Development of a Self-Assembled Hydrogels Based on Carboxymethyl Chitosan and Oxidized Hyaluronic Acid Containing Tanshinone Extract Nanocrystals for Enhanced Dissolution and Acne Treatment
Abstract
1. Introduction
2. Results and Discussions
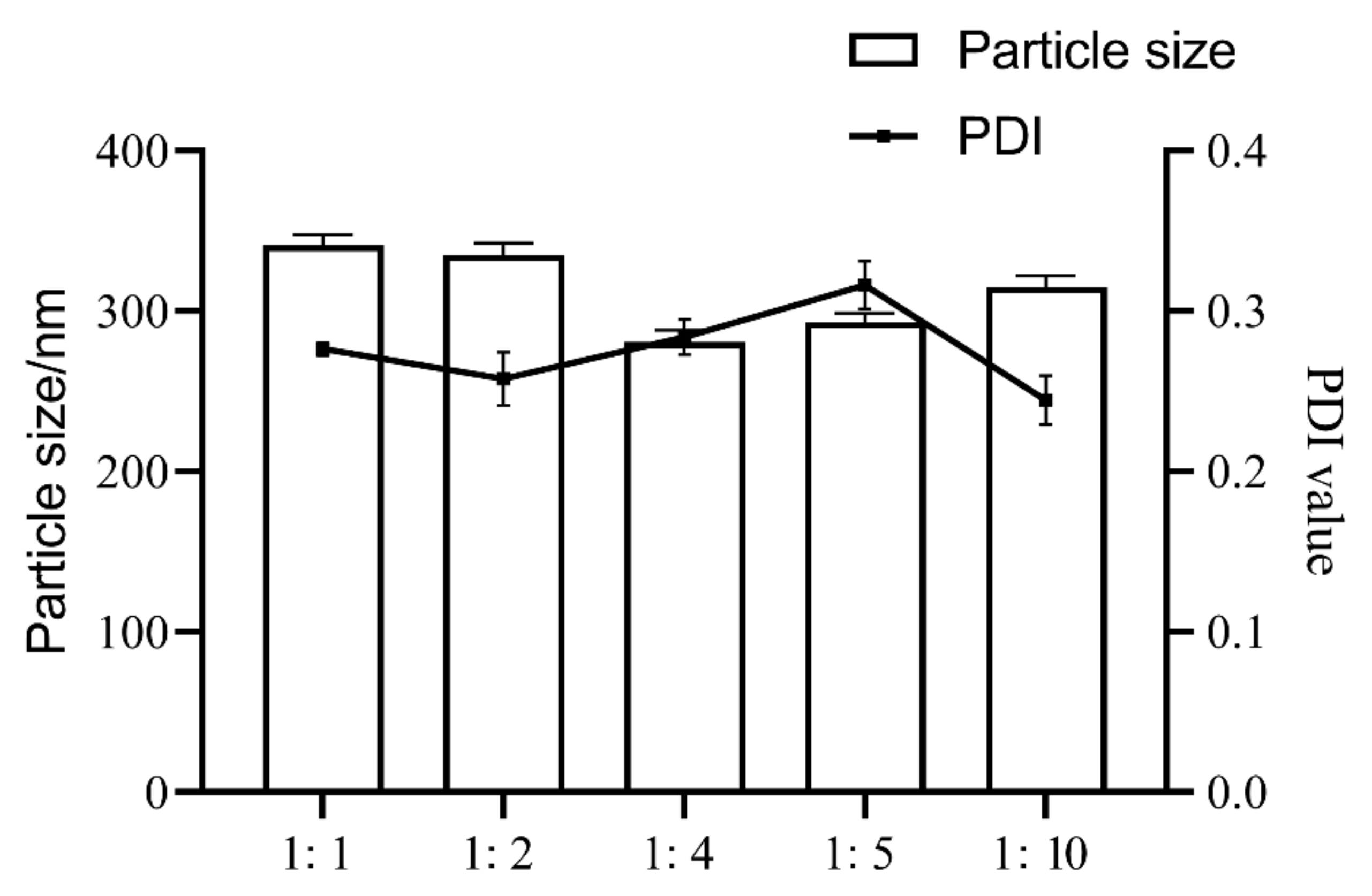
2.1. Optimization of TNCs Prescriptions
2.2. Optimization of TNC Processes
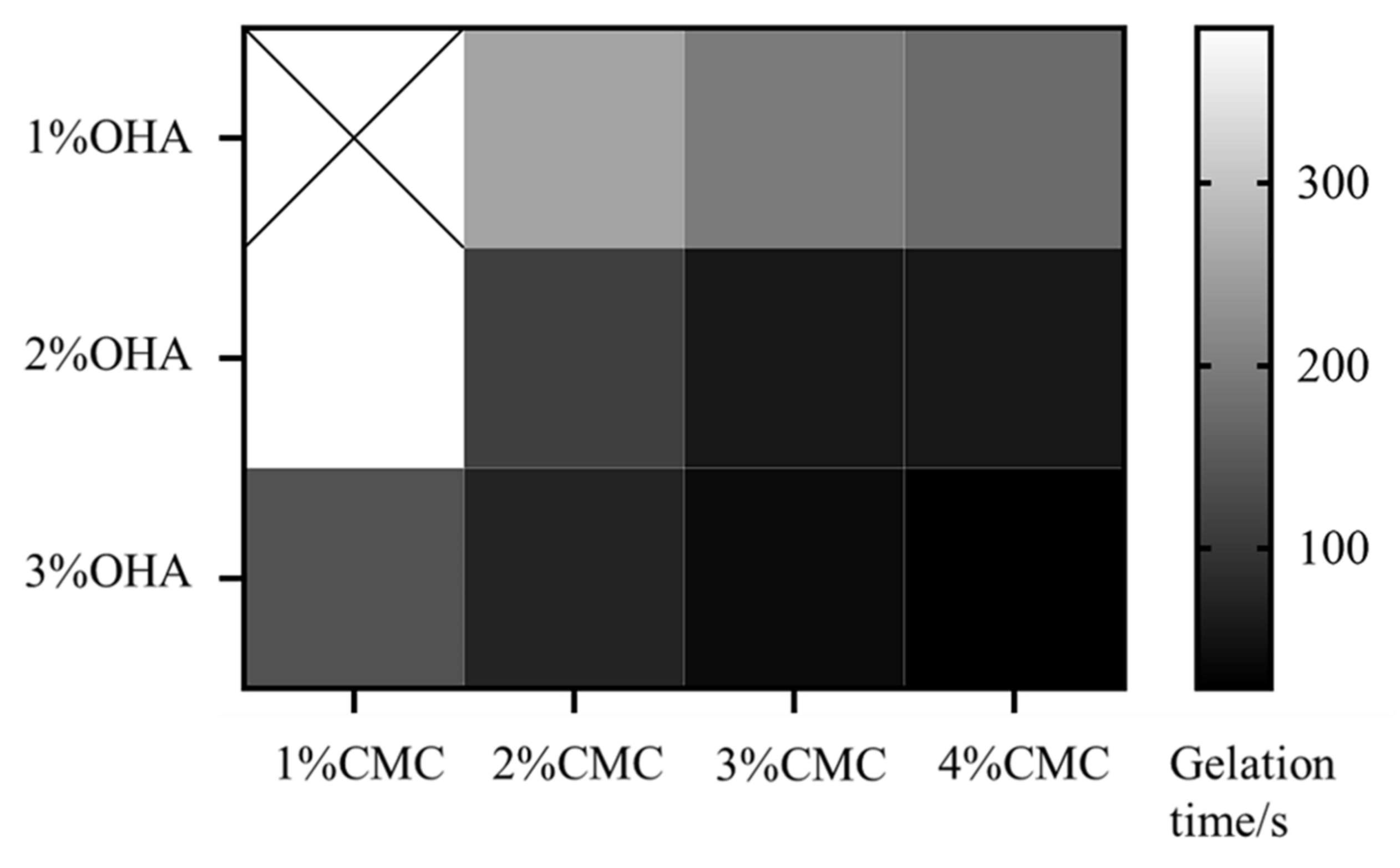
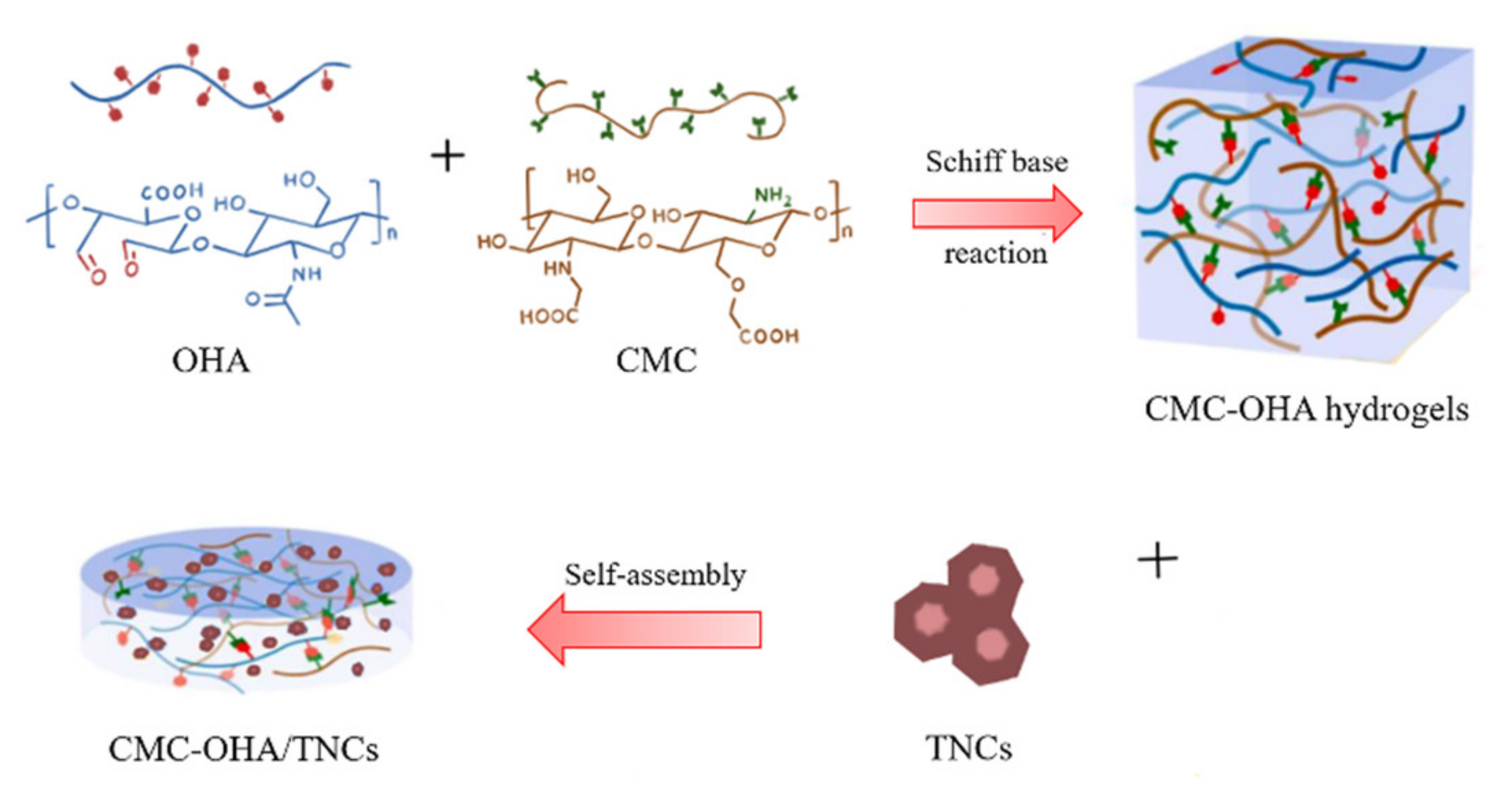
2.3. Preparation and Characterization of CMC-OHA/TNCs
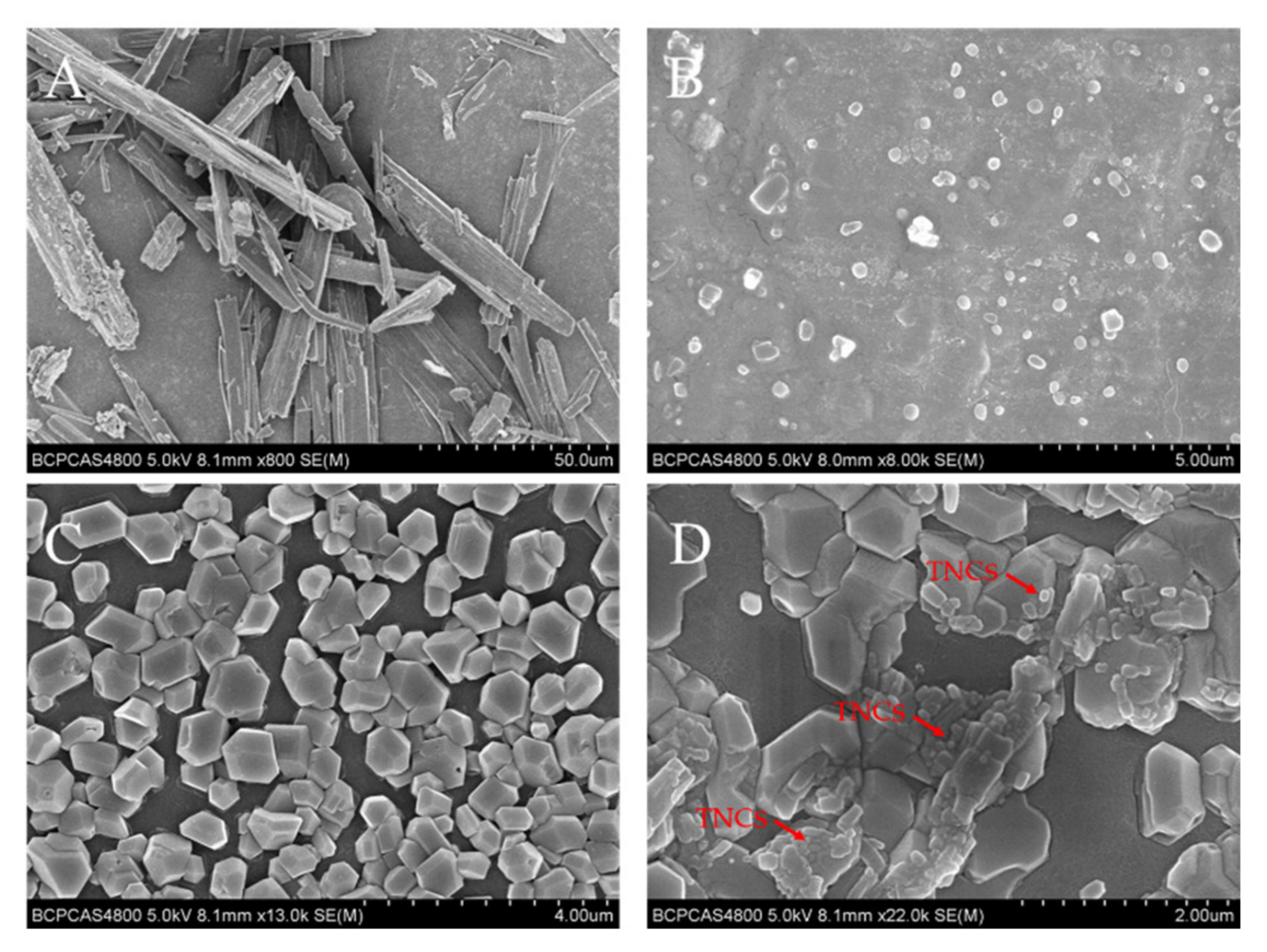
2.4. Morphology of CMC-OHA/TNCs
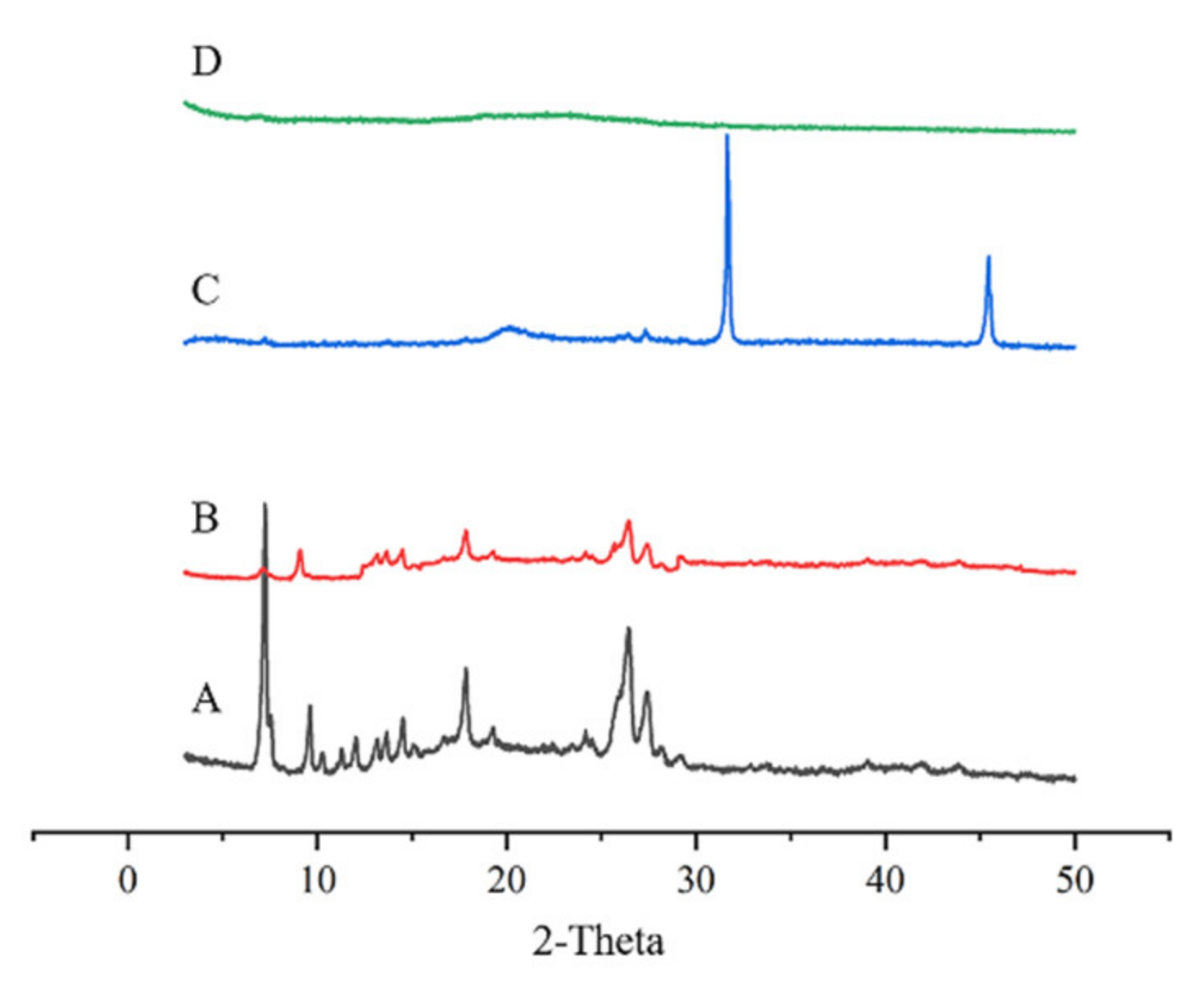
2.5. X-ray Powder Diffraction (XRD) of CMC-OHA/TNCs
2.6. In Vitro Transdermal Assays
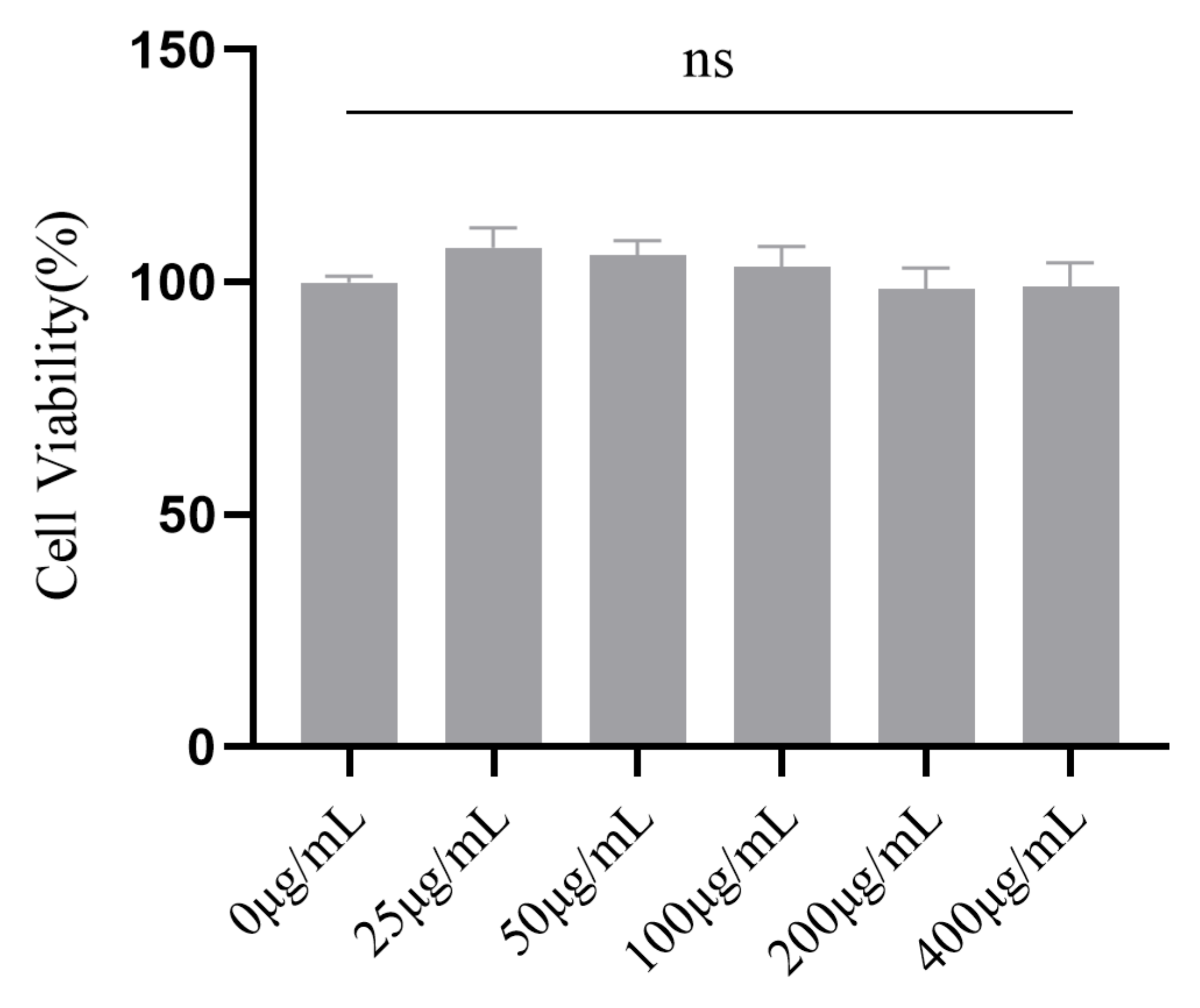
2.7. In Vitro Cytotoxicity of CMC-OHA/TNCs
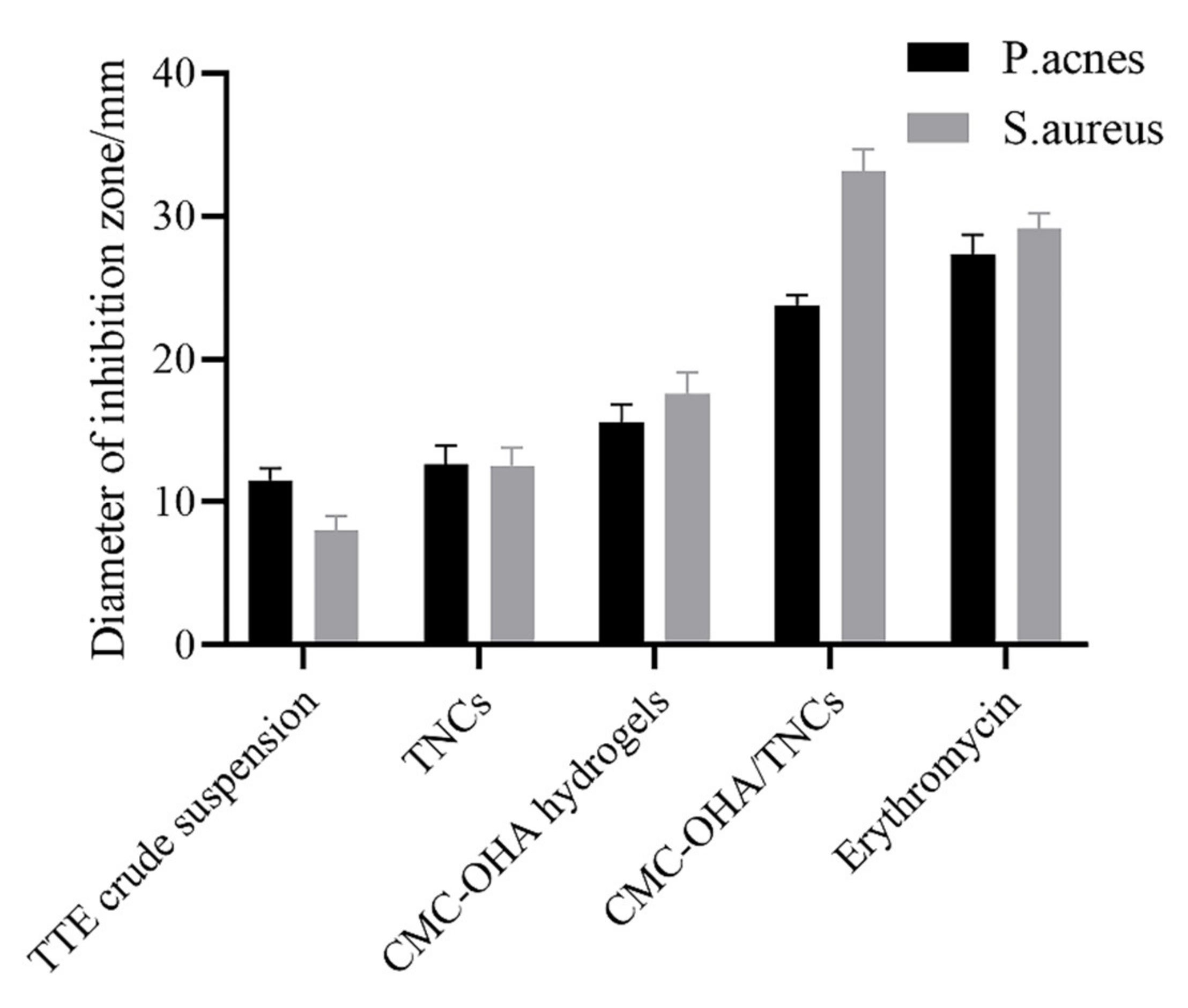
2.8. In Vitro Antibacterial Activity Assay
3. Materials and Methods
3.1. Materials
3.2. Preparation of TNCs
3.3. Optimization of Prescriptions and Processes for TNCs
3.4. Particle Size and Determination
3.5. Synthesis and Fourier Transform Infrared Spectroscopy (FTIR) Analysis of OHA
3.6. Preparation of CMC-OHA/TNCs
3.7. Morphology of CMC-OHA/TNCs
3.8. X-ray Powder Diffraction (XRD) of CMC-OHA/TNCs
3.9. Determination of Cryptotanshinone and Tanshinone IIA
3.10. In Vitro Transdermal Permeation
3.11. CCK-8 Assay
3.12. In Vitro Antibacterial Activity Assay
3.13. Statistical Analysis
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
References
- Juhl, C.R.; Bergholdt, H.K.M.; Miller, I.M.; Jemec, G.B.E.; Kanters, J.K.; Ellervik, C. Lactase Persistence, Milk Intake, and Adult Acne: A Mendelian Randomization Study of 20,416 Danish Adults. Nutrients 2018, 10, 1041. [Google Scholar] [CrossRef] [PubMed]
- Yang, Z.; Zhang, Y.; Lazic Mosler, E.; Hu, J.; Li, H.; Zhang, Y.; Liu, J.; Zhang, Q. Topical benzoyl peroxide for acne. Cochrane Database Syst. Rev. 2020, 3, CD011154. [Google Scholar] [CrossRef]
- Wang, Y.-Y.; Ryu, A.R.; Jin, S.; Jeon, Y.-M.; Lee, M.-Y. Chlorin e6-Mediated Photodynamic Therapy Suppresses P. acnes-Induced Inflammatory Response via NFκB and MAPKs Signaling Pathway. PLoS ONE 2017, 12, e0170599. [Google Scholar] [CrossRef] [PubMed]
- Chuang, L.-T.; Shih, Y.-H.; Huang, W.-C.; Lin, L.-C.; Hsu, C.; Chyuan, J.-H.; Tsai, T.-H.; Tsai, P.-J. In Vitro and In Vivo Screening of Wild Bitter Melon Leaf for Anti-Inflammatory Activity against Cutibacterium acnes. Molecules 2020, 25, 4277. [Google Scholar] [CrossRef] [PubMed]
- Frade, M.L.; de Annunzio, S.R.; Calixto, G.M.F.; Victorelli, F.D.; Chorilli, M.; Fontana, C.R. Assessment of Chitosan-Based Hydrogel and Photodynamic Inactivation against Propionibacterium acnes. Molecules 2018, 23, 473. [Google Scholar] [CrossRef] [PubMed]
- Say, Y.-H.; Heng, A.H.S.; Reginald, K.; Wong, Y.R.; Teh, K.F.; Rawanan Shah, S.M.; Sio, Y.Y.; Ng, Y.T.; Matta, S.A.; Pang, S.L.; et al. Modifiable and non-modifiable epidemiological risk factors for acne, acne severity and acne scarring among Malaysian Chinese: A cross-sectional study. BMC Public Health 2021, 21, 601. [Google Scholar] [CrossRef]
- Marito, S.; Keshari, S.; Traisaeng, S.; My, D.T.T.; Balasubramaniam, A.; Adi, P.; Hsieh, M.-F.; Herr, D.R.; Huang, C.-M. Electricity-producing Staphylococcus epidermidis counteracts Cutibacterium acnes. Sci. Rep. 2021, 11, 12001. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Xi, P.; Wang, T.; Miao, M.S. Effect of Total Alkali in Leonuri Herba on rat ear acne model of serum IL-6 level, Thymus and Spleen Tissue Morphology. Saudi J. Biol. Sci. 2017, 24, 718–723. [Google Scholar] [CrossRef]
- Chen, T.; Zhu, Z.; Du, Q.; Wang, Z.; Wu, W.; Xue, Y.; Wang, Y.; Wu, Y.; Zeng, Q.; Jiang, C.; et al. A Skin Lipidomics Study Reveals the Therapeutic Effects of Tanshinones in a Rat Model of Acne. Front. Pharmacol. 2021, 12, 675659. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Zhou, Y. The therapeutic effect of tanshinone IIA on Propionibacterium acnes-induced inflammation in vitro. Dermatol. Ther. 2018, 31, e12716. [Google Scholar] [CrossRef]
- Yao, Y.; Zuo, J.; Chen, L. Clinical efficacy of tanshinone capsules combined with varying concentrations of 5-ALA-PDT in the treatment of cystic acne. Am. J. Transl. Res. 2021, 13, 10816–10822. [Google Scholar]
- Liu, Y.C.; Lin, M.T.; Ng, A.H.C.; Wong, T.T.; Mehta, J.S. Nanotechnology for the Treatment of Allergic Conjunctival Diseases. Pharmaceuticals 2020, 13, 351. [Google Scholar] [CrossRef] [PubMed]
- Romero, G.B.; Arntjen, A.; Keck, C.M.; Müller, R.H. Amorphous cyclosporin A nanoparticles for enhanced dermal bioavailability. Int. J. Pharm. 2016, 498, 217–224. [Google Scholar] [CrossRef] [PubMed]
- Navarro-Partida, J.; Castro-Castaneda, C.R.; Santa Cruz-Pavlovich, F.J.; Aceves-Franco, L.A.; Guy, T.O.; Santos, A. Lipid-Based Nanocarriers as Topical Drug Delivery Systems for Intraocular Diseases. Pharmaceutics 2021, 13, 678. [Google Scholar] [CrossRef] [PubMed]
- Xie, Y.; Chen, Z.; Su, R.; Li, Y.; Qi, J.; Wu, W.; Lu, Y. Preparation and Optimization of Amorphous Ursodeoxycholic Acid Nano-suspensions by Nanoprecipitation based on Acid-base Neutralization for Enhanced Dissolution. Curr. Drug Deliv. 2017, 14, 483–491. [Google Scholar] [CrossRef]
- Abd-Elsalam, W.H.; El-Zahaby, S.A.; Al-Mahallawi, A.M. Formulation and in vivo assessment of terconazole-loaded polymeric mixed micelles enriched with Cremophor EL as dual functioning mediator for augmenting physical stability and skin delivery. Drug Deliv. 2018, 25, 484–492. [Google Scholar] [CrossRef]
- Hatahet, T.; Morille, M.; Hommoss, A.; Dorandeu, C.; Müller, R.H.; Bégu, S. Dermal quercetin smartCrystals®: Formulation development, antioxidant activity and cellular safety. Eur. J. Pharm. Biopharm. Off. J. Arb. Fur Pharm. Verfahr. EV 2016, 102, 51–63. [Google Scholar] [CrossRef]
- Liu, X.; Gan, H.; Hu, C.; Sun, W.; Zhu, X.; Meng, Z.; Gu, R.; Wu, Z.; Dou, G. Silver sulfadiazine nanosuspension-loaded thermosensitive hydrogel as a topical antibacterial agent. Int. J. Nanomed. 2019, 14, 289–300. [Google Scholar] [CrossRef] [PubMed]
- Sánchez, N.; González-Ramírez, M.C.; Contreras, E.G.; Ubilla, A.; Li, J.; Valencia, A.; Wilson, A.; Green, J.B.A.; Tucker, A.S.; Gaete, M. Balance Between Tooth Size and Tooth Number Is Controlled by Hyaluronan. Front. Physiol. 2020, 11, 996. [Google Scholar] [CrossRef]
- Sip, S.; Paczkowska-Walendowska, M.; Rosiak, N.; Miklaszewski, A.; Grabańska-Martyńska, K.; Samarzewska, K.; Cielecka-Piontek, J. Chitosan as Valuable Excipient for Oral and Topical Carvedilol Delivery Systems. Pharmaceuticals 2021, 14, 712. [Google Scholar] [CrossRef] [PubMed]
- Song, F.; Kong, Y.; Shao, C.; Cheng, Y.; Lu, J.; Tao, Y.; Du, J.; Wang, H. Chitosan-based multifunctional flexible hemostatic bio-hydrogel. Acta Biomater. 2021, 136, 170–183. [Google Scholar] [CrossRef]
- Morello, G.; Quarta, A.; Gaballo, A.; Moroni, L.; Gigli, G.; Polini, A.; Gervaso, F. A thermo-sensitive chitosan/pectin hydrogel for long-term tumor spheroid culture. Carbohydr. Polym. 2021, 274, 118633. [Google Scholar] [CrossRef]
- Kumar, V.; Kumar, R.; Jain, V.K.; Nagpal, S. Preparation and characterization of nanocurcumin based hybrid virosomes as a drug delivery vehicle with enhanced anticancerous activity and reduced toxicity. Sci. Rep. 2021, 11, 368. [Google Scholar] [CrossRef]
- Zhang, R.; Li, X.; He, K.; Sheng, X.; Deng, S.; Shen, Y.; Chang, G.; Ye, X. Preparation and properties of redox responsive modified hyaluronic acid hydrogels for drug release. Polym. Adv. Technol. 2017, 28, 759–763. [Google Scholar] [CrossRef]
- Pyo, S.M.; Hespeler, D.; Keck, C.M.; Müller, R.H. Dermal miconazole nitrate nanocrystals—Formulation development, increased antifungal efficacy & skin penetration. Int. J. Pharm. 2017, 531, 350–359. [Google Scholar] [CrossRef]
- Zhou, Y.; Fang, Q.; Niu, B.; Wu, B.; Zhao, Y.; Quan, G.; Pan, X.; Wu, C. Comparative studies on amphotericin B nanosuspensions prepared by a high pressure homogenization method and an antisolvent precipitation method. Colloids Surf. B Biointerfaces 2018, 172, 372–379. [Google Scholar] [CrossRef] [PubMed]
- Wu, M.; Chen, J.; Huang, W.; Yan, B.; Peng, Q.; Liu, J.; Chen, L.; Zeng, H. Injectable and Self-Healing Nanocomposite Hydrogels with Ultrasensitive pH-Responsiveness and Tunable Mechanical Properties: Implications for Controlled Drug Delivery. Biomacromolecules 2020, 21, 2409–2420. [Google Scholar] [CrossRef] [PubMed]
- Nagase, S.; Ogai, K.; Urai, T.; Shibata, K.; Matsubara, E.; Mukai, K.; Matsue, M.; Mori, Y.; Aoki, M.; Arisandi, D.; et al. Distinct Skin Microbiome and Skin Physiological Functions between Bedridden Older Patients and Healthy People: A Single-Center Study in Japan. Front. Med. 2020, 7, 101. [Google Scholar] [CrossRef]
- Qian, C.; Zhang, T.; Gravesande, J.; Baysah, C.; Song, X.; Xing, J. Injectable and self-healing polysaccharide-based hydrogel for pH-responsive drug release. Int. J. Biol. Macromol. 2019, 123, 140–148. [Google Scholar] [CrossRef] [PubMed]
- Turakhia, B.; Chikkala, S.; Shah, S. Novelty of Bioengineered Iron Nanoparticles in Nanocoated Surgical Cotton: A Green Chemistry. Adv. Pharmacol. Sci. 2019, 2019, 9825969. [Google Scholar] [CrossRef] [PubMed]
- Pestov, A.V.; Mehaev, A.V.; Kodess, M.I.; Ezhikova, M.A.; Azarova, Y.A.; Bratskaya, S.Y. Imidazolyl derivative of chitosan with high substitution degree: Synthesis, characterization and sorption properties. Carbohydr. Polym. 2016, 138, 252. [Google Scholar] [CrossRef] [PubMed]
- Chrząszcz, M.; Miazga-Karska, M.; Klimek, K.; Granica, S.; Tchórzewska, D.; Ginalska, G.; Szewczyk, K. Extracts from Cephalaria Uralensis (Murray) Roem. & Schult. and Cephalaria Gigantea (Ledeb.) Bobrov as Potential Agents for Treatment of Acne Vulgaris: Chemical Characterization and In Vitro Biological Evaluation. Antioxidants 2020, 9, 796. [Google Scholar] [CrossRef] [PubMed]
- Tyner, H.; Patel, R. Propionibacterium acnes biofilm—A sanctuary for Staphylococcus aureus? Anaerobe 2016, 40, 63–67. [Google Scholar] [CrossRef] [PubMed]
- Tomić, I.; Miočić, S.; Pepić, I.; Šimić, D.; Filipović-Grčić, J. Efficacy and Safety of Azelaic Acid Nanocrystal-Loaded In Situ Hydrogel in the Treatment of Acne Vulgaris. Pharmaceutics 2021, 13, 567. [Google Scholar] [CrossRef] [PubMed]
- Pineau, R.M.; Hanson, S.E.; Lyles, J.T.; Quave, C.L. Growth Inhibitory Activity of Callicarpa americana Leaf Extracts against Cutibacterium acnes. Front. Pharmacol. 2019, 10, 1206. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.; Oh, S.; Noh, H.B.; Ji, S.; Lee, S.H.; Koo, J.M.; Choi, C.W.; Jhun, H.P. In Vitro Antioxidant and Anti-Propionibacterium acnes Activities of Cold Water, Hot Water, and Methanol Extracts, and Their Respective Ethyl Acetate Fractions, from Sanguisorba officinalis L. Roots. Molecules 2018, 23, 3001. [Google Scholar] [CrossRef]
- Li, X.-X.; Zheng, X.; Liu, Z.; Xu, Q.; Tang, H.; Feng, J.; Yang, S.; Vong, C.T.; Gao, H.; Wang, Y. Cryptotanshinone from Salvia miltiorrhiza Bunge (Danshen) inhibited inflammatory responses via TLR4/MyD88 signaling pathway. Chin. Med. 2020, 15, 20. [Google Scholar] [CrossRef]
- Hu, B.; Gao, M.; Boakye-Yiadom, K.O.; Ho, W.; Yu, W.; Xu, X.; Zhang, X.Q. An intrinsically bioactive hydrogel with on-demand drug release behaviors for diabetic wound healing. Bioact. Mater. 2021, 6, 592–606. [Google Scholar] [CrossRef] [PubMed]
- Neutelings, T.; Nusgens, B.V.; Liu, Y.; Tavella, S.; Ruggiu, A.; Cancedda, R.; Gabriel, M.; Colige, A.; Lambert, C. Skin physiology in microgravity: A 3-month stay aboard ISS induces dermal atrophy and affects cutaneous muscle and hair follicles cycling in mice. NPJ Microgravity 2015, 1, 15002. [Google Scholar] [CrossRef]
- Tolentino, S.; Pereira, M.N.; Cunha-Filho, M.; Gratieri, T.; Gelfuso, G.M. Targeted clindamycin delivery to pilosebaceous units by chitosan or hyaluronic acid nanoparticles for improved topical treatment of acne vulgaris. Carbohydr. Polym. 2021, 253, 117295. [Google Scholar] [CrossRef]

 , design points above predicted value; ○, design points below predicted value.
, design points above predicted value; ○, design points below predicted value.
 , design points above predicted value; ○, design points below predicted value.
, design points above predicted value; ○, design points below predicted value.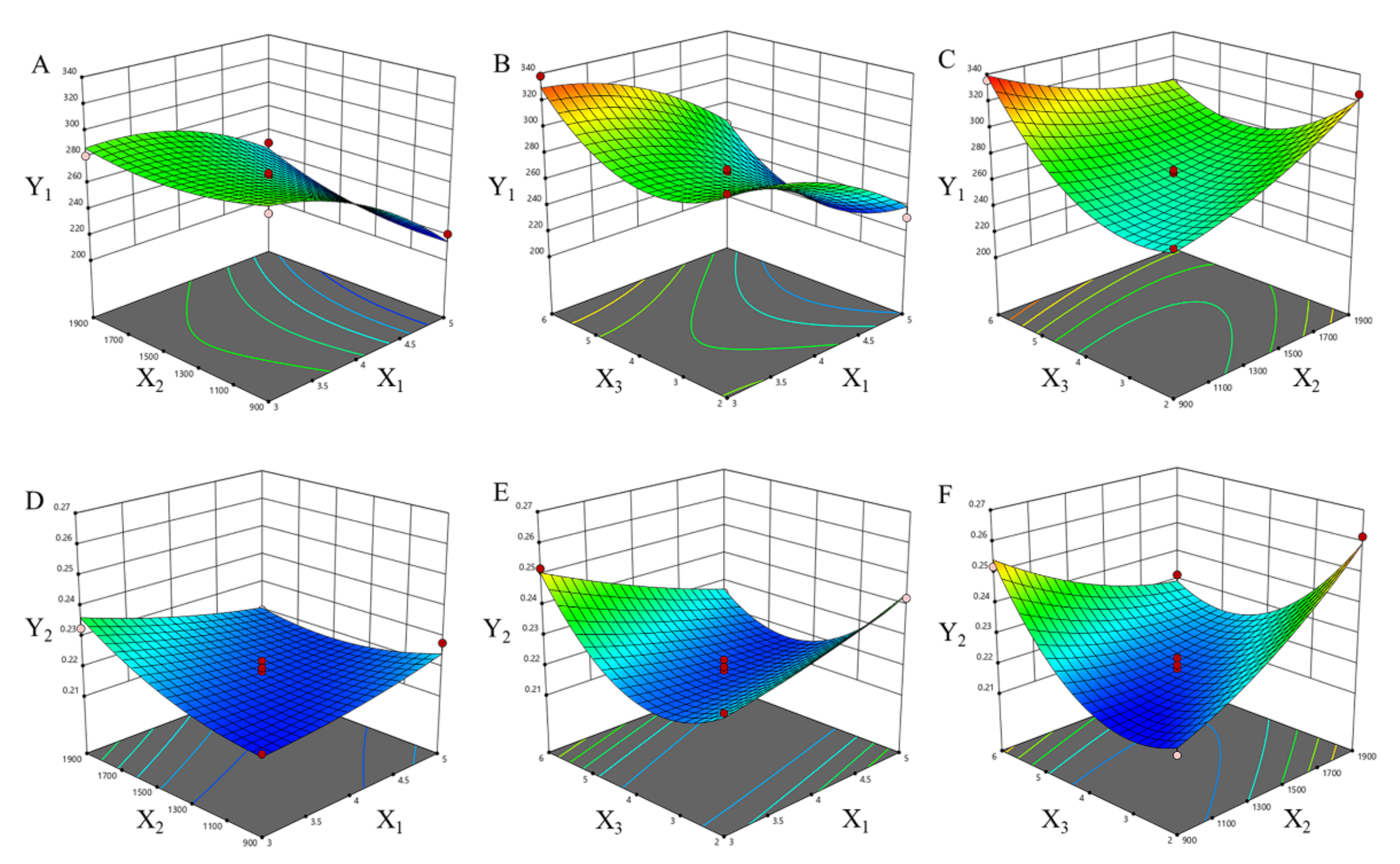



| Run | Independent Variables | Response Value | |||
|---|---|---|---|---|---|
| X1 (mL) | X2 (rpm) | X3 (h) | Y1 (nm) | Y2 | |
| 1 | 3 | 1400 | 4 | 281.2 | 0.2328 |
| 2 | 4 | 900 | 6 | 335.5 | 0.2520 |
| 3 | 4 | 900 | 2 | 260.6 | 0.2148 |
| 4 | 4 | 1400 | 4 | 267.5 | 0.2220 |
| 5 | 5 | 900 | 4 | 220.8 | 0.2280 |
| 6 | 4 | 1900 | 6 | 297.9 | 0.2316 |
| 7 | 5 | 1400 | 6 | 262.8 | 0.2256 |
| 8 | 0 | 1900 | 2 | 325.2 | 0.2616 |
| 9 | 5 | 1400 | 2 | 230.8 | 0.2424 |
| 10 | 3 | 1400 | 6 | 338.0 | 0.2520 |
| 11 | 4 | 1400 | 4 | 264.8 | 0.2196 |
| 12 | 4 | 1400 | 4 | 266.1 | 0.2148 |
| 13 | 5 | 1900 | 4 | 249.6 | 0.2196 |
| 14 | 4 | 1400 | 4 | 257.9 | 0.2184 |
| 15 | 3 | 900 | 4 | 286.4 | 0.2160 |
| 16 | 3 | 1400 | 2 | 297.0 | 0.2280 |
| 17 | 4 | 1400 | 4 | 268.5 | 0.2148 |
| Variables | p-Value | |
|---|---|---|
| Y1 | Y2 | |
| Model | <0.0001 | 0.0001 |
| X1 | <0.0001 | 0.2440 |
| X2 | 0.0488 | 0.0122 |
| X3 | 0.0008 | 0.2079 |
| X1X2 | 0.0581 | 0.0109 |
| X1X3 | 0.5657 | 0.0009 |
| X2X3 | 0.0003 | <0.0001 |
| X12 | 0.0065 | 0.4034 |
| X22 | 0.0511 | 0.0372 |
| X32 | <0.0001 | <0.0001 |
| R2 | 0.9776 | 0.9727 |
| Formulation | Concentration (μg/mL) | |||
|---|---|---|---|---|
| P. acnes | S. aureus | |||
| MIC | MBC | MIC | MBC | |
| TE crude suspension | 125 | 250 | 125 | 64 |
| TNCs | 31 | 63 | 63 | 63 |
| CMC-OHA/TNCs | 16 | 63 | 31 | 31 |
| Level | |||
|---|---|---|---|
| Low (−1) | Medium (0) | High (+1) | |
| Independent variables | |||
| The amount of grinding media | 3 | 4 | 5 |
| Grinding media | 900 | 1400 | 1900 |
| Grinding media | 2 | 4 | 6 |
| Dependent variables | Constraints | ||
| Y1 = Particle size(nm) | Minimize Minimize | ||
| Y2 = PDI | |||
| Diameter of Inhibitory Zones | Sensitivity | Score |
|---|---|---|
| Diameter > 20 mm | Extremely sensitive | 4 |
| 20 mm > Diameter ≥ 15 mm | Highly sensitive | 3 |
| 15 mm > Diameter ≥ 10 mm | Medium sensitivity | 2 |
| 10 mm > Diameter ≥ 7 mm | Hypersensitive | 1 |
| 7 mm > Diameter | Insensitive | 0 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tang, X.; Liu, Y.; Yuan, H.; Gao, R. Development of a Self-Assembled Hydrogels Based on Carboxymethyl Chitosan and Oxidized Hyaluronic Acid Containing Tanshinone Extract Nanocrystals for Enhanced Dissolution and Acne Treatment. Pharmaceuticals 2022, 15, 1534. https://doi.org/10.3390/ph15121534
Tang X, Liu Y, Yuan H, Gao R. Development of a Self-Assembled Hydrogels Based on Carboxymethyl Chitosan and Oxidized Hyaluronic Acid Containing Tanshinone Extract Nanocrystals for Enhanced Dissolution and Acne Treatment. Pharmaceuticals. 2022; 15(12):1534. https://doi.org/10.3390/ph15121534
Chicago/Turabian StyleTang, Xiaohan, Yan Liu, Hailong Yuan, and Rong Gao. 2022. "Development of a Self-Assembled Hydrogels Based on Carboxymethyl Chitosan and Oxidized Hyaluronic Acid Containing Tanshinone Extract Nanocrystals for Enhanced Dissolution and Acne Treatment" Pharmaceuticals 15, no. 12: 1534. https://doi.org/10.3390/ph15121534
APA StyleTang, X., Liu, Y., Yuan, H., & Gao, R. (2022). Development of a Self-Assembled Hydrogels Based on Carboxymethyl Chitosan and Oxidized Hyaluronic Acid Containing Tanshinone Extract Nanocrystals for Enhanced Dissolution and Acne Treatment. Pharmaceuticals, 15(12), 1534. https://doi.org/10.3390/ph15121534






