; Mbese, Z.; Aderibigbe, B.A. Polymer-Based Wound Dressing Materials Loaded with Bioactive Agents: Potential Materials for the Treatment of Diabetic Wounds. Polymers 2022, 14, 724. [Google Scholar] [CrossRef]
- Urciuolo, F.; Casale, C.; Imparato, G.; Netti, P.A. Bioengineered Skin Substitutes: The Role of Extracellular Matrix and Vascularization in the Healing of Deep Wounds. J. Clin. Med. 2019, 8, 2083. [Google Scholar] [CrossRef] [PubMed]
- Oualla-Bachiri, W.; Fernández-González, A.; Quiñones-Vico, M.I.; Arias-Santiago, S. From Grafts to Human Bioengineered Vascularized Skin Substitutes. Int. J. Mol. Sci. 2020, 21, 8197. [Google Scholar] [CrossRef] [PubMed]
- Polverino, G.; Russo, F.; D’Andrea, F. Bioactive Dressing: A New Algorithm in Wound Healing. J. Clin. Med. 2024, 13, 2488. [Google Scholar] [CrossRef]
- Jiang, Z.; Zheng, Z.; Yu, S.; Gao, Y.; Ma, J.; Huang, L.; Yang, L. Nanofiber Scaffolds as Drug Delivery Systems Promoting Wound Healing. Pharmaceutics 2023, 15, 1829. [Google Scholar] [CrossRef]
- Yasin, S.N.N.; Said, Z.; Halib, N.; Rahman, Z.A.; Mokhzani, N.I. Polymer-Based Hydrogel Loaded with Honey in Drug Delivery System for Wound Healing Applications. Polymers 2023, 15, 3085. [Google Scholar] [CrossRef] [PubMed]
- Sethuram, L.; Thomas, J. Therapeutic Applications of Electrospun Nanofibers Impregnated with Various Biological Macromolecules for Effective Wound Healing Strategy—A Review. Biomed. Pharmacother. 2023, 157, 113996. [Google Scholar] [CrossRef]
- Liu, Y.; Li, C.; Feng, Z.; Han, B.; Yu, D.-G.; Wang, K. Advances in the Preparation of Nanofiber Dressings by Electrospinning for Promoting Diabetic Wound Healing. Biomolecules 2022, 12, 1727. [Google Scholar] [CrossRef] [PubMed]
- Shalaby, M.A.; Anwar, M.M.; Saeed, H. Nanomaterials for Application in Wound Healing: Current State-of-the-Art and Future Perspectives. J. Polym. Res. 2022, 29, 91. [Google Scholar] [CrossRef]
- Zhang, H.; Lin, X.; Cao, X.; Wang, Y.; Wang, J.; Zhao, Y. Developing Natural Polymers for Skin Wound Healing. Bioact. Mater. 2024, 33, 355–376. [Google Scholar] [CrossRef] [PubMed]
- Sell, S.A.; Wolfe, P.S.; Garg, K.; McCool, J.M.; Rodriguez, I.A.; Bowlin, G.L. The Use of Natural Polymers in Tissue Engineering: A Focus on Electrospun Extracellular Matrix Analogues. Polymers 2010, 2, 522–553. [Google Scholar] [CrossRef]
- Oliveira, C.; Sousa, D.; Teixeira, J.A.; Ferreira-Santos, P.; Botelho, C.M. Polymeric Biomaterials for Wound Healing. Front. Bioeng. Biotechnol. 2023, 11, 1136077. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Y.; Qiu, Y.; Wang, H.; Chen, Y.; Jin, S.; Chen, S. Preparation of Nanofibers with Renewable Polymers and Their Application in Wound Dressing. Int. J. Polym. Sci. 2016, 2016, 4672839. [Google Scholar] [CrossRef]
- Satchanska, G.; Davidova, S.; Petrov, P.D. Natural and Synthetic Polymers for Biomedical and Environmental Applications. Polymers 2024, 16, 1159. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Xu, H.; Zhang, M.; Yu, D.-G. Electrospun Medicated Nanofibers for Wound Healing: Review. Membranes 2021, 11, 770. [Google Scholar] [CrossRef] [PubMed]
- Masood, N.; Ahmed, R.; Tariq, M.; Ahmed, Z.; Masoud, M.S.; Ali, I.; Asghar, R.; Andleeb, A.; Hasan, A. Silver Nanoparticle Impregnated Chitosan-PEG Hydrogel Enhances Wound Healing in Diabetes Induced Rabbits. Int. J. Pharm. 2019, 559, 23–36. [Google Scholar] [CrossRef] [PubMed]
- Wu, C.; Long, L.; Zhang, Y.; Xu, Y.; Lu, Y.; Yang, Z.; Guo, Y.; Zhang, J.; Hu, X.; Wang, Y. Injectable Conductive and Angiogenic Hydrogels for Chronic Diabetic Wound Treatment. J. Control. Release 2022, 344, 249–260. [Google Scholar] [CrossRef] [PubMed]
- Xu, Z.; Liu, Y.; Ma, R.; Chen, J.; Qiu, J.; Du, S.; Li, C.; Wu, Z.; Yang, X.; Chen, Z.; et al. Thermosensitive Hydrogel Incorporating Prussian Blue Nanoparticles Promotes Diabetic Wound Healing via ROS Scavenging and Mitochondrial Function Restoration. ACS Appl. Mater. Interfaces 2022, 14, 14059–14071. [Google Scholar] [CrossRef] [PubMed]
- Jiang, Y.; Han, Y.; Wang, J.; Lv, F.; Yi, Z.; Ke, Q.; Xu, H. Space-Oriented Nanofibrous Scaffold with Silicon-Doped Amorphous Calcium Phosphate Nanocoating for Diabetic Wound Healing. ACS Appl. Bio Mater. 2019, 2, 787–795. [Google Scholar] [CrossRef] [PubMed]
- Cam, M.E.; Ertas, B.; Alenezi, H.; Hazar-Yavuz, A.N.; Cesur, S.; Ozcan, G.S.; Ekentok, C.; Guler, E.; Katsakouli, C.; Demirbas, Z.; et al. Accelerated Diabetic Wound Healing by Topical Application of Combination Oral Antidiabetic Agents-Loaded Nanofibrous Scaffolds: An in Vitro and in Vivo Evaluation Study. Mater. Sci. Eng. C 2021, 119, 111586. [Google Scholar] [CrossRef]
- Ali, I.H.; Khalil, I.A.; El-Sherbiny, I.M. Design, Development, in-Vitro and in-Vivo Evaluation of Polylactic Acid-Based Multifunctional Nanofibrous Patches for Efficient Healing of Diabetic Wounds. Sci. Rep. 2023, 13, 3215. [Google Scholar] [CrossRef]
- Di Cristo, F.; Valentino, A.; De Luca, I.; Peluso, G.; Bonadies, I.; Di Salle, A.; Calarco, A. Polylactic Acid/Poly(Vinylpyrrolidone) Co-Electrospun Fibrous Membrane as a Tunable Quercetin Delivery Platform for Diabetic Wounds. Pharmaceutics 2023, 15, 805. [Google Scholar] [CrossRef]
- Zheng, Z.; Liu, Y.; Huang, W.; Mo, Y.; Lan, Y.; Guo, R.; Cheng, B. Neurotensin-Loaded PLGA/CNC Composite Nanofiber Membranes Accelerate Diabetic Wound Healing. Artif. Cells Nanomed. Biotechnol. 2018, 46, 493–501. [Google Scholar] [CrossRef]
- Hasan, N.; Cao, J.; Lee, J.; Naeem, M.; Hlaing, S.P.; Kim, J.; Jung, Y.; Lee, B.-L.; Yoo, J.-W. PEI/NONOates-Doped PLGA Nanoparticles for Eradicating Methicillin-Resistant Staphylococcus aureus Biofilm in Diabetic Wounds via Binding to the Biofilm Matrix. Mater. Sci. Eng. C 2019, 103, 109741. [Google Scholar] [CrossRef]
- Lv, H.; Zhao, M.; Li, Y.; Li, K.; Chen, S.; Zhao, W.; Wu, S.; Han, Y. Electrospun Chitosan–Polyvinyl Alcohol Nanofiber Dressings Loaded with Bioactive Ursolic Acid Promoting Diabetic Wound Healing. Nanomaterials 2022, 12, 2933. [Google Scholar] [CrossRef]
- Ningrum, D.R.; Hanif, W.; Mardhian, D.F.; Asri, L.A.T.W. In Vitro Biocompatibility of Hydrogel Polyvinyl Alcohol/Moringa Oleifera Leaf Extract/Graphene Oxide for Wound Dressing. Polymers 2023, 15, 468. [Google Scholar] [CrossRef] [PubMed]
- Yu, J.; Wang, P.; Yin, M.; Zhang, K.; Wang, X.; Han, B. Carboxymethyl Chitosan-Grafted Polyvinylpyrrolidone-Iodine Microspheres for Promoting the Healing of Chronic Wounds. Bioengineered 2022, 13, 8735–8746. [Google Scholar] [CrossRef] [PubMed]
- Makadia, H.K.; Siegel, S.J. Poly Lactic-Co-Glycolic Acid (PLGA) as Biodegradable Controlled Drug Delivery Carrier. Polymers 2011, 3, 1377–1397. [Google Scholar] [CrossRef]
- Liu, Y.; Zhou, S.; Gao, Y.; Zhai, Y. Electrospun Nanofibers as a Wound Dressing for Treating Diabetic Foot Ulcer. Asian J. Pharm. Sci. 2019, 14, 130–143. [Google Scholar] [CrossRef]
- Castro, V.O.; Fredel, M.C.; Aragones, Á.; de Oliveira Barra, G.M.; Cesca, K.; Merlini, C. Electrospun Fibrous Membranes of Poly (Lactic-Co-Glycolic Acid) with β-Tricalcium Phosphate for Guided Bone Regeneration Application. Polym. Test. 2020, 86, 106489. [Google Scholar] [CrossRef]
- Nofar, M.; Sacligil, D.; Carreau, P.J.; Kamal, M.R.; Heuzey, M.-C. Poly (Lactic Acid) Blends: Processing, Properties and Applications. Int. J. Biol. Macromol. 2019, 125, 307–360. [Google Scholar] [CrossRef] [PubMed]
- Capuana, E.; Lopresti, F.; Ceraulo, M.; La Carrubba, V. Poly-l-Lactic Acid (PLLA)-Based Biomaterials for Regenerative Medicine: A Review on Processing and Applications. Polymers 2022, 14, 1153. [Google Scholar] [CrossRef]
- Liu, C.; Du, G.; Guo, Q.; Li, R.; Li, C.; He, H. Fabrication and Characterization of Polylactic Acid Electrospun Wound Dressing Modified with Polyethylene Glycol, Rosmarinic Acid and Graphite Oxide. Nanomaterials 2023, 13, 2000. [Google Scholar] [CrossRef] [PubMed]
- Raina, N.; Pahwa, R.; Khosla, J.K.; Gupta, P.N.; Gupta, M. Polycaprolactone-Based Materials in Wound Healing Applications. Polym. Bull. 2022, 79, 7041–7063. [Google Scholar] [CrossRef]
- Song, R.; Murphy, M.; Li, C.; Ting, K.; Soo, C.; Zheng, Z. Current Development of Biodegradable Polymeric Materials for Biomedical Applications. Drug Des. Dev. Ther. 2018, 12, 3117–3145. [Google Scholar] [CrossRef]
- Murugan, D.; Suresh, A.; Thakur, G.; Singh, B.N. Fabrication and Evaluation of Poly(ε-Caprolactone) Based Nanofibrous Scaffolds Loaded with Homoeopathic Mother Tincture of Syzygium Cumini for Wound Healing Applications. OpenNano 2023, 14, 100189. [Google Scholar] [CrossRef]
- Zhong, Y.; Lin, Q.; Yu, H.; Shao, L.; Cui, X.; Pang, Q.; Zhu, Y.; Hou, R. Construction Methods and Biomedical Applications of PVA-Based Hydrogels. Front. Chem. 2024, 12, 1376799. [Google Scholar] [CrossRef]
- Costa-Júnior, E.S.; Barbosa-Stancioli, E.F.; Mansur, A.A.P.; Vasconcelos, W.L.; Mansur, H.S. Preparation and Characterization of Chitosan/Poly(Vinyl Alcohol) Chemically Crosslinked Blends for Biomedical Applications. Carbohydr. Polym. 2009, 76, 472–481. [Google Scholar] [CrossRef]
- Sabarees, G.; Velmurugan, V.; Tamilarasi, G.P.; Alagarsamy, V.; Raja Solomon, V. Recent Advances in Silver Nanoparticles Containing Nanofibers for Chronic Wound Management. Polymers 2022, 14, 3994. [Google Scholar] [CrossRef]
- Fatahian, R.; Mirjalili, M.; Khajavi, R.; Rahimi, M.K.; Nasirizadeh, N. Fabrication of Antibacterial and Hemostatic Electrospun PVA Nanofibers for Wound Healing. SN Appl. Sci. 2020, 2, 1288. [Google Scholar] [CrossRef]
- Baranwal, J.; Barse, B.; Fais, A.; Delogu, G.L.; Kumar, A. Biopolymer: A Sustainable Material for Food and Medical Applications. Polymers 2022, 14, 983. [Google Scholar] [CrossRef] [PubMed]
- Tuwalska, A.; Grabska-Zielińska, S.; Sionkowska, A. Chitosan/Silk Fibroin Materials for Biomedical Applications—A Review. Polymers 2022, 14, 1343. [Google Scholar] [CrossRef] [PubMed]
- Radulescu, D.-M.; Andronescu, E.; Vasile, O.R.; Ficai, A.; Vasile, B.S. Silk Fibroin-Based Scaffolds for Wound Healing Applications with Metal Oxide Nanoparticles. J. Drug Deliv. Sci. Technol. 2024, 96, 105689. [Google Scholar] [CrossRef]
- Vepari, C.; Kaplan, D.L. Silk as a Biomaterial. Prog. Polym. Sci. 2007, 32, 991–1007. [Google Scholar] [CrossRef] [PubMed]
- Fang, G.; Sapru, S.; Behera, S.; Yao, J.; Shao, Z.; Kundu, S.C.; Chen, X. Exploration of the Tight Structural–Mechanical Relationship in Mulberry and Non-Mulberry Silkworm Silks. J. Mater. Chem. B 2016, 4, 4337–4347. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, T.; Puchalla, N.; Schendzielorz, M.; Kramell, A.E. Degumming and Characterization of Bombyx Mori and Non-Mulberry Silks from Saturniidae Silkworms. Sci. Rep. 2023, 13, 19504. [Google Scholar] [CrossRef]
- Lewis, R.V. Spider Silk: Ancient Ideas for New Biomaterials. Chem. Rev. 2006, 106, 3762–3774. [Google Scholar] [CrossRef]
- Murugesh Babu, K. Silk from Silkworms and Spiders as High-Performance Fibers. In Structure and Properties of High-Performance Fibers; Elsevier: Amsterdam, The Netherlands, 2017; pp. 327–366. [Google Scholar]
- Römer, L.; Scheibel, T. The Elaborate Structure of Spider Silk: Structure and Function of a Natural High Performance Fiber. Prion 2008, 2, 154–161. [Google Scholar] [CrossRef] [PubMed]
- Kunz, R.I.; Brancalhão, R.M.C.; Ribeiro, L.d.F.C.; Natali, M.R.M. Silkworm Sericin: Properties and Biomedical Applications. BioMed Res. Int. 2016, 2016, 8175701. [Google Scholar] [CrossRef]
- Reizabal, A.; Costa, C.M.; Pérez-Álvarez, L.; Vilas-Vilela, J.L.; Lanceros-Méndez, S. Silk Fibroin as Sustainable Advanced Material: Material Properties and Characteristics, Processing, and Applications. Adv. Funct. Mater. 2023, 33, 202210764. [Google Scholar] [CrossRef]
- Vidya, M.; Rajagopal, S. Silk Fibroin: A Promising Tool for Wound Healing and Skin Regeneration. Int. J. Polym. Sci. 2021, 2021, 9069924. [Google Scholar] [CrossRef]
- Nguyen, T.P.; Nguyen, Q.V.; Nguyen, V.-H.; Le, T.-H.; Huynh, V.Q.N.; Vo, D.-V.N.; Trinh, Q.T.; Kim, S.Y.; Le, Q. Van Silk Fibroin-Based Biomaterials for Biomedical Applications: A Review. Polymers 2019, 11, 1933. [Google Scholar] [CrossRef] [PubMed]
- Yonesi, M.; Garcia-Nieto, M.; Guinea, G.V.; Panetsos, F.; Pérez-Rigueiro, J.; González-Nieto, D. Silk Fibroin: An Ancient Material for Repairing the Injured Nervous System. Pharmaceutics 2021, 13, 429. [Google Scholar] [CrossRef]
- Yao, X.; Zou, S.; Fan, S.; Niu, Q.; Zhang, Y. Bioinspired Silk Fibroin Materials: From Silk Building Blocks Extraction and Reconstruction to Advanced Biomedical Applications. Mater. Today Bio 2022, 16, 100381. [Google Scholar] [CrossRef] [PubMed]
- Qi, Y.; Wang, H.; Wei, K.; Yang, Y.; Zheng, R.-Y.; Kim, I.; Zhang, K.-Q. A Review of Structure Construction of Silk Fibroin Biomaterials from Single Structures to Multi-Level Structures. Int. J. Mol. Sci. 2017, 18, 237. [Google Scholar] [CrossRef] [PubMed]
- Wang, Q.; Schniepp, H.C. Nanofibrils as Building Blocks of Silk Fibers: Critical Review of the Experimental Evidence. JOM 2019, 71, 1248–1263. [Google Scholar] [CrossRef]
- Ling, S.; Chen, W.; Fan, Y.; Zheng, K.; Jin, K.; Yu, H.; Buehler, M.J.; Kaplan, D.L. Biopolymer Nanofibrils: Structure, Modeling, Preparation, and Applications. Prog. Polym. Sci. 2018, 85, 1–56. [Google Scholar] [CrossRef] [PubMed]
- Sashina, E.S.; Bochek, A.M.; Novoselov, N.P.; Kirichenko, D.A. Structure and Solubility of Natural Silk Fibroin. Russ. J. Appl. Chem. 2006, 79, 869–876. [Google Scholar] [CrossRef]
- Bandyopadhyay, A.; Chowdhury, S.K.; Dey, S.; Moses, J.C.; Mandal, B.B. Silk: A Promising Biomaterial Opening New Vistas Towards Affordable Healthcare Solutions. J. Indian Inst. Sci. 2019, 99, 445–487. [Google Scholar] [CrossRef]
- De Giorgio, G.; Matera, B.; Vurro, D.; Manfredi, E.; Galstyan, V.; Tarabella, G.; Ghezzi, B.; D’Angelo, P. Silk Fibroin Materials: Biomedical Applications and Perspectives. Bioengineering 2024, 11, 167. [Google Scholar] [CrossRef] [PubMed]
- Sun, W.; Gregory, D.A.; Tomeh, M.A.; Zhao, X. Silk Fibroin as a Functional Biomaterial for Tissue Engineering. Int. J. Mol. Sci. 2021, 22, 1499. [Google Scholar] [CrossRef]
- Deptuch, T.; Dams-Kozlowska, H. Silk Materials Functionalized via Genetic Engineering for Biomedical Applications. Materials 2017, 10, 1417. [Google Scholar] [CrossRef]
- Mazurek, Ł.; Szudzik, M.; Rybka, M.; Konop, M. Silk Fibroin Biomaterials and Their Beneficial Role in Skin Wound Healing. Biomolecules 2022, 12, 1852. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.-L.; Li, X.-W.; Xu, W.; Yu, Q.-Y.; Fang, S.-M. Advances of Regenerated and Functionalized Silk Biomaterials and Application in Skin Wound Healing. Int. J. Biol. Macromol. 2024, 254, 128024. [Google Scholar] [CrossRef]
- Lehmann, T.; Vaughn, A.E.; Seal, S.; Liechty, K.W.; Zgheib, C. Silk Fibroin-Based Therapeutics for Impaired Wound Healing. Pharmaceutics 2022, 14, 651. [Google Scholar] [CrossRef]
- Li, Y.-Y.; Ji, S.-F.; Fu, X.-B.; Jiang, Y.-F.; Sun, X.-Y. Biomaterial-Based Mechanical Regulation Facilitates Scarless Wound Healing with Functional Skin Appendage Regeneration. Mil. Med. Res. 2024, 11, 13. [Google Scholar] [CrossRef] [PubMed]
- Muncie, J.M.; Weaver, V.M. The Physical and Biochemical Properties of the Extracellular Matrix Regulate Cell Fate. Curr. Top. Dev. Biol. 2018, 130, 1–37. [Google Scholar] [PubMed]
- Chen, Z.; Du, C.; Liu, S.; Liu, J.; Yang, Y.; Dong, L.; Zhao, W.; Huang, W.; Lei, Y. Progress in Biomaterials Inspired by the Extracellular Matrix. Giant 2024, 19, 100323. [Google Scholar] [CrossRef]
- Kolimi, P.; Narala, S.; Nyavanandi, D.; Youssef, A.A.A.; Dudhipala, N. Innovative Treatment Strategies to Accelerate Wound Healing: Trajectory and Recent Advancements. Cells 2022, 11, 2439. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Wang, L.; Xu, C.; Cao, Y.; Liu, S.; Reis, R.L.; Kundu, S.C.; Yang, X.; Xiao, B.; Duan, L. Transparent Silk Fibroin Film-Facilitated Infected-Wound Healing through Antibacterial, Improved Fibroblast Adhesion and Immune Modulation. J. Mater. Chem. B 2024, 12, 475–488. [Google Scholar] [CrossRef] [PubMed]
- Park, Y.R.; Sultan, M.T.; Park, H.J.; Lee, J.M.; Ju, H.W.; Lee, O.J.; Lee, D.J.; Kaplan, D.L.; Park, C.H. NF-ΚB Signaling Is Key in the Wound Healing Processes of Silk Fibroin. Acta Biomater. 2018, 67, 183–195. [Google Scholar] [CrossRef] [PubMed]
- Barrientos, S.; Stojadinovic, O.; Golinko, M.S.; Brem, H.; Tomic-Canic, M. Growth Factors and Cytokines in Wound Healing. Wound Repair Regen. 2008, 16, 585–601. [Google Scholar] [CrossRef]
- Bao, P.; Kodra, A.; Tomic-Canic, M.; Golinko, M.S.; Ehrlich, H.P.; Brem, H. The Role of Vascular Endothelial Growth Factor in Wound Healing. J. Surg. Res. 2009, 153, 347–358. [Google Scholar] [CrossRef]
- Aykac, A.; Karanlik, B.; Sehirli, A.O. Protective Effect of Silk Fibroin in Burn Injury in Rat Model. Gene 2018, 641, 287–291. [Google Scholar] [CrossRef]
- Indrakumar, S.; Dash, T.K.; Mishra, V.; Tandon, B.; Chatterjee, K. Silk Fibroin and Its Nanocomposites for Wound Care: A Comprehensive Review. ACS Polym. Au 2024, 4, 168–188. [Google Scholar] [CrossRef]
- Sta Agueda, J.R.H.; Chen, Q.; Maalihan, R.D.; Ren, J.; da Silva, Í.G.M.; Dugos, N.P.; Caldona, E.B.; Advincula, R.C. 3D Printing of Biomedically Relevant Polymer Materials and Biocompatibility. MRS Commun. 2021, 11, 197–212. [Google Scholar] [CrossRef]
- Anusiya, G.; Jaiganesh, R. A Review on Fabrication Methods of Nanofibers and a Special Focus on Application of Cellulose Nanofibers. Carbohydr. Polym. Technol. Appl. 2022, 4, 100262. [Google Scholar] [CrossRef]
- Abdulhussain, R.; Adebisi, A.; Conway, B.R.; Asare-Addo, K. Electrospun Nanofibers: Exploring Process Parameters, Polymer Selection, and Recent Applications in Pharmaceuticals and Drug Delivery. J. Drug Deliv. Sci. Technol. 2023, 90, 105156. [Google Scholar] [CrossRef]
- Jiang, X.; Zeng, Y.-E.; Li, C.; Wang, K.; Yu, D.-G. Enhancing Diabetic Wound Healing: Advances in Electrospun Scaffolds from Pathogenesis to Therapeutic Applications. Front. Bioeng. Biotechnol. 2024, 12, 1354286. [Google Scholar] [CrossRef] [PubMed]
- Reneker, D.H.; Yarin, A.L.; Zussman, E.; Xu, H. Electrospinning of Nanofibers from Polymer Solutions and Melts. Adv. Appl. Mech. 2007, 41, 43–346. [Google Scholar]
- Nadaf, A.; Gupta, A.; Hasan, N.; Fauziya; Ahmad, S.; Kesharwani, P.; Ahmad, F.J. Recent Update on Electrospinning and Electrospun Nanofibers: Current Trends and Their Applications. RSC Adv. 2022, 12, 23808–23828. [Google Scholar] [CrossRef] [PubMed]
- Ahmadi Bonakdar, M.; Rodrigue, D. Electrospinning: Processes, Structures, and Materials. Macromol 2024, 4, 58–103. [Google Scholar] [CrossRef]
- Şener, A.G.; Altay, A.S.; Altay, F. Effect of Voltage on Morphology of Electrospun Nanofibers. In Proceedings of the 2011 7th International Conference on Electrical and Electronics Engineering (ELECO), Bursa, Turkey, 1–4 December 2011; pp. 324–328. [Google Scholar]
- Xue, J.; Wu, T.; Dai, Y.; Xia, Y. Electrospinning and Electrospun Nanofibers: Methods, Materials, and Applications. Chem. Rev. 2019, 119, 5298–5415. [Google Scholar] [CrossRef] [PubMed]
- Deitzel, J.M.; Kleinmeyer, J.; Harris, D.; Beck Tan, N.C. The Effect of Processing Variables on the Morphology of Electrospun Nanofibers and Textiles. Polymer 2001, 42, 261–272. [Google Scholar] [CrossRef]
- Keirouz, A.; Wang, Z.; Reddy, V.S.; Nagy, Z.K.; Vass, P.; Buzgo, M.; Ramakrishna, S.; Radacsi, N. The History of Electrospinning: Past, Present, and Future Developments. Adv. Mater. Technol. 2023, 8, 202201723. [Google Scholar] [CrossRef]
- Tucker, N.; Stanger, J.J.; Staiger, M.P.; Razzaq, H.; Hofman, K. The History of the Science and Technology of Electrospinning from 1600 to 1995. J. Eng. Fiber. Fabr. 2012, 7, 155892501200702. [Google Scholar] [CrossRef]
- Ghajarieh, A.; Habibi, S.; Talebian, A. Biomedical Applications of Nanofibers. Russ. J. Appl. Chem. 2021, 94, 847–872. [Google Scholar] [CrossRef]
- Azimi, B.; Maleki, H.; Zavagna, L.; De la Ossa, J.G.; Linari, S.; Lazzeri, A.; Danti, S. Bio-Based Electrospun Fibers for Wound Healing. J. Funct. Biomater. 2020, 11, 67. [Google Scholar] [CrossRef] [PubMed]
- Venmathi Maran, B.A.; Jeyachandran, S.; Kimura, M. A Review on the Electrospinning of Polymer Nanofibers and Its Biomedical Applications. J. Compos. Sci. 2024, 8, 32. [Google Scholar] [CrossRef]
- Muthukrishnan, L. An Overview on Electrospinning and Its Advancement toward Hard and Soft Tissue Engineering Applications. Colloid Polym. Sci. 2022, 300, 875–901. [Google Scholar] [CrossRef] [PubMed]
- Buzgo, M.; Mickova, A.; Rampichova, M.; Doupnik, M. Blend Electrospinning, Coaxial Electrospinning, and Emulsion Electrospinning Techniques. In Core-Shell Nanostructures for Drug Delivery and Theranostics; Elsevier: Amsterdam, The Netherlands, 2018; pp. 325–347. [Google Scholar]
- Qin, X. Coaxial Electrospinning of Nanofibers. In Electrospun Nanofibers; Elsevier: Amsterdam, The Netherlands, 2017; pp. 41–71. [Google Scholar]
- Abadi, B.; Goshtasbi, N.; Bolourian, S.; Tahsili, J.; Adeli-Sardou, M.; Forootanfar, H. Electrospun Hybrid Nanofibers: Fabrication, Characterization, and Biomedical Applications. Front. Bioeng. Biotechnol. 2022, 10, 986975. [Google Scholar] [CrossRef] [PubMed]
- Gupta, P.; Wilkes, G.L. Some Investigations on the Fiber Formation by Utilizing a Side-by-Side Bicomponent Electrospinning Approach. Polymer 2003, 44, 6353–6359. [Google Scholar] [CrossRef]
- Zhang, X.; Wang, Y.; Gao, Z.; Mao, X.; Cheng, J.; Huang, L.; Tang, J. Advances in Wound Dressing Based on Electrospinning Nanofibers. J. Appl. Polym. Sci. 2024, 141, 54746. [Google Scholar] [CrossRef]
- Opneja, A.; Kapoor, S.; Stavrou, E.X. Contribution of Platelets, the Coagulation and Fibrinolytic Systems to Cutaneous Wound Healing. Thromb. Res. 2019, 179, 56–63. [Google Scholar] [CrossRef] [PubMed]
- Rickel, A.P.; Deng, X.; Engebretson, D.; Hong, Z. Electrospun Nanofiber Scaffold for Vascular Tissue Engineering. Mater. Sci. Eng. C Mater. Biol. Appl. 2021, 129, 112373. [Google Scholar] [CrossRef]
- Nazarnezhad, S.; Baino, F.; Kim, H.-W.; Webster, T.J.; Kargozar, S. Electrospun Nanofibers for Improved Angiogenesis: Promises for Tissue Engineering Applications. Nanomaterials 2020, 10, 1609. [Google Scholar] [CrossRef]
- Karthikeyan, K.; Sekar, S.; Pandima Devi, M.; Inbasekaran, S.; Lakshminarasaiah, C.H.; Sastry, T.P. Fabrication of Novel Biofibers by Coating Silk Fibroin with Chitosan Impregnated with Silver Nanoparticles. J. Mater. Sci. Mater. Med. 2011, 22, 2721–2726. [Google Scholar] [CrossRef] [PubMed]
- Aznar-Cervantes, S.; Martínez, J.G.; Bernabeu-Esclapez, A.; Lozano-Pérez, A.A.; Meseguer-Olmo, L.; Otero, T.F.; Cenis, J.L. Fabrication of Electrospun Silk Fibroin Scaffolds Coated with Graphene Oxide and Reduced Graphene for Applications in Biomedicine. Bioelectrochemistry 2016, 108, 36–45. [Google Scholar] [CrossRef]
- Miguel, S.P.; Simões, D.; Moreira, A.F.; Sequeira, R.S.; Correia, I.J. Production and Characterization of Electrospun Silk Fibroin Based Asymmetric Membranes for Wound Dressing Applications. Int. J. Biol. Macromol. 2019, 121, 524–535. [Google Scholar] [CrossRef] [PubMed]
- Rama, M.; Vijayalakshmi, U. Influence of Silk Fibroin on the Preparation of Nanofibrous Scaffolds for the Effective Use in Osteoregenerative Applications. J. Drug Deliv. Sci. Technol. 2021, 61, 102182. [Google Scholar] [CrossRef]
- Jao, W.; Yang, M.; Lin, C.; Hsu, C. Fabrication and Characterization of Electrospun Silk Fibroin/TiO2 Nanofibrous Mats for Wound Dressings. Polym. Adv. Technol. 2012, 23, 1066–1076. [Google Scholar] [CrossRef]
- Khan, A.U.R.; Morsi, Y.; Zhu, T.; Ahmad, A.; Xie, X.; Yu, F.; Mo, X. Electrospinning: An Emerging Technology to Construct Polymer-Based Nanofibrous Scaffolds for Diabetic Wound Healing. Front. Mater. Sci. 2021, 15, 10–35. [Google Scholar] [CrossRef]
- Kubera Sampath Kumar, S.; Prakash, C.; Vaidheeswaran, S.; Karthic Kumar, B.; Subramanian, S. Design and Characterization of Secondary and Tertiary Layers of a Multilayer Wound Dressing System. J. Test. Eval. 2020, 48, 2683–2698. [Google Scholar] [CrossRef]

| S.No. | Growth Factors | Sources of Growth Factors | Function |
|---|---|---|---|
| 1. | EGF | Platelets and macrophages | Re-epithelialization; granulation tissue formation |
| 2. | PDGF | Platelets; keratinocytes; macrophages; endothelial cells; fibroblasts | Inflammation; granulation tissue formation/angiogenesis; re-epithelialization; matrix formation and remodeling |
| 3. | TGF-β | Platelets; keratinocytes; macrophages; lymphocytes; fibroblasts | Inflammation; granulation tissue formation; re-epithelialization; matrix formation and remodeling |
| 4. | TNF-α | Neutrophils; macrophages | collagen expression; re-epithelialization |
| 5. | VEGF | Platelets; neutrophils; macrophages; endothelial cells; smooth muscle cells; fibroblasts | granulation tissue formation/angiogenesis/neo-vascularization |
| 6. | FGF | Macrophages, fibroblasts, endothelial cells | Angiogenesis, granulation tissue formation, re-epithelialization, collagen synthesis |
| 7. | IGF | Platelets, macrophages, fibroblasts | Re-epithelialization, matrix formation and remodeling, cell migration |
| 8. | KGF | Fibroblasts | Stimulates keratinocyte proliferation and migration, re-epithelialization |
| 9. | HGF | Mesenchymal cells, fibroblasts | Promotes epithelial and endothelial cell proliferation, re-epithelialization, angiogenesis |
| S.No. | Synthetic Polymers | Formulation | Experimental Animals | Highlights |
|---|---|---|---|---|
| 1. | Polyethylene Glycol (PEG) | Chitosan crosslinked PEG Hydrogels loaded with silver nanoparticles | Rabbits | High porosity and improved antioxidant property and antimicrobial property. Boosted wound healing in experimental animals [44] |
| Quaternized chitosan Combined PEG-CHO hydrogels | Rats | Good mechanical properties and Biocompatibilty, and improved angiogenesis and accelerated the process of wound healing in experimental animals [45] | ||
| PEG-PDLLA Hydrogels | Mice | Enhanced angiogenesis and decreases the ROS, IL-6 and TNF. Promotes the healing of wounds [46] | ||
| 2. | Polycaprolactone (PCL) | Composite PCL/electrospun nanocoated scaffolds with ACP and Si | Diabetic mice | Better mechanical stability, enhanced wound healing of full thickness wound by stimulating angiogenesis, collagen deposition and re-epithelialization [47] |
| Composite nanofibrous scaffolds made of chitosan, gelatin, PCL, PVP | Diabetic rats | Cytocompatibility with respect to L929 cells. Accelerated the wound healing process by improving the collagen synthesis, lowering the inflammatory cytokines TNF, IL-6, IL-1 and NFkB [48] | ||
| 3. | Polylactic acid (PLA) | Multilayered nanofibrous PLA patches | Diabetic rats | Better wound healing activity by adequate fibroblasts proliferation, angiogenesis and resulting in a healing of full thickness wound [49] |
| Electrospun fibers made of PLA and PVP | Diabetic mice | Possesses anti-inflammatory and antibacterial activity prompting wound healing process [50] | ||
| 4. | Poly(lactic-co-glycolic acid) (PLGA) | Composite PLGA/CNC nanofiber | Diabetic mice | Better cytocompatibility by fibroblast adhesion and accelerated full thickness wound healing decreasing the expression of IL-6 and IL-1B [51] |
| PLGA incorporated nanoparticles | Diabetic mice | Very beneficial against MRSA diabetic wounds possess better wound healing efficiency [52] | ||
| 5. | Polyvinyl alcohol (PVA) | PVA incorporated nanofibers | Diabetic mice | Accelerated closure of full-thickness
|
| PVA/GO hydrogels | Fibroblast cell lines | Good cytocompatibility and antibacterial activity and promote better wound healing activity [54] | ||
| 6. | Polyvinyl pyrrolidone (PVP) | Composite nanofibrous scaffolds made of chitosan, gelatin and PVP | Diabetic rats | High tensile strength, accelerated wound healing by improving the collagen remodelling by decreasing the levels of TNF, IL-6 and NFKB [55] |
| PVP-grafted microspheres | Diabetic mice | Antibacterial and accelerated wound healing activity in experimental animal [55] |
| S.No. | Methods | Advantages | Disadvantages |
|---|---|---|---|
| 1. | Electrospinning |
|
|
| 2. | Freeze Drying |
|
|
| 3. | Solvent Casting |
|
|
| 4. | Hydrogel Formation |
|
|
| 5. | Lyophilization |
|
|
| 6. | 3D Printing |
|
|
| Comparison | Extracellular Matrix (ECM) | Electrospun Scaffolds |
|---|---|---|
| Components | Comprised of a dynamic 3D network of polysaccharides and natural polymers (collagen, elastin, fibrinogen, etc.) | Primarily made from synthetic and natural polymers |
| Structure | Consists mainly of fibers with diameters between 50 and 500 nm | Nanofibers typically range from 10 µm to 500 nm in diameter, produced via electrospinning |
| Role in Wound Healing |
|
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Aldahish, A.; Shanmugasundaram, N.; Vasudevan, R.; Alqahtani, T.; Alqahtani, S.; Mohammad Asiri, A.; Devanandan, P.; Thamaraikani, T.; Vellapandian, C.; Jayasankar, N. Silk Fibroin Nanofibers: Advancements in Bioactive Dressings through Electrospinning Technology for Diabetic Wound Healing. Pharmaceuticals 2024, 17, 1305. https://doi.org/10.3390/ph17101305
Aldahish A, Shanmugasundaram N, Vasudevan R, Alqahtani T, Alqahtani S, Mohammad Asiri A, Devanandan P, Thamaraikani T, Vellapandian C, Jayasankar N. Silk Fibroin Nanofibers: Advancements in Bioactive Dressings through Electrospinning Technology for Diabetic Wound Healing. Pharmaceuticals. 2024; 17(10):1305. https://doi.org/10.3390/ph17101305
Chicago/Turabian StyleAldahish, Afaf, Nirenjen Shanmugasundaram, Rajalakshimi Vasudevan, Taha Alqahtani, Saud Alqahtani, Ahmad Mohammad Asiri, Praveen Devanandan, Tamilanban Thamaraikani, Chitra Vellapandian, and Narayanan Jayasankar. 2024. "Silk Fibroin Nanofibers: Advancements in Bioactive Dressings through Electrospinning Technology for Diabetic Wound Healing" Pharmaceuticals 17, no. 10: 1305. https://doi.org/10.3390/ph17101305
APA StyleAldahish, A., Shanmugasundaram, N., Vasudevan, R., Alqahtani, T., Alqahtani, S., Mohammad Asiri, A., Devanandan, P., Thamaraikani, T., Vellapandian, C., & Jayasankar, N. (2024). Silk Fibroin Nanofibers: Advancements in Bioactive Dressings through Electrospinning Technology for Diabetic Wound Healing. Pharmaceuticals, 17(10), 1305. https://doi.org/10.3390/ph17101305









