Optimization of Long-Acting Bronchodilator Dose Ratios Using Isolated Guinea Pig Tracheal Rings for Synergistic Combination Therapy in Asthma and COPD
Abstract
1. Introduction
2. Results
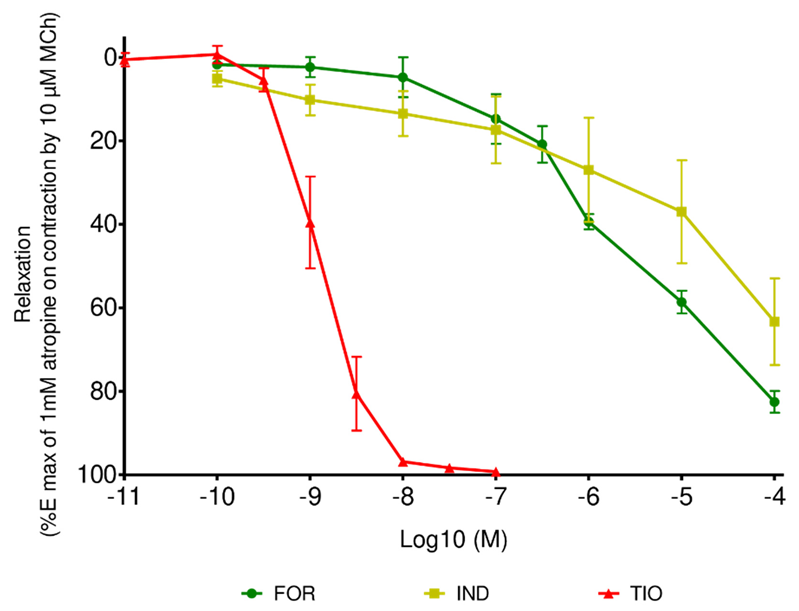
2.1. Individual Relaxant Effect
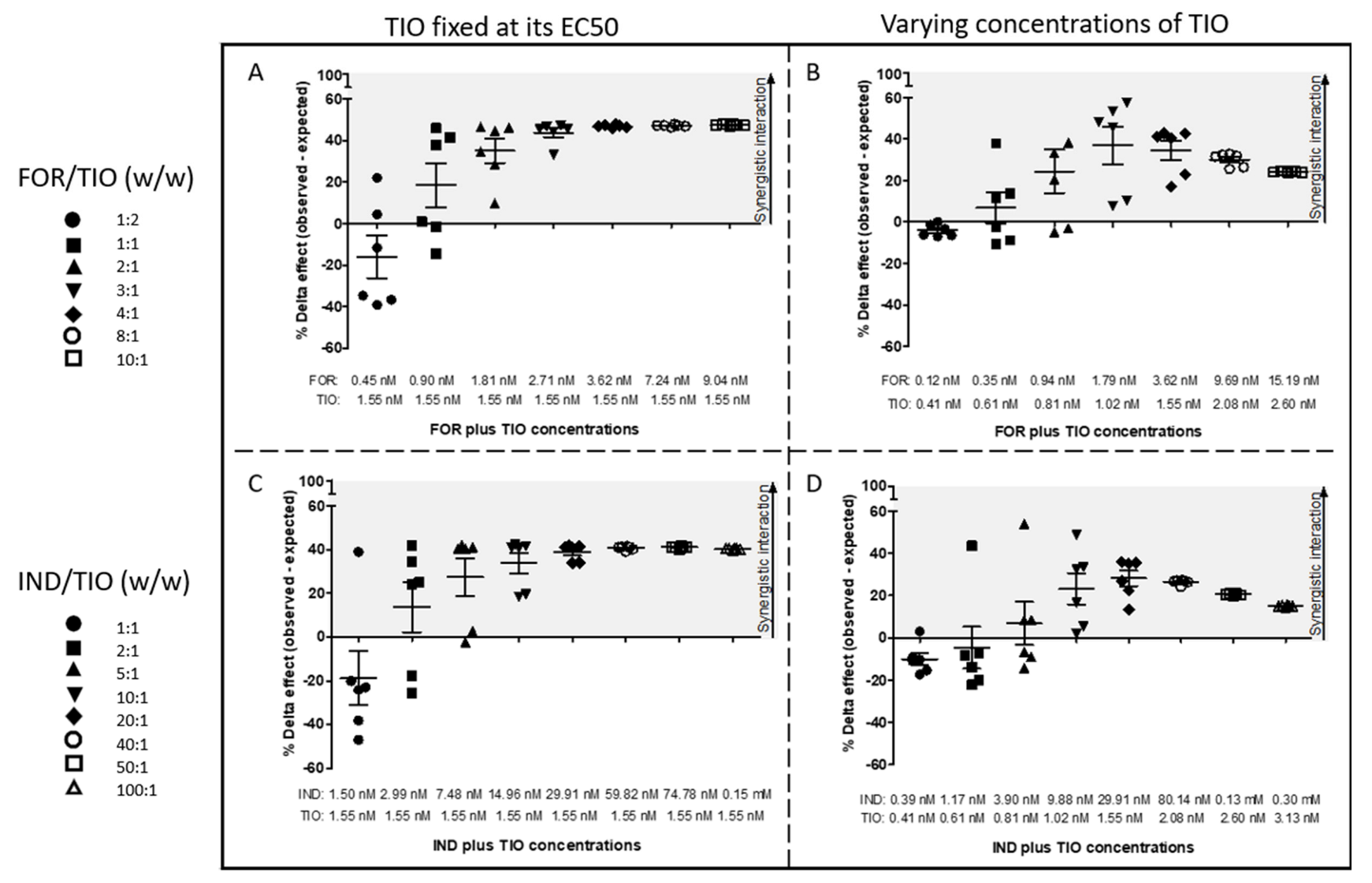
2.2. Interaction between LABA and LAMA Based on a Non-Constant Dose Ratio
2.3. Interaction between LABA and LAMA Based on a Constant Dose Ratio
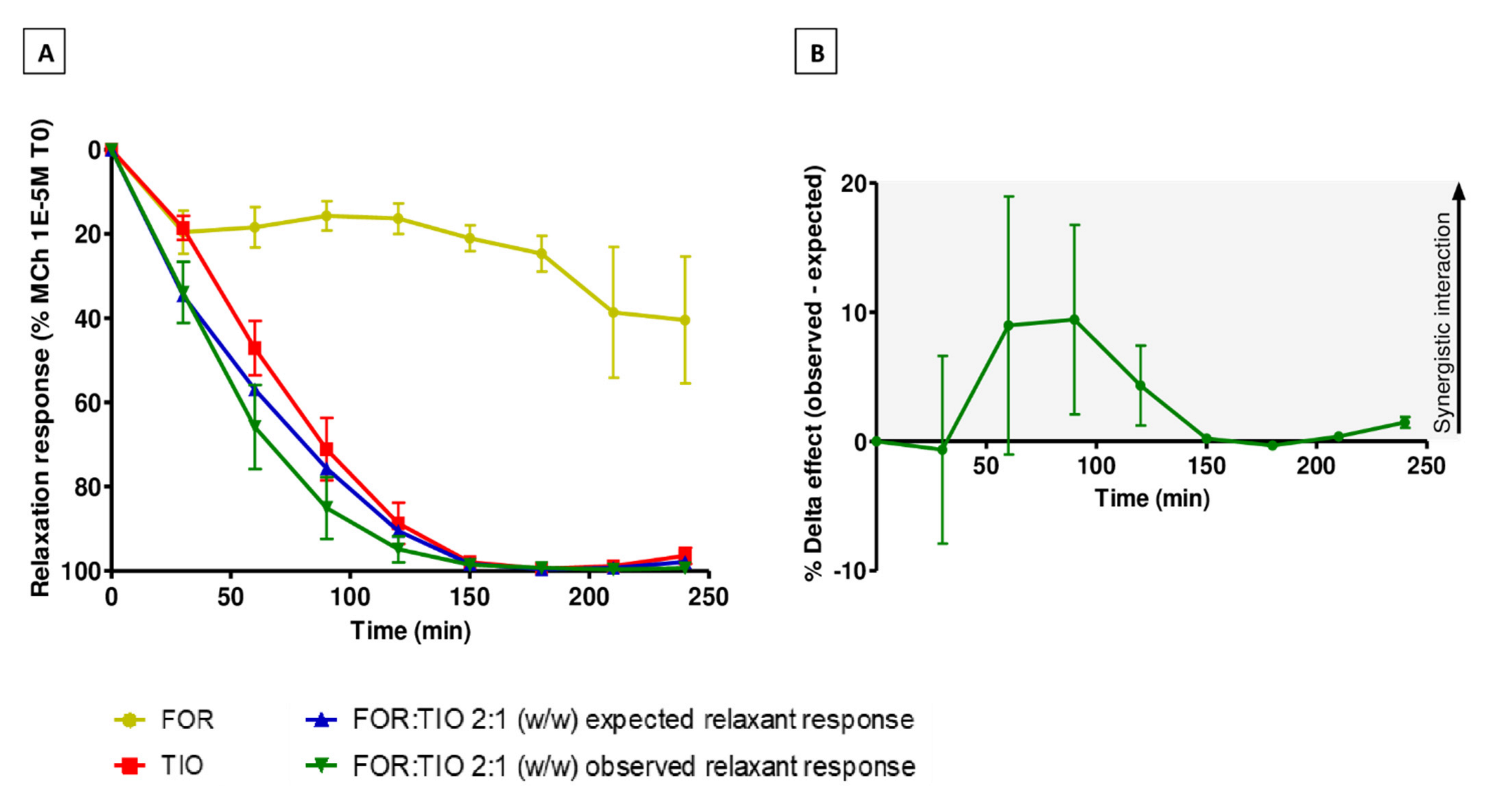
2.4. Interaction between LABA and LAMA Over Time
3. Discussion
4. Materials and Methods
4.1. Drugs
4.2. Animals
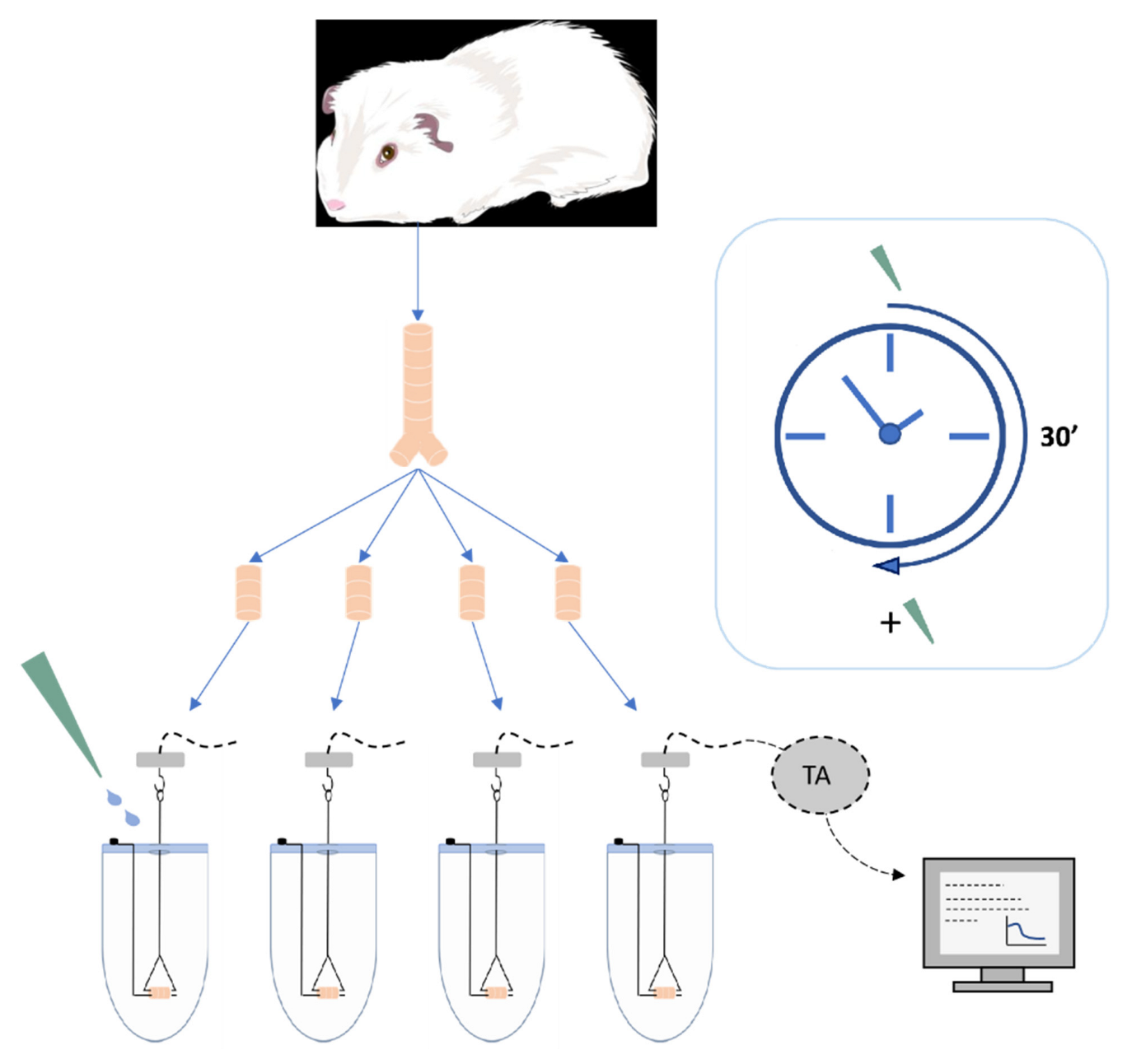
4.3. Preparation of Isolated Tracheal Rings from Dunkin Hartley Guinea Pig
4.4. Experimental Protocol
4.4.1. Cumulative Dose Fashion
4.4.2. Study Design
Interaction between LABA and LAMA Based on a Non-Constant Dose Ratio
Interaction between LABA and LAMA Based on a Constant Dose Ratio
Interaction between LABA and LAMA Over Time
4.5. Drug Interaction Analysis
4.6. Statistical Analysis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| ANOVA | Analysis of variance |
| ASM | Airway smooth muscle |
| BI | Bliss independence |
| CI | Combination index |
| COPD | Chronic obstructive pulmonary disease |
| ΔE | Delta effect |
| DRI | Dose reduction index |
| EC50-70 | Submaximal effective concentration size between 50% and 70% of the maximum concentration |
| FOR | Formoterol fumarate dihydrate |
| IND | Indacaterol maleate |
| LABA | Long-acting β2-agonist |
| LAMA | Long-acting muscarinic antagonist |
| pEC50 | Negative logarithm of the half maximal effective concentration |
| SEM | Standard error of the mean |
| TIO | Tiotropium bromide monohydrate |
| UT | Unified theory |
References
- GINA S. Comitee, Global Initiative for Asthma—Global Strategy for Asthma Management and Prevention. Updated 2021. Available online: http://www.ginasthma.org (accessed on 15 December 2021).
- GOLD S. Comitee, Global Initiative for Chronic Obstructive Lung Disease—Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease (2022 Report). Available online: http://www.goldcopd.org (accessed on 11 February 2022).
- Nunes, C.; Pereira, A.M.; Morais-almeida, M. Asthma costs and social impact. Asthma Res. Pract. 2017, 3, 1. [Google Scholar] [CrossRef] [PubMed]
- Calzetta, L.; Matera, M.G.; Cazzola, M. Pharmacological interaction between LABAs and LAMAs in the airways: Optimizing synergy. Eur. J. Pharmacol. 2015, 761, 168–173. [Google Scholar] [CrossRef] [PubMed]
- Calzetta, L.; Koziol-White, C. Pharmacological interactions: Synergism, or not synergism, that is the question. Curr. Res. Pharmacol. Drug Discov. 2021, 2, 100046. [Google Scholar] [CrossRef] [PubMed]
- Calzetta, L.; Matera, M.G.; Cazzola, M.; Rogliani, P. Optimizing the Development Strategy of Combination Therapy in Respiratory Medicine: From Isolated Airways to Patients. Adv. Ther. 2019, 36, 3291–3298. [Google Scholar] [CrossRef]
- Herlihy, J.T.; Semenov, I.; Brenner, R. Assessment of Airway Hyperresponsiveness in Murine Tracheal Rings. Mouse Model. Allergy Dis. Methods Protoc. Methods Mol. Biol. 2013, 1032, 257–269. [Google Scholar] [CrossRef]
- Jespersen, B.; Tykocki, N.R.; Watts, S.W.; Cobbett, P.J. Measurement of Smooth Muscle Function in the Isolated Tissue Bath-applications to Pharmacology Research. J. Vis. Exp. 2015, 95, e52324. [Google Scholar] [CrossRef]
- Semenov, I.; Herlihy, J.T.; Brenner, R. In vitro Measurements of Tracheal Constriction Using Mice. J. Vis. Exp. 2012, 64, e3703. [Google Scholar] [CrossRef]
- Adner, M.; Canning, B.J.; Meurs, H.; Ford, W.; Ramírez, P.R.; van den Berg, M.P.M.; Dahlén, S.-E. Back to the future: Re-establishing Guinea pig in vivo asthma models. Clin. Sci. 2020, 134, 1219–1242. [Google Scholar] [CrossRef]
- Canning, B.J.; Chou, Y. Using guinea pigs in studies relevant to asthma and COPD. Pulm. Pharmacol. Ther. 2008, 21, 702–720. [Google Scholar] [CrossRef]
- Nials, A.T.; Coleman, R.A.; Johnson, M.; Magnussen, H.; Rabe, K.F.; Vardey, C.J. Effects of β-adrenoceptor agonists in human bronchial smooth muscle. Br. J. Pharmacol. 1993, 110, 1112–1116. [Google Scholar] [CrossRef]
- Ressmeyer, A.R.; Larsson, A.K.; Vollmer, E.; Dahlèn, S.E.; Uhlig, S.; Martin, C. Characterisation of guinea pig precision-cut lung slices: Comparison with human tissues. Eur. Respir. J. 2006, 28, 603–611. [Google Scholar] [CrossRef] [PubMed]
- Tanner, L.; Single, A.B. Animal Models Reflecting Chronic Obstructive Pulmonary Disease and Related Respiratory Disorders: Translating Pre-Clinical Data into Clinical Relevance. J. Innate Immun. 2020, 12, 203–225. [Google Scholar] [CrossRef] [PubMed]
- Venkatasamy, R.; Spina, D. Novel relaxant effects of RPL554 on guinea pig tracheal smooth muscle contractility. Br. J. Pharmacol. 2016, 173, 2335–2351. [Google Scholar] [CrossRef]
- Aalbers, R.; Maleki-Yazdi, M.R.; Hamilton, A.; Waitere-Wijker, S.; Zhao, Y.; Amatto, V.C.; Bjermer, L. Randomized, Double-Blind, Dose-Finding Study for Tiotropium when Added to Olodaterol, Administered via the Respimat® Inhaler in Patients with Chronic Obstructive Pulmonary Disease. Adv. Ther. 2015, 32, 809–822. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Maltais, F.; Hamilton, A.; Voß, F.; Maleki-Yazdi, M.R. Dose Determination for a Fixed-Dose Drug Combination: A Phase II Randomized Controlled Trial for Tiotropium/Olodaterol Versus Tiotropium in Patients with COPD. Adv. Ther. 2019, 36, 962–968. [Google Scholar] [CrossRef]
- Calzetta, L.; Rogliani, P.; Page, C.; Rinaldi, B.; Cazzola, M.; Matera, M.G. Pharmacological characterization of the interaction between tiotropium bromide and olodaterol on human bronchi and small airways. Pulm. Pharmacol. Ther. 2019, 56, 39–50. [Google Scholar] [CrossRef]
- Cazzola, M.; Calzetta, L.; Ora, J.; Puxeddu, E.; Rogliani, P.; Matera, M.G. Searching for the synergistic effect between aclidinium and formoterol: From bench to bedside. Respir. Med. 2015, 109, 1305–1311. [Google Scholar] [CrossRef] [PubMed]
- Halpin, D.M.G. Tiotropium in asthma: What is the evidence and how does it fit in? World Allergy Organ. J. 2016, 9, 29. [Google Scholar] [CrossRef]
- Mansfield, L.; Bernstein, J.A. Tiotropium in asthma: From bench to bedside. Respir. Med. 2019, 154, 47–55. [Google Scholar] [CrossRef]
- Anzueto, A.; Miravitlles, M. Tiotropium in chronic obstructive pulmonary disease—A review of clinical development. Respir. Res. 2020, 21, 199. [Google Scholar] [CrossRef]
- Chung, V.C.H.; Ma, P.H.X.; Hui, D.S.C.; Tam, W.W.S.; Tang, J.L. Indacaterol for Chronic Obstructive Pulmonary Disease: Systematic Review and Meta-Analysis. PLoS ONE 2013, 8, e70784. [Google Scholar] [CrossRef]
- Vogelberg, C. Tiotropium in the add-on treatment of asthma in adults: Clinical trial evidence and experience. Ther. Adv. Respir. Dis. 2016, 10, 525–533. [Google Scholar] [CrossRef]
- D’Urzo, A.D.; Singh, D.; Donohue, J.F.; Chapman, K.R.; Wise, R.A. Aclidinium bromide/formoterol fumarate as a treatment for COPD: An update. Expert Rev. Respir. Med. 2021, 15, 1093–1106. [Google Scholar] [CrossRef] [PubMed]
- Heo, Y.A. Budesonide/Glycopyrronium/Formoterol: A Review in COPD. Drugs 2021, 81, 1411–1422. [Google Scholar] [CrossRef] [PubMed]
- Solidoro, P.; Patrucco, F.; Bagnasco, D. Comparing a fixed combination of budesonide/formoterol with other inhaled corticosteroid plus long-acting beta-agonist combinations in patients with chronic obstructive pulmonary disease: A review. Expert Rev. Respir. Med. 2019, 13, 1087–1094. [Google Scholar] [CrossRef] [PubMed]
- Tashkin, D.P.; Ferguson, G.T. Combination bronchodilator therapy in the management of chronic obstructive pulmonary disease. Respir. Res. 2013, 14, 49. [Google Scholar] [CrossRef]
- Blair, H.A. Indacaterol/Glycopyrronium/Mometasone: A Review in Asthma. Drugs 2021, 81, 709–719. [Google Scholar] [CrossRef]
- Brittain, D.; Andrea, P.D.; Gruen, E.; Hosoe, M.; Jain, D.; Jauernig, J.; Tillmann, H.C. A Review of the Unique Drug Development Strategy of Indacaterol Acetate/Glycopyrronium Bromide/Mometasone Furoate: A First-in-Class, Once-Daily, Single-Inhaler, Fixed-Dose Combination Treatment for Asthma. Adv. Ther. 2022, 39, 2365–2378. [Google Scholar] [CrossRef]
- Albuquerque, A.A.S.; Carvalho, M.T.M.; Evora, P.M.; De Nadai, T.R.; Celotto, A.C.; Evora, P.R.B. In vitro reactivity (‘organ chamber’) of guinea pig tracheal rings-methodology considerations. Ann. Transl. Med. 2016, 4, 216. [Google Scholar] [CrossRef]
- Matera, M.G.; Page, C.P.; Calzetta, L.; Rogliani, P.; Cazzola, M. Pharmacology and Therapeutics of Bronchodilators Revisited. Pharmacol. Rev. 2020, 72, 218–252. [Google Scholar] [CrossRef] [PubMed]
- Vardanyan, R.S.; Hruby, V.J. Cholinomimetics. In Synthesis of Essential Drugs, 1st ed.; Elsevier: Amsterdam, The Netherlands, 2006; pp. 179–193. [Google Scholar]
- Buels, K.S.; Fryer, A.D. Muscarinic receptor antagonists: Effects on pulmonary function. Handb. Exp. Pharmacol. 2012, 208, 317–341. [Google Scholar] [CrossRef]
- O’Connor, B.; Towes, L.J.; Barnes, P.J. Prolonged Effed of notropium Bromide on Methacholine-induced Bronchoconstridion in Asthma. Am. J. Respir. Crit. Care Med. 1996, 154, 876–880. [Google Scholar] [CrossRef] [PubMed]
- Terzano, C.; Petroianni, A.; Ricci, A.; Antoni, L.D.; Allegra, L. Early protective effects of tiotropium bromide in patients with airways hyperresponsiveness. Eur. Rev. Med. Pharmacol. Sci. 2004, 8, 259–264. [Google Scholar] [PubMed]
- Barisione, G.; Baroffio, M.; Crimi, E.; Brusasco, V. Beta-adrenergic agonists. Pharmaceuticals 2010, 3, 1016–1044. [Google Scholar] [CrossRef] [PubMed]
- Cazzola, M.; Page, C.P.; Calzetta, L.; Matera, M.G. Pharmacology and Therapeutics of Bronchodilators. Pharmacol. Rev. 2012, 64, 450–504. [Google Scholar] [CrossRef]
- Meurs, H.; Oenema, T.A.; Kistemaker, L.E.M.; Gosens, R. A new perspective on muscarinic receptor antagonism in obstructive airways diseases. Curr. Opin. Pharmacol. 2013, 13, 316–323. [Google Scholar] [CrossRef]
- Rhoden, K.J.; Meldrum, L.A.; Barnes, P.J. Inhibition of cholinergic neurotransmission in human airways by β-2 adrenoreceptors. J. Appl. Physiol. 1988, 65, 700–705. [Google Scholar] [CrossRef] [PubMed]
- Roffel, A.F.; Meurs, H.; Elzinga, C.R.S.; Zaagsma, J. Muscarinic M2 receptors do not participate in the functional antagonism between methacholine and isoprenaline in guinea pig tracheal smooth muscle. Eur. J. Pharmacol. 1993, 249, 235–238. [Google Scholar] [CrossRef]
- Torphy, T.J. Differential relaxant effects of isoproterenol on methacholine- versus leukotriene D4-induced contraction in the guinea-pig trachea. Eur. J. Pharmacol. 1984, 102, 549–553. [Google Scholar] [CrossRef]
- Villetti, G.; Bergamaschi, M.; Bassani, F.; Bolzoni, P.T.; Harrison, S.; Gigli, P.M.; Janni, A.; Geppetti, P.; Civelli, M.; Patacchini, R. Pharmacological assessment of the duration of action of glycopyrrolate vs. tiotropium and ipratropium in guinea-pig and human airways. Br. J. Pharmacol. 2006, 148, 291–298. [Google Scholar] [CrossRef] [PubMed]
- Calzetta, L.; Matera, M.G.; Rogliani, P.; Cazzola, M. Dual LABA/LAMA bronchodilators in chronic obstructive pulmonary disease: Why, when, and how. Expert Rev. Respir. Med. 2018, 12, 261–264. [Google Scholar] [CrossRef]
- Lee, M.K.; Lim, K.H.; Millns, P.; Mohankumar, S.K.; Ng, S.T.; Tan, C.S.; Then, S.-M.; Mbaki, Y.; Ting, K.-N. Bronchodilator effects of Lignosus rhinocerotis extract on rat isolated airways is linked to the blockage of calcium entry. Phytomedicine 2018, 42, 172–179. [Google Scholar] [CrossRef] [PubMed]
- Chou, T. Theoretical Basis, Experimental Design, and Computerized Simulation of Synergism and Antagonism in Drug Combination Studies. Pharmacol. Rev. 2006, 58, 621–681. [Google Scholar] [CrossRef] [PubMed]
- Mahler, D.A.; D’Urzo, A.; Bateman, E.D.; Özkan, S.A.; White, T.; Peckitt, C.; Kramer, B. Concurrent use of indacaterol plus tiotropium in patients with COPD provides superior bronchodilation compared with tiotropium alone: A randomised, double-blind comparison. Thorax 2012, 67, 781–788. [Google Scholar] [CrossRef] [PubMed]
- Matsushima, S.; Inui, N.; Yasui, H.; Kono, M.; Nakamura, Y.; Toyoshima, M.; Shirai, T.; Suda, T. Indacaterol and tiotropium combination therapy in patients with chronic obstructive pulmonary disease. Pulm. Pharmacol. Ther. 2015, 30, 11–15. [Google Scholar] [CrossRef]
- Cazzola, M.; Tashkin, D.P. Combination of formoterol and tiotropium in the treatment of COPD: Effects on lung function. COPD J. Chronic Obstr. Pulm. Dis. 2009, 6, 404–415. [Google Scholar] [CrossRef]
- van Noord, J.A.; Aumann, J.L.; Janssens, E.; Smeets, J.J.; Verhaert, J.; Disse, B.; Mueller, A.; Cornelissen, P.J.G. Comparison of tiotropium once daily, formoterol twice daily and both combined once daily in patients with COPD. Eur. Respir. J. 2005, 26, 214–222. [Google Scholar] [CrossRef]
- Foucquier, J.; Guedj, M. Analysis of drug combinations: Current methodological landscape. Pharmacol. Res. Perspect. 2015, 3, e00149. [Google Scholar] [CrossRef]
- Goldoni, M.; Johansson, C.A. Mathematical approach to study combined effects of toxicants in vitro: Evaluation of the Bliss independence criterion and the Loewe additivity model. Toxicol. Vitr. 2007, 21, 759–769. [Google Scholar] [CrossRef] [PubMed]
- Greco, W.R.; Bravo, G.; Parsons, J.C. The Search for Synergy: A Critical Review from a Response Surface Perspective. Am. Soc. Pharmacol. Exp. Ther. 1995, 47, 331–385. [Google Scholar]
- Roell, K.R.; Reif, D.M.; Motsinger-Reif, A.A. An introduction to terminology and methodology of chemical synergy-Perspectives from across disciplines. Front. Pharmacol. 2017, 8, 158. [Google Scholar] [CrossRef] [PubMed]
- Demidenko, E.; Miller, T.W. Statistical determination of synergy based on Bliss definition of drugs independence. PLoS ONE 2019, 14, e0224137. [Google Scholar] [CrossRef] [PubMed]
- Yeh, T.; Wechsler, A.S. Chapter 49 The Isolated Organ in Research. In Surgical Research Basic Principles and Clinical Practice, 3rd ed.; Troidl, H., McKneally, M.F., Mulder, D.S., Wechsler, A.S., McPeek, P., Spitzer, W.O., Eds.; Springer: New York, NY, USA, 1998; pp. 435–452. [Google Scholar] [CrossRef]
- Rosethorne, E.M.; Turner, R.J.; Fairhurst, R.A.; Charlton, S.J. Efficacy is a contributing factor to the clinical onset of bronchodilation of inhaled β2-adrenoceptor agonists. Naunyn. Schmiedebergs. Arch. Pharmacol. 2010, 382, 255–263. [Google Scholar] [CrossRef] [PubMed]
- Battram, C.; Charlton, S.J.; Cuenoud, B.; Dowling, M.R.; Fairhurst, R.A.; Farr, D.; Fozard, J.R.; Leighton-Davies, J.R.; Lewis, C.A.; McEvoy, L.; et al. In vitro and in vivo pharmacological characterization of 5-[(R)-2-(5,6-diethyl-indan-2-ylamino)-1-hydroxy-ethyl]-8-hydroxy-1H-quinolin-2-one (indacaterol), a novel inhaled β2 adrenoceptor agonist with a 24-h duration of action. J. Pharmacol. Exp. Ther. 2006, 317, 762–770. [Google Scholar] [CrossRef] [PubMed]
- Aparici, M.; Carcasona, C.; Ramos, I.; Cortijo, J.; Puig, C.; Vilella, D.; Doe, C.; Gavaldà, A.; Miralpeix, M. Pharmacological preclinical characterization of LAS190792, a novel inhaled bifunctional muscarinic receptor antagonist/b2-adrenoceptor agonist (MABA) molecule. Pulm. Pharmacol. Ther. 2017, 46, 408–410. [Google Scholar] [CrossRef] [PubMed]
- Gomart, S.; Damoiseaux, C.; Jespers, P.; Makanga, M.; Labranche, N.; Pochet, S.; Michaux, C.; Berkenboom, G.; Naeije, R.; McEntee, K.; et al. Pulmonary vasoreactivity in spontaneously hypertensive rats—Effects of endothelin-1 and leptin. Respir. Res. 2014, 15, 1–12. [Google Scholar] [CrossRef]
- de Sousa, A.A.S.; Soares, P.M.G.; de Almeida, A.N.S.; Maia, A.R.; de Souza, E.P.; Assreuy, A.M.S. Antispasmodic effect of Mentha piperita essential oil on tracheal smooth muscle of rats. J. Ethnopharmacol. 2010, 130, 433–436. [Google Scholar] [CrossRef]
- Lam, M.; Royce, S.G.; Donovan, C.; Jelinic, M.; Parry, L.J.; Samuel, C.S.; Bourke, J.E. Serelaxin elicits bronchodilation and enhances β-adrenoceptor-mediated airway relaxation. Front. Pharmacol. 2016, 7, 1–12. [Google Scholar] [CrossRef]
- Mhanna, M.J.; Koester, J.F.; Cohn, R.C. Effects of (R, R)-and (R, R/S, S)—Formoterol on Airway Relaxation and Contraction in an Experimental Rat Model. Curr. Ther. Res. 2007, 68, 249–261. [Google Scholar] [CrossRef] [PubMed]
- Aparici, M.; Gavaldà, A.; Ramos, I.; Carcasona, C.; Otal, R.; Fernández-Blanco, J.A.; Montero, J.L.; García, V.M.; López, R.; de Alba, J.; et al. In vitro and in vivo preclinical profile of abediterol (LAS100977), an inhaled long-acting B2-adrenoreceptor agonist, compared with indacaterol, olodaterol and vilanterol. Eur. J. Pharmacol. 2016, 770, 61–69. [Google Scholar] [CrossRef]
- Lin, Y.-Y.; Chou, Y.-L.; Chu, Y.-H.; Wu, C.-C.; Wang, J.-Y.; Wang, H.-W. Effects of cromolyn sodium on isolated rat’s trachea. Allergy Rhinol. 2011, 2, 46–50. [Google Scholar] [CrossRef] [PubMed]
- Waldman, S.A. Does potency predict clinical efficacy? Illustration through an antihistamine model. Ann. Allergy Asthma Immunol. 2002, 89, 7–12. [Google Scholar] [CrossRef]
- Ericsson, T.; Fridén, M.; Kärrman-mårdh, C.; Dainty, I.; Grime, K. Benchmarking of Human Dose Prediction for Inhaled Medicines from Preclinical In Vivo Data. Pharm. Res. 2017, 34, 2557–2567. [Google Scholar] [CrossRef] [PubMed]
- Petraitis, V.; Petraitiene, R.; Hope, W.W.; Meletiadis, J.; Mickiene, D.; Hughes, J.E.; Cotton, M.P. Combination Therapy in Treatment of Experimental Pulmonary Aspergillosis: In Vitro and In Vivo Correlations of the Concentration- and Dose—Dependent Interactions between Anidulafungin and Voriconazole by Bliss Independence Drug Interaction Analysis. Antimicrob. Agents Chemother. 2009, 53, 2382–2391. [Google Scholar] [CrossRef] [PubMed]
- Zhang, N.; Fu, J.-N.; Chou, T.-C. Synergistic combination of microtubule targeting anticancer fludelone with cytoprotective panaxytriol derived from panax ginseng against MX-1 cells in vitro: Experimental design and data analysis using the combination index method. Am. J. Cancer Res. 2016, 6, 97–104. [Google Scholar] [PubMed]
- Melot, C. Qu’est-ce qu’un intervalle de confiance ? Rev. Mal. Respir. 2003, 20, 599–601. [Google Scholar] [CrossRef] [PubMed]

| A | Tiotropium bromide monohydrate | Formoterol fumarate dihydrate | Relaxant effect (%) | CI | Interaction magnitude |
| 1.55 nM | 0.45 nM | 35.12 | 3.522 | − − − − − | |
| 1.55 nM | 0.90 nM | 69.49 | 0.834 | + + | |
| 1.55 nM | 1.81 nM | 86.51 | 0.294 | + + + + | |
| 1.55 nM | 2.71 nM | 95.34 | 0.102 | + + + + | |
| 1.55 nM | 3.62 nM | 98.64 | 0.035 | + + + + + | |
| 1.55 nM | 7.24 nM | 99.3 | 0.020 | + + + + + | |
| 1.55 nM | 9.04 nM | 99.7 | 0.009 | + + + + + | |
| B | Tiotropium bromide monohydrate | Formoterol fumarate dihydrate | Relaxant effect (%) | CI | Interaction magnitude |
| 0.41 nM | 0.12 nM | 10.49 | 2.158 | − − − − | |
| 0.61 nM | 0.35 nM | 33.20 | 1.174 | − − | |
| 0.81 nM | 0.94 nM | 59.17 | 0.652 | + + + | |
| 1.02 nM | 1.79 nM | 79.21 | 0.337 | + + + | |
| 1.55 nM | 3.62 nM | 91.34 | 0.183 | + + + + | |
| 2.08 nM | 9.69 nM | 97.35 | 0.080 | + + + + + | |
| 2.60 nM | 15.19 nM | 99.59 | 0.060 | + + + + + | |
| C | Tiotropium bromide monohydrate | Indacaterol maleate | Relaxant effect (%) | CI | Interaction magnitude |
| 1.55 nM | 1.50 nM | 36445,00 | 3.865 | − − − − − | |
| 1.55 nM | 2.99 nM | 69.54 | 0.928 | + | |
| 1.55 nM | 7.48 nM | 83.93 | 0.385 | + + + | |
| 1.55 nM | 14.96 nM | 91.03 | 0.190 | + + + + | |
| 1.55 nM | 29.91 nM | 96.59 | 0.076 | + + + + + | |
| 1.55 nM | 59.82 nM | 99.06 | 0.025 | + + + + + | |
| 1.55 nM | 74.78 nM | 99.64 | 0.011 | + + + + + | |
| 1.55 nM | 0.15 mM | 99.86 | 0.005 | + + + + + | |
| D | Tiotropium bromide monohydrate | Indacaterol maleate | Relaxant effect (%) | CI | Interaction magnitude |
| 0.41 nM | 0.39 nM | 9.92 | 18.707 | − − − − − − | |
| 0.61 nM | 1.17 nM | 27.91 | 1.779 | − − − − | |
| 0.81 nM | 3.90 nM | 48.10 | 0.895 | + | |
| 1.02 nM | 9.88 nM | 71.56 | 0.440 | + + + | |
| 1.55 nM | 29.91 nM | 90.30 | 0.203 | + + + + | |
| 2.08 nM | 80.14 nM | 97.99 | 0.067 | + + + + + | |
| 2.60 nM | 0.13 mM | 99.12 | 0.041 | + + + + + | |
| 3.13 nM | 0.30 mM | 99,59 | 0.025 | + + + + + |
| DRI50 | |||
|---|---|---|---|
| LABA/LAMA Combination | TIO | FOR | IND |
| FOR/TIO 2:1 (w/w) | 1.38 | 4 338 | / |
| FOR/TIO 3:1 (w/w) | 1.23 | 2 586 | / |
| IND/TIO 10:1 (w/w) | 1.27 | / | 4 484 |
| IND/TIO 20:1 (w/w) | 1.35 | / | 2 370 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Menchi, E.; El Khattabi, C.; Pochet, S.; Denis, O.; Amighi, K.; Wauthoz, N. Optimization of Long-Acting Bronchodilator Dose Ratios Using Isolated Guinea Pig Tracheal Rings for Synergistic Combination Therapy in Asthma and COPD. Pharmaceuticals 2022, 15, 963. https://doi.org/10.3390/ph15080963
Menchi E, El Khattabi C, Pochet S, Denis O, Amighi K, Wauthoz N. Optimization of Long-Acting Bronchodilator Dose Ratios Using Isolated Guinea Pig Tracheal Rings for Synergistic Combination Therapy in Asthma and COPD. Pharmaceuticals. 2022; 15(8):963. https://doi.org/10.3390/ph15080963
Chicago/Turabian StyleMenchi, Elena, Charaf El Khattabi, Stéphanie Pochet, Olivier Denis, Karim Amighi, and Nathalie Wauthoz. 2022. "Optimization of Long-Acting Bronchodilator Dose Ratios Using Isolated Guinea Pig Tracheal Rings for Synergistic Combination Therapy in Asthma and COPD" Pharmaceuticals 15, no. 8: 963. https://doi.org/10.3390/ph15080963
APA StyleMenchi, E., El Khattabi, C., Pochet, S., Denis, O., Amighi, K., & Wauthoz, N. (2022). Optimization of Long-Acting Bronchodilator Dose Ratios Using Isolated Guinea Pig Tracheal Rings for Synergistic Combination Therapy in Asthma and COPD. Pharmaceuticals, 15(8), 963. https://doi.org/10.3390/ph15080963







