Characterization of Potential Intoxications with Medicines in a Regional Setting
Abstract
1. Introduction
2. Results
2.1. Calls Received by CIAV: Number, Type of Consultant and Call Origin
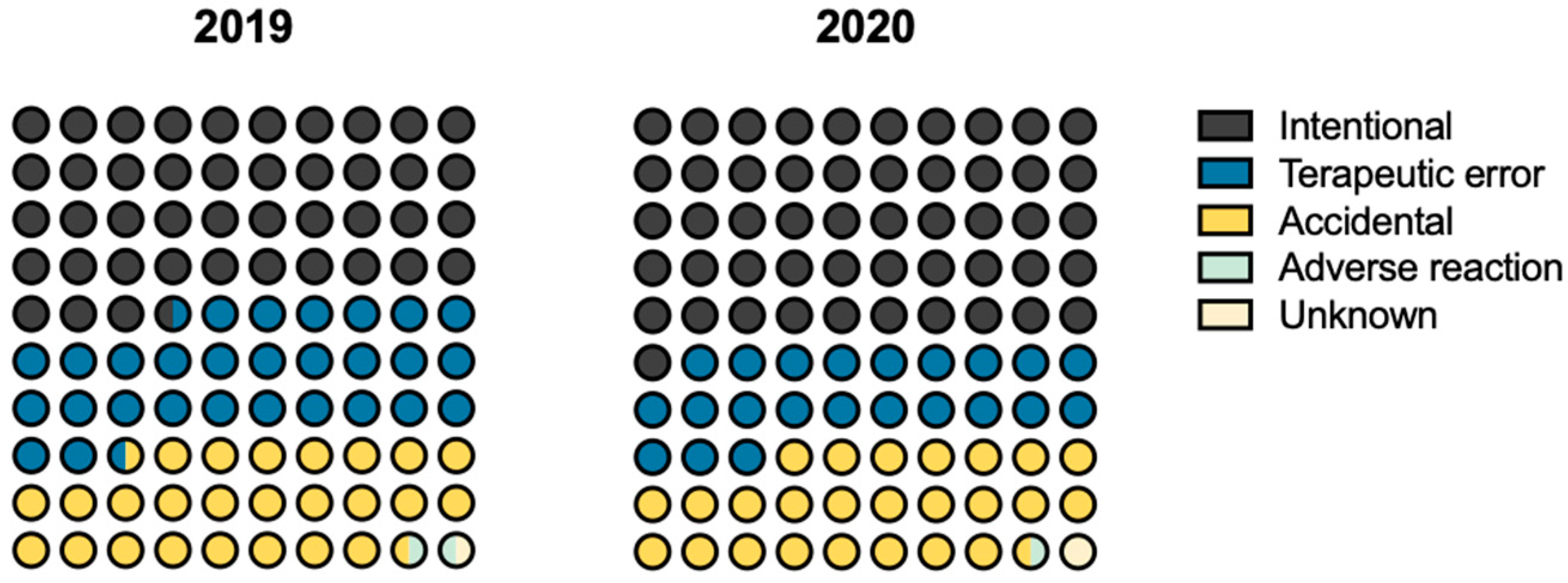
2.2. Characterisation of Intoxications
2.3. Pharmacotherapeutic Groups and Drugs Involved
3. Discussion
4. Materials and Methods
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Eddleston, M. Patterns and problems of deliberate self-poisoning in the developing world. QJM Int. J. Med. 2000, 93, 715–731. [Google Scholar] [CrossRef] [PubMed]
- Smith, S.W.; Farmer, B.M. Toxicology in the Service of Patient and Medication Safety: A Selected Glance at Past and Present Innovations. J. Med. Toxicol. 2015, 11, 245. [Google Scholar] [CrossRef] [PubMed]
- Gokalp, G. Evaluation of poisoning cases admitted to pediatric emergency department. Int. J. Pediatr. Adolesc. Med. 2019, 6, 109–114. [Google Scholar] [CrossRef] [PubMed]
- Albano, G.D.; Malta, G.; La Spina, C.; Rifiorito, A.; Provenzano, V.; Triolo, V.; Vaiano, F.; Bertol, E.; Zerbo, S.; Argo, A. Toxicological Findings of Self-Poisoning Suicidal Deaths: A Systematic Review by Countries. Toxics 2022, 10, 654. [Google Scholar] [CrossRef]
- Piccioni, A.; Cicchinelli, S.; Saviano, L.; Gilardi, E.; Zanza, C.; Brigida, M.; Tullo, G.; Volonnino, G.; Covino, M.; Franceschi, F.; et al. Risk Management in First Aid for Acute Drug Intoxication. Int. J. Environ. Res. Public Health 2020, 17, 8021. [Google Scholar] [CrossRef] [PubMed]
- European Monitoring Centre for Drugs and Drug Addiction. Update from the EMCDDA Expert Network Drug-Related Deaths and Mortality in Europe; EMCDDA: Luxembourg, 2019. [Google Scholar]
- CIAV—Centro de Informação Antivenenos. Available online: https://www.inem.pt/category/servicos/centro-de-informacao-antivenenos/ (accessed on 26 December 2022).
- European Monitoring Centre for Drugs and Drug Addiction. Drug-Related Deaths and Mortality in Europe: Update from the EMCDDA Expert Network; EMCDDA: Lisbon, Portugal, 2021. [Google Scholar] [CrossRef]
- Bian, W.; Zhu, N.; Han, D.; Gu, F.; Hu, Y. Analysis of Influencing Factors of Acute Medication Poisoning in Adults in Emergency Department of Our Hospital from 2016 to 2019 and Observation of Curative Effect of Optimizing Emergency Procedures. Evid. Based Complement. Altern. Med. 2021, 2021, 5265804. [Google Scholar] [CrossRef]
- Gummin, D.D.; Mowry, J.B.; Beuhler, M.C.; Spyker, D.A.; Rivers, L.J.; Feldman, R.; Brown, K.; Nathaniel, P.T.P.; Bronstein, A.C.; Weber, J.A. 2021 Annual Report of the National Poison Data System© (NPDS) from America’s Poison Centers: 39th Annual Report. Clin. Toxicol. 2022, 60, 1381–1643. [Google Scholar] [CrossRef]
- Hernández-Calle, D.; Martínez-Alés, G.; López-Cuadrado, T. Suicidal and accidental drug poisoning mortality among older adults and working-age individuals in Spain between 2000 and 2018. BMC Geriatr. 2022, 22, 1–10. [Google Scholar] [CrossRef]
- Martins, S.S.; Sampson, L.; Cerdá, M.; Galea, S. Worldwide Prevalence and Trends in Unintentional Drug Overdose: A Systematic Review of the Literature. Am. J. Public Health 2015, 105, e29–e49. [Google Scholar] [CrossRef]
- Cucinotta, D.; Vanelli, M. WHO declares COVID-19 a pandemic. Acta Biomed. 2020, 91, 157–160. [Google Scholar] [CrossRef]
- Guengerich, F.P. Mechanisms of Drug Toxicity and Relevance to Pharmaceutical Development. Drug Metab. Pharm. 2011, 26, 3–14. [Google Scholar] [CrossRef] [PubMed]
- Instituto Nacional de Estatística-Statistics Portugal. Censos 2021. Available online: https://censos.ine.pt/xportal/xmain?xpgid=censos21_main&xpid=CENSOS21&xlang=pt (accessed on 26 December 2022).
- Serviço Nacional de Saúde. Relatório Anual Atividades Específicas Desenvolvidas nos Centros de Orientação de Doentes Urgentes (CODU)-2020. 2021. Available online: https://www.inem.pt/wp-content/uploads/2021/04/Relatorio-de-Atividades-Especificas-CODU-2020.pdf (accessed on 26 December 2022).
- GDS Covid-19 Country Reports|Global Drug Survey. 2020. Available online: https://www.globaldrugsurvey.com/wp-content/themes/globaldrugsurvey/assets/GDS_COVID-19-GLOBAL_Interim_Report-2020.pdf (accessed on 26 December 2022).
- Hardon, A.; Hodgkin, C.; Fresle, D. How to Investigate the Use of Medicines by Consumers; World Health Organization: Geneva, Switzerland, 2004. [Google Scholar]
- Centro de Informação Antivenenos. Centro de Informação Antivenenos-Dados Estatísticos 2021. 2021. Available online: https://www.inem.pt/wp-content/uploads/2022/03/Boletim-CIAV_Ano-2021.pdf (accessed on 26 December 2022).
- Santana, R.; Rocha, J.; Sousa, J.; Soares, P. A Procura de Serviços de Urgência/Emergência hospitlar: Tendênias durnte o primeiro mês de reposta à COVID-19. 2021. Available online: https://www.ensp.unl.pt/wp-content/uploads/2017/06/tendencia-de-resposta-dos-servicos-de-urg-emerg-covid-19.pdf (accessed on 26 December 2022).
- Entidade Reguladora da Saúde. Informação de Monitorização-Impacto da pandemia COVID-19 no Sistema de Saúde—Período de Março a Junho de 2020, Porto. 2020. Available online: https://transparencia.sns.gov.pt (accessed on 26 December 2022).
- Ministério da Saúde. SNS 24. Available online: https://www.sns24.gov.pt/ (accessed on 26 December 2022).
- Gummin, D.D.; Mowry, J.B.; Beuhler, M.C.; Spyker, D.A.; Brooks, D.E.; Dibert, K.W.; Rivers, L.J.; Pham, N.P.T.; Ryan, M.L. 2019 Annual Report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 37th Annual Report. Clin. Toxicol. 2020, 58, 1360–1541. [Google Scholar] [CrossRef] [PubMed]
- Gummin, D.D.; Mowry, J.B.; Beuhler, M.C.; Spyker, D.A.; Bronstein, A.C.; Rivers, L.J.; Pham, N.P.T.; Weber, J. 2020 Annual Report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 38th Annual Report. Clin. Toxicol. 2021, 59, 1282–1501. [Google Scholar] [CrossRef] [PubMed]
- Kovess-Masfety, V.; Boyd, A.; Van de Velde, S.; De Graaf, R.; Vilagut, G.; Haro, J.M.; Florescu, S.; O’Neill, S.; Weinberg, L.; Alonso, J.; et al. Are there gender differences in service use for mental disorders across countries in the European Union? Results from the EU-World Mental Health survey. J. Epidemiol. Commun. Health 2014, 68, 649–656. [Google Scholar] [CrossRef]
- Bertakis, K.D.; Azari, R.; Helms, L.J.; Callahan, E.J.; Robbins, J.A. Gender differences in the utilization of health care services. J. Fam. Pract. 2000, 49, 147–152. [Google Scholar]
- Fundação Francisco Manuel dos Santos and PORDATA-Estatísticas Sobre Portugal e Europa. Portugal: População Residente, Média Anual: Total e Por Grupo Etário|Pordata. Available online: https://www.pordata.pt/portugal/populacao+residente++media+anual+total+e+por+grupo+etario-10 (accessed on 26 December 2022).
- Alves, E.E.; Brandão, P.; Magalhães, T.; Carvalho, F.; Dinis-Oliveira, R.J. Fatal Intoxications in the North of Portugal: 12 Years of Retrospective Analysis. Curr. Drug Saf. 2017, 12, 39–45. [Google Scholar] [CrossRef]
- Blaiss, M.S.; Deshazo, R.D. Drug Allergy. Pediatr. Clin. N. Am. 1988, 35, 1131–1147. [Google Scholar] [CrossRef]
- Sammons, H.M.; Choonara, I. Learning Lessons from Adverse Drug Reactions in Children. Children 2016, 3, 1. [Google Scholar] [CrossRef]
- Safe Kids Worldwide. Safe Storage, Safe Dosing, Safe Kids A Report to the Nation on Safe Medication, Washington, D.C. 2012. Available online: https://www.safekids.org/sites/default/files/documents/ResearchReports/medicine-safety-study-2012.pdf (accessed on 26 December 2022).
- Jerónimo, M.; Piñar, S.; Samos, P.; González, A.M.; Bellsolà, M.; Sabaté, A.; León, J.; Aliart, X.; Martín, L.M.; Aceña, R.; et al. Intentos e ideas de suicidio durante la pandemia por COVID-19 en comparación con los años previos. Rev. de Psiquiatr. y Salud Ment. 2021; in press. [Google Scholar] [CrossRef]
- Kim, J.; de Jesus, O. Medication Routes of Administration; StatPearls: Tampa, FL, USA, 2022. Available online: https://www.ncbi.nlm.nih.gov/books/NBK568677/ (accessed on 26 December 2022).
- Olsen, S.J.; Winn, A.K.; Budd, A.P.; Prill, M.M.; Steel, J.; Midgley, C.M.; Kniss, K.; Burns, E.; Rowe, T.; Foust, A.; et al. Changes in Influenza and Other Respiratory Virus Activity During the COVID-19 Pandemic—United States, 2020–2021. MMWR Morb. Mortal. Wkly. Rep. 2021, 70, 1013–1019. [Google Scholar] [CrossRef]
- Bellmann, R.; Joannidis, M. Vergiftungen mit psychotropen Substanzen. Med. Klin. Intensiv. Notf. 2017, 112, 557–575. [Google Scholar] [CrossRef]
- Furtado, C. Psicofármacos: Evolução do Consumo em Portugal Continental (2000-2012); Cláudia, F., Ed.; Gabinete de Estudos e Projectos: Almeirim, Portugal, 2013. [Google Scholar]
- Furtado, C.; Fernandes, E. Evolução da pandemia em Portugal: Psicofármacos na última década em Portugal. Infarmed Notícias 2020, 71, 26–29. [Google Scholar]
- Estrela, M.; Herdeiro, M.T.; Ferreira, P.L.; Roque, F. The Use of Antidepressants, Anxiolytics, Sedatives and Hypnotics in Europe: Focusing on Mental Health Care in Portugal and Prescribing in Older Patients. Int. J. Environ. Res. Public Health 2020, 17, 8612. [Google Scholar] [CrossRef] [PubMed]
- Ferreira, R.; Cunha, B.; Ferreira, D.M.; Devesa, N.; Pimentel, J. Intoxicações Agudas num Serviço de Medicina Intensiva: Anos 2002 a 2014. Med. Interna-Rev. Soc. Port. Med. Interna 2016, 23, 3. [Google Scholar]
- Prado, D.M.L.D.; Silvino, V.O.; Vieira, E.G.; Rosa, B.V.; e Silva, A.S.V.; dos Santos, M.A.P. O Efeito da Máscara Cirúrgica de Proteção Respiratória nos Marcadores Fisiológicos de Desempenho Aeróbio em um Corredor Recreacional. Arq. Bras. de Cardiol. 2021, 117, 23–28. [Google Scholar] [CrossRef]
- Paiva, J.A.; Lebre, A.; Silva, M.G.; Valente, M.; Pacheco, P. Infeções e Resistências a Antimicrobianos-Relatório do Programa Prioritário PPCIRA 2021. Available online: https://www.dgs.pt/programa-nacional-de-controlo-da-infeccao/relatorios/infecoes-e-resistencias-aos-antimicrobianos-2021-relatorio-anual-do-programa-prioritario-pdf.aspx (accessed on 26 December 2022).
- Infarmed. Medicamentos Não Sujeitos a Receita Médica (MNSRM)-Monitorização das Vendas fora das Farmácia (Jan-Dez 2020); Infarmed: Lisboa, Portugal, 2021. [Google Scholar]
- United Nations and International Narcotics Control Board. Psychotropic Substances-2021. Statistics for 2020. Assessments of Annual Medical and Scientific Requirements for 2022; United Nations Publications: Vienna, Austria, 2022; Available online: www.incb.org (accessed on 26 December 2022).
- Bouchette, D.; Akhondi, H.; Quick, J. Zolpidem; StatPearls: Tampa, FL, USA, 2022; pp. 1–5. [Google Scholar] [CrossRef]
- Liu, K.; Chen, Y.; Wu, D.; Lin, R.; Wang, Z.; Pan, L. Effects of progressive muscle relaxation on anxiety and sleep quality in patients with COVID-19. Complement. Ther. Clin. Prac. 2020, 39, 101132. [Google Scholar] [CrossRef]
- Rismanbaf, A.; Zarei, S. Liver and Kidney Injuries in COVID-19 and Their Effects on Drug Therapy; a Letter to Editor. Arch. Acad. Emerg. Med. 2020, 8, e17. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7075271/ (accessed on 26 December 2022).
- Santi, P. Coronavirus: Pourquoi l’ibuprofène est Déconseillé. Available online: https://www.lemonde.fr/planete/article/2020/03/16/coronavirus-mise-en-garde-contre-l-ibuprofene_6033233_3244.html (accessed on 26 December 2022).
- Moore, N.; Carleton, B.; Blin, P.; Bosco-Levy, P.; Droz, C. Does Ibuprofen Worsen COVID-19? Drug Saf. 2020, 43, 611–614. [Google Scholar] [CrossRef]
- Sridharan, G.K.; Kotagiri, R.; Chandiramani, V.H.; Mohan, B.P.; Vegunta, R.; Vegunta, R.; Rokkam, V.R.P. COVID-19 and Avoiding Ibuprofen. How Good Is the Evidence? Am. J. Ther. 2020, 27, e400–e402. [Google Scholar] [CrossRef]
- Poutoglidou, F.; Saitis, A.; Kouvelas, D. Ibuprofen and COVID-19 disease: Separating the myths from facts. Expert Rev. Respir. Med. 2021, 15, 979–983. [Google Scholar] [CrossRef]
- Infarmed. Monitorização do Consumo de Medicamentos-Meio ambulatório. Janeiro-Dezembro 2021; Infarmed: Lisboa, Portugal, 2022; Available online: https://www.infarmed.pt/documents/15786/4373142/dezembro/10c6aafe-bdf6-7601-9cf3-9e190f801531?version=1.0 (accessed on 26 December 2022).
- Prontuário Terapêutico. Infarmed-Autoridade Nacional do Medicamento e Produtos de Saúde. Available online: https://app10.infarmed.pt/prontuario/index.php (accessed on 26 December 2022).





| Rank | n | 2019 | n | 2020 |
|---|---|---|---|---|
| 1 | 71 | Paracetamol | 63 | Paracetamol |
| 2 | 59 | Ibuprofen | 55 | Diazepam |
| 3 | 42 | Clonazepam | 47 | Quetiapine |
| 4 | 40 | Alprazolam | 38 | Alprazolam |
| 5 | 39 | Quetiapine | 29 | Clonazepam |
| 6 | 26 | Mexazolam | 28 | Ibuprofen |
| 7 | 26 | Diazepam | 28 | Bromazepam |
| 8 | 25 | Zolpidem | 28 | Lorazepam |
| 9 | 23 | Escitalopram | 25 | Sertraline |
| 10 | 22 | Lorazepam | 23 | Olanzapine |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nascimento, T.; Santos, T.; Rato, F.; De Sousa-Coelho, A.L. Characterization of Potential Intoxications with Medicines in a Regional Setting. Pharmaceuticals 2023, 16, 308. https://doi.org/10.3390/ph16020308
Nascimento T, Santos T, Rato F, De Sousa-Coelho AL. Characterization of Potential Intoxications with Medicines in a Regional Setting. Pharmaceuticals. 2023; 16(2):308. https://doi.org/10.3390/ph16020308
Chicago/Turabian StyleNascimento, Tânia, Teresa Santos, Fátima Rato, and Ana Luísa De Sousa-Coelho. 2023. "Characterization of Potential Intoxications with Medicines in a Regional Setting" Pharmaceuticals 16, no. 2: 308. https://doi.org/10.3390/ph16020308
APA StyleNascimento, T., Santos, T., Rato, F., & De Sousa-Coelho, A. L. (2023). Characterization of Potential Intoxications with Medicines in a Regional Setting. Pharmaceuticals, 16(2), 308. https://doi.org/10.3390/ph16020308






