Self-Emulsifying Drug Delivery Systems (SEDDS): Measuring Energy Dynamics to Determine Thermodynamic and Kinetic Stability
Abstract
:1. Introduction
2. Results and Discussion
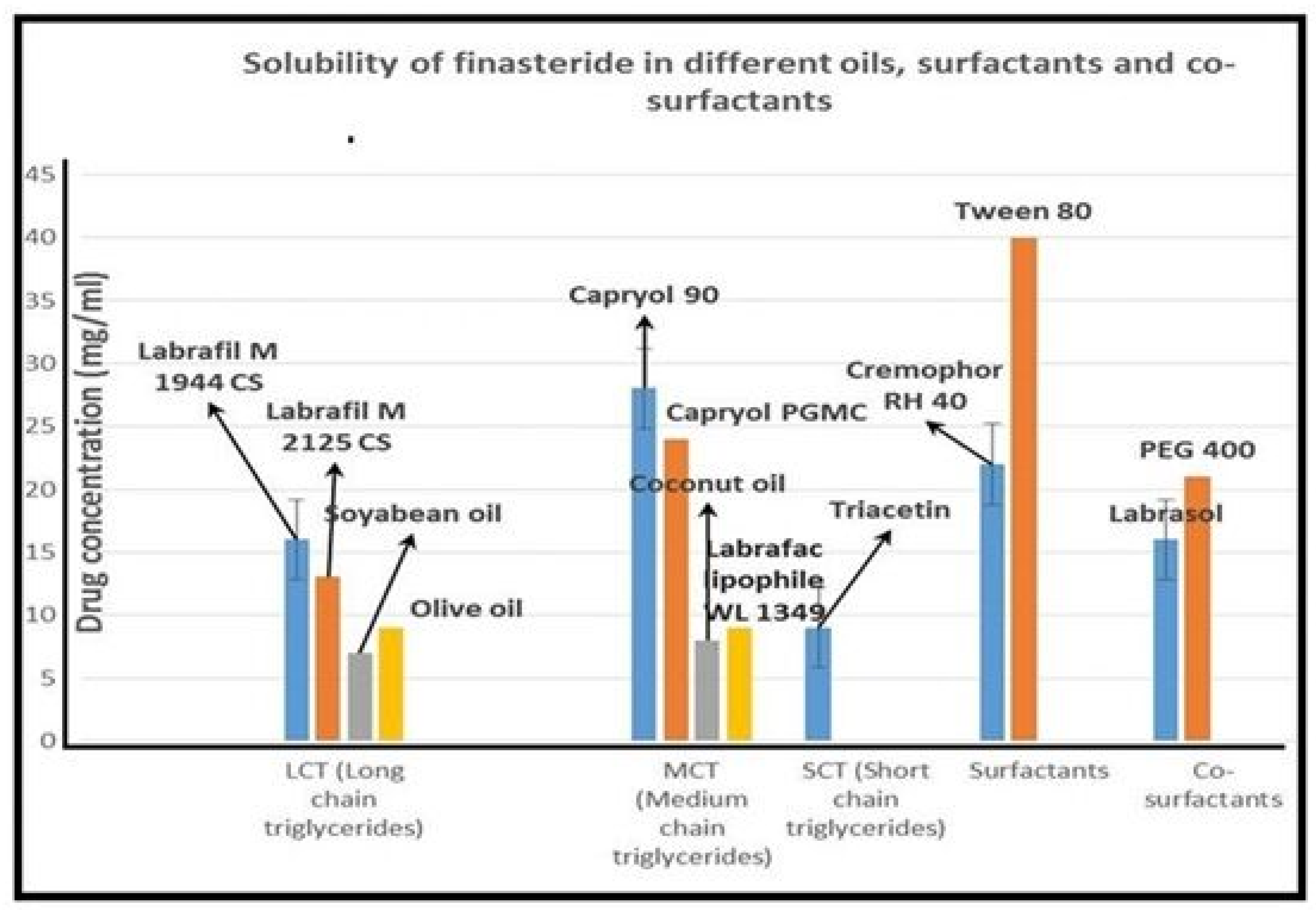
2.1. Selection of Oil, Surfactant and Cosurfactant
2.2. Ternary Phase Diagram and Features of SEDDS
2.3. Optimization of Finasteride SEDDS in Liquid Form (L-SEDDS)
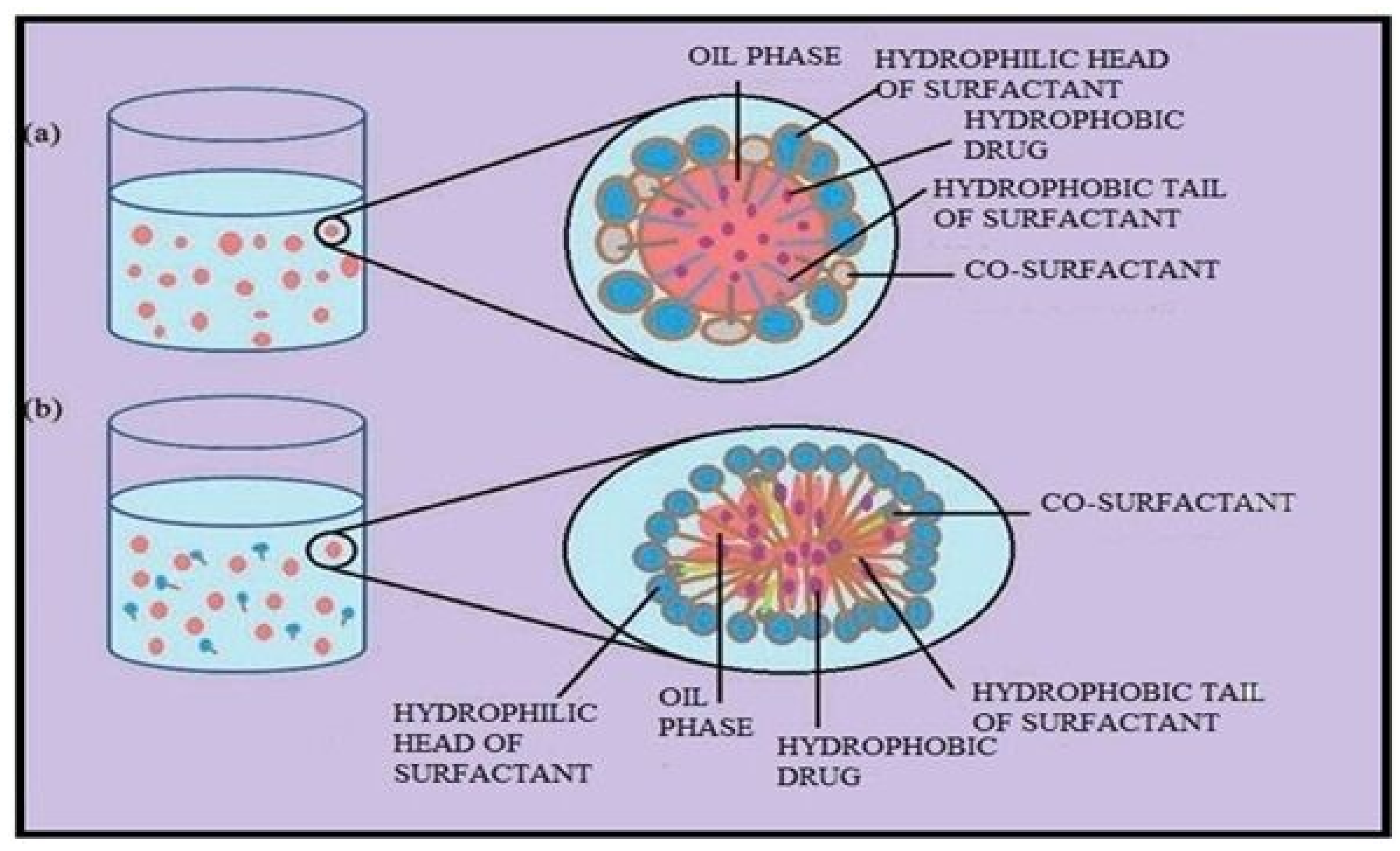
2.4. Differentiation between Nanoemulsions and Microemulsions
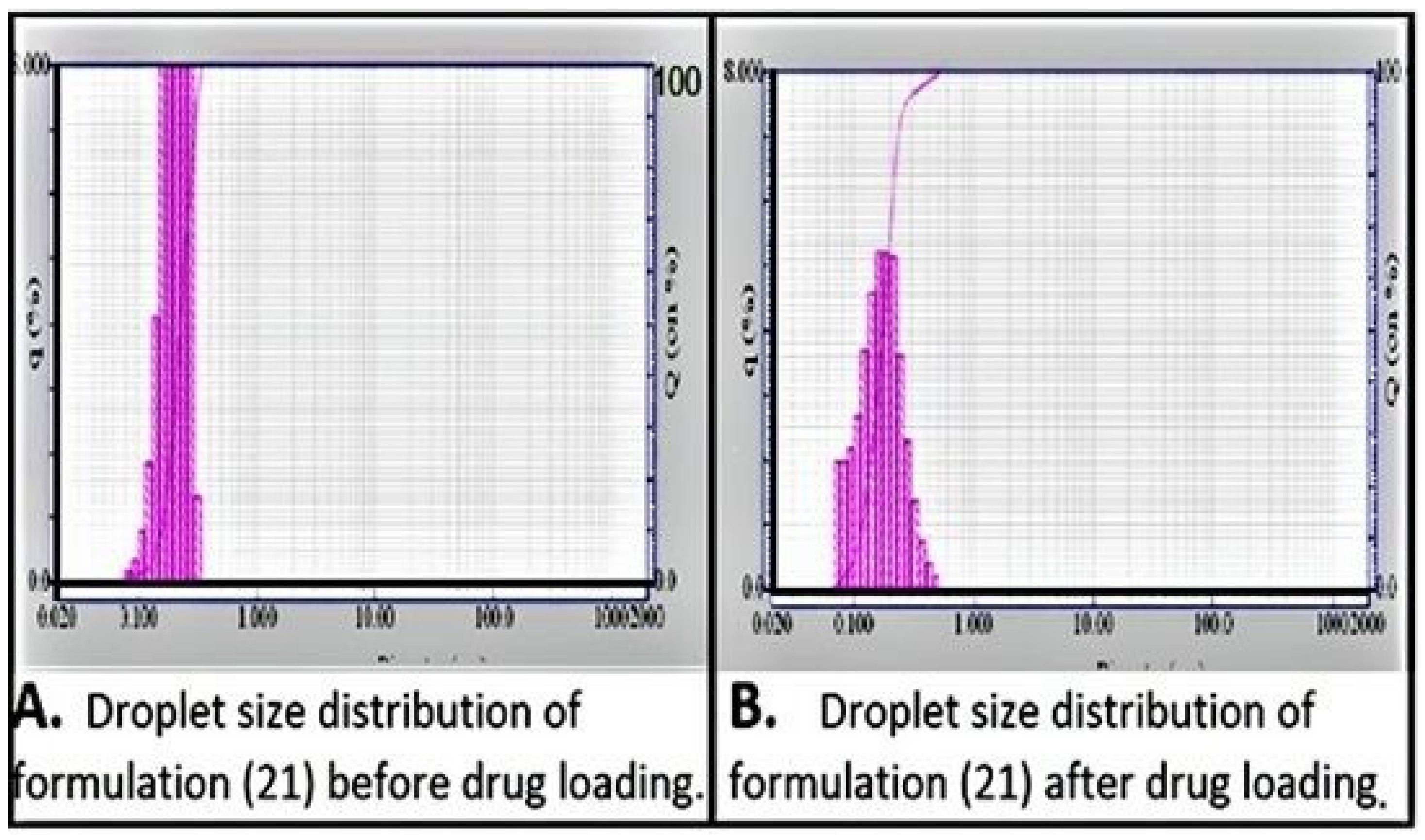
2.4.1. Droplet Size Distribution
2.4.2. Droplet Shape
2.4.3. Dilution
2.4.4. Temperature Change
2.5. Characterization of Solid SNEDDS (S-SNEDDS)
2.5.1. Physical Characterization of S-SNEDDS
2.5.2. Surface Morphology
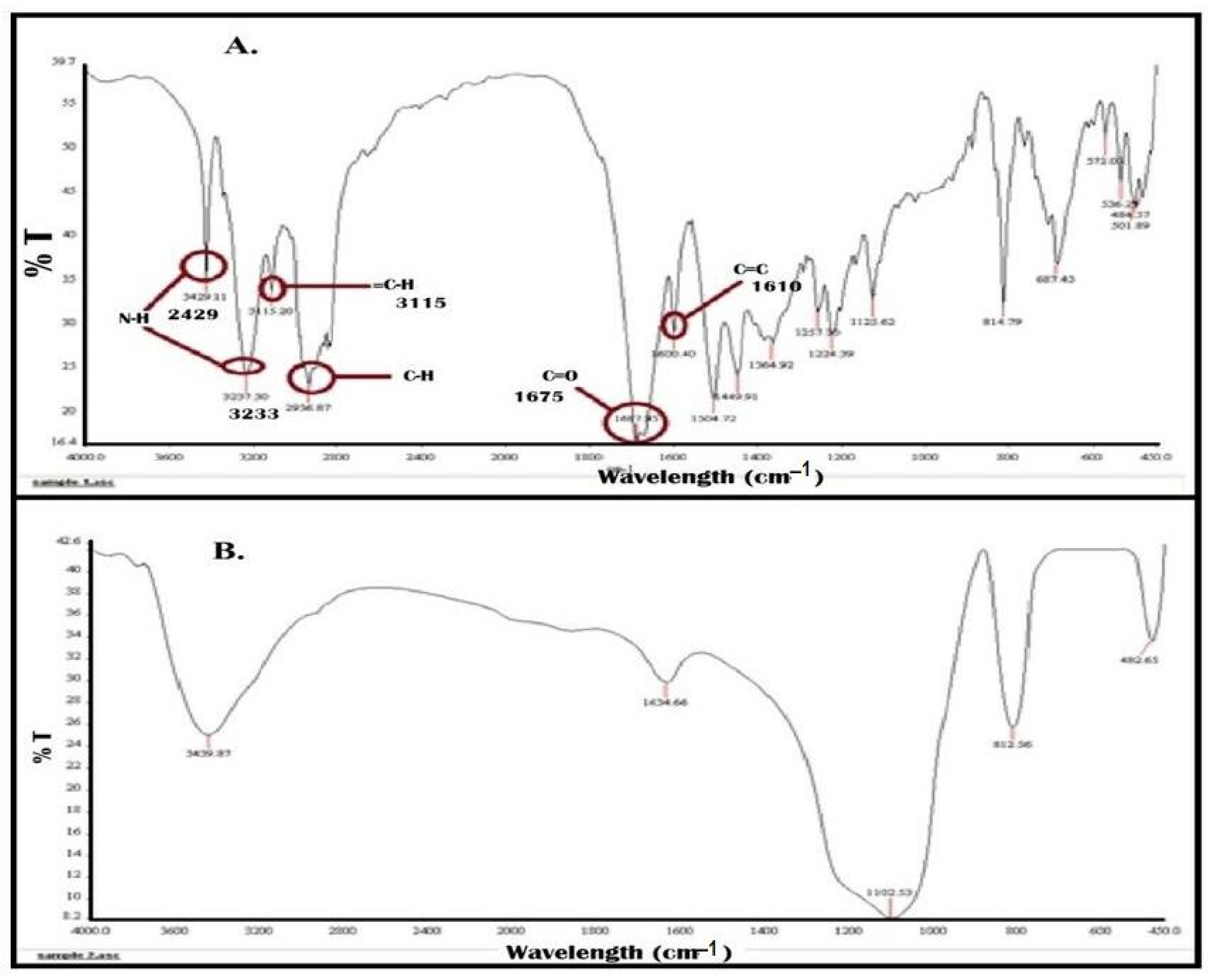
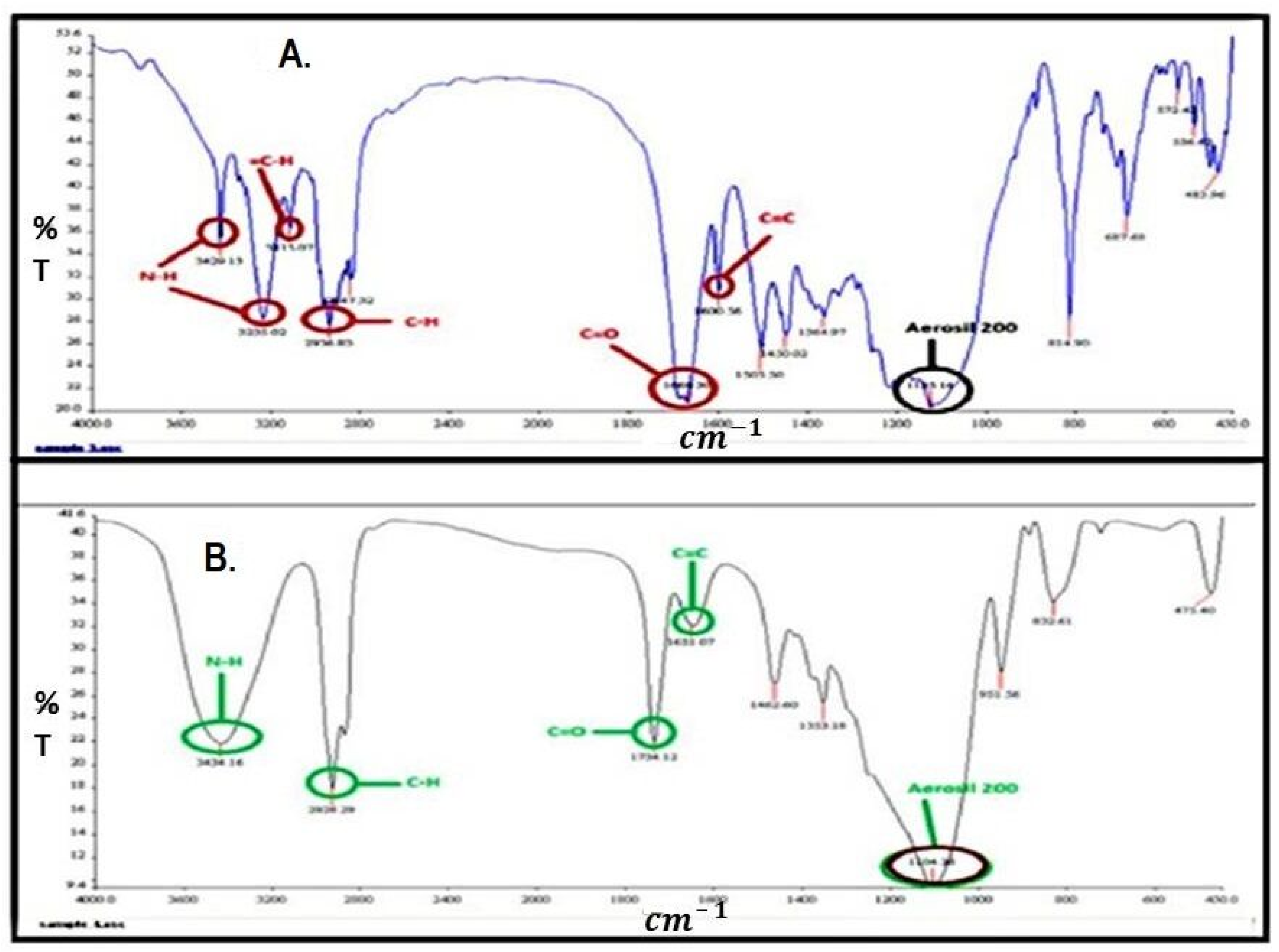
2.5.3. Fourier Transform Infrared Spectroscopy
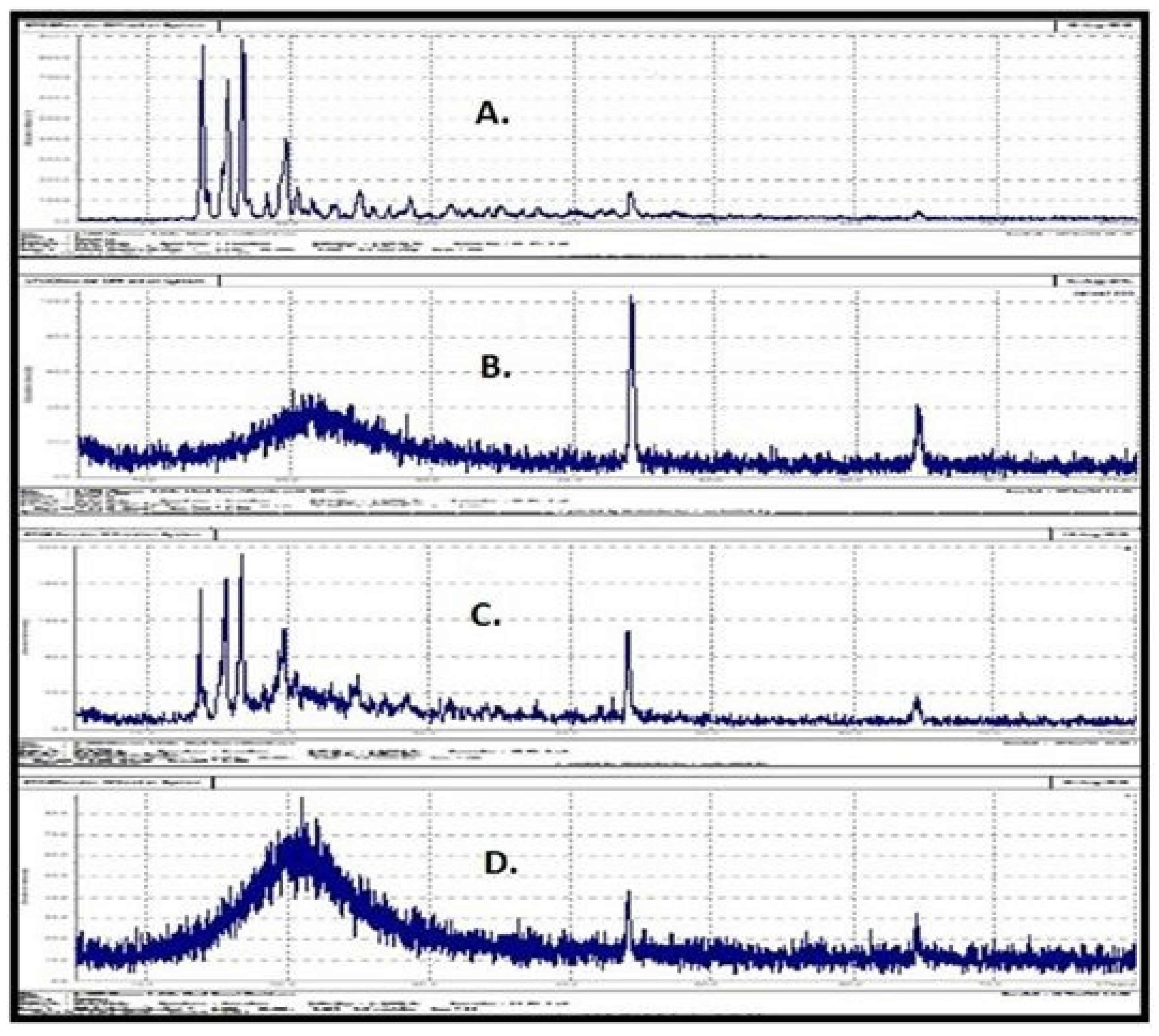
2.5.4. Powder X-ray Diffraction (PXRD) Studies
2.5.5. In Vitro Dispersion Profiles
2.6. Drug Content
2.7. Stability Studies
2.8. In Vivo Bioavailability Study
3. Materials and Methods
3.1. Materials
3.2. Methods
3.2.1. Solubility Studies
3.2.2. Selection of Surfactant and Co-Surfactant
3.2.3. Construction of Ternary Phase Diagram
3.2.4. Preparation of Liquid SEDDS (L-SEDDS)
3.2.5. Percentage Transmittance, Saturated Solubility of SEDDS, and Self-Emulsification Time Determination
3.2.6. Optimization of L-SEDDS
3.2.7. Confirmation of Dispersion’s Nature (Distinction between Nanoemulsions and Microemulsions)
Particle Size Distribution, Polydispersity and Shape Analysis
Dilution and pH Change
Effect of Temperature Change
Effect of Centrifugation
3.2.8. Preparation of Solid SEDDS (S-SEDDS)
3.2.9. Characterization of S-SEDDS
Surface Morphology
Fourier Transform Infrared Spectroscopy (FTIR)
Powder X-ray Diffraction (PXRD) Studies
Physical Characterization of S-SEDDS
- a Analysis of flow properties S-SEDDS powder
- b Hardness of S-SNEDDS tablets
- c Friability testing S-SNEDDS tablets
- d Uniformity of weight and disintegration time S-SNEDDS tablets
- e In vitro dispersion profile
- f Drug content
Stability Studies
In Vivo Bioavailability Study
Statistical Analysis
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Fong, S.Y.K.; Martins, S.M.; Brandl, M.; Bauer-Brandl, A. Solid Phospholipid Dispersions for Oral Delivery of Poorly Soluble Drugs: Investigation into Celecoxib Incorporation and Solubility-In Vitro Permeability Enhancement. J. Pharm. Sci. 2016, 105, 1113–1123. [Google Scholar] [CrossRef]
- Rehman, F.U.; Shah, K.U.; Shah, S.U.; Khan, I.U.; Khan, G.M.; Khan, A. From nanoemulsions to self-nanoemulsions, with recent advances in self-nanoemulsifying drug delivery systems (SNEDDS). Expert Opin. Drug Deliv. 2016, 14, 1325–1340. [Google Scholar] [CrossRef] [PubMed]
- Yeom, D.W.; Song, Y.S.; Kim, S.R.; Lee, S.G.; Kang, M.H.; Lee, S.; Choi, Y.W. Development and optimization of a self-microemulsifying drug delivery system for ator vastatin calcium by using D-optimal mixture design. Int. J. Nanomed. 2015, 10, 3865. [Google Scholar]
- Singh, G.; Pai, R.S. Trans-resveratrol self-nano-emulsifying drug delivery system (SNEDDS) with enhanced bioavailability potential: Optimization, pharmacokinetics and in situ single pass intestinal perfusion (SPIP) studies. Drug Deliv. 2015, 22, 522–530. [Google Scholar] [CrossRef]
- Cherniakov, I.; Domb, A.J.; Hoffman, A. Self-nano-emulsifying drug delivery systems: An update of the biopharmaceutical aspects. Expert Opin. Drug Deliv. 2015, 12, 1121–1133. [Google Scholar] [CrossRef]
- Mir, M.; Ishtiaq, S.; Rabia, S.; Khatoon, M.; Zeb, A.; Khan, G.M.; Rehman, A.U.; Din, F.U. Nanotechnology: From In Vivo Imaging System to Controlled Drug Delivery. Nanoscale Res. Lett. 2017, 12, 1–16. [Google Scholar] [CrossRef]
- Wang, Z.; Sun, J.; Wang, Y.; Liu, X.; Liu, Y.; Fu, Q.; Meng, P.; He, Z. Solid self-emulsifying nitrendipine pellets: Preparation and in vitro/in vivo evaluation. Int. J. Pharm. 2010, 383, 1–6. [Google Scholar] [CrossRef]
- Shakeel, F.; Haq, N.; El-Badry, M.; Alanazi, F.K.; Alsarra, I. Ultra fine super self-nanoemulsifying drug delivery system (SNEDDS) enhanced solubility and dissolution of indomethacin. J. Mol. Liq. 2013, 180, 89–94. [Google Scholar] [CrossRef]
- Anton, N.; Vandamme, T.F. Nano-emulsions and Micro-emulsions: Clarifications of the Critical Differences. Pharm. Res. 2010, 28, 978–985. [Google Scholar] [CrossRef]
- Fanun, M. Microemulsions: Properties and Applications; CRC Press: Boca Raton, FL, USA, 2008. [Google Scholar]
- Wennerström, H.; Balogh, J.; Olsson, U. Interfacial tensions in microemulsions. Colloids Surf. A Physicochem. Eng. Asp. 2006, 291, 69–77. [Google Scholar] [CrossRef]
- McClements, D.J. Nanoemulsions versus microemulsions: Terminology, differences, and similarities. Soft Matter 2012, 8, 1719–1729. [Google Scholar] [CrossRef]
- Solans, C.; Izquierdo, P.; Nolla, J.; Azemar, N.; Garcia-Celma, M.J. Nano-emulsions. Curr. Opin. Colloid Interface Sci. 2005, 10, 102–110. [Google Scholar] [CrossRef]
- McClements, D.J. Edible nanoemulsions: Fabrication, properties, and functional performance. Soft Matter 2010, 7, 2297–2316. [Google Scholar] [CrossRef]
- McClements, D.J. Food Emulsions: Principles, Practices, and Techniques; CRC Press: Boca Raton, FL, USA, 2015. [Google Scholar]
- Jonsson, B.; Lindman, B.; Holmberg, K.; Kronberg, B. Surfactants and Polymers in Aqueous Solution; John Wiley & Sons: Chichester, UK, 1998. [Google Scholar]
- Yang, Y.; Leser, M.E.; Sher, A.A.; McClements, D.J. Formation and stability of emulsions using a natural small molecule surfactant: Quillaja saponin (Q-Naturale®). Food Hydrocoll. 2012, 30, 589–596. [Google Scholar] [CrossRef]
- Yi, T.; Wan, J.; Xu, H.; Yang, X. A new solid self-microemulsifying formulation prepared by spray-drying to improve the oral bioavailability of poorly water soluble drugs. Eur. J. Pharm. Biopharm. 2008, 70, 439–444. [Google Scholar] [CrossRef]
- Zhang, P.; Liu, Y.; Feng, N.; Xu, J. Preparation and evaluation of self-microemulsifying drug delivery system of oridonin. Int. J. Pharm. 2008, 355, 269–276. [Google Scholar] [CrossRef]
- Ansari, K.A.; Pagar, K.P.; Anwar, S.; Vavia, P.R.; Storti-Filho, A.; Damke, E.; Carrara, M.A.; Batista, M.R.; Donatti, L.; Boer, C.G.; et al. Design and optimization of self-microemulsifying drug delivery system (SMEDDS) of felodipine for chronotherapeutic application. Braz. J. Pharm. Sci. 2014, 50, 203–212. [Google Scholar] [CrossRef]
- Fagir, W.; Hathout, R.M.; A Sammour, O.; ElShafeey, A.H. Self-microemulsifying systems of Finasteride with enhanced oral bioavailability: Multivariate statistical evaluation, characterization, spray-drying and in vivo studies in human volunteers. Nanomedicine 2015, 10, 3373–3389. [Google Scholar] [CrossRef]
- Kahlweit, M.; Strey, R.; Busse, G. Microemulsions: A qualitative thermodynamic approach. J. Phys. Chem. 1990, 94, 3881–3894. [Google Scholar] [CrossRef]
- Kahlweit, M.; Busse, G.; Faulhaber, B.; Jen, J. Shape Changes of Globules in Nonionic Microemulsions. J. Phys. Chem. 1996, 100, 14991–14994. [Google Scholar] [CrossRef]
- Tadros, T.; Izquierdo, P.; Esquena, J.; Solans, C. Formation and stability of nano-emulsions. Adv. Colloid Interface Sci. 2004, 108, 303–318. [Google Scholar] [CrossRef] [PubMed]
- Da Silva, L.M.; Montanari, C.M.; Santos, O.M.M.; Cazedey, E.C.L.; Ângelo, M.L.; de Araújo, M.B. Quality evaluation of the Finasteride polymorphic forms I and II in capsules. J. Pharm. Biomed. Anal. 2015, 105, 24–31. [Google Scholar] [CrossRef] [PubMed]
- Cha, E.K.; Shariat, S.F. The use of 5α-reductase inhibitors for the prevention and treatment of prostate cancer. Eur. Urol. 2011, 59, 515–517. [Google Scholar] [CrossRef] [PubMed]
- Almeida, H.M.; Marques, H.M.C. Physicochemical characterization of finasteride: PEG 6000 and finasteride: Kollidon K25 solid dispersions, and finasteride: β-cyclodextrin inclusion complexes. J. Incl. Phenom. Macrocycl. Chem. 2011, 70, 397–406. [Google Scholar] [CrossRef]
- Zabkowski, T. Evaluation of the clinical indications, adverse drug reactions, and finasteride use in patients with benign prostatic hyperplasia in Poland. Pharmacol. Rep. 2014, 66, 565–569. [Google Scholar] [CrossRef]
- Bandopadhyay, S.; Katare, O.; Singh, B. Development of optimized supersaturable self-nanoemulsifying systems of ezetimibe: Effect of polymers and efflux transporters. Expert Opin. Drug Deliv. 2014, 11, 479–492. [Google Scholar] [CrossRef]
- Rashid, R.; Kim, D.W.; Din, F.U.; Mustapha, O.; Yousaf, A.; Park, J.H.; Kim, J.O.; Yong, C.S.; Choi, H.-G. Effect of hydroxypropylcellulose and Tween 80 on physicochemical properties and bioavailability of ezetimibe-loaded solid dispersion. Carbohydr. Polym. 2015, 130, 26–31. [Google Scholar] [CrossRef]
- Mohd, A.B.; Sanka, K.; Bandi, S.; Diwan, P.; Shastri, N. Solid self-nanoemulsifying drug delivery system (S-SNEDDS) for oral delivery of glimepiride: Development and antidiabetic activity in albino rabbits. Drug Deliv. 2013, 22, 499–508. [Google Scholar] [CrossRef]
- Gupta, S.; Chavhan, S.; Sawant, K.K. Self-nanoemulsifying drug delivery system for adefovir dipivoxil: Design, characterization, in vitro and ex vivo evaluation. Colloids Surfaces A: Physicochem. Eng. Asp. 2011, 392, 145–155. [Google Scholar] [CrossRef]
- Abdelbary, G.; Amin, M.; Salah, S. Self nano-emulsifying simvastatin based tablets: Design and in vitro/in vivo evaluation. Pharm. Dev. Technol. 2013, 18, 1294–1304. [Google Scholar] [CrossRef]
- Agrawal, A.G.; Kumar, A.; Gide, P.S. Formulation of solid self-nanoemulsifying drug delivery systems using N-methyl pyrrolidone as cosolvent. Drug Dev. Ind. Pharm. 2014, 41, 594–604. [Google Scholar] [CrossRef] [PubMed]
- Sinko, P.; Martin, A. Micromeritics. J. Pharm. Pharm. Sci. 2006, 533–560. [Google Scholar]
- Miao, Y.; Chen, G.; Ren, L.; Pingkai, O. Characterization and evaluation of self-nanoemulsifying sustained-release pellet formulation of ziprasidone with enhanced bioavailability and no food effect. Drug Deliv. 2014, 23, 2163–2172. [Google Scholar] [CrossRef] [PubMed]
- Baloch, J.; Sohail, M.F.; Sarwar, H.S.; Kiani, M.H.; Khan, G.M.; Jahan, S.; Rafay, M.; Chaudhry, M.T.; Yasinzai, M.; Shahnaz, G. Self-Nanoemulsifying Drug Delivery System (SNEDDS) for Improved Oral Bioavailability of Chlorpromazine: In Vitro and In Vivo Evaluation. Medicina 2019, 55, 210. [Google Scholar] [CrossRef] [PubMed]
- Kang, J.H.; Oh, D.H.; Oh, Y.-K.; Yong, C.S.; Choi, H.-G. Effects of solid carriers on the crystalline properties, dissolution and bioavailability of flurbiprofen in solid self-nanoemulsifying drug delivery system (solid SNEDDS). Eur. J. Pharm. Biopharm. 2011, 80, 289–297. [Google Scholar] [CrossRef]
- Chen, Y.; Li, G.; Wu, X.; Chen, Z.; Hang, J.; Qin, B.; Chen, S.; Wang, R. Self-Microemulsifying Drug Delivery System (SMEDDS) of Vinpocetine: Formulation Development and in Vivo Assessment. Biol. Pharm. Bull. 2008, 31, 118–125. [Google Scholar] [CrossRef]
- Balakrishnan, P.; Lee, B.-J.; Oh, D.H.; Kim, J.O.; Hong, M.J.; Jee, J.-P.; Kim, J.A.; Yoo, B.K.; Woo, J.S.; Yong, C.S.; et al. Enhanced oral bioavailability of dexibuprofen by a novel solid Self-emulsifying drug delivery system (SEDDS). Eur. J. Pharm. Biopharm. 2009, 72, 539–545. [Google Scholar] [CrossRef]
- Rao, J.; McClements, D.J. Formation of Flavor Oil Microemulsions, Nanoemulsions and Emulsions: Influence of Composition and Preparation Method. J. Agric. Food Chem. 2011, 59, 5026–5035. [Google Scholar] [CrossRef]
- Evilevitch, A.; Jönsson, B.; Olsson, U.; Wennerström, H. Molecular Transport in a Nonequilibrium Droplet Microemulsion System. Langmuir 2001, 17, 6893–6904. [Google Scholar] [CrossRef]
- Rao, J.; McClements, D.J. Lemon oil solubilization in mixed surfactant solutions: Rationalizing microemulsion & nanoemulsion formation. Food Hydrocoll. 2012, 26, 268–276. [Google Scholar] [CrossRef]
- Kahlweit, M.; Strey, R.; Busse, G. Weakly to strongly structured mixtures. Phys. Rev. E 1993, 47, 4197–4209. [Google Scholar] [CrossRef] [PubMed]
- Izquierdo, P.; Esquena, J.; Tadros, T.F.; Dederen, C.; Garcia, M.J.; Azemar, N.; Solans, C. Formation and Stability of Nano-Emulsions Prepared Using the Phase Inversion Temperature Method. Langmuir 2001, 18, 26–30. [Google Scholar] [CrossRef]
- Thi, T.D.; Van Speybroeck, M.; Barillaro, V.; Martens, J.; Annaert, P.; Augustijns, P.; Van Humbeeck, J.; Vermant, J.; Mooter, G.V.D. Formulate-ability of ten compounds with different physicochemical profiles in SMEDDS. Eur. J. Pharm. Sci. 2009, 38, 479–488. [Google Scholar] [CrossRef] [PubMed]
- Agrawal, A.G.; Kumar, A.; Gide, P.S. Formulation development and in vivo hepatoprotective activity of self nanoemulsifying drug delivery system of antioxidant coenzyme Q10. Arch. Pharmacal. Res. 2014. [Google Scholar] [CrossRef]
- Parmar, K.; Patel, J.; Sheth, N. Self nano-emulsifying drug delivery system for Embelin: Design, characterization and in-vitro studies. Asian J. Pharm. Sci. 2015, 10, 396–404. [Google Scholar] [CrossRef]
- Khan, A.W.; Kotta, S.; Ansari, S.H.; Sharma, R.K.; Ali, J. Potentials and challenges in self-nanoemulsifying drug delivery systems. Expert Opin. Drug Deliv. 2012, 9, 1305–1317. [Google Scholar] [CrossRef]
- Wang, L.; Dong, J.; Chen, J.; Eastoe, J.; Li, X. Design and optimization of a new self-nanoemulsifying drug delivery system. J. Colloid Interface Sci. 2008, 330, 443–448. [Google Scholar] [CrossRef]




| Surfactant | Solubility (mg/mL) | Self-Emulsification Time (s) | Percentage Transmittance (%) | ||
|---|---|---|---|---|---|
| Tween 80 | 46 ± 6 | 50 | 80 | ||
| Cremophore RH 40 | 20 ± 5 | 20 | 99 | ||
| Cremophore RH 40 | Tween 80 | Cremophore RH 40 | Tween 80 | ||
| Co-surfactant (used along with surfactants Cremophore RH 40 and Tween 80) | |||||
| PEG 400 (Co-surfactant) | 21 ± 3 | 10 | 38 | 99 | 84 |
| Labrasol (Co-surfactant) | 12 ± 2 | 16 | 42 | 98 | 84 |
| Formulation with Composition (oil, Surfactant, Co-Surfactant) | Saturated Solubility (mg/mL) | Percentage Transmittance (%) | Droplet Size (nm) | Self-Emulsification Time (s) |
|---|---|---|---|---|
| 13 (40%, 40%, 20%) | 21 | 87 | 273 | 10 |
| 21 (30%, 52.5% 17.5%) | 22 | 94 | 180 | 10 |
| 22 (40%, 45%, 15%) | 21 | 92 | 211 | 15 |
| Ingredients | Formulation 1 (Aerosil 200) | Formulation 2 (Avicel) |
|---|---|---|
| Formulations (% w/w) | ||
| Finasteride | 1.25 | 1.25 |
| Cremophore RH 40 | 32 | 32 |
| Capryol 90 | 18 | 18 |
| PEG 400 | 11 | 11 |
| Avicel | ---- | 36.75 |
| Aerosil | 36.75 | ---- |
| Mg stearate | 1 | 1 |
| Carr’s index (CI) | 11% | 6% |
| Angle of repose | 25° | 31° |
| Hardness of tablets | 5.5 ± 0.35 Kg | 4.2 ± 0.71 Kg |
| Hausner ratio (HR) | 1.12 | 1.0 |
| Friability test | 0.30 ± 0.1% | 0.45 ± 0.05% |
| Disintegration time | 6 min | 6 min |
| Uniformity of weight (Tablets) | 400 ± 2.4 mg | 400 ± 3.5 mg |
| Time (Month) | Droplet Size (nm) | Drug Content (%) | In Vitro Dispersion (% Drug Released after 60 min) | |||
|---|---|---|---|---|---|---|
| S-SNEDDS Tablets | L-SNEDDS | S-SNEDDS Tablets | L-SNEDDS | S-SNEDDS Tablets | L-SNEDDS | |
| 1 | 182 ± 2 | 190 ± 1 | >95 ± 1.23 | >95 ± 1.32 | 92% ± 0.56 | 93% ± 1.00 |
| 2 | 190 ± 1 | 195 ± 2 | >95 ± 1.40 | >95 ± 1.56 | 93% ± 1.41 | 90% ± 1.88 |
| 3 | 195 ± 1 | 193 ± 3 | >95 ± 1.52 | >90 ± 1.63 | 90% ± 1.51 | 84% ± 1.50 |
| 6 | 194 ± 2 | 210 ± 3 | >95 ±1.50 | >90 ± 2.71 | 93% ± 1.62 | 81% ± 2.19 |
| Formulation | AUC (h. µg/mL) | Cmax (µg/mL) | Tmax (h) | t1/2 (h) | Ke (h−1) |
|---|---|---|---|---|---|
| S-SNEDDS tablets | 280.92 ± 33.9 | 1.214 ± 0.45 | 1.02 ± 0.2 | 9.92 ± 1.51 | 0.09 ± 0.02 |
| L-SNEDDS | 287.03 ± 34.4 | 1.236 ± 0.42 | 1.00 ± 0.2 | 9.01 ± 1.47 | 0.10 ± 0.02 |
| Commercial tablets | 93.51 ± 10.73 * | 0.591 ± 0.21 * | 1.12 ± 0.5 | 7.76 ± 1.16 | 0.19 ± 0.05 |
| Title | Formulation Code with Percentage Transmittance and Results of Physical Examination in Codes | Oil Phase (Capryol 90) µL | Surfactant (Cremophore RH 40) µL | Co-Surfactant (PEG 400) µL | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Km Ratio (Surfactant to co-surfactant ratio) | 1:1 | 2:1 | 3:1 | 1:1 | 2:1 | 3:1 | 1:1 | 2:1 | 3:1 | 1:1 | 2:1 | 3:1 | |||
| X 1 | 93 (++) | X 10 | 94.5 (++) | X 19 | 21.2 (--) | 100 | 100 | 100 | 450 | 600 | 675 | 450 | 300 | 225 | |
| X 2 | 94.5 (++) | X 11 | 94.6 (++) | X 20 | 95.1 (+++) | 200 | 200 | 200 | 400 | 533 | 600 | 400 | 267 | 200 | |
| X 3 | 94.5 (++) | X 12 | 94.6 (++) | X 21 | 96.6 (+++) | 300 | 300 | 300 | 350 | 467 | 525 | 350 | 234 | 175 | |
| X 4 | 93.4 (++) | X 13 | 92.4 (++) | X 22 | 96.1 (+++) | 400 | 400 | 400 | 300 | 400 | 450 | 300 | 200 | 150 | |
| X 5 | 94 (++) | X 14 | 92.5 (++) | X 23 | 93.4 (++) | 500 | 500 | 500 | 250 | 333 | 375 | 250 | 167 | 125 | |
| X 6 | 86 (+) | X 15 | 92.3 (++) | X 24 | 91 (++) | 600 | 600 | 600 | 200 | 266 | 300 | 200 | 134 | 100 | |
| X 7 | 72 (-) | X 16 | 84 (-) | X 25 | 91 (++) | 700 | 700 | 700 | 150 | 200 | 225 | 150 | 100 | 75 | |
| X 8 | 10 (--) | X 17 | 47 (--) | X 26 | 86 (+) | 800 | 800 | 800 | 100 | 133 | 150 | 100 | 67 | 50 | |
| X 9 | 01 (--) | X 18 | 25 (--) | X 27 | 71.4 (-) | 900 | 900 | 900 | 50 | 66 | 75 | 50 | 34 | 25 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rehman, F.U.; Farid, A.; Shah, S.U.; Dar, M.J.; Rehman, A.U.; Ahmed, N.; Rashid, S.A.; Shaukat, I.; Shah, M.; Albadrani, G.M.; et al. Self-Emulsifying Drug Delivery Systems (SEDDS): Measuring Energy Dynamics to Determine Thermodynamic and Kinetic Stability. Pharmaceuticals 2022, 15, 1064. https://doi.org/10.3390/ph15091064
Rehman FU, Farid A, Shah SU, Dar MJ, Rehman AU, Ahmed N, Rashid SA, Shaukat I, Shah M, Albadrani GM, et al. Self-Emulsifying Drug Delivery Systems (SEDDS): Measuring Energy Dynamics to Determine Thermodynamic and Kinetic Stability. Pharmaceuticals. 2022; 15(9):1064. https://doi.org/10.3390/ph15091064
Chicago/Turabian StyleRehman, Fiza Ur, Arshad Farid, Shefaat Ullah Shah, Muhammad Junaid Dar, Asim Ur Rehman, Naveed Ahmed, Sheikh Abdur Rashid, Irfan Shaukat, Muddaser Shah, Ghadeer M. Albadrani, and et al. 2022. "Self-Emulsifying Drug Delivery Systems (SEDDS): Measuring Energy Dynamics to Determine Thermodynamic and Kinetic Stability" Pharmaceuticals 15, no. 9: 1064. https://doi.org/10.3390/ph15091064
APA StyleRehman, F. U., Farid, A., Shah, S. U., Dar, M. J., Rehman, A. U., Ahmed, N., Rashid, S. A., Shaukat, I., Shah, M., Albadrani, G. M., Kamel, M., Altyar, A. E., Abdel-Daim, M. M., & Shah, K. U. (2022). Self-Emulsifying Drug Delivery Systems (SEDDS): Measuring Energy Dynamics to Determine Thermodynamic and Kinetic Stability. Pharmaceuticals, 15(9), 1064. https://doi.org/10.3390/ph15091064








