A 5-Year Study of Antiseizure Medications (ASMs) Monitoring in Patients with Neuropsychiatric Disorders in an Italian Clinical Center
Abstract
1. Introduction
2. Results
2.1. Description of ASMs C(p) Samples during the Period 2018–2022
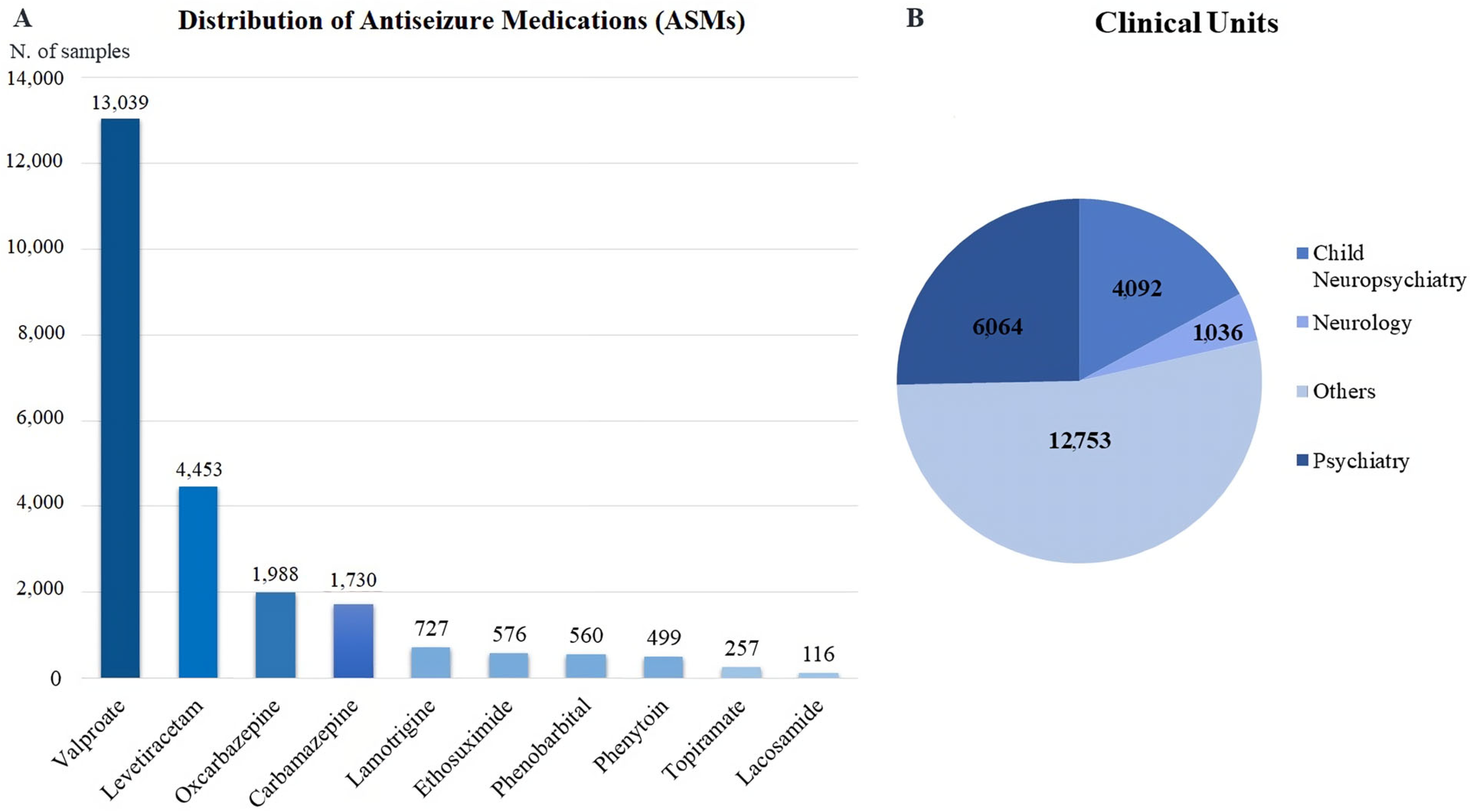
2.2. General Distribution of ASMs C(p) Samples
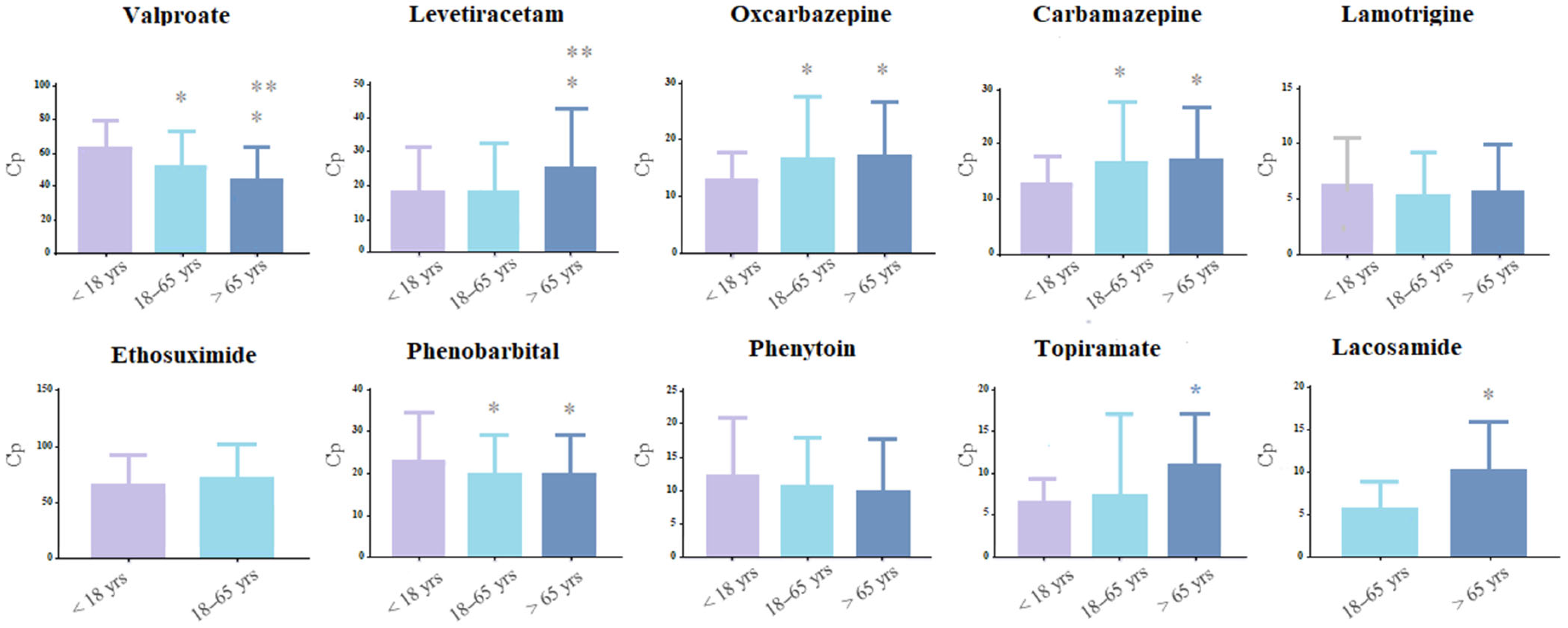
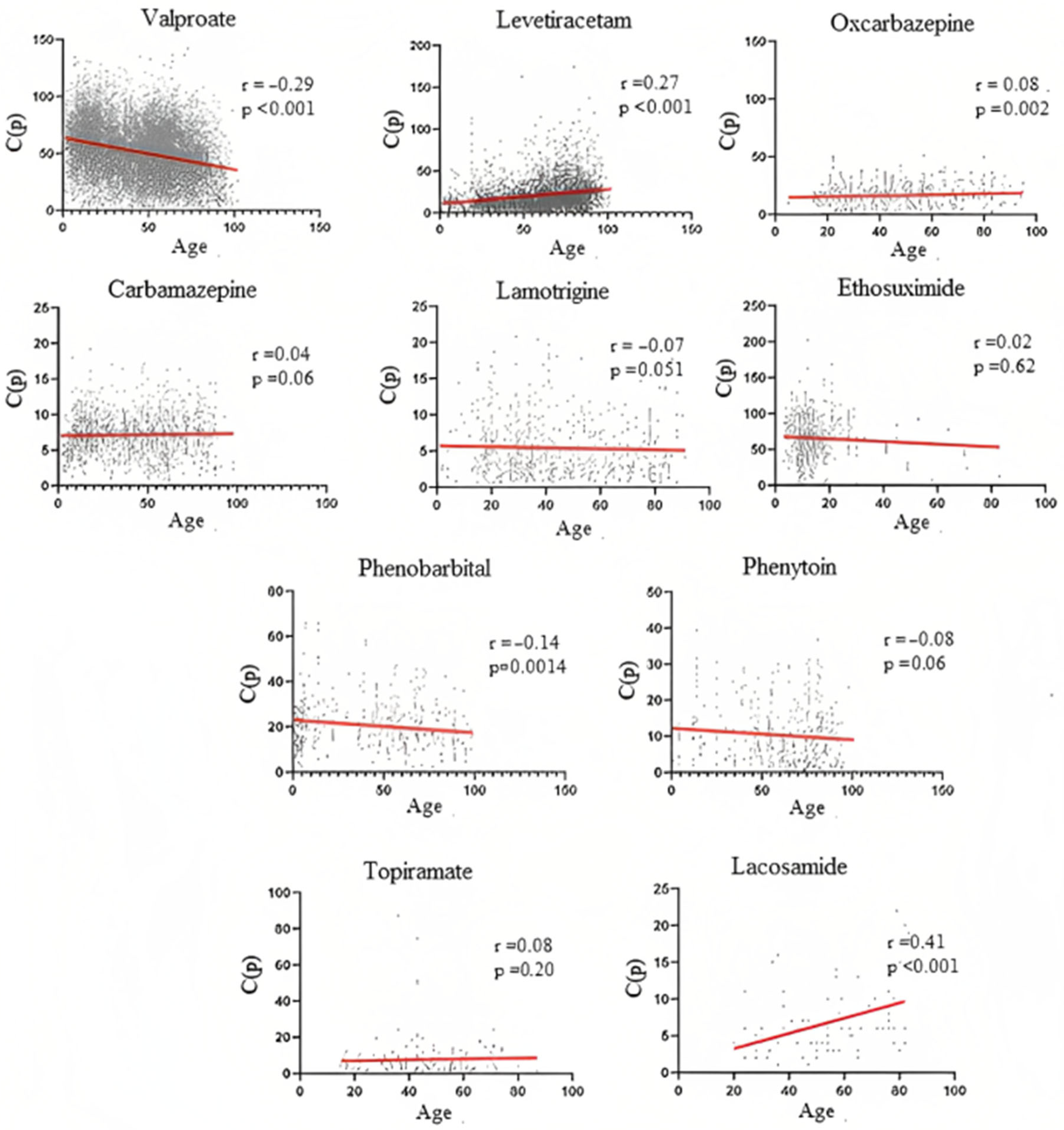
2.3. Distribution of ASMs C(p) Samples across Different Ages
2.4. Distribution of ASMs C(p) Samples in Relation to Gender
2.5. Analysis of the ASMs C(p) Samples Comparing the Neurological, Psychiatric, and Child Neuropsychiatry Units
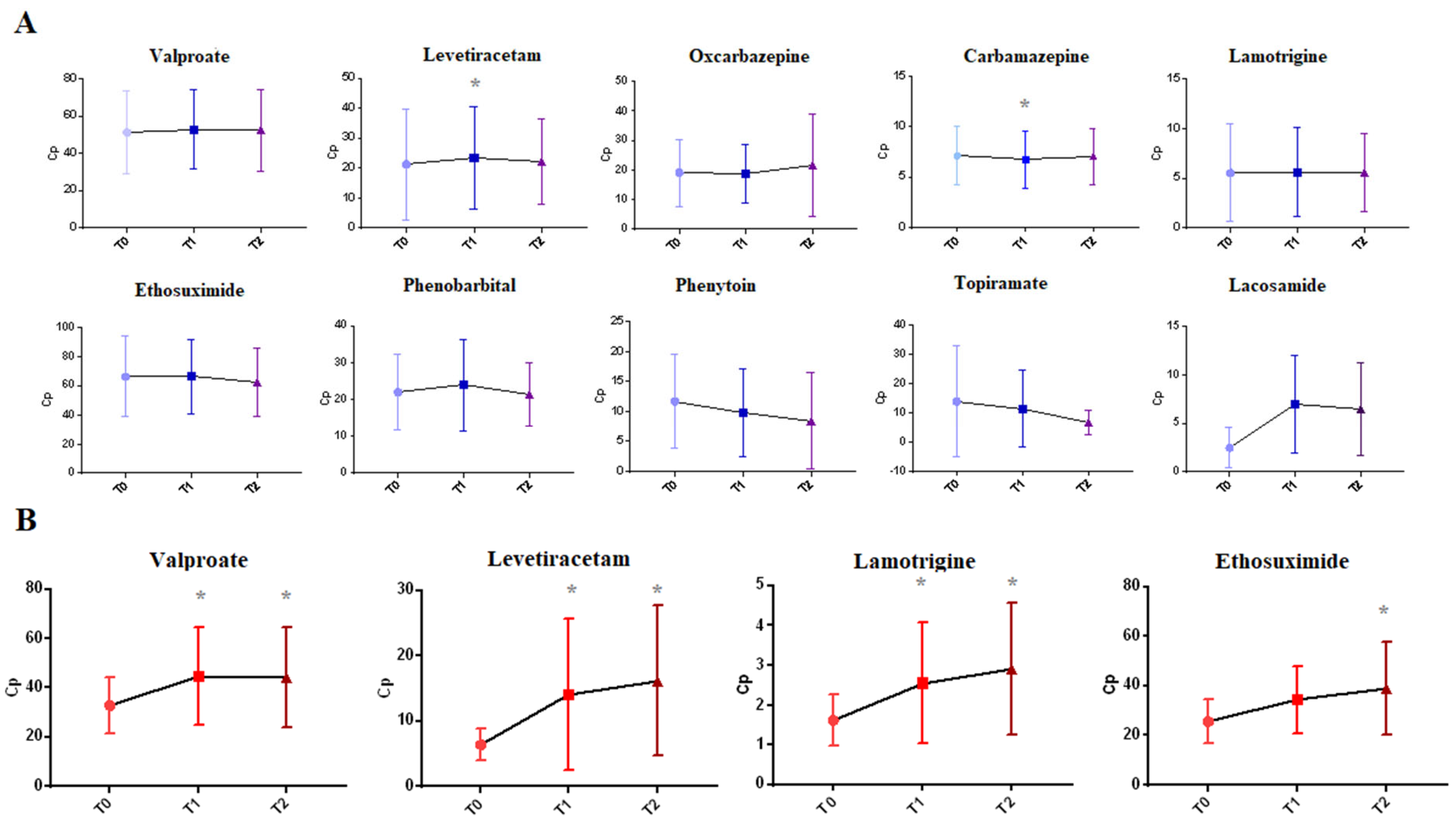
2.6. Analysis of Multiple Dosing for Patients Plasma Monitored Repeatedly during One Year
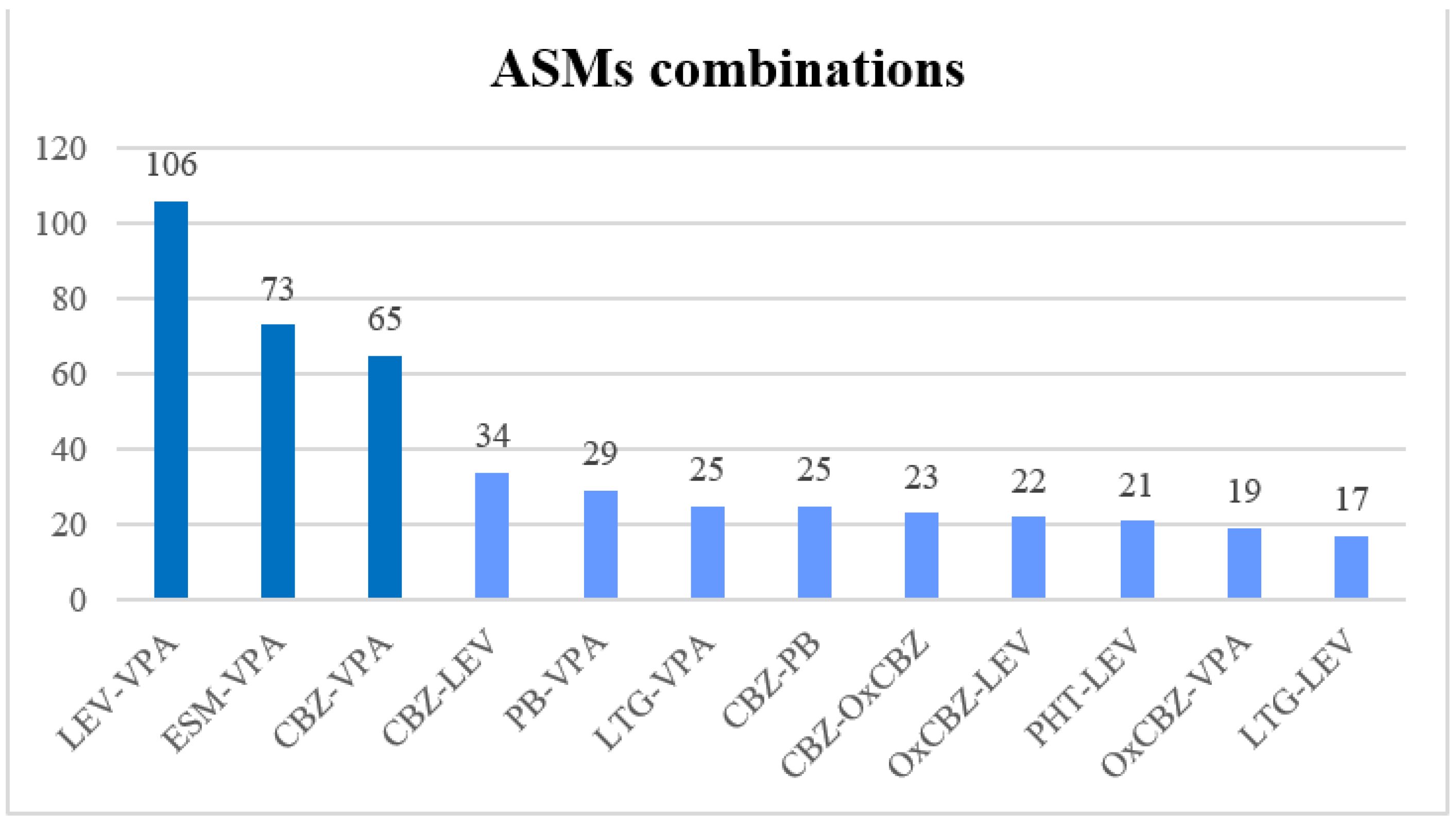
2.7. Analysis of the ASMs in Combination Therapy
3. Discussion
4. Materials and Methods
4.1. Study Sample
4.2. Analytical Determination of ASMs Plasma Concentrations
4.3. Data Analysis
4.4. Ethical Statement
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kwan, P.; Schachter, S.C.; Brodie, M.J. Drug-resistant epilepsy. N. Engl. J. Med. 2011, 365, 919–926. [Google Scholar] [CrossRef]
- Mendlewicz, J.; Massat, I.; Linotte, S.; Kasper, S.; Konstantinidis, A.; Lecrubier, Y.; Montgomery, S.; Serretti, A.; Zohar, J.; Souery, D. Identification of clinical factors associated with resistance to antidepressants in bipolar depression: Results from an European Multicentre Study. Int. Clin. Psychopharmacol. 2010, 25, 297–301. [Google Scholar] [CrossRef]
- Palleria, C.; Di Paolo, A.; Giofrè, C.; Caglioti, C.; Leuzzi, G.; Siniscalchi, A.; De Sarro, G.; Gallelli, L. Pharmacokinetic drug-drug interaction and their implication in clinical management. J. Res. Med. Sci. Off. J. Isfahan Univ. Med. Sci. 2013, 18, 601–610. [Google Scholar]
- Hiemke, C.; Bergemann, N.; Clement, H.W.; Conca, A.; Deckert, J.; Domschke, K.; Eckermann, G.; Egberts, K.; Gerlach, M.; Greiner, C.; et al. Consensus Guidelines for Therapeutic Drug Monitoring in Neuropsychopharmacology: Update 2017. Pharmacopsychiatry 2018, 51, 9–62. [Google Scholar] [CrossRef]
- Touw, D.J.; Neef, C.; Thomson, A.H.; Vinks, A.A. Cost-effectiveness of therapeutic drug monitoring: A systematic review. Ther. Drug Monit. 2005, 27, 10–17. [Google Scholar] [CrossRef]
- Kolachalam, S.; Aringhieri, S.; Scarselli, M. Therapeutic Drug Monitoring in Neuropsychiatric Disorders. In Brain and Heart Dynamics; Springer: Cham, Switzerland, 2020; pp. 1–11. [Google Scholar] [CrossRef]
- Patsalos, P.N.; Berry, D.J.; Bourgeois, B.F.D.; Cloyd, J.C.; Glauser, T.A.; Johannessen, S.I.; Leppik, I.E.; Tomson, T.; Perucca, E. Antiepileptic drugs—Best practice guidelines for therapeutic drug monitoring: A position paper by the subcommission on therapeutic drug monitoring, ILAE Commission on Therapeutic Strategies. Epilepsia 2008, 49, 1239–1276. [Google Scholar] [CrossRef]
- Bialer, M. Why are antiepileptic drugs used for nonepileptic conditions? Epilepsia 2012, 53 (Suppl. 7), 26–33. [Google Scholar] [CrossRef]
- Cutrer, F.M.; Limmroth, V.; Moskowitz, M.A. Possible mechanisms of valproate in migraine prophylaxis. Cephalalgia 1997, 17, 93–100. [Google Scholar] [CrossRef]
- Natale, G.; Fini, E.; Calabrò, P.F.; Carli, M.; Scarselli, M.; Bocci, G. Valproate and lithium: Old drugs for new pharmacological approaches in brain tumors? Cancer Lett. 2023, 560, 216125. [Google Scholar] [CrossRef]
- Scarselli, M. Lithium and Valproic Acid in Bipolar Disorders and Beyond. Curr. Neuropharmacol. 2023, 21, 56126. [Google Scholar] [CrossRef]
- Freitag, F.G.; Collins, S.D.; Carlson, H.A.; Goldstein, J.; Saper, J.; Silberstein, S.; Mathew, N.; Winner, P.K.; Deaton, R.; Sommerville, K. A randomized trial of divalproex sodium extended-release tablets in migraine prophylaxis. Neurology 2002, 58, 1652–1659. [Google Scholar] [CrossRef]
- Smits, J.E.M.P.; Wallenburg, E.; van Spanje, A.; van Luin, M.; Marijnissen, R.M. Valproate Intoxication in a Patient With Blood Valproate Levels Within Therapeutic Range. J. Clin. Psychiatry 2017, 78, e413–e414. [Google Scholar] [CrossRef]
- Talaei, A.; Dastgheib, M.S.; Soltanifar, A.; Mokhber, N.; Akhondzadeh, S.; Afzaljavan, F. Oxcarbazepine versus sodium valproate in treatment of acute mania: A double-blind randomized clinical trial. Int. Clin. Psychopharmacol. 2022, 37, 116–121. [Google Scholar] [CrossRef]
- Unholzer, S.; Haen, E. Retrospective analysis of therapeutic drug monitoring data for treatment of bipolar disorder with lamotrigine. Pharmacopsychiatry 2015, 48, 211–214. [Google Scholar] [CrossRef]
- Gill, D.; Derry, S.; Wiffen, P.J.; Moore, R.A. Valproic acid and sodium valproate for neuropathic pain and fibromyalgia in adults. Cochrane Database Syst. Rev. 2011, 2011, CD009183. [Google Scholar] [CrossRef]
- Nevitt, S.J.; Sudell, M.; Cividini, S.; Marson, A.G.; Tudur Smith, C. Antiepileptic drug monotherapy for epilepsy: A network meta-analysis of individual participant data. Cochrane Database Syst. Rev. 2022, 4, CD011412. [Google Scholar] [CrossRef]
- Kanner, A.M.; Bicchi, M.M. Antiseizure Medications for Adults With Epilepsy: A Review. JAMA 2022, 327, 1269–1281. [Google Scholar] [CrossRef]
- EMA. PRAC recommends new measures to avoid valproate exposure in pregnancy. Medicines 2018, 44, 1–4. [Google Scholar]
- Grant, S.M.; Faulds, D. Oxcarbazepine. A review of its pharmacology and therapeutic potential in epilepsy, trigeminal neuralgia and affective disorders. Drugs 1992, 43, 873–888. [Google Scholar] [CrossRef]
- Pal, D.K.; Das, T.; Chaudhury, G.; Johnson, A.L.; Neville, B.G. Randomised controlled trial to assess acceptability of phenobarbital for childhood epilepsy in rural India. Lancet 1998, 351, 19–23. [Google Scholar] [CrossRef]
- Kale, R.; Perucca, E. Revisiting phenobarbital for epilepsy. Br. Med. J. 2004, 329, 1199–1200. [Google Scholar] [CrossRef] [PubMed]
- Oyemolade, T.A.; Adeolu, A.A.; Badejo, O.A.; Balogun, J.A.; Shokunbi, M.T.; Malomo, A.O.; Adeleye, A.O. Efficacy of 48 h dose of phenytoin in prevention of early post-traumatic seizure. BMJ Neurol. Open 2023, 5, e000377. [Google Scholar] [CrossRef] [PubMed]
- Kwan, P.; Brodie, M.J. Early identification of refractory epilepsy. N. Engl. J. Med. 2000, 342, 314–319. [Google Scholar] [CrossRef]
- Zhu, L.-N.; Chen, D.; Xu, D.; Tan, G.; Wang, H.-J.; Liu, L. Newer antiepileptic drugs compared to levetiracetam as adjunctive treatments for uncontrolled focal epilepsy: An indirect comparison. Seizure 2017, 51, 121–132. [Google Scholar] [CrossRef]
- Crapanzano, C.; Casolaro, I.; Amendola, C.; Damiani, S. Lithium and Valproate in Bipolar Disorder: From International Evidence-based Guidelines to Clinical Predictors. Clin. Psychopharmacol. Neurosci. Off. Sci. J. Korean Coll. Neuropsychopharmacol. 2022, 20, 403–414. [Google Scholar] [CrossRef]
- Jannuzzi, G.; Cian, P.; Fattore, C.; Gatti, G.; Bartoli, A.; Monaco, F.; Perucca, E. A multicenter randomized controlled trial on the clinical impact of therapeutic drug monitoring in patients with newly diagnosed epilepsy. The Italian TDM Study Group in Epilepsy. Epilepsia 2000, 41, 222–230. [Google Scholar] [CrossRef]
- Al-Roubaie, Z.; Guadagno, E.; Ramanakumar, A.V.; Khan, A.Q.; Myers, K.A. Clinical utility of therapeutic drug monitoring of antiepileptic drugs: Systematic review. Neurol. Clin. Pract. 2020, 10, 344–355. [Google Scholar] [CrossRef]
- Hodges, J.C.; Treadwell, J.; Malphrus, A.D.; Tran, X.G.; Giardino, A.P. Identification and Prevention of Antiepileptic Drug Noncompliance: The Collaborative Use of State-Supplied Pharmaceutical Data. ISRN Pediatr. 2014, 2014, 734689. [Google Scholar] [CrossRef]
- Pennazio, F.; Brasso, C.; Villari, V.; Rocca, P. Current Status of Therapeutic Drug Monitoring in Mental Health Treatment: A Review. Pharmaceutics 2022, 14, 2674. [Google Scholar] [CrossRef]
- Werler, M.M.; Ahrens, K.A.; Bosco, J.L.F.; Mitchell, A.A.; Anderka, M.T.; Gilboa, S.M.; Holmes, L.B. Use of antiepileptic medications in pregnancy in relation to risks of birth defects. Ann. Epidemiol. 2011, 21, 842–850. [Google Scholar] [CrossRef]
- Hussein, A.; Abdulgalil, A.; Omer, F.; Eltoum, H.; Hamad, A.; El-Adil, O.; Mubarak, B.; Malkaldar, M.; Idris, I.; Alwidaa, Y.; et al. Correlation between Serum Level of Antiepileptic Drugs and their Side Effects. Oman Med. J. 2010, 25, 17–21. [Google Scholar] [CrossRef]
- Riva, R.; Albani, F.; Contin, M.; Baruzzi, A. Pharmacokinetic interactions between antiepileptic drugs. Clinical considerations. Clin. Pharmacokinet. 1996, 31, 470–493. [Google Scholar] [CrossRef]
- Fuhr, L.M.; Marok, F.Z.; Hanke, N.; Selzer, D.; Lehr, T. Pharmacokinetics of the CYP3A4 and CYP2B6 Inducer Carbamazepine and Its Drug-Drug Interaction Potential: A Physiologically Based Pharmacokinetic Modeling Approach. Pharmaceutics 2021, 13, 270. [Google Scholar] [CrossRef]
- Brigo, F.; Igwe, S.C. Ethosuximide, sodium valproate or lamotrigine for absence seizures in children and adolescents. Cochrane Database Syst. Rev. 2017, 2, CD003032. [Google Scholar] [CrossRef]
- Marson, A.; Burnside, G.; Appleton, R.; Smith, D.; Leach, J.P.; Sills, G.; Tudur-Smith, C.; Plumpton, C.; Hughes, D.A.; Williamson, P.; et al. The SANAD II study of the effectiveness and cost-effectiveness of valproate versus levetiracetam for newly diagnosed generalised and unclassifiable epilepsy: An open-label, non-inferiority, multicentre, phase 4, randomised controlled trial. Lancet 2021, 397, 1375–1386. [Google Scholar] [CrossRef]
- Glauser, T.A.; Cnaan, A.; Shinnar, S.; Hirtz, D.G.; Dlugos, D.; Masur, D.; Clark, P.O.; Adamson, P.C. Ethosuximide, valproic acid, and lamotrigine in childhood absence epilepsy: Initial monotherapy outcomes at 12 months. Epilepsia 2013, 54, 141–155. [Google Scholar] [CrossRef]
- Yee, C.S.; Vázquez, G.H.; Hawken, E.R.; Biorac, A.; Tondo, L.; Baldessarini, R.J. Long-Term Treatment of Bipolar Disorder with Valproate: Updated Systematic Review and Meta-analyses. Harv. Rev. Psychiatry 2021, 29, 188–195. [Google Scholar] [CrossRef]
- Rosemond, E.; Rossi, M.; McMillin, S.M.; Scarselli, M.; Donaldson, J.G.; Wess, J. Regulation of M₃ muscarinic receptor expression and function by transmembrane protein 147. Mol. Pharmacol. 2011, 79, 251–261. [Google Scholar] [CrossRef]
- Carli, M.; Risaliti, E.; Francomano, M.; Kolachalam, S.; Longoni, B.; Bocci, G.; Maggio, R.; Scarselli, M. A 5-Year Study of Lithium and Valproic Acid Drug Monitoring in Patients with Bipolar Disorders in an Italian Clinical Center. Pharmaceuticals 2022, 15. [Google Scholar] [CrossRef]
- Linde, M.; Mulleners, W.M.; Chronicle, E.P.; McCrory, D.C. Valproate (valproic acid or sodium valproate or a combination of the two) for the prophylaxis of episodic migraine in adults. Cochrane Database Syst. Rev. 2013, CD010611. [Google Scholar] [CrossRef]
- Hakami, T. Efficacy and tolerability of antiseizure drugs. Ther. Adv. Neurol. Disord. 2021, 14, 17562864211037430. [Google Scholar] [CrossRef] [PubMed]
- Rheims, S.; Ryvlin, P. Patients’ safety in the epilepsy monitoring unit: Time for revising practices. Curr. Opin. Neurol. 2014, 27, 213–218. [Google Scholar] [CrossRef] [PubMed]
- Callenbach, P.M.C.; Arts, W.F.M.; ten Houten, R.; Augustijn, P.; Gunning, W.B.; Peeters, E.A.J.; Weber, A.M.; Stroink, H.; Geerts, Y.; Geerts, A.T.; et al. Add-on levetiracetam in children and adolescents with refractory epilepsy: Results of an open-label multi-centre study. Eur. J. Paediatr. Neurol. EJPN Off. J. Eur. Paediatr. Neurol. Soc. 2008, 12, 321–327. [Google Scholar] [CrossRef] [PubMed]
- Goldberg-Stern, H.; Feldman, L.; Eidlitz-Markus, T.; Kramer, U.; Perez, S.; Pollak, L.; Phatal-Valevski, A. Levetiracetam in children, adolescents and young adults with intractable epilepsy: Efficacy, tolerability and effect on electroencephalogram--a pilot study. Eur. J. Paediatr. Neurol. EJPN Off. J. Eur. Paediatr. Neurol. Soc. 2013, 17, 248–253. [Google Scholar] [CrossRef] [PubMed]
- Verrotti, A.; Prezioso, G.; Di Sabatino, F.; Franco, V.; Chiarelli, F.; Zaccara, G. The adverse event profile of levetiracetam: A meta-analysis on children and adults. Seizure 2015, 31, 49–55. [Google Scholar] [CrossRef]
- Mula, M. Pharmacological treatment of focal epilepsy in adults: An evidence based approach. Expert Opin. Pharmacother. 2021, 22, 317–323. [Google Scholar] [CrossRef]
- Marson, A.G.; Al-Kharusi, A.M.; Alwaidh, M.; Appleton, R.; Baker, G.A.; Chadwick, D.W.; Cramp, C.; Cockerell, O.C.; Cooper, P.N.; Doughty, J.; et al. The SANAD study of effectiveness of valproate, lamotrigine, or topiramate for generalised and unclassifiable epilepsy: An unblinded randomised controlled trial. Lancet 2007, 369, 1016–1026. [Google Scholar] [CrossRef]
- Frey, N.; Bodmer, M.; Bircher, A.; Rüegg, S.; Jick, S.S.; Meier, C.R.; Spoendlin, J. The risk of Stevens-Johnson syndrome and toxic epidermal necrolysis in new users of antiepileptic drugs. Epilepsia 2017, 58, 2178–2185. [Google Scholar] [CrossRef]
- Mustafa, S.S.; Ostrov, D.; Yerly, D. Severe Cutaneous Adverse Drug Reactions: Presentation, Risk Factors, and Management. Curr. Allergy Asthma Rep. 2018, 18, 26. [Google Scholar] [CrossRef]
- Jacob, L.; Hamer, H.M.; Kostev, K. Adherence to antiepileptic drugs in children and adolescents: A retrospective study in primary care settings in Germany. Epilepsy Behav. 2017, 75, 36–41. [Google Scholar] [CrossRef]
- Shetty, J.; Greene, S.A.; Mesalles-Naranjo, O.; Kirkpatrick, M. Adherence to antiepileptic drugs in children with epilepsy in a Scottish population cohort. Dev. Med. Child Neurol. 2016, 58, 469–474. [Google Scholar] [CrossRef]
- Ge, P.; Liu, S.-T.; Xu, S.-X.; Zhang, J.-Z.; Lai, Y.-J.; Fu, R.-C.; Ke, X.-Y.; Zhao, J.; Bian, Y.; Wu, Y.-B. The Influence of Parents on Medication Adherence of Their Children in China: A Cross-Sectional Online Investigation Based on Health Belief Model. Front. Public Health 2022, 10, 845032. [Google Scholar] [CrossRef]
- Sommer, B.R.; Fenn, H.H. Review of topiramate for the treatment of epilepsy in elderly patients. Clin. Interv. Aging 2010, 5, 89–99. [Google Scholar] [CrossRef]
- Lippa, C.F.; Rosso, A.; Hepler, M.; Jenssen, S.; Pillai, J.; Irwin, D. Levetiracetam: A practical option for seizure management in elderly patients with cognitive impairment. Am. J. Alzheimers Dis. Other Demen. 2010, 25, 149–154. [Google Scholar] [CrossRef]
- Tomson, T.; Battino, D.; Bonizzoni, E.; Craig, J.; Lindhout, D.; Sabers, A.; Perucca, E.; Vajda, F. Dose-dependent risk of malformations with antiepileptic drugs: An analysis of data from the EURAP epilepsy and pregnancy registry. Lancet Neurol. 2011, 10, 609–617. [Google Scholar] [CrossRef]
- Tomson, T.; Battino, D.; Bonizzoni, E.; Craig, J.; Lindhout, D.; Perucca, E.; Sabers, A.; Thomas, S.V.; Vajda, F. Comparative risk of major congenital malformations with eight different antiepileptic drugs: A prospective cohort study of the EURAP registry. Lancet Neurol. 2018, 17, 530–538. [Google Scholar] [CrossRef]
- Tomson, T.; Battino, D.; Bonizzoni, E.; Craig, J.; Lindhout, D.; Perucca, E.; Sabers, A.; Thomas, S.V.; Vajda, F. Declining malformation rates with changed antiepileptic drug prescribing: An observational study. Neurology 2019, 93, e831–e840. [Google Scholar] [CrossRef]
- Grunze, A.; Amann, B.L.; Grunze, H. Efficacy of Carbamazepine and Its Derivatives in the Treatment of Bipolar Disorder. Medicina 2021, 57, 433. [Google Scholar] [CrossRef]
- Aldaz, A.; Ferriols, R.; Aumente, D.; Calvo, M.V.; Farre, M.R.; García, B.; Marqués, R.; Mas, P.; Porta, B.; Outeda, M.; et al. Pharmacokinetic monitoring of antiepileptic drugs. Farm. Hosp. Organo Of. Expr. Cient. Soc. Esp. Farm. Hosp. 2011, 35, 326–339. [Google Scholar] [CrossRef]
 ) indicates under-range dosage, blue (🟦) in range, orange (🟧) over-range, and red (🟥) toxic levels. VPA, LEV, OxCBZ, ESM, and PB intervals are 5 μg/mL; PHT intervals are 2 μg/mL; CBZ, LTG, TPM, and LCS intervals are 1 μg/mL.
) indicates under-range dosage, blue (🟦) in range, orange (🟧) over-range, and red (🟥) toxic levels. VPA, LEV, OxCBZ, ESM, and PB intervals are 5 μg/mL; PHT intervals are 2 μg/mL; CBZ, LTG, TPM, and LCS intervals are 1 μg/mL.
 ) indicates under-range dosage, blue (🟦) in range, orange (🟧) over-range, and red (🟥) toxic levels. VPA, LEV, OxCBZ, ESM, and PB intervals are 5 μg/mL; PHT intervals are 2 μg/mL; CBZ, LTG, TPM, and LCS intervals are 1 μg/mL.
) indicates under-range dosage, blue (🟦) in range, orange (🟧) over-range, and red (🟥) toxic levels. VPA, LEV, OxCBZ, ESM, and PB intervals are 5 μg/mL; PHT intervals are 2 μg/mL; CBZ, LTG, TPM, and LCS intervals are 1 μg/mL.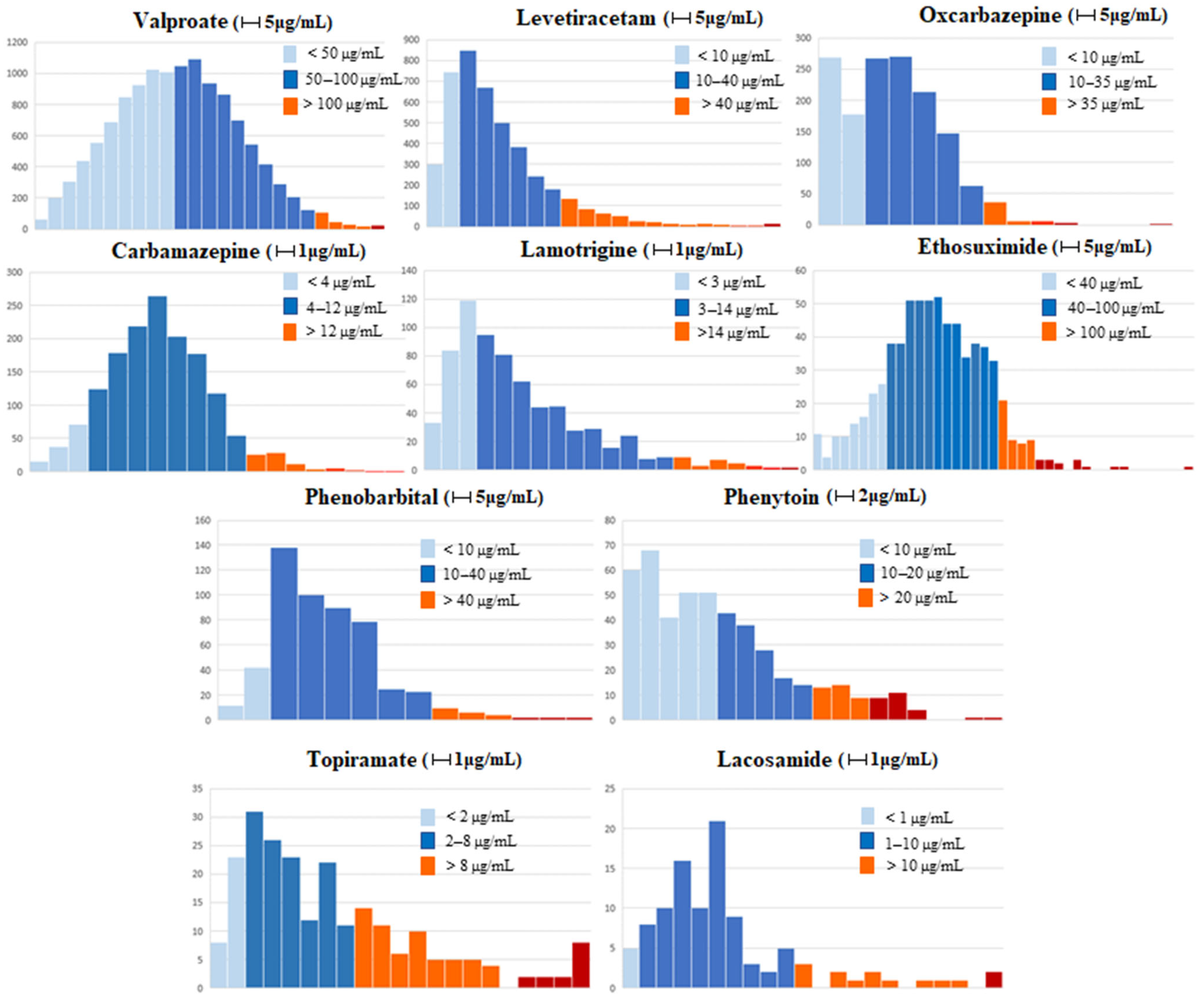
| ASM (Reference Range) | C(p) (Mean) | In Range | Under-Range | Over-Range |
|---|---|---|---|---|
| Valproate (50–100 μg/mL) | 51.3 ± 22.2 | 49.8% | 48.4% | 1.8% |
| Levetiracetam (10–40 μg/mL) | 21.2 ± 16.3 | 65.5% | 23.7% | 10.8% |
| Oxcarbazepine (10–35 μg/mL) | 16.3 ± 10.6 | 68.5% | 27.6% | 3.9% |
| Carbamazepine (4–12 μg/mL) | 7.14 ± 2.67 | 76.4% | 17.9% | 3.7% |
| Lamotrigine (3–14 μg/mL) | 5.4 ± 3.9 | 64.1% | 32.8% | 4.4% |
| Ethosuximide (40–100 μg/mL) | 65.8 ± 27.6 | 74.3% | 16.6% | 9% |
| Phenobarbital (10–40 μg/mL) | 20.5 ± 10.5 | 85.6% | 9.5% | 4.9% |
| Phenytoin (10–20 μg/mL) | 10.3 ± 7.8 | 56.7% | 30.2% | 13.1% |
| Topiramate (2–8 μg/mL) | 7.6 ± 9.4 | 55.2% | 12.6% | 32.2% |
| Lacosamide (1–10 μg/mL) | 6.6 ± 4.4 | 85.1% | 0% | 13.9% |
| ASM (Reference Range) | Female Mean Age | Male Mean Age | Females Mean C(p) | Males Mean C(p) |
|---|---|---|---|---|
| Valproate (50–100 μg/mL) | 48.9 ± 23.6 (2236) | 40.2 ± 22.5 * (2714) | 51.7 ± 22.6 | 51.05 ± 21.9 |
| Levetiracetam (10–40 μg/mL) | 62.2 ± 22.1 (946) | 60.1 ± 20.7 * (880) | 22.9 ± 18 | 19.5 ± 14.2 § |
| Oxcarbazepine (10–35 μg/mL) | 44.6 ± 19.5 (190) | 49.3 ± 20.1 * (134) | 15.6 ± 10.7 | 17.2 ± 10.3 § |
| Carbamazepine (4–12 μg/mL) | 40.5 ± 24.2 (357) | 38.9 ± 24 (362) | 6.97 ± 2.6 | 7.3 ± 2.8 § |
| Lamotrigine (3–14 μg/mL) | 39.6 ± 19.7 (211) | 48.2 ± 22.9 * (99) | 5.4 ± 3.5 | 5.5 ± 4.7 |
| Ethosuximide (40–100 μg/mL) | 14.4 ± 9.8 (109) | 13.9 ± 9.7 (93) | 67.4 ± 28.7 | 64 ± 26.2 |
| Phenobarbital (10–40 μg/mL) | 36.7 ± 32.2 (108) | 46.4 ± 27.2 * (119) | 19.8 ± 9.4 | 21 ± 11.1 |
| Phenytoin (10–20 μg/mL) | 61 ± 25.5 (89) | 59.2 ± 22.9 (105) | 9.9 ± 7.9 | 10.5 ± 7.8 |
| Topiramate (2–8 μg/mL) | 47.8 ± 17.5 (60) | 44.8 ± 14.4 (52) | 7.9 ± 9.8 | 7.2 ± 8.9 |
| Lacosamide (1–10 μg/mL) | 56.9 ± 18.1 (37) | 49 ± 16.8 * (33) | 7.2 ± 5.6 | 6.1 ± 2.9 |
| ASM (Reference Range) | Psychiatry Unit Mean C(p) | Neurology Unit Mean C(p) | Child Neuropsy Unit Mean C(p) |
|---|---|---|---|
| Valproate (50–100 μg/mL) | 51 ± 21.2 (5191) | 45 ± 22.4 * (240) | 60.9 ± 20.6 *, ** (2627) |
| Oxcarbazepine (10–35 μg/mL) | 13.7 ± 8.1 (320) | 21.3 ± 13 * (27) | 18 ± 11.6 * (123) |
| Carbamazepine (4–12 μg/mL) | 6.6 ± 2.6 (182) | 9.1 ± 3.8 * (30) | 7.1 ± 2.5 ** (474) |
| Lamotrigine (3–14 μg/mL) | 2.5 ± 1.7 (12) | 4.7 ± 4.8 (26) | 5.3 ± 3.5 * (59) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Biso, L.; Carli, M.; Kolachalam, S.; Monticelli, G.; Calabrò, P.F.; di Paolo, A.; Giorgi, F.S.; Bocci, G.; Scarselli, M. A 5-Year Study of Antiseizure Medications (ASMs) Monitoring in Patients with Neuropsychiatric Disorders in an Italian Clinical Center. Pharmaceuticals 2023, 16, 945. https://doi.org/10.3390/ph16070945
Biso L, Carli M, Kolachalam S, Monticelli G, Calabrò PF, di Paolo A, Giorgi FS, Bocci G, Scarselli M. A 5-Year Study of Antiseizure Medications (ASMs) Monitoring in Patients with Neuropsychiatric Disorders in an Italian Clinical Center. Pharmaceuticals. 2023; 16(7):945. https://doi.org/10.3390/ph16070945
Chicago/Turabian StyleBiso, Letizia, Marco Carli, Shivakumar Kolachalam, Giorgio Monticelli, Pasquale Fabio Calabrò, Antonello di Paolo, Filippo Sean Giorgi, Guido Bocci, and Marco Scarselli. 2023. "A 5-Year Study of Antiseizure Medications (ASMs) Monitoring in Patients with Neuropsychiatric Disorders in an Italian Clinical Center" Pharmaceuticals 16, no. 7: 945. https://doi.org/10.3390/ph16070945
APA StyleBiso, L., Carli, M., Kolachalam, S., Monticelli, G., Calabrò, P. F., di Paolo, A., Giorgi, F. S., Bocci, G., & Scarselli, M. (2023). A 5-Year Study of Antiseizure Medications (ASMs) Monitoring in Patients with Neuropsychiatric Disorders in an Italian Clinical Center. Pharmaceuticals, 16(7), 945. https://doi.org/10.3390/ph16070945







