Lactic Acidosis Related to Pharmacotherapy and Human Diseases
Abstract
1. Introduction
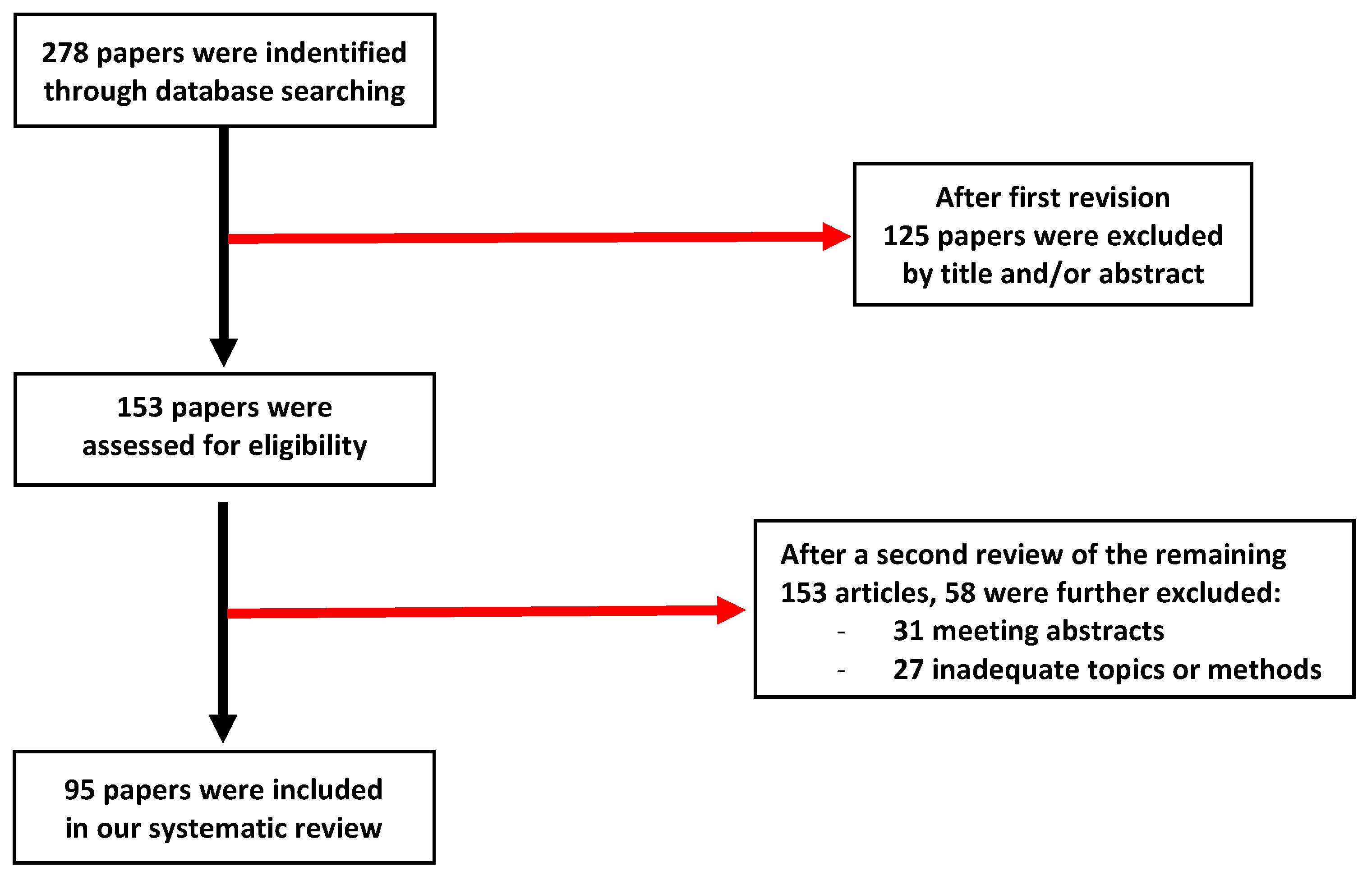
2. Material and Methods
2.1. Levo-Lactate and Destro-Lactate
2.2. Levo-Lactic Acidosis
2.3. Type A: Levo-Lactic Acidosis Related to Low DO2
2.4. Type B1: Levo-Lactic Acidosis Related to Underlying Disease and Type B3: Levo-Lactic Acidosis Related to Altered Lactate Metabolism
2.5. L-Lactic Acidosis Related to Medications
2.6. Treatment
3. Results and Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Gharipour, A.; Razavi, R.; Gharipour, M.; Modarres, R.; Nezafati, P.; Mirkheshti, N. The incidence and outcome of severe hyperlactatemia in critically ill patients. Intern. Emerg. Med. 2021, 16, 115–123. [Google Scholar] [CrossRef] [PubMed]
- Piccioni, A.; Saviano, A.; Cicchinelli, S.; Valletta, F.; Santoro, M.C.; de Cunzo, T.; Zanza, C.; Longhitano, Y.; Tullo, G.; Tilli, P.; et al. Proadrenomedullin in Sepsis and Septic Shock: A Role in the Emergency Department. Medicina 2021, 57, 920. [Google Scholar] [CrossRef] [PubMed]
- Gunnerson, K.J.; Saul, M.; He, S.; Kellum, J.A. Lactate versus non-lactate metabolic acidosis: A retrospective outcome evaluation of critically ill patients. Crit. Care 2006, 10, 1–9. [Google Scholar] [CrossRef]
- Pohanka, M. D-Lactic Acid as a Metabolite: Toxicology, Diagnosis, and Detection. Biomed Res. Int. 2020, 2020, 3419034. [Google Scholar] [CrossRef] [PubMed]
- Evans, O.B.; Stacpoole, P.W. Prolonged hypolactatemia and increased total pyruvate dehydrogenase activity by dichloroacetate. Biochem. Pharmacol. 1982, 31, 1295–1300. [Google Scholar] [CrossRef] [PubMed]
- Merrells, R.J.; Cripps, A.J.; Chivers PTFournier, P.A. Role of lactic acidosis as a mediator of sprint-mediated nausea. Physiol. Rep. 2019, 7, e14283. [Google Scholar] [CrossRef] [PubMed]
- Theobald, J.; Schneider, J.; Cheema, N.; DesLauriers, C. Time to development of metformin-associated lactic acidosis. Clin. Toxicol. 2020, 58, 758–762. [Google Scholar] [CrossRef] [PubMed]
- Zanza, C.; Thangathurai, J.; Audo, A.; Muir, H.A.; Candelli, M.; Pignataro, G.; Thangathurai, D.; Cicchinelli, S.; Racca, F.; Longhitano, Y.; et al. Oxidative stress in critical care and vitamins supplement therapy: “a beneficial care enhancing”. Eur. Rev. Med. Pharm. Sci. 2019, 23, 7703–7712. [Google Scholar] [CrossRef] [PubMed]
- Petersen, C. D-lactic acidosis. Nutr. Clin. Pract. 2017, 20, 634–645. [Google Scholar] [CrossRef]
- Fabian, E.; Kramer, L.; Siebert, F.; Högenauer, C.; Raggam, R.B.; Wenzl, H.; Krejs, G.J. D-Lactic acidosis-case report and review of the literature. Z. Für. Gastroenterol. 2017, 55, 75–82. [Google Scholar] [CrossRef]
- Alarcon, P.; Hidalgo, A.I.; Manosalva, C.; Cristi, R.; Teuber, S.; Hidalgo, M.A.; Burgos, R.A. Metabolic disturbances in synovial fluid are involved in the onset of synovitis in heifers with acute ruminal acidosis. Sci. Rep. 2019, 9, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Naik, P.; Singh, S.; Dave, V.P.; Ali, M.H.; Kumar, A.; Joseph, J. Vitreous d-lactate levels as a biomarker in the diagnosis of presumed infectious culture negative endophthalmitis. Curr. Eye Res. 2020, 45, 184–189. [Google Scholar] [CrossRef] [PubMed]
- Terpstra, M.L.; Sinnige, M.; Hugenholtz, F.; Peters-Sengers, H.; Remmerswaal, E.B.M.; Geerlings, S.E.; Bemelman, F.J. Butyrate production in patients with end-stage renal disease. Int. J. Nephrol. Renov. Dis. 2019, 12, 87–101. [Google Scholar] [CrossRef] [PubMed]
- Jorgensen, V.L.; Reiter, N.; Perner, A. Luminal concentrations of L- and D-lactate in the rectum may relate to severity of disease and outcome in septic patients. Crit. Care 2006, 10, R163. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.S.; Li, Y.C.; Tsai, P.Y.; Lin, C.-E.; Chen, C.-M.; Chen, S.-M.; Lee, J. Accumulation of methylglyoxal andd-lactate in Pb-induced nephrotoxicity in rats. Biomed. Chromatogr. 2017, 31, e3869. [Google Scholar] [CrossRef]
- Geissler, A.J.; Behr, J.; von Kamp, K.; Vogel, R.F. Metabolic strategies of beer spoilage lactic acid bacteria in beer. Int. J. Food Microbiol. 2016, 216, 60–68. [Google Scholar] [CrossRef]
- Andersen, L.W.; Mackenhauer, J.; Roberts, J.C.; Berg, K.M.; Cocchi, M.N.; Donnino, M.W. Etiology and therapeutic approach to elevated lactate levels. Mayo Clin. Proc. 2013, 88, 1127–1140. [Google Scholar] [CrossRef]
- Liu, Z.; Meng, Z.; Li, Y.; Zhao, J.; Wu, S.; Gou, S.; Wu, H. Prognostic accuracy of the serum lactate level, the SOFA score and the qSOFA score for mortality among adults with Sepsis. Scand. J. Trauma Resusc. Emerg. Med. 2019, 27, 51. [Google Scholar] [CrossRef]
- Van Beest, P.A.; Brander, L.; Jansen, S.P.; Rommes, J.H.; Kuiper, M.A.; Spronk, P.E. Cumulative lactate and hospital mortality in ICU patients. Ann. Intensive Care 2013, 3, 6. [Google Scholar] [CrossRef]
- Pro, C.I.; Yealy, D.M.; Kellum, J.A.; Huang, D.T.; Barnato, A.E.; Weissfeld, L.A.; Pike, F.; Terndrup, T.; Wang, H.E.; Hou, P.C.; et al. A randomized trial of protocol-based care for early septic shock. N. Engl. J. Med. 2014, 370, 1683–1693. [Google Scholar]
- Kliegel, A.; Losert, H.; Sterz, F.; Holzer, M.; Zeiner, A.; Havel, C.; Laggner, A.N. Serial lactate determinations for prediction of outcome after cardiac arrest. Medicine 2004, 83, 274–279. [Google Scholar] [CrossRef] [PubMed]
- Mitchell, J.H.; Wildenthal, K.; Johnson, R.L., Jr. The effects of acid-base disturbances on cardiovascular and pulmonary function. Kidney Int. 1972, 1, 375–389. [Google Scholar] [CrossRef] [PubMed]
- Davies, A.O. Rapid desensitization and uncoupling of human betaadrenergic receptors in an in vitro model of lactic acidosis. J Clin. Endocrinol. Metab. 1984, 59, 398–405. [Google Scholar] [CrossRef] [PubMed]
- van Hall, G. Lactate kinetics in human tissues at rest and during exercise. Acta Physiol. 2010, 199, 499–508. [Google Scholar] [CrossRef]
- Connor, H.; Woods, H.F. Quantitative aspects of L(þ)-lactate metabolism in human beings. Ciba Found. Symp. 1982, 87, 214–234. [Google Scholar]
- Jansson, P.A.; Smith, U.; Lonnroth, P. Evidence for lactate production by human adipose tissue in vivo. Diabetologia 1990, 33, 253–256. [Google Scholar] [CrossRef]
- Wilson, T.H. The role of lactic acid production in glucose absorption from the intestine. J. Biol. Chem. 1956, 222, 751–763. [Google Scholar] [CrossRef]
- Bellomo, R. Bench-to-bedside review: Lactate and the kidney. Crit. Care 2002, 6, 322–326. [Google Scholar] [CrossRef]
- Connor, H.; Woods, H.F.; Ledingham, J.G.; Murray, J.D. A model of L(þ)- lactate metabolism in normal man. Ann. Nutr. Metab. 1982, 26, 254–263. [Google Scholar] [CrossRef]
- Kamel SKamel Man SOh Mitchell, L. Halperin, L-lactic acidosis: Pathophysiology, classification, and causes; emphasis on biochemical and metabolic basis. Kidney Int. 2020, 97, 75–88, ISSN 0085-2538. [Google Scholar]
- Ritter, J.M.; Doktor, H.S.; Benjamin, N. Paradoxical effect of bicarbonate on cytoplasmic pH. Lancet 1990, 335, 1243–1246. [Google Scholar] [CrossRef] [PubMed]
- Halperin, M.L.; Cheema-Dhadli, S.; Halperin, F.A.; Kamel, K.S. Rationale for the use of sodium bicarbonate in a patient with lactic acidosis due to a poor cardiac output. Nephron 1994, 66, 258–261. [Google Scholar] [CrossRef] [PubMed]
- Cerda, J.; Tolwani, A.J.; Warnock, D.G. Critical care nephrology:management of acid-base disorders with CRRT. Kidney Int. 2012, 82, 9–18. [Google Scholar] [CrossRef] [PubMed]
- De Corte, W.; Vuylsteke, S.; De Waele, J.J.; Dhondt, A.W.; Decruyenaere, J.; Vanholder, R.; Hoste, E.A.J. Severe lactic acidosis incritically ill patients with acute kidney injury treated with renal replacement therapy. J. Crit. Care 2014, 29, 650–655. [Google Scholar] [CrossRef] [PubMed]
- Gowrishankar, M.; Kamel, K.S.; Halperin, M.L. A brain protein centered view of Hþ buffering. J. Am. Soc. Nephrol. 2007, 18, 2278–2280. [Google Scholar] [CrossRef]
- Lieberman, J.A.; Weiskopf, R.B.; Kelley, S.D.; Feiner, J.; Noorani, M.; Leung, J.; Toy, P.; Viele, M. Critical oxygen delivery in conscious humans is less than 7.3 ml O2 × kg−1 × min−1. Anesthesiology 2000, 92, 407–413. [Google Scholar] [CrossRef]
- Van Woerkens, E.C.; Trouwborst, A.; van Lanschot, J.J. Profound hemodilution: What is the critical level of hemodilution at which oxygen delivery-dependent oxygen consumption starts in an anesthetized human? Anesth. Analg. 1992, 75, 818–821. [Google Scholar] [CrossRef]
- Zhang, H.; Vincent, J.L. Oxygen extraction is altered by endotoxin during tamponade-induced stagnant hypoxia in the dog. Circ. Shock. 1993, 40, 168–176. [Google Scholar]
- Nathan, A.T.; Singer, M. The oxygen trail: Tissue oxygenation. Br. Med. Bull. 1999, 55, 96–108. [Google Scholar] [CrossRef]
- Chiolero, R.L.; Revelly, J.P.; Leverve, X.; Gersbach, P.; Cayeux, M.; Berger, M.M.; Tappy, L. Effects of cardiogenic shock on lactate and glucose metabolism after heart surgery. Crit. Care Med. 2000, 28, 3784–3791. [Google Scholar] [CrossRef]
- Akkose, S.; Ozgurer, A.; Bulut, M.; Koksal, O.; Ozdemír, F.; Ozguç, H. Relationships between markers of inflammation, severity of injury, and clinical outcomes in hemorrhagic shock. Adv. Ther. 2007, 24, 955–962. [Google Scholar] [CrossRef] [PubMed]
- Friedman, G.; De Backer, D.; Shahla, M.; Vincent, J.L. Oxygen supply dependency can characterize septic shock. Intensive Care Med. 1998, 24, 118–123. [Google Scholar] [CrossRef] [PubMed]
- Singel, D.J.; Stamler, J.S. Chemical physiology of blood flow regulation by red blood cells: The role of nitric oxide and S-nitrosohemoglobin. Annu. Rev. Physiol. 2005, 67, 99–145. [Google Scholar] [CrossRef] [PubMed]
- Revelly, J.P.; Ayuse, T.; Brienza, N.; Fessler, H.E.; Robotham, J.L. Endotoxic shock alters distribution of blood flow within the intestinal wall. Crit. Care Med. 1996, 24, 1345–1351. [Google Scholar] [CrossRef]
- Cerwinka, W.H.; Cooper, D.; Krieglstein, C.F.; Ross, C.R.; McCord, J.M.; Granger, D.N. Superoxide mediates endotoxin-induced platelet-endothelial cell adhesion in intestinal venules. Am. J. Physiol. Heart Circ. Physiol. 2003, 284, H535–H541. [Google Scholar] [CrossRef][Green Version]
- Fink, M.P. Intestinal epithelial hyperpermeability: Update on the pathogenesis of gut mucosal barrier dysfunction in critical illness. Curr Opin Crit. Care 2003, 9, 143–151. [Google Scholar] [CrossRef]
- Taylor, D.J.; Faragher, E.B.; Evanson, J.M. Inflammatory cytokines stimulate glucose uptake and glycolysis but reduce glucose oxidation in human dermal fibroblasts in vitro. Circ. Shock. 1992, 37, 105–110. [Google Scholar]
- Kraut, J.A.; Madias, N.E. Lactic acidosis: Current treatments and future directions. Am. J. Kidney Dis. 2016, 68, 473–482. [Google Scholar] [CrossRef]
- Fulop, M.; Bock, J.; Ben-Ezra, J.; Antony, M.; Danzig, J.; Gage, J.S. Plasma lactate and 3-hydroxybutyrate levels in patients with acute ethanol intoxication. Am. J. Med. 1986, 80, 191–194. [Google Scholar] [CrossRef]
- MacDonald, L.; Kruse, J.A.; Levy, D.B.; Marulendra, S.; Sweeny, P.J. Lactic acidosis and acute ethanol intoxication. Am. J. Emerg. Med. 1994, 12, 32–35. [Google Scholar] [CrossRef]
- Donnino, M.W.; Vega, J.; Miller, J.; Walsh, M. Myths and misconceptions of Wernicke’s encephalopathy: What every emergency physician should know. Ann. Emerg. Med. 2007, 50, 715–721. [Google Scholar] [CrossRef] [PubMed]
- Shull, P.D.; Rapoport, J. Life-threatening reversible acidosis caused by alcohol abuse. Nat. Rev. Nephrol. 2010, 6, 555–559. [Google Scholar] [CrossRef] [PubMed]
- Klein, M.; Weksler, N.; Gurman, G.M. Fatal metabolic acidosis caused by thiamine deficiency. J. Emerg. Med. 2004, 26, 301–303. [Google Scholar] [CrossRef] [PubMed]
- Neale, B.W.; Mesler, E.L.; Young, M.; Rebuck, J.A.; Weise, W.J. Propylene glycol-induced lactic acidosis in a patient with normal renal function: A proposed mechanism and monitoring recommendations. Ann. Pharm. 2005, 39, 1732–1736. [Google Scholar] [CrossRef]
- Kelner, M.J.; Bailey, D.N. Propylene glycol as a cause of lactic acidosis. J. Anal. Toxicol. 1985, 9, 40–42. [Google Scholar] [CrossRef]
- Arbour, R.; Esparis, B. Osmolar gap metabolic acidosis in a 60-year-old man treated for hypoxemic respiratory failure. Chest 2000, 118, 545–546. [Google Scholar] [CrossRef]
- Duriseti, P.; Moreno Vanegas, Y.; Jaber, B.L.; Balakrishnan, V.S.; Madias, N.E. Malignancy-induced lactic acidosis in adult lymphoma. Clin. Nephrol. 2021, 95, 1–21. [Google Scholar] [CrossRef] [PubMed]
- Yang, R.; Wang, Z.; Jia, Y.; Li, H.; Mou, Y. Comparison of Clinical Efficacy of Sodium Nitroprusside and Urapidil in the Treatment of Acute Hypertensive Cerebral Hemorrhage. J. Healthc. Eng. 2022, 2022, 2209070. [Google Scholar] [CrossRef] [PubMed]
- Tinker, J.H.; Michenfelder, J.D. Sodium nitroprusside: Pharmacology, toxicology and therapeutics. Anesthesiology 1976, 45, 340–354. [Google Scholar] [CrossRef]
- Borron, S.W.; Baud, F.J. Antidotes for acute cyanide poisoning. Curr. Pharm. Biotechnol. 2012, 13, 1940–1948. [Google Scholar] [CrossRef]
- Bulathsinghala, M.; Keefer, K.; Van de Louw, A. Trimethoprim/sulfamethoxazole-induced severe lactic acidosis: A case report and review of the literature. Medicine 2016, 95, e3478. [Google Scholar] [CrossRef] [PubMed]
- Schramm, C.; Wanitschke, R.; Galle, P.R. Thiamine for the treatment of nucleoside analogue-induced severe lactic acidosis. Eur. J. Anaesthesiol. 1999, 16, 733–735. [Google Scholar] [CrossRef] [PubMed]
- Luzzati, R.; Del Bravo, P.; Di Perri, G.; Luzzani, A.; Concia, E. Riboflavine and severe lactic acidosis. Lancet 1999, 353, 901–902. [Google Scholar] [CrossRef] [PubMed]
- Garrabou, G.; Soriano, A.; Lopez, S.; Guallar, J.P.; Giralt, M.; Villarroya, F.; Martiínez, J.A.; Casademont, J.; Cardellach, F.; Mensa, J.; et al. Reversible inhibition of mitochondrial protein synthesis during linezolid-related. Antimicrob. Agents Chemother. 2007, 51, 962–967. [Google Scholar] [CrossRef] [PubMed]
- Soriano, A.; Miro, O.; Mensa, J. Mitochondrial toxicity associated with linezolid. N. Engl. J. Med. 2005, 353, 2305–2306. [Google Scholar] [CrossRef]
- Wolf, A.; Weir, P.; Segar, P.; Stone, J.; Shield, J. Impaired fatty acid oxidation in propofol infusion syndrome. Lancet 2001, 357, 606–607. [Google Scholar] [CrossRef] [PubMed]
- Inzucchi, S.E.; Bergenstal, R.M.; Buse, J.B.; Diamant, M.; Ferrannini, E.; Nauck, M.; Peters, A.L.; Tsapas, A.; Wender, R.; Matthews, D.R.; et al. Management of hyperglycemia in type 2 diabetes: A patient-centered approach: Position statement of the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care 2012, 35, 1364–1379. [Google Scholar] [CrossRef]
- Misbin, R.I. The phantom of lactic acidosis due to metformin in patients with diabetes. Diabetes Care 2004, 27, 1791–1793. [Google Scholar] [CrossRef]
- Laforest, C.; Saint-Marcoux, F.; Amiel, J.B.; Pichon, N.; Merle, L. Monitoring of metformininduced lactic acidosis in a diabetic patient with acute kidney failure and effect of hemodialysis. Int. J. Clin. Pharm. Ther. 2013, 51, 147–151. [Google Scholar] [CrossRef]
- Gabow, P.A.; Anderson, R.J.; Potts, D.E.; Schrier, R.W. Acid-base disturbances in the salicylate-intoxicated adult. Arch. Intern. Med. 1978, 138, 1481–1484. [Google Scholar] [CrossRef]
- Jorgensen, T.G.; Weis-Fogh, U.S.; Nielsen, H.H.; Olesen, H.P. Salicylate- and aspirin-induced uncoupling of oxidative phosphorylation in mitochondria isolated from the mucosal membrane of the stomach. Scand. J. Clin. Lab. Investig. 1976, 36, 649–654. [Google Scholar] [CrossRef] [PubMed]
- Silvestre, J.; Carvalho, S.; Mendes, V.; Coelho, L.; Tapadinhas, C.; Ferreira, P.; Povoa, P.; Ceia, F. Metformin-induced lactic acidosis: A case series. J. Med. Case Rep. 2007, 1, 126. [Google Scholar] [CrossRef] [PubMed]
- Heinig, R.E.; Clarke, E.F.; Waterhouse, C. Lactic acidosis and liver disease. Arch. Intern. Med. 1979, 139, 1229–1232. [Google Scholar] [CrossRef] [PubMed]
- Smith, Z.R.; Horng, M.; Rech, M.A. Medication-Induced Hyperlactatemia and Lactic Acidosis: A Systematic Review of the Literature. Pharmacotherapy 2019, 39, 946–963. [Google Scholar] [CrossRef] [PubMed]
- Link, M.S.; Berkow, L.C.; Kudenchuk, P.J.; Halperin, H.R.; Hess, E.P.; Moitra, V.K.; Neumar, R.W.; O’Neil, B.J.; Paxton, J.H.; Silvers, S.M.; et al. Part 7: Adult advanced cardiovascular life support: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2015, 132 (Suppl. 2), S444–S464. [Google Scholar] [CrossRef]
- Severs, D.; Hoorn, E.J.; Rookmaaker, M.B. A critical appraisal of intravenous fluids: From the physiological basis to clinical evidence. Nephrol. Dial. Transpl. 2014, 30, 178–187. [Google Scholar] [CrossRef]
- O’Dell, E.; Tibby, S.M.; Durward, A.; Murdoch, I.A. Hyperchloremia is the dominant cause of metabolic acidosis in the postresuscitation phase of pediatric meningococcal sepsis. Crit. Care Med. 2007, 35, 2390–2394. [Google Scholar] [CrossRef]
- Cooper, D.J.; Walley, K.R.; Wiggs, B.R.; Russell, J.A. Bicarbonate does not improve hemodynamics in critically ill patients who have lactic acidosis: A prospective, controlled clinical study. Ann. Intern. Med. 1990, 112, 492–498. [Google Scholar] [CrossRef]
- Myburgh, J.A.; Mythen, M.G. Resuscitation fluids. N. Engl. J. Med. 2013, 369, 1243–1251. [Google Scholar] [CrossRef]
- Yunos, N.M.; Bellomo, R.; Hegarty, C.; Story, D.; Ho, L.; Bailey, M. Association between a chloride-liberal vs chloriderestrictive intravenous fluid administration strategy and kidney injury in critically ill adults. JAMA 2012, 308, 1566–1572. [Google Scholar] [CrossRef]
- Kraut, J.A.; Madias, N.E. Lactic acidosis. N. Engl. J. Med. 2014, 371, 2309–2319. [Google Scholar] [CrossRef] [PubMed]
- Vincent, J.L.; De Backer, D. Circulatory shock. N. Engl. J. Med. 2013, 369, 1726–1734. [Google Scholar] [CrossRef] [PubMed]
- Kraut, J.A.; Madias, N.E. Treatment of acute metabolic acidosis: A pathophysiologic approach. Nat. Rev. Nephrol. 2012, 8, 589–601. [Google Scholar] [CrossRef]
- De Backer, D.; Creteur, J.; Dubois, M.J.; Sakr, Y.; Koch, M.; Verdant, C.; Vincent, J. The effects of dobutamine on microcirculatory alterations in patients with septic shock are independent of its systemic effects. Crit. Care Med. 2006, 34, 403–408. [Google Scholar] [CrossRef] [PubMed]
- Jung, B.; Rimmele, T.; Le Goff, C.; Chanques, G.; Corne, P.; Jonquet, O.; Muller, L.; Lefrant, J.-Y.; Guervilly, C.; Papazian, L.; et al. Severe metabolic or mixed acidemia on intensive care unit admission: Incidence, prognosis and administration of buffer therapy: A prospective, multiple-center study. Crit. Care 2011, 15, R238. [Google Scholar] [CrossRef] [PubMed]
- Bjerneroth, G. Tribonat--a comprehensive summary of its properties. Crit. Care Med. 1999, 27, 1009–1013. [Google Scholar] [CrossRef] [PubMed]
- Hood, V.L.; Tannen, R.L. Protection of acid–base balance by pH regulation of acid production. N. Engl. J. Med. 1998, 339, 819–826. [Google Scholar] [CrossRef]
- Okorie, O.N.; Dellinger, P. Lactate: Biomarker and potential therapeutic target. Crit. Care Clin. 2011, 27, 299–326. [Google Scholar] [CrossRef]
- Kruse, O.; Grunnet, N.; Barfod, C. Blood lactate as a predictor for in-hospital mortality in patients admitted acutely to hospital: A systematic review. Scand. J. Trauma Resusc. Emerg. Med. 2011, 19, 74. [Google Scholar] [CrossRef]
- Lee, S.W.; Hong, Y.S.; Park, D.W.; Choi, S.; Moon, S.; Park, J.; Kim, J.; Baek, K. Lactic acidosis not hyperlactatemia as a predictor of in hospital mortality in septic emergency patients. Emerg. Med. J. 2008, 25, 659–665. [Google Scholar] [CrossRef]
- Jansen, T.C.; van Bommel, J.; Schoonderbeek, F.J.; Visser, S.J.S.; van der Klooster, J.M.; Lima, A.P.; Willemsen, S.P.; Bakke, J. Early lactate-guided therapy in intensive care unit patients: A multicenter, open-label, randomized controlled trial. Am. J. Respir. Crit. Care Med. 2010, 182, 752–761. [Google Scholar] [CrossRef] [PubMed]
- Longhitano, Y.; Zanza, C.; Thangathurai, D.; Taurone, S.; Kozel, D.; Racca, F.; Audo, A.; Ravera, E.; Migneco, A.; Piccioni, A.; et al. Gut Alterations in Septic Patients: A Biochemical Literature Review. Rev. Recent Clin. Trials. 2020, 15, 289–297. [Google Scholar] [CrossRef] [PubMed]
- Piccioni, A.; Valletta, F.; Zanza, C.; Esperide, A.; Franceschi, F. Novel biomarkers to assess the risk for acute coronary syndrome: Beyond troponins. Intern. Emerg. Med. 2020, 15, 1193–1199. [Google Scholar] [CrossRef] [PubMed]

| Lactate Classification | Mechanism | Medication | Treatment |
|---|---|---|---|
| Tybe A | Reduced Cardiac Output | Clozapine, Diltiazem, Nifedipine, Procainamide | Medication Withheld Supportive Treatment Iniatiated |
| Type B-1 | Drug Induced Disease | Hepatic Failure (Acetaminophen, Erlotinib, Fludarabine) Mesenteric Ischemia (Canaglifozin) Gastrointestinal Ischemia (Epinephrine) Pancreatitis (Cimetidine, Exetanide, Rifampin, Isoniazid, Pyrazinamide, Ethambutol) Acute Kidney Injury (Exetanide, Ibuprofen, NSAID) Hemolytic Anemia (Sulfamethoxazole and Trimethoprim, Nitrofurantoin) Rhabdomyolysis (ralgtegravir) Hypoxiemia (Opioids) | Medication Withheld Antidotes Administered If Applicable Supportive Treatment Initiated |
| Type B-2 Related to Metabolism Impairment | Increased Pyruvate Production | Albuterol, Metaproterenol, Salmeterol, Sorbitol, Caffeine, Theophylline, Epinephrine, Terbutaline | Medication Withheld AntidotesAdministered If Applicable Supportive Treatment Initiated |
| Alterations in Glucose Metabolism Favoring Accumulation of Lactate Relative to Pyruvate | Ethanol, Niacin, Oxaliplatin, Streptozocin | Medication Withheld Supportive Treatment Initiated | |
| Propylene Glycol excipient | Diazepam, Lorazepam, Etomidate, Pentobarbital, Sulfamethoxazole and Trimethoprim, Nitroglycerin | Medication Withheld Supportive Treatment Initiated | |
| Type B-2 related to mitochondrial impairment | Inhibition of Mitochondrial Protein Synthesis/Function | Acetaminophen, Carboplatin, Linezolid, Simvastatin, Minocycline, Telbivudine, Adefovir, Entecavir, Linezoild | Medication Withheld Supportive Treatment Initiated |
| Inhibition of Mitochondrial Electron Transport Chain | Clozapine, Propofol, Sodium Nitroprusside, Valproate, Venlafaxine | Medication Withheld Supportive Treatment Initiated | |
| Mitochondrial Toxicity | Ganciclovir, Valanciclovir, Ribavirin-Sofosbuvir, Adasabuvir.Ombitasvir, Paritaprevir, Ritonavir | Medication Withheld Supportive Treatment Initiated | |
| Uncoupling Oxidative Phosphorylation | Sulfasalazine, Metformin | Medication Withheld Supportive Treatment Initiated | |
| Type D | Bacterial Overgrowth in Setting of Short Bowel Syndrome | Doxycicline, Sulfamethoxazole and Trimethoprim | Medication Withheld Supportive Treatment Initiated |
| Type of Acidosis | Mechanism | Causes | Therapies |
|---|---|---|---|
| Type A | Mismatch VO2(O2 Consumption) DO2(O2 Delivery) | Any Shock(Septic, Cardiogenic, Hypovolemic, Obstructive) Trauma Severe Hypoxemia Carbon Monoxide Infection | Adequate Alveolar Ventilation Adequate Circulation Volume Continuous Dyalisis Antibiotics Cardiovascular Treatment Withheld Medications |
| Type B-1 | Related to Specific Disease | Hepatopathy Thiamine Deficiency Malignancy Cyanide Poisoning | Stop Drug Administration Support Therapy |
| Type B-2 Type B-3 | Related to Toxins or Drugs Related to Metabolism Alterations | See Table 1 Congenital L-LA Ethanol Intoxication Methanol Intoxication | See Table 1 Support Therapy |
| Type D | d-Lactate Excessive production | Short Bowel Syndrome | Surgery and Support |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zanza, C.; Facelli, V.; Romenskaya, T.; Bottinelli, M.; Caputo, G.; Piccioni, A.; Franceschi, F.; Saviano, A.; Ojetti, V.; Savioli, G.; et al. Lactic Acidosis Related to Pharmacotherapy and Human Diseases. Pharmaceuticals 2022, 15, 1496. https://doi.org/10.3390/ph15121496
Zanza C, Facelli V, Romenskaya T, Bottinelli M, Caputo G, Piccioni A, Franceschi F, Saviano A, Ojetti V, Savioli G, et al. Lactic Acidosis Related to Pharmacotherapy and Human Diseases. Pharmaceuticals. 2022; 15(12):1496. https://doi.org/10.3390/ph15121496
Chicago/Turabian StyleZanza, Christian, Valentina Facelli, Tastiana Romenskaya, Maria Bottinelli, Giorgia Caputo, Andrea Piccioni, Francesco Franceschi, Angela Saviano, Veronica Ojetti, Gabriele Savioli, and et al. 2022. "Lactic Acidosis Related to Pharmacotherapy and Human Diseases" Pharmaceuticals 15, no. 12: 1496. https://doi.org/10.3390/ph15121496
APA StyleZanza, C., Facelli, V., Romenskaya, T., Bottinelli, M., Caputo, G., Piccioni, A., Franceschi, F., Saviano, A., Ojetti, V., Savioli, G., & Longhitano, Y. (2022). Lactic Acidosis Related to Pharmacotherapy and Human Diseases. Pharmaceuticals, 15(12), 1496. https://doi.org/10.3390/ph15121496









