2.3. Analysis on the Factorial Design
Formula optimization on transethosomes was carried out with the aim of estimating the optimum formula based on the resulting response variables to serve as a reference for the formulation of the base for the active substance to be used. The formula optimization method used is the Response Surface Method (RSM). RSM is a collection of statistical and mathematical techniques that are useful for developing, improving, and optimizing processes in which the response is influenced by several factors (independent variables). In addition to generating mathematical models, SRM can also explain the effect of independent variables, which explain a process. The main idea of this method is to determine the effect of the independent variable on the response, to obtain a model of the relationship between the independent variable and the response, and to obtain the process conditions that produce the best response. The advantages of the RSM method include that it does not require large amounts of experimental data and does not take a long time.
The experimental design used in this study was a two-level factorial design. The two-level factorial design method can estimate the factors that have the most influence on the specified response value and the interaction between factors on the determined response value. In addition to studying the interaction between factors, the two-level factorial design provides less data than the three-level factorial design so that it can save time and materials for use in research [
33]. In this study, the factors used were phospholipids and tween 80, with the response variables in the form of particle size and polydispersity index, as it showed at
Table 1. Particle size and polydispersity index values of the resulting transethosomes are influenced by variations in phospholipid concentrations and tween 80 (
Table 2). Phospholipids serve as the main constituent components of vesicles. Phospholipids used in the form of Phospholipon, 90 G which contains phosphatidylcholine soybean granules of 94–102%.
Data processing using a two-level factorial design method with software Design Expert® 11 (trial version) was carried out to find the formula that produced the most optimum response value. The response values tested in this software are particle size and polydispersity index. The response value that is entered into this factorial design will later determine which factors have the most influence on the intended response value, as well as study the interactions between factors that affect the response value.
Analysis of variation was performed on each parameter of particle size (PSA) and polydispersity index (PDI). This factorial design can provide a significance value for each test parameter on the response results in each formula with ANOVA. p-value less than 0.05 indicates that these factors show a significant difference in effect on the response to each formula. This shows that the different formulas for phospholipids and tween 80 affect the values for PSA and PDI.
The results of the analysis of response data on particle size and the polydispersity index on design expert 11 software (trial version) resulted in a general equation of factorial design of the relationship between factors and responses according to the general equation Y = b0 + baXA + bbXB + babXAXb as follows:
Final Equation in Terms of Actual Factors:
Data analysis performed on Design Expert® 11 provides recommendations for formulas with the best phospholipid and tween 80 compositions, and can predict the value of each particle size parameter and polydispersity index that will be generated from the formula. This software will present the response value of particle size and polydispersity index for each formula in the form of a 3-dimensional response surface graph, contour plot and regression equation model. A contour plot is a graph that shows a 3-dimensional surface of a response from its 2-dimensional shape (contour plot). The 3-dimensional response surface graph and the contour graph depict the relationship between particle size response and polydiversities index to the concentration of phospholipids and tween 80 in each transethosomal formula. The graph of the contour plot of the response has several colors. This color gradient indicates the significance of the desired response starting from dark blue to red. The blue area shows the lowest percent response value, while the red area shows the highest response value.
The three-dimensional graph is a visualization of the general polynomial equation that helps in determining the optimum point of each variable used. This polynomial equation is only valid and suitable for predicting particle size. The three-dimensional graph is a visualization of the general polynomial equation that helps in determining the optimum point of each variable used. This polynomial equation is only valid for predicting particle size in the range of phospholipid concentrations of 3–5% w/w and tween 80 1.5–2.5% w/w. The color difference on the curve indicates a change in the response value to the particle size, due to changes in the combination of variables. The difference in height on the surface shows different response values for each combination of formulas. The blue color indicates the lowest particle size response value of 128.8 nm, while the yellow color indicates the highest particle size response value of 811.7 nm. The highest particle size was found in formula 3 with a phospholipid concentration of 5% w/w and tween 80 was 1.5% w/w, while the lowest particle size response was found in formula 1 with a phospholipid concentration of 3% w/w and tween 80 of 2.5% w/w.
This particle size response contour plot maps phospholipids on the 1× axis, tween 80 on the ×2 axis, and the particle size response value as a contour. The size response graph shows that the particle size value will increase if the concentration of phospholipids and tween 80 used approaches the red or orange colored area, because in the red region the particle value produced is the highest. On the x-axis, it can be seen that the higher the concentration of phospholipids contained in the formula, the larger the particle size that will be produced. In contrast to the y-axis, the greater the amount of tween 80 concentration contained in the formula, the smaller the particle size produced. The formula recommended by the Design Expert®11 software will be predicted to have a particle size value of 129.8 nm (<200nm).
In the range of phospholipid concentrations of 3–5% w/w and tween 80 1.5–2.5% w/w, the color difference on the curve indicates a change in the response value to the particle size. The difference in height on the surface shows different response values for each combination of formulas. The blue color indicates the lowest particle size response value of 128.8 nm, while the yellow color indicates the highest particle size response value of 811.7 nm. The highest particle size was found in formula 3 with a phospholipid concentration of 3% w/w and tween 80 was 2.5% w/w, while the lowest particle size response was found in formula 1 with a phospholipid concentration of 3% w/w and tween 80 of 1.5% w/w.
The most recommended formula by the response surface method has a composition of 3%
w/
w phospholipid concentration and 2.5%
w/
w tween 80 concentration. The formula is predicted to have a particle size of 139.3 nm and a polydispersity index of 0.226. The range of values that meet the requirements for particle size is less than 300 nm and polydispersity index is less than 0.5 [
37].
From the 3-dimensional response surface graph of the polydispersity index response, the equation model that describes the relationship between the polydispersity index and the concentration of phospholipids and tween 80 is a quadratic equation model that has a minimum polydispersity index value. The green color indicates the lowest polydispersity index response value, which is 0.019, while the red color indicates the highest polydispersity index response value, which is 0.594. The highest polydispersity index was found in formula 3, with a phospholipid concentration of 5% w/w and tween 80 of 1.5% w/w. The lowest polydispersity index response was also found in formula 2, with a phospholipid concentration of 3% w/w and tween 80 of 2.5% w/w.
This polydispersity index response graph depicts phospholipids on the
x-axis, tween 80 on the
y-axis, and the response value of the polydispersity index as a contour. The size response chart shows that the value of the polydispersity index will increase if the concentration of phospholipids and tween 80 used approaches the red area, because in the red area the polydispersity index value is the highest. On the
x-axis, it can be seen that the higher the phospholipid in the formula, the higher the polydispersity index. In contrast to the
y-axis, the greater the volume of tween 80, the smaller the polydispersity index. The formula recommended by the Design Expert
®11 software will be predicted to have a polydispersity index value of 0.019 as the lowest polydispersity index response that showed at
Figure 2. The polydispersity index is a condition in the distribution of particles that describes the level of uniformity of particle size in a component. The smaller the polydispersity index value, the more likely it is that the distribution of particles in a component has a good level of size uniformity [
38].
Design Expert® 11 provides the best formula solution based on the desirability value. The desirability value is the value of the optimization objective function, which indicates the program’s ability to fulfill the requirements based on the criteria set in the final product. The desirability value explains the close relationship, or not, a response value generated by the factor with the requirement value/ideal value. The desirability value has a range from 0–1. Where, the closer the desirability value is to a value of 1, the better the software’s ability to produce optimum formulas and meet the requirements. The actual purpose of optimization is not to be able to get a desirability value of 1, but to find the best conditions that consider all functions, factors, and responses.
In the criteria for the optimum acceptance of the transethosomal formula, the particle size value entered into the goal is the particle size value according to the requirements of the transethosomal preparation, which is less than 300 in the minimized category. In determining the optimum particle size value in the minimized category, the lower limit value of 100 is the lowest desired value and the upper limit value of 300 is the highest value that is still acceptable [
21]. If the particle size value is getting closer to 100, the closer the particle size value to the optimal result will be, which will affect the desirability value. Determination of the value of the requirement for the polydispersity index used the manimize category; because the requirement for the value is less than 0.5, if the value of the polydispersity index is closer to 0, the transethosomal preparation is more homogeneous and has higher physical stability.
After determining the requirements for the optimum particle size and polydispersity index in transethosomal preparations, Design Expert
® 11 provides the most optimum composition of phospholipid and tween 80 formulas based on the highest desirability value. The best value of particle size, polydispersity index and desirability are in the
Table 3.
Desirability indicates the possibility of obtaining a formula according to the desired criteria. Desirability is the optimization target value that can be achieved with a value range of 0–1. In the optimization of this formulation, the aim is to achieve the maximum desirability value by finding the best conditions that bring together all the test variables. The formula with the highest level of desirability will occupy the top position from the various suggestions offered. The higher the level of desirability, the closer the response results will be to the predicted value.
The
Table 3 provides four recommendations for the best formula for the composition of phospholipids and tween 80, which produce the most optimum polydispersity index and particle size.
This contour plot depicts the phospholipid factor on the x-axis, tween 80 on the y-axis, and the desirability value as a contour. The desirability value has a range of 0 to 1. If the response is closer to the blue contour, then the resulting response does not meet the satisfaction of the particle size criteria and the optimum polydispersity index because the desirability value is close to 0. If the response is getting closer to the red contour, the resulting response will be increasingly fulfilled by the satisfaction of the particle size criteria, and the optimum polydispersity index because it is close to the desirability value of 1.
The most recommended formula by the response surface method has a composition of 3% w/w phospholipid concentration and 2.5% w/w tween 80 concentration. The formula is predicted to have a particle size of 139.3 nm and a polydispersity index of 0.226. Based on the optimization results, the formula best meets the desired optimization target because it has the highest desirability value of 0.664 (selected row). Desirability of 0.664 means that this formula will produce a product that has characteristics that match the optimization target of 66.4%. Accepted desirability value must be higher than 0.6.
2.7. In Vitro Permeation of Catechin from the Transethosomal Gel
During the penetration test with the Franz diffusion cell, the receptor compartment of the device was kept at a temperature of 32 + 0.5 °C, which represents body temperature. The receptor compartment fluid was stirred with a magnetic stirrer at a speed of 600 rpm to simulate body conditions and ensure homogeneity. This velocity is used because it is considered a suitable velocity to homogenize the fluid in the receptor compartment. At speeds lower than 600 rpm it will be difficult to homogenize the fluid in the receptor compartment [
44].
In permease testing, drug levels will move from the donor compartment (high catechin concentration) to the receptor compartment which contains phosphate buffer medium pH 5.8. The receptor compartment has a large volume compared to the amount of substance that penetrates. This large volume aims to accommodate a large volume of liquid so as to create a sink condition. The sink condition is a condition where the volume of liquid to dissolve the substance is so large that it will not hinder drug penetration. This is because the large volume of fluid will not cause saturation in the receptor compartment. Drug penetration from the donor compartment to the receptor compartment is based on the principle of passive diffusion which uses the drug concentration gradient as the driving force for drug penetration.
Catechins that have left the gel preparation will be dissolved in the receptor fluid. Samples were taken of as much as 2 mL at 30, 90, 150, 210, 270, 330, 390, 450, 510, 570 min and 1, 2, 3, 4, 5, 6, 7, 8, 9, 10 h that determined the drug concentration in the receptor compartment. The sample taken from the receptor compartment is put into a vial as much as 2 mL, and each time the sample is taken it must be replaced with a new receptor fluid with the same volume to keep the volume of fluid in the receptor compartment constant, which is 20 mL. The drug concentration in the donor compartment will decrease and the drug concentration in the receptor compartment will rise to a steady state at a certain time and at a certain concentration. The absorption results obtained were entered into the regression equation and the concentration of the drug penetrated was obtained. Based on the concentration data, the cumulative amount and total flux can be calculated each time the drug is penetrated.
The cumulative results of catechin penetration through PTFE membranes for 10 h from non-transethosomal gel and transethosomal gel formulations and formulas were 112.741 ± 2.241 μg and 172.454 ± 5.287 μg, respectively. From
Figure 9, the cumulative graph of the transethosomal gel and non-transethosomal gel can be seen. The onset or peak time of the two gels was different; the transethosomal gel had a peak at 3 h, while the non-transethosomal gel had a peak at 5.5 h.
Furthermore, the cumulative amount of drug penetrated is plotted at each sampling time. The regression equation obtained from this cumulative amount shows the total flux of the penetrated drug.
The graph in
Figure 10 shows the rate or flow rate of catechins that are penetrated in each unit of time. It can be seen that the catechins that penetrated per unit time in both formulas showed a similar profile pattern from 0 to 10 h. However, there is a difference in the number of catechins penetrated.
The flux of drug through the membrane can be affected by its diffusion coefficient across the stratum corneum by interfering with the barrier system of the stratum corneum. To increase the drug flux across the skin membrane, penetration-enhancing compounds can be used [
45,
46].
According to the cumulative amount and drug flux data, gels with transethosomal carriers had higher flux values and permeability than gel preparations without transethosomes. This is because transethosomes have small particle sizes, contain phospholipids, ethanol, propylene glycol and surfactants that can help penetrate catechins from gel preparations into the skin.
The presence of ethanol as a penetration enhancer will help penetrate the transetosomal gel by increasing the fluidity of lipids in the stratum corneum and reducing the density of lipids in the skin. Therefore, the very soft transethosomal vesicles of the stratum corneum penetrate the structure of the stratum corneum and create a kind of drug absorption pathway in the skin. Phospholipids, as transethosomes, are also one of the factors that help penetrate catechins in the skin by merging with phospholipids in the bilayer membrane of the skin because they have a chemical structure similar to that based on the principle of like dissolves like. In addition, the addition of surfactant tween 80 can form vesicles that are ultra-deformable or more flexible through pores measuring 20–30 nm.
It can be concluded that the factors that can affect drug absorption through the skin are the viscosity of the preparation, the dissolution of a drug in the carrier, the diffusion of the dissolved drug from the carrier to the skin surface, and the penetration of the drug through the skin layer, especially the stratum corneum.
Determination of release kinetics aims to determine the mechanism of drug release from transdermal preparations. Determination of the release kinetics of the preparation of non-transethosomal gel preparations and transethosomal gels was carried out based on the value of the correlation coefficient (r2) through a linear equation according to the order. For zero order, the drug release kinetics is determined by plotting the time in hours against the permeation percentage, while for the first order drug release, kinetics is determined by plotting the time value in hours against the logarithm of the permeation percentage. Drug release kinetics of Higuchi model is determined by the root of the square of time to the cumulative percentage of permeation; then, for the Korsmeyer–Peppas model, drug release kinetics is determined by the logarithm of time to the logarithm of the cumulative percentage of permeation.
Based on the correlation coefficient values obtained from plotting the data on the graph, the dominant reaction order in the drug release kinetics can be determined. The most dominant reaction order is indicated by the correlation coefficient value closest to 1 (one). The correlation coefficient data from each preparation are as follows.
At
Table 5, both of TCG and NTCG showed that catechin release had Higuchi’s order The Higuchi’s order indicates that in the permeation process of catechins’ passive diffusion occurs and this is in accordance with the theory of transdermal delivery.
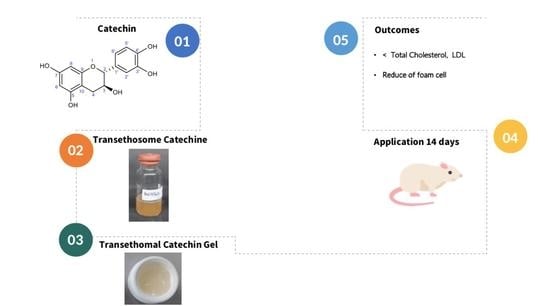
2.8. Result of Antihypercholesterol in Rats
TCG and NTCG preparations were applied to the shaved backs of rats, then covered with cellophane plaster (
Figure 11). Rats are test animals that are often used and are also suggested in research on the activity of active compounds [
47]. The results showed that induction of triton X-100 could increase cholesterol levels in groups of rats, except in the normal group. Hypercholesterol conditions absolutely must occur so that the effect of the treatment given to rats which aims to observe cholesterol reduction can be observed properly. It can be seen that there is a decrease in cholesterol in the parameters of total cholesterol and LDL in the group given oral simvastatin, TCG, and NTCG.
The measurement of total cholesterol was based on an enzymatic reaction using KIT CHOL (LabKit) due to the oxidation of free cholesterol by cholesterol oxidase to form peroxide compounds that affect the oxidative multiplication of phenol and 4-aminoantipyrine (4-AAP) to form a red quinoneimine dye. The chromophore group on the quinoneimine compound provides absorption when read on spectrophotometry, where the light intensity is proportional to the cholesterol concentration of the sample. The measurement results of total cholesterol levels can be seen in
Table 6.
Flavonoid compounds have antihypercholesterolemic activity, with their mechanism of action being the reduction of LDL in the body. Flavonoids can also increase the density of LDL receptors in the liver and bind to apolipoprotein B. Flavonoids can reduce cholesterol levels in the blood by inhibiting the work of the HMG Co-A reductase enzyme. The function of HMG Co-A reductase is an enzyme to convert HMG Co-A into mevalonate. Thus, if HMG Co-A reductase is inhibited then mevalonate is inhibited or cannot be formed. The mechanism of these flavonoids is similar to the mechanism of antihyperlipidemic drugs of the statin group or the HMG Co-A reductase inhibitor class [
48]. The flavonoid content that plays a major role in reducing triglyceride levels is catechin compounds [
49].
Catechins can regulate genes that can metabolize total cholesterol, so that a decrease in LDL levels in blood plasma a catechin effect on lipogenesis gene expression.
The percentage of cholesterol reduction on the two parameters in two weeks is shown in the
Figure 12. The positive group showed the largest cholesterol reduction percentage. The TGC group had a higher percentage reduction in total cholesterol and LDL than the NTCG group. Based on these results, it can be concluded that TCG preparations have the potential to be used as antihypercholesterolemia, especially in reducing total cholesterol and LDL. The addition of catechin transethosomes loaded into the gel is necessary to obtain better cholesterol and LDL reduction values. According to statistical calculations of significance between groups obtained, if
p < 0.05 then there was a significant difference. Therefore, it can be interpreted that in the total cholesterol results there was a significant difference between the normal group and the NTCG group and the normal group with the TCG group (
Table 7).
Transethosomes are a better type of UDV compared to the other two types because they contain the advantages possessed by transfersomes and ethosomes. Transethosomes have high ethanol content (30–40%) together with edge activator. The mechanism of skin penetration on transethosomes is a combination of transfersome and ethosomal mechanisms, and is rated higher in studies of vesicle elasticity and permeation through the skin so as to increase the amount of active substance that enters systemically [
50]. Ethanol is used as an efficient penetration enhancer in transethosomes because it has an interdigitating effect on the lipid bilayer and increases the fluidity of the stratum corneum lipids [
51,
52]. Edge activator can damage the transethosomal lipid bilayer and increase the flexibility of the preparation [
51,
53]. Edge activator can be a surfactant that can lower the interfacial tension and prevent particle aggregation that can occur during storage. Transetosomes can increase drug permeability in the skin to systemic, which can avoid first pass metabolism, controlled drug release, reduce drug side effects, increase pharmacological effects, avoid fluctuations in drug levels, and are comfortable to use so as to improve patient compliance [
40].