Inflammation in Coronary Atherosclerosis: Insights into Pathogenesis and Therapeutic Potential of Anti-Inflammatory Drugs
Abstract
:1. Introduction
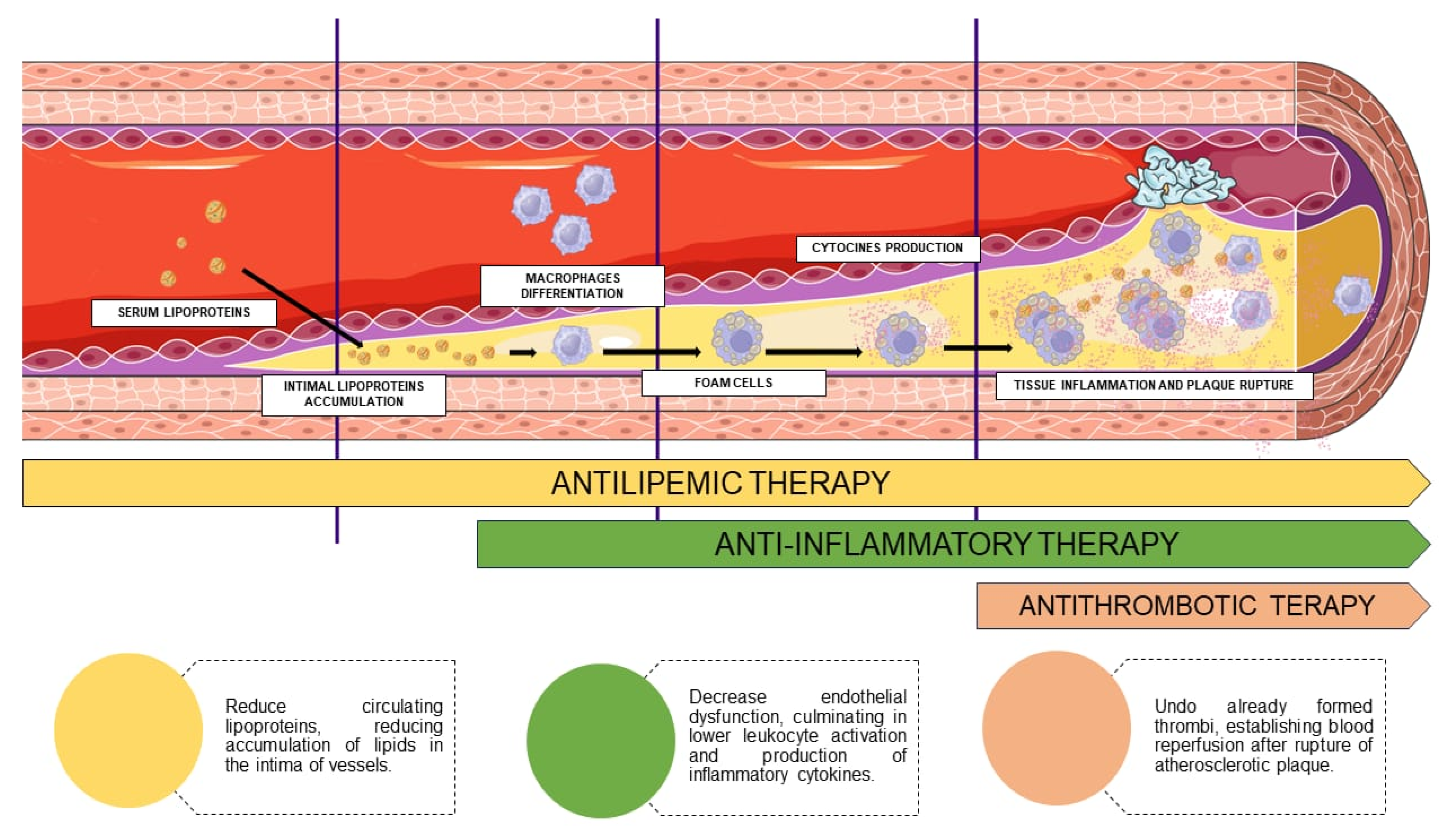
2. Atherosclerosis and Inflammation
3. Anti-Inflammatory Therapy for Coronary Artery Disease
4. Relevant Clinical Trials That Have Used Colchicine in CAD
5. Relevant Clinical Trials That Have Used Other Anti-Inflammatories Drugs in CAD
6. Relevant Clinical Trials That Have Used Non-Traditional Therapies with Anti-Inflammatories Properties in CAD
7. Future Perspectives
8. Conclusions
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hansson, G.K. Inflammation, Atherosclerosis, and Coronary Artery Disease. N. Engl. J. Med. 2005, 352, 1685–1695. Available online: www.nejm.org (accessed on 15 November 2022). [CrossRef] [PubMed]
- Arbab-Zadeh, A.; Nakano, M.; Virmani, R.; Fuster, V. Acute coronary events. Circulation 2012, 125, 1147–1156. [Google Scholar] [CrossRef] [PubMed]
- Ruparelia, N.; Choudhury, R. Inflammation and atherosclerosis: What is on the horizon? Heart 2020, 106, 80–85. [Google Scholar] [CrossRef]
- Falk, E.; Nakano, M.; Bentzon, J.F.; Finn, A.V.; Virmani, R. Update on acute coronary syndromes: The pathologists’ view. Eur. Heart J. 2013, 34, 719–728. [Google Scholar] [CrossRef] [PubMed]
- Lawler, P.R.; Bhatt, D.L.; Godoy, L.C.; Lüscher, T.F.; Bonow, R.O.; Verma, S.; Ridker, P.M. Targeting cardiovascular inflammation: Next steps in clinical translation. Eur. Heart J. 2021, 42, 113–131. [Google Scholar] [CrossRef] [PubMed]
- Spagnoli, L.G.; Bonanno, E.; Sangiorgi, G.; Mauriello, A. Role of Inflammation in Atherosclerosis. J. Nucl. Med. 2007, 48, 1800–1815. [Google Scholar] [CrossRef] [PubMed]
- Engelen, S.E.; Robinson, A.J.B.; Zurke, Y.X.; Monaco, C. Therapeutic strategies targeting inflammation and immunity in atherosclerosis: How to proceed? Nat. Rev. Cardiol. 2022, 19, 522–542. [Google Scholar] [CrossRef]
- Tucker, B.; Ephraums, J.; King, T.W.; Abburi, K.; Rye, K.-A.; Cochran, B.J. Impact of Impaired Cholesterol Homeostasis on Neutrophils in Atherosclerosis. Arter. Thromb. Vasc. Biol. 2023, 43, 618–627. [Google Scholar] [CrossRef]
- Soehnlein, O.; Libby, P. Targeting inflammation in atherosclerosis—From experimental insights to the clinic. Nat. Rev. Drug Discov. 2021, 20, 589–610. [Google Scholar] [CrossRef]
- Koenig, W. Persistent inflammatory residual risk despite aggressive cholesterol-lowering therapy: Further evidence fuelling the dual target concept. Eur. Heart J. 2020, 41, 2962–2964. [Google Scholar] [CrossRef]
- Ridker, P.M.; Cushman, M.; Stampfer, M.J.; Tracy, R.P.; Hennekens, C.H. Inflammation, Aspirin, and the Risk of Cardiovascular Disease in Apparently Healthy Men. N. Engl. J. Med. 1997, 336, 973–979. [Google Scholar] [CrossRef] [PubMed]
- Libby, P.; Ridker, P.M.; Hansson, G.K. Inflammation in Atherosclerosis. From Pathophysiology to Practice. J. Am. Coll. Cardiol. 2009, 54, 2129–2138. [Google Scholar] [CrossRef] [PubMed]
- Ridker, P.M.; Bhatt, D.L.; Pradhan, A.D.; Glynn, R.J.; MacFadyen, J.G.; Nissen, S.E. Inflammation and cholesterol as predictors of cardiovascular events among patients receiving statin therapy: A collaborative analysis of three randomised trials. Lancet 2023, 401, 1293–1301. [Google Scholar] [CrossRef] [PubMed]
- Visseren, F.L.; Mach, F.; Smulders, Y.M.; Carballo, D.; Koskinas, K.C.; Bäck, M.; Benetos, A.; Biffi, A.; Boavida, J.-M.; Capodanno, D.; et al. 2021 ESC Guidelines on cardiovascular disease prevention in clinical practice. Eur. Heart J. 2021, 42, 3227–3337. [Google Scholar] [CrossRef] [PubMed]
- Virani, S.S.; Newby, L.K.; Arnold, S.V.; Bittner, V.; Brewer, L.C.; Demeter, S.H.; Dixon, D.L.; Fearon, W.F.; Hess, B.; Johnson, H.M.; et al. 2023 AHA/ACC/ACCP/ASPC/NLA/PCNA Guideline for the Management of Patients with Chronic Coronary Disease: A Report of the American Heart Association/American College of Cardiology Joint Committee on Clinical Practice Guidelines. Circulation 2023. Available online: https://www.ahajournals.org/doi/10.1161/CIR.0000000000001168 (accessed on 30 July 2023). [CrossRef] [PubMed]
- Alomair, B.M.; Al-Kuraishy, H.M.; Al-Gareeb, A.I.; Al-Hamash, S.M.; De Waard, M.; Sabatier, J.-M.; Saad, H.M.; Batiha, G.E.-S. Montelukast and Acute Coronary Syndrome: The Endowed Drug. Pharmaceuticals 2022, 15, 1147. [Google Scholar] [CrossRef] [PubMed]
- Hoxha, M.; Lewis-Mikhael, A.-M.; Bueno-Cavanillas, A. Potential role of leukotriene receptor antagonists in reducing cardiovascular and cerbrovascular risk: A systematic review of human clinical trials and in vivo animal studies. Biomed. Pharmacother. 2018, 106, 956–965. [Google Scholar] [CrossRef]
- Tardif, J.C.; Kouz, S.; Waters, D.D.; Bertrand, O.F.; Diaz, R.; Maggioni, A.P.; Pinto, F.J.; Ibrahim, R.; Gamra, H.; Kiwan, G.S.; et al. Efficacy and Safety of Low-Dose Colchicine after Myocardial Infarction. N. Engl. J. Med. 2019, 381, 2497–2505. [Google Scholar] [CrossRef]
- Ridker, P.M.; Everett, B.M.; Thuren, T.; MacFadyen, J.G.; Chang, W.H.; Ballantyne, C.; Fonseca, F.; Nicolau, J.; Koenig, W.; Anker, S.D.; et al. Antiinflammatory Therapy with Canakinumab for Atherosclerotic Disease. N. Engl. J. Med. 2017, 377, 1119–1131. [Google Scholar] [CrossRef]
- Niu, Y.; Bai, N.; Ma, Y.; Zhong, P.-Y.; Shang, Y.-S.; Wang, Z.-L. Safety and efficacy of anti-inflammatory therapy in patients with coronary artery disease: A systematic review and meta-analysis. BMC Cardiovasc. Disord. 2022, 22, 84. [Google Scholar] [CrossRef]
- Nidorf, S.M.; Eikelboom, J.W.; Budgeon, C.A.; Thompson, P.L. Low-dose colchicine for secondary prevention of cardiovascular disease. J. Am. Coll. Cardiol. 2013, 61, 404–410. [Google Scholar] [CrossRef] [PubMed]
- Martínez, G.J.; Robertson, S.; Barraclough, J.; Xia, Q.; Mallat, Z.; Bursill, C.; Celermajer, D.S.; Patel, S. Colchicine Acutely Suppresses Local Cardiac Production of Inflammatory Cytokines in Patients with an Acute Coronary Syndrome. J. Am. Heart Assoc. 2015, 4, e002128. [Google Scholar] [CrossRef] [PubMed]
- Akodad, M.; Lattuca, B.; Nagot, N.; Georgescu, V.; Buisson, M.; Cristol, J.P.; Leclercq, F.; Macia, J.-C.; Gervasoni, R.; Cung, C.-C.; et al. COLIN: Intérêt d’un traitement par colchicine dans l’infarctus du myocarde avec réponse inflammatoire. Arch. Cardiovasc. Dis. 2017, 110, 395–402. [Google Scholar] [CrossRef] [PubMed]
- Tong, D.C.; Quinn, S.; Nasis, A.; Hiew, C.; Roberts-Thomson, P.; Adams, H.; Sriamareswaran, R.; Htun, N.M.; Wilson, W.; Stub, D.; et al. Colchicine in Patients with Acute Coronary Syndrome the Australian COPS Randomized Clinical Trial. Circulation 2020, 142, 1890–1900. [Google Scholar] [CrossRef] [PubMed]
- Nidorf, S.M.; Fiolet, A.T.L.; Mosterd, A.; Eikelboom, J.W.; Schut, A.; Opstal, T.S.J.; Salem, H.K.; Xu, X.-F.; Ireland, M.A.; Lenderink, T.; et al. Colchicine in Patients with Chronic Coronary Disease. N. Engl. J. Med. 2020, 383, 1838–1847. [Google Scholar] [CrossRef]
- Shah, B.; Pillinger, M.; Zhong, H.; Cronstein, B.; Xia, Y.; Lorin, J.D.; Smilowitz, N.R.; Feit, F.; Ratnapala, N.; Keller, N.M.; et al. Effects of Acute Colchicine Administration Prior to Percutaneous Coronary Intervention: COLCHICINE-PCI Randomized Trial. Circ. Cardiovasc. Interv. 2020, 13, e008717. [Google Scholar] [CrossRef]
- Morton, A.; Rothman, A. The effect of interleukin-1 receptor antagonist therapy on markers of inflammation in non-ST elevation acute coronary syndromes: The MRC-ILA Heart Study. Eur. Heart J. 2015, 36, 377–384. [Google Scholar] [CrossRef] [PubMed]
- Kleveland, O.; Kunszt, G.; Bratlie, M.; Ueland, T.; Broch, K.; Holte, E.; Michelsen, A.E.; Bendz, B.; Amundsen, B.H.; Espevik, T.; et al. Effect of a single dose of the interleukin-6 receptor antagonist tocilizumab on inflammation and troponin T release in patients with non-ST-elevation myocardial infarction: A double-blind, randomized, placebo-controlled phase 2 trial. Eur. Heart J. 2016, 37, 2406–2413. [Google Scholar] [CrossRef]
- Ridker, P.M.; Everett, B.M.; Pradhan, A.; MacFadyen, J.G.; Solomon, D.H.; Zaharris, E.; Mam, V.; Hasan, A.; Rosenberg, Y.; Iturriaga, E.; et al. Low-Dose Methotrexate for the Prevention of Atherosclerotic Events. N. Engl. J. Med. 2019, 380, 752–762. [Google Scholar] [CrossRef]
- Abbate, A.; Trankle, C.R.; Buckley, L.F.; Lipinski, M.J.; Appleton, D.; Kadariya, D.; Canada, J.M.; Carbone, S.; Roberts, C.S.; Abouzaki, N.; et al. Interleukin-1 Blockade Inhibits the Acute Inflammatory Response in Patients with ST-Segment–Elevation Myocardial Infarction. J. Am. Heart Assoc. 2020, 9, e014941. [Google Scholar] [CrossRef]
- Kapoor, D.; Trikha, D.; Vijayvergiya, R.; Parashar, K.K.; Kaul, D.; Dhawan, V. Short-Term Adjuvant Therapy with Terminalia arjuna Attenuates Ongoing Inflammation and Immune Imbalance in Patients with Stable Coronary Artery Disease: In Vitro and In Vivo Evidence. J. Cardiovasc. Transl. Res. 2015, 8, 173–186. [Google Scholar] [CrossRef] [PubMed]
- Lee, B.-J.; Lin, J.-S.; Lin, Y.-C.; Lin, P.-T. Antiinflammatory effects of l-carnitine supplementation (1000 mg/d) in coronary artery disease patients. Nutrition 2015, 31, 475–479. [Google Scholar] [CrossRef]
- Altunina, N.V.; Lizogub, V.G.; Bondarchuk, O.M. Alpha-Lipoic Acid as a Means of Influence on Systemic Inflammation in Type 2 Diabetes Mellitus Patients with Prior Myocardial Infarction. J. Med. Life 2020, 13, 32–36. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.-S.; Yen, P.-T.; Weng, S.-F.; Hsu, J.-H.; Yeh, J.-L. Clinical Patterns of Traditional Chinese Medicine for Ischemic Heart Disease Treatment: A Population-Based Cohort Study. Medicina 2022, 58, 879. [Google Scholar] [CrossRef] [PubMed]
- Deftereos, S.G.; Beerkens, F.J.; Shah, B.; Giannopoulos, G.; Vrachatis, D.A.; Giotaki, S.G.; Siasos, G.; Nicolas, J.; Arnott, C.; Patel, S.; et al. Colchicine in Cardiovascular Disease: In-Depth Review. Circulation 2022, 145, 61–78. [Google Scholar] [PubMed]
- Pradhan, A.D. Time to commence or time out for colchicine in secondary prevention of cardiovascular disease? Eur. Heart J. 2021, 42, 2776–2779. [Google Scholar] [CrossRef]
- Nelson, K.; Fuster, V.; Ridker, P.M. Low-Dose Colchicine for Secondary Prevention of Coronary Artery Disease: JACC Review Topic of the Week. J. Am. Coll. Cardiol. 2023, 82, 648–660. [Google Scholar] [CrossRef]
- Chow, S.L.; Bozkurt, B.; Baker, W.L.; Bleske, B.E.; Breathett, K.; Fonarow, G.C.; Greenberg, B.; Khazanie, P.; Leclerc, J.; Morris, A.A.; et al. Complementary and Alternative Medicines in the Management of Heart Failure: A Scientific Statement from the American Heart Association. Circulation 2023, 147, e4–e30. [Google Scholar] [CrossRef]
- Kapoor, D.; Vijayvergiya, R.; Dhawan, V. Terminalia arjuna in coronary artery disease: Ethnopharmacology, pre-clinical, clinical & safety evaluation. J. Ethnopharmacol. 2014, 155, 1029–1045. [Google Scholar]
- Ma, X.J.; Duan, W.H.; Zhang, Y.; Gao, J.; Guan, B.Y.; Chen, K.J.; Shi, D.Z. Combination of Activating Blood Circulation and Detoxifying Chinese Medicines Played an Anti-Inflammatory Role in Unstable Angina Patients after Percutaneous Coronary Intervention: A Multicenter, Open-Labeled, Randomized Controlled Trial. China J. Integr. Med. 2021, 27, 803–810. [Google Scholar] [CrossRef]
- Freires, I.A.; de Alencar, S.M.; Rosalen, P.L. A pharmacological perspective on the use of Brazilian Red Propolis and its isolated compounds against human diseases. Eur. J. Med. Chem. 2016, 110, 267–279. [Google Scholar] [CrossRef] [PubMed]
- Berretta, A.A.; Silveira, M.A.D.; Cóndor Capcha, J.M.; De Jong, D. Propolis and its potential against SARS-CoV-2 infection mechanisms and COVID-19 disease: Running title: Propolis against SARS-CoV-2 infection and COVID-19. Biomed. Pharmacother. 2020, 131, 110622. [Google Scholar] [CrossRef] [PubMed]
- Hallajzadeh, J.; Milajerdi, A.; Amirani, E.; Attari, V.E.; Maghsoudi, H.; Mirhashemi, S.M. Effects of propolis supplementation on glycemic status, lipid profiles, inflammation and oxidative stress, liver enzymes, and body weight: A systematic review and meta-analysis of randomized controlled clinical trials. J. Diabetes Metab. Disord. 2021, 20, 831–843. Available online: https://doi.org/10.1007/s40200-020-00696-w (accessed on 12 August 2023). [CrossRef] [PubMed]
- Machado, J.L.; Assunção, A.K.M.; da Silva, M.C.P.; Reis , A.S.D.; Costa, G.C.; de Sousa Arruda, D.; Rocha, B.A.; de Oliveira Lima Leite Vaz, M.M.; de Andrade Paes, A.M.; Guerra, R.N.M.; et al. Brazilian green propolis: Anti-inflammatory property by an immunomodulatory activity. Complement. Altern. Med. 2012, 2012, 157652. [Google Scholar] [CrossRef] [PubMed]
- Duarte Silveira, M.A.; Malta-Santos, H.; Rebouças-Silva, J.; Teles, F.; Batista Dos Santos Galvão, E.; Pinto De Souza, S.; Dantas Dutra, F.R.; Dantas Gomes, M.M.; Teixeira, M.B.; Rebelo da Conceição, L.F.M.; et al. Effects of Standardized Brazilian Green Propolis Extract (EPP-AF®) on Inflammation in Haemodialysis Patients: A Clinical Trial. Int. J. Nephrol. 2022, 2022, 1035475. [Google Scholar] [CrossRef] [PubMed]
- Duarte Silveira, M.A.; De Jong, D.; Berretta, A.A.; dos Galvão, E.B.S.; Ribeiro, J.C.; Cerqueira-Silva, T.; Chaves Amorim, T.; Rebelo da Conceição, L.F.M.; Dantas Gomes, M.M.; Teixeira, M.B.; et al. Efficacy of Brazilian green propolis (EPP-AF®) as an adjunct treatment for hospitalized COVID-19 patients: A randomized, controlled clinical trial. Biomed. Pharmacother. 2021, 138, 111526. [Google Scholar] [CrossRef] [PubMed]
- Silva, H.; Francisco, R.; Saraiva, A.; Francisco, S.; Carrascosa, C.; Raposo, A. The Cardiovascular Therapeutic Potential of Propolis—A Comprehensive Review. Biology 2021, 10, 27. [Google Scholar] [CrossRef]
- Bojić, M.; Antolić, A.; Tomičić, M.; Debeljak, Ž.; Maleš, Ž. Propolis ethanolic extracts reduce adenosine diphosphate induced platelet aggregation determined on whole blood. Nutr. J. 2018, 17, 52. [Google Scholar] [CrossRef]
| Trial | Year of Study | Nº of Patients | Inclusion Criteria | Investigated Drug | Primary Outcomes | Results |
|---|---|---|---|---|---|---|
| Nidorf et al. * [21] | 2013 | 532 | Patients with chronic coronary disease using statins and standard secondary prevention therapy | Colchicine 0.5 mg o.d. vs. no colchicine | ACS, out-of-hospital cardiac arrest, and/or non-cardioembolic ischemic stroke | After a median of 36 months, 5.3% of patients in the colchicine group had a primary outcome versus 15% in the no colchicine group (HR 0.33, 95% CI 0.18–0.59; p < 0.001). |
| Martínez et al. [22] | 2015 | 83 | Patients with ACS (excluding STEMI), stable CAD, and controls (no evidence of lesions) who would undergo coronary angiography | Colchicine 1 mg o.d. vs. placebo | Assessment of IL-1β, IL-6, and IL-18 levels in coronary arteries | Colchicine significantly reduced the transcoronary gradients of these markers in patients with ACS (p = 0.028, 0.032, and 0.032, for IL-1b, IL-18, and IL-6, respectively). There was no difference for those with stable CAD. |
| Akodad et al. [23] | 2017 | 44 | Patients with STEMI who underwent an angioplasty of the culprit lesion | Colchicine 1 mg o.d. + OMT vs. OMT | CRP peak assessment during hospitalization | No significant difference in CRP peak between those who used or did not use colchicine (29.03 mg/L × 21.86 mg/L, respectively, p = 0.86). |
| Tardif et al. [18] | 2019 | 4745 | Patients who had AMI within 30 days and were treated with PCI and were using statins and OMT | Colchicine 0.5 mg o.d. vs. placebo | Cardiovascular death, CPR, AMI, stroke, or hospitalization for angina with subsequent revascularization | Colchicine reduced the primary endpoint (HR 0.77, 95% CI 0.61–0.96, p = 0.02) at 19.6 months of follow-up. |
| Tong et al. [24] | 2020 | 795 | Patients with ACS and evidence of CAD on coronary angiography who were treated with PCI or medical therapy | Colchicine 0.5 mg b.i.d. for 30 days followed by 0.5 mg o.d. vs. placebo | Death for any cause, ACS, ischemia-driven urgent revascularization, and stroke | Over the 12-month follow-up period, there was no significant difference in primary endpoint between the two groups (24 (6.1%) in the colchicine group versus 38 (9.5%) in the placebo group). |
| Nidorf et al. [25] | 2020 | 5572 | Patients with stable CAD receiving OMT for at least six months (catheterization or coronary CT angiography with significant lesion or calcium score with Agatston score > 400) | Colchicine 0.5 mg o.d. vs. placebo | Cardiovascular death, spontaneous AMI, stroke, and coronary revascularization | After 28.6 months, colchicine reduced the primary endpoint (HR 0.69, 95% CI 0.57–0.83, p < 0.001). |
| Shah et al. [26] | 2020 | 400 | Patients with stable CAD who would undergo coronary angioplasty | Colchicine 1.8 mg o.d. vs. placebo | Evaluation of myocardial injury reduction after angioplasty | No difference in myocardial injury related to angioplasty. No differences in the secondary endpoint of MACE reduction at 30 days. There was an attenuation in the increase in IL-6 and CRP in the colchicine group within 24 h after the procedure. |
| Trial | Year of Study | Nº of Patients | Inclusion Criteria | Investigated Drug | Primary Outcomes | Results |
|---|---|---|---|---|---|---|
| Morton et al. [27] | 2015 | 182 | Patients with NSTEMI presenting with <48 h from onset of chest pain | Anakinra (100 mg o.d.) vs. placebo | Evaluation of AUC of serum hs-CRP over the first 7 days | The hs-CRP AUC was 21.98 mg day/L in the IL-1ra group and 43.50 mg day/L in the placebo group, with the geometric mean ratio between IL-1ra and placebo being 0.51 (95% CI: 0.32–0.79, p = 0.0028). |
| Kleveland et al. [28] | 2016 | 117 | Patients with NSTEMI scheduled for coronary angiography. | Tocilizumab (single dose of 280 mg) or placebo | Evaluation of AUC of serum hs-CRP on days 1 and 3 | The median AUC for hs-CRP during hospitalization was 2.1 times greater in the placebo group than in the tocilizumab group (4.2 vs. 2.0 mg/L/h, p < 0.001). |
| Ridker et al. [19] | 2017 | 10061 | Patients with previous AMI and high hs-CRP (>2 mg/L) | Canakinumab (50 mg, 150 mg e 300 mg) vs. placebo | Nonfatal AMI, nonfatal stroke, and cardiovascular death | Only the 150 mg dose showed a significant reduction in the primary outcome vs. placebo (HR 0.85, p = 0.02) after 3.7 years. There was a reduction in hs-CRP and IL-6 levels with all doses. |
| Ridker et al. [29] | 2019 | 4786 | Patients with a history of AMI or multivessel CAD and T2DM or metabolic syndrome | Low-dose methotrexate vs. placebo | Nonfatal AMI, nonfatal stroke, and cardiovascular death | No difference in primary outcome between groups (HR 0.96, CI 0.79–1.16 p = 0.67). No reductions in hsCRP, IL-6, and IL-1β levels were observed. |
| Abbate et al. [30] | 2020 | 99 | Patients with an STEMI who underwent urgent coronary angiography within 12 h of symptom onset | Anakinra 100 mg o.d. vs. Anakinra 100 mg b.i.d. vs. placebo | Evaluation of AUC of serum hs-CRP at baseline, 72 h, and day 14 | The AUC of hs-CRP was lower in the anakinra group versus the placebo (median, 67 (IQ range 39–120) versus 214 (IQ range 131–394) mg day/L; p < 0.001. No significant differences were observed between the two regimens of anakinra. The incidence of death or new-onset or worsening HF was lower with anakinra (p = 0.046). |
| Trial | Year of Study | Nº of Patients | Inclusion Criteria | Investigated Drug | Primary Outcomes | Results |
|---|---|---|---|---|---|---|
| Kapoor et al. [31] | 2015 | 116 | Patients with stable CAD and OMT | Terminalia arjuna 500 mg b.i.d. vs. placebo | Assessment of levels of inflammatory markers (IL-6, IL-18, TNF-α, IL-10, and hs-CRP) and lipid profile | T. arjuna reduced CT, TG, VLDL, IL-6, IL-18, TNF-α, and hsCRP. There was an increase in HDL and IL-10. No differences were observed in MACE. |
| Bor-Jen Lee et al. [32] | 2015 | 47 | Patients with CAD (catheterization with lesion > 50% or previous angioplasty) | L-carnitine 1000 mg o.d. vs. placebo | Assessment of levels of inflammatory markers (IL-6, TNF-α, and CRP) | LC supplementation reduced CRP levels by 10%, IL-6 by 17%, and TNF-α by 6% (p = 0.03) when compared to placebo after 12 weeks. |
| Altunina et al. [33] | 2020 | 112 | Patients with T2DM and a history of previous AMI using oral hypoglycemic agents, antiplatelet agents, and statins | ALA 600 mg vs. placebo | Assessment of CRP, IL-6, TNF-α, and IL-10 levels | ALA was associated with a 30.9% reduction in CRP, 29.7% in IL-6, and 22.7% in TNF-α after 4 months. |
| Wang et al. [34] | 2021 | 154 | Patients aged 40–75 years with unstable angina who underwent angioplasty within the last 48 h | ABCD group (Guanxin Danshen Dropping Pill 0.4 g and andrographis 0.2 g) vs. ABC (Guanxin Danshen Dropping Pill 0.4 g) | hs-CRP evaluation | After 30 days, the ABCD group showed a reduction in hs-CRP compared to the ABC group (2.96 mg/L × 1.54 mg/L, p < 0.05). The ABCD group also showed a reduction in IL-6 and TNF-α levels. There was an improvement in the angina score in the ABCD group versus the ABC group (p < 0.05). |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Figueiredo, C.S.; Roseira, E.S.; Viana, T.T.; Silveira, M.A.D.; de Melo, R.M.V.; Fernandez, M.G.; Lemos, L.M.G.; Passos, L.C.S. Inflammation in Coronary Atherosclerosis: Insights into Pathogenesis and Therapeutic Potential of Anti-Inflammatory Drugs. Pharmaceuticals 2023, 16, 1242. https://doi.org/10.3390/ph16091242
Figueiredo CS, Roseira ES, Viana TT, Silveira MAD, de Melo RMV, Fernandez MG, Lemos LMG, Passos LCS. Inflammation in Coronary Atherosclerosis: Insights into Pathogenesis and Therapeutic Potential of Anti-Inflammatory Drugs. Pharmaceuticals. 2023; 16(9):1242. https://doi.org/10.3390/ph16091242
Chicago/Turabian StyleFigueiredo, Clara Salles, Elias Soares Roseira, Tainá Teixeira Viana, Marcelo Augusto Duarte Silveira, Rodrigo Morel Vieira de Melo, Miguel Godeiro Fernandez, Livia Maria Goes Lemos, and Luiz Carlos Santana Passos. 2023. "Inflammation in Coronary Atherosclerosis: Insights into Pathogenesis and Therapeutic Potential of Anti-Inflammatory Drugs" Pharmaceuticals 16, no. 9: 1242. https://doi.org/10.3390/ph16091242
APA StyleFigueiredo, C. S., Roseira, E. S., Viana, T. T., Silveira, M. A. D., de Melo, R. M. V., Fernandez, M. G., Lemos, L. M. G., & Passos, L. C. S. (2023). Inflammation in Coronary Atherosclerosis: Insights into Pathogenesis and Therapeutic Potential of Anti-Inflammatory Drugs. Pharmaceuticals, 16(9), 1242. https://doi.org/10.3390/ph16091242





