Osmotic Pump Drug Delivery Systems—A Comprehensive Review
Abstract
1. Introduction
History
2. Basic Components of Osmotic Pump Systems
2.1. Drug
2.2. Osmotic Agent
2.3. Semipermeable Membrane
2.4. Wicking Agent [37]
2.5. Pore-Forming Agents
2.6. Coating Solvents
3. Delivery Orifice
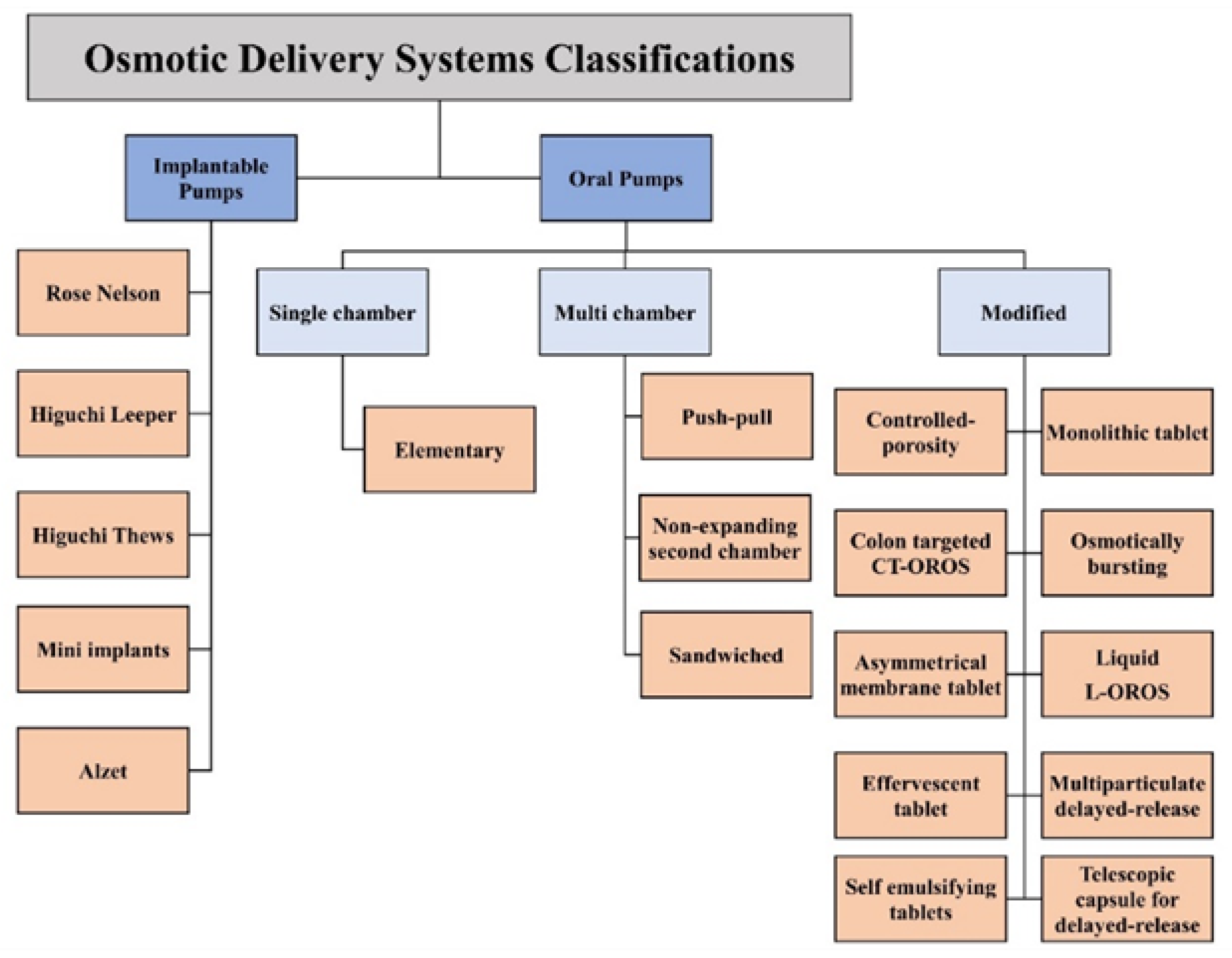
4. Types of Osmotic Drug Delivery Systems
4.1. Implantable Systems
4.1.1. The Rose–Nelson Pump
4.1.2. The Higuchi–Leeper Pump
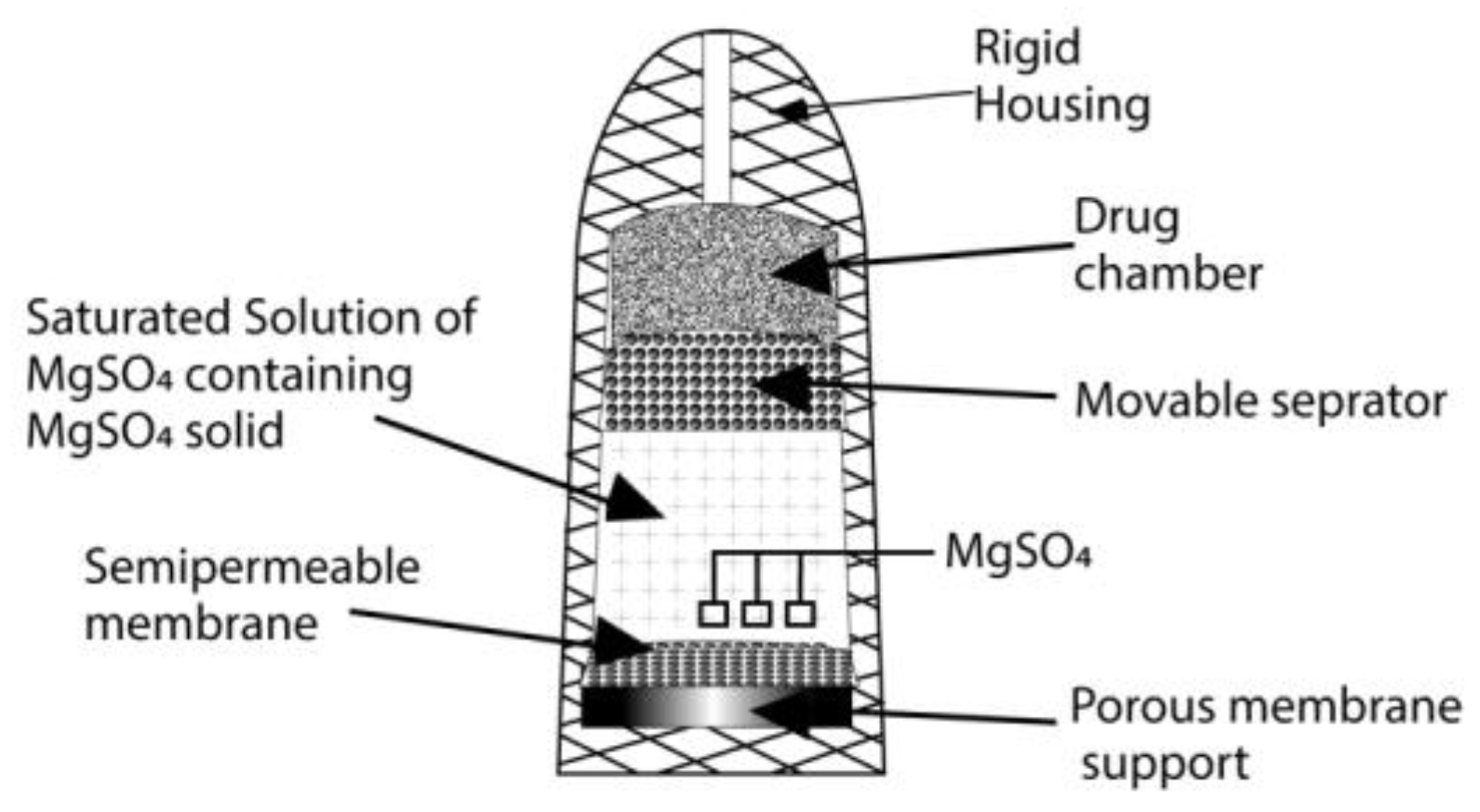
4.1.3. The Higuchi–Theeuwes Pump
4.1.4. The Implantable Mini Osmotic Pump
4.1.5. The Alzet Osmotic Pump
4.2. Oral Systems
4.2.1. Single-Chamber Osmotic Systems
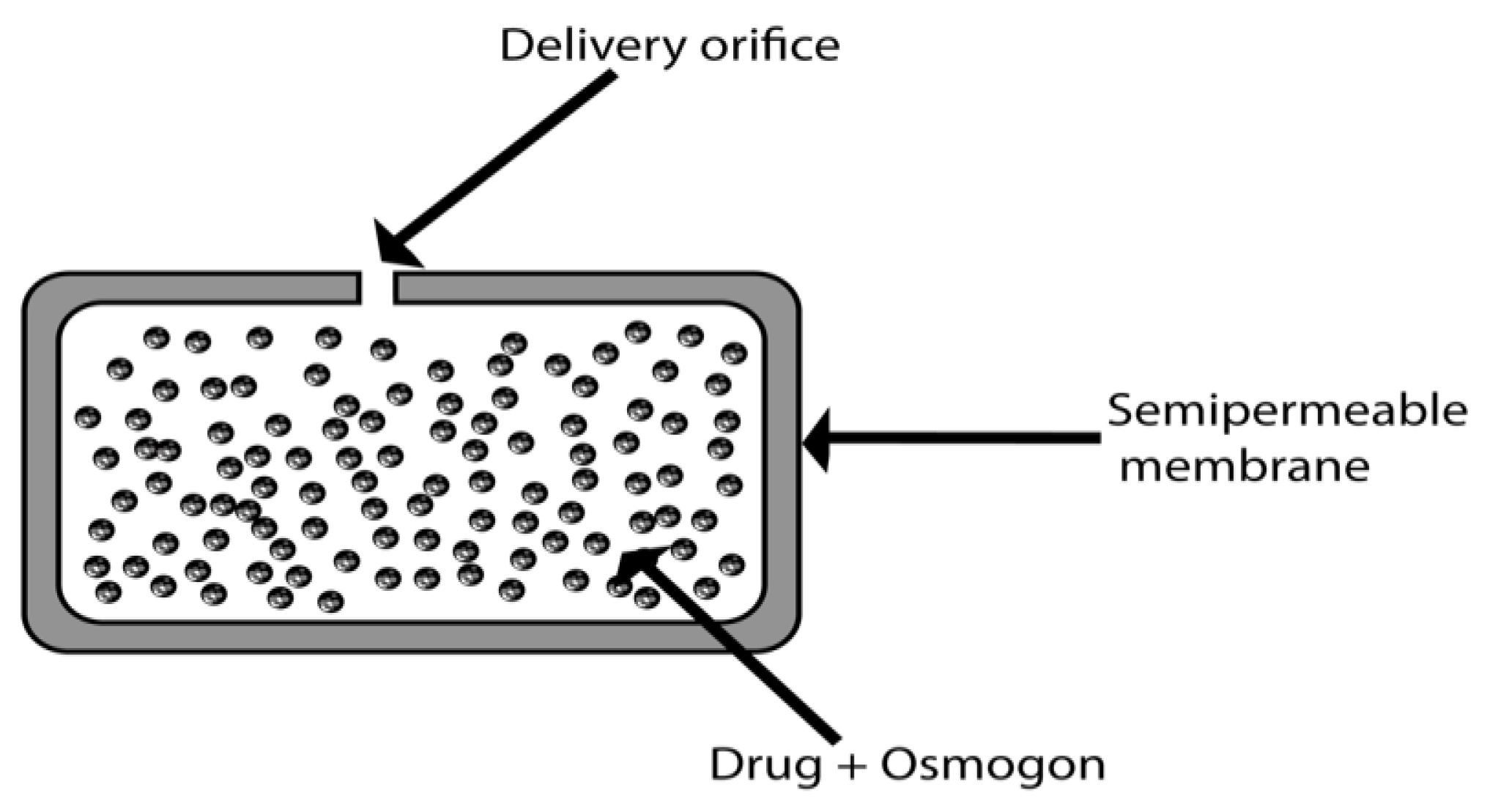
Elementary Osmotic Pump (EOP)
4.2.2. Multichambered Osmotic Pumps
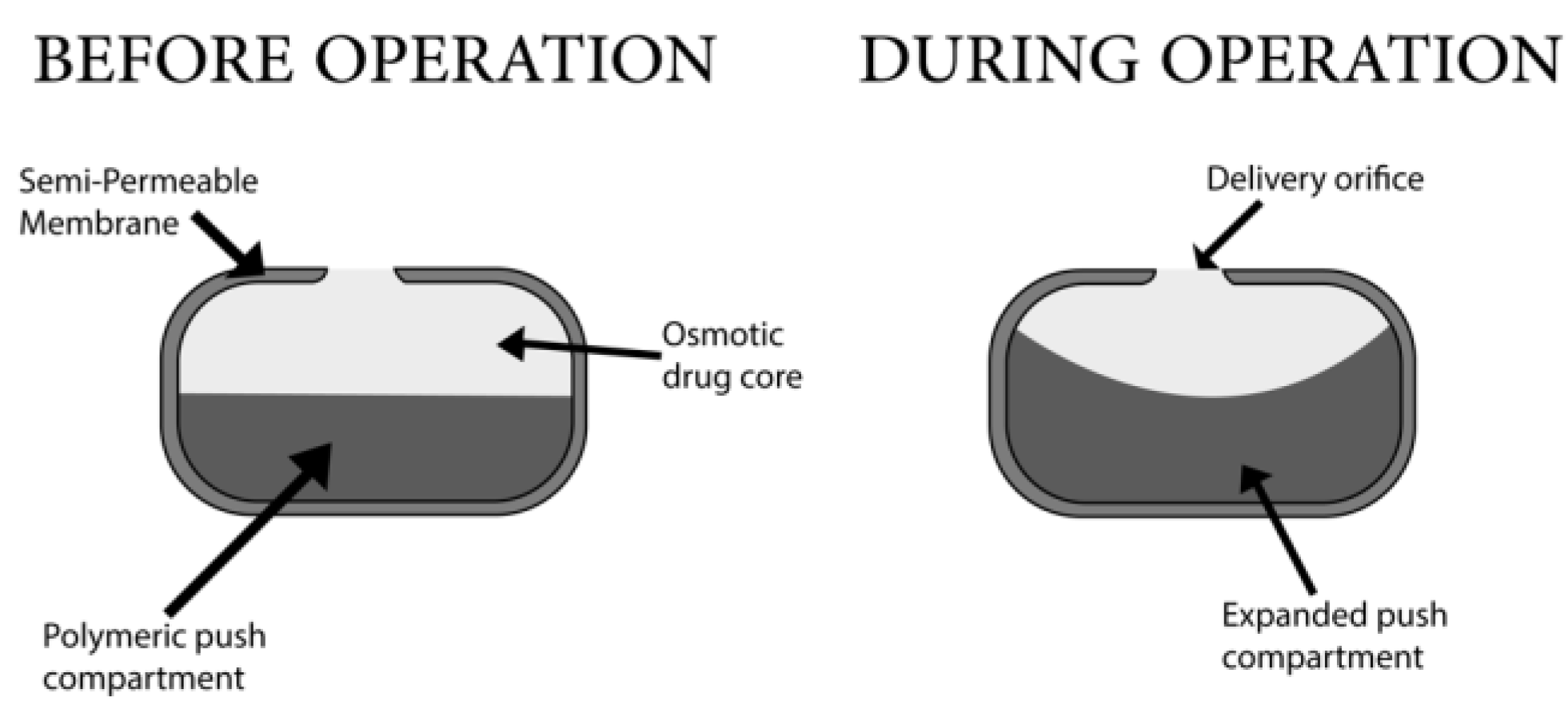
Push–Pull Osmotic Pump
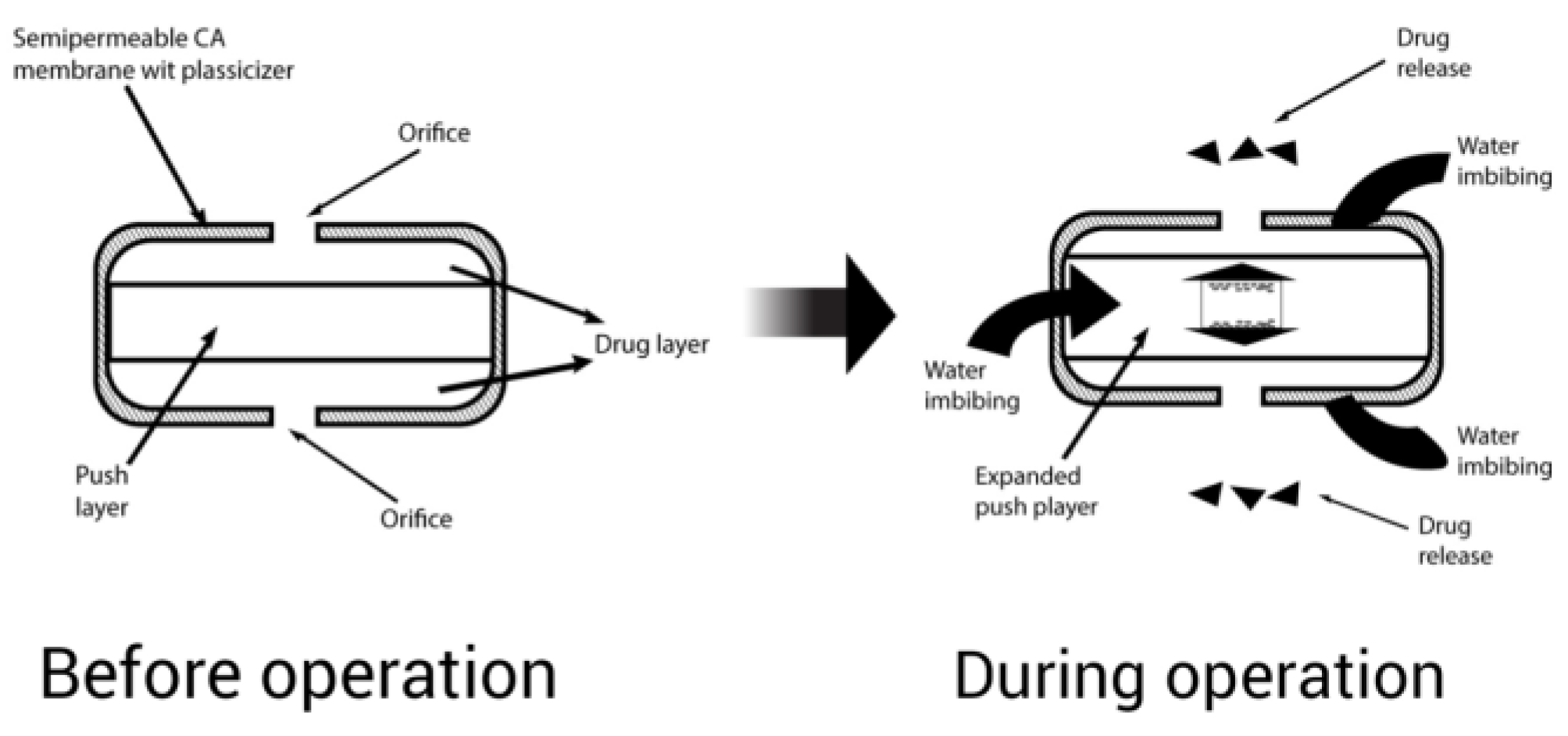
Sandwiched Osmotic Tablet
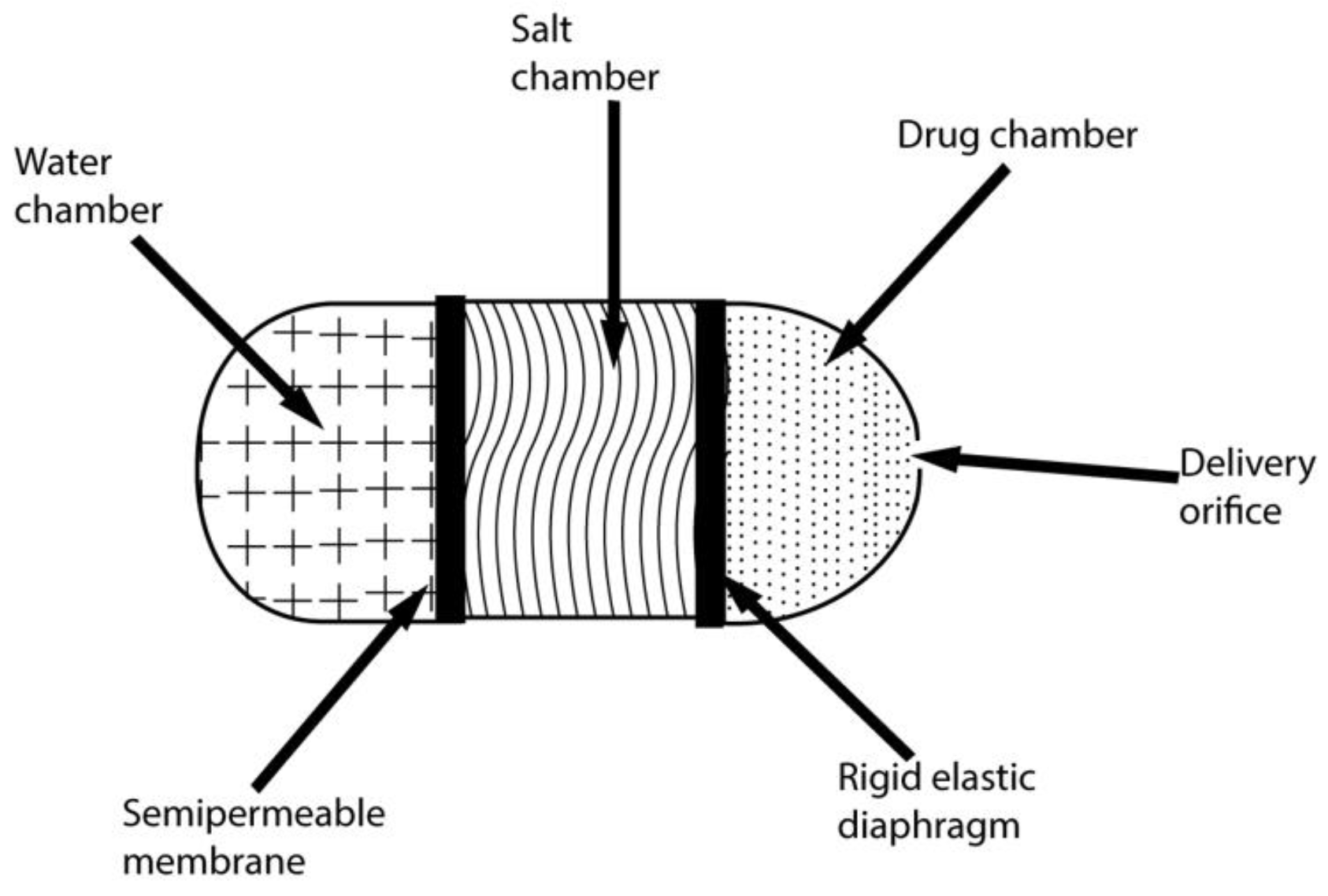
Osmotic Pump with a Non-Expanding Second Chamber
4.2.3. Specific Types
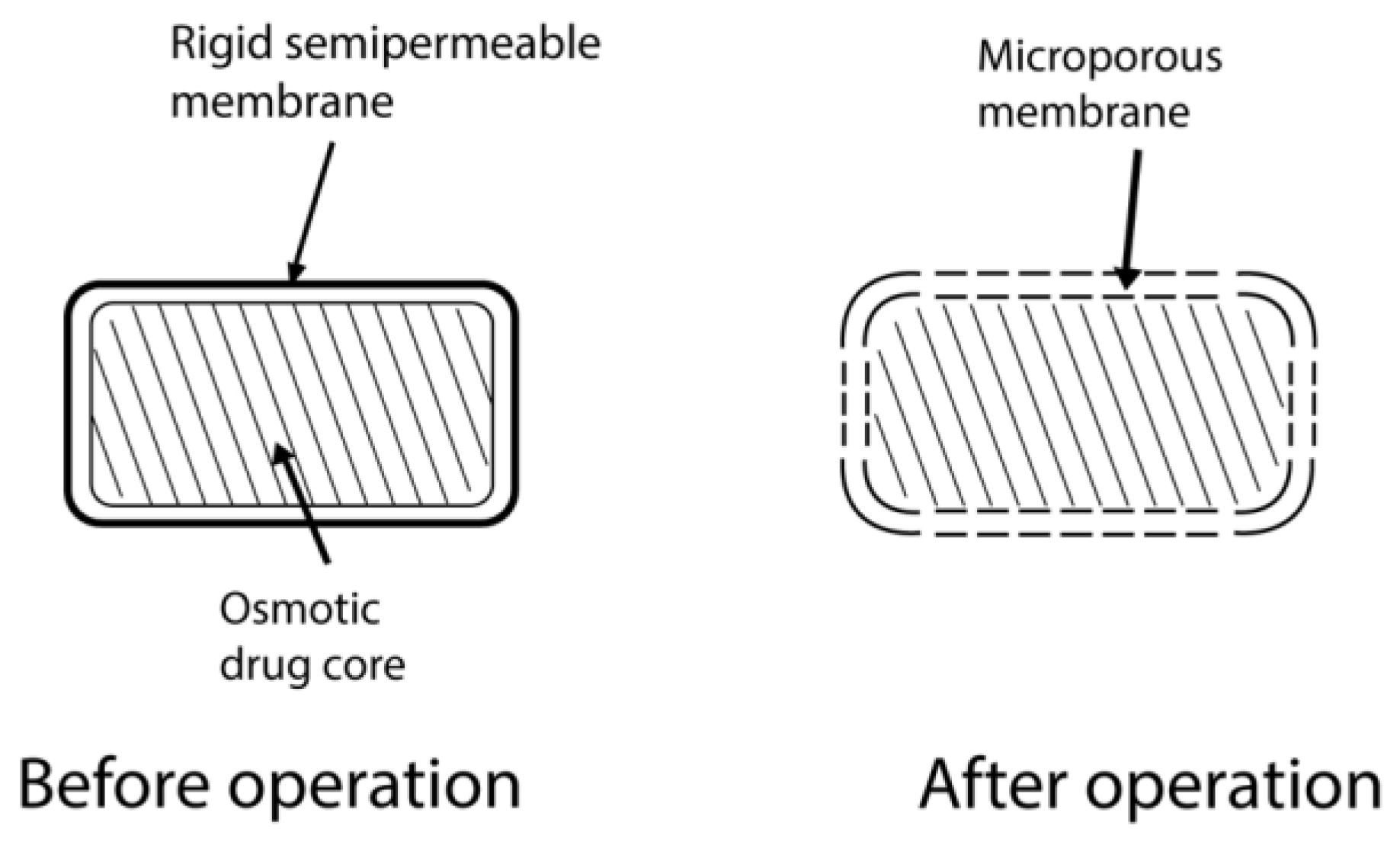
Controlled-Porosity Osmotic Pump
Monolithic Osmotic System
Colon-Targeted Oral Osmotic System [93]
Osmotically Bursting Osmotic Pump
Asymmetrical-Membrane Osmotic Tablet
Liquid Oral Osmotic System
Effervescent Osmotic Tablet
Multiparticulate Delayed-Release System
Self-Emulsified Osmotic Tablet
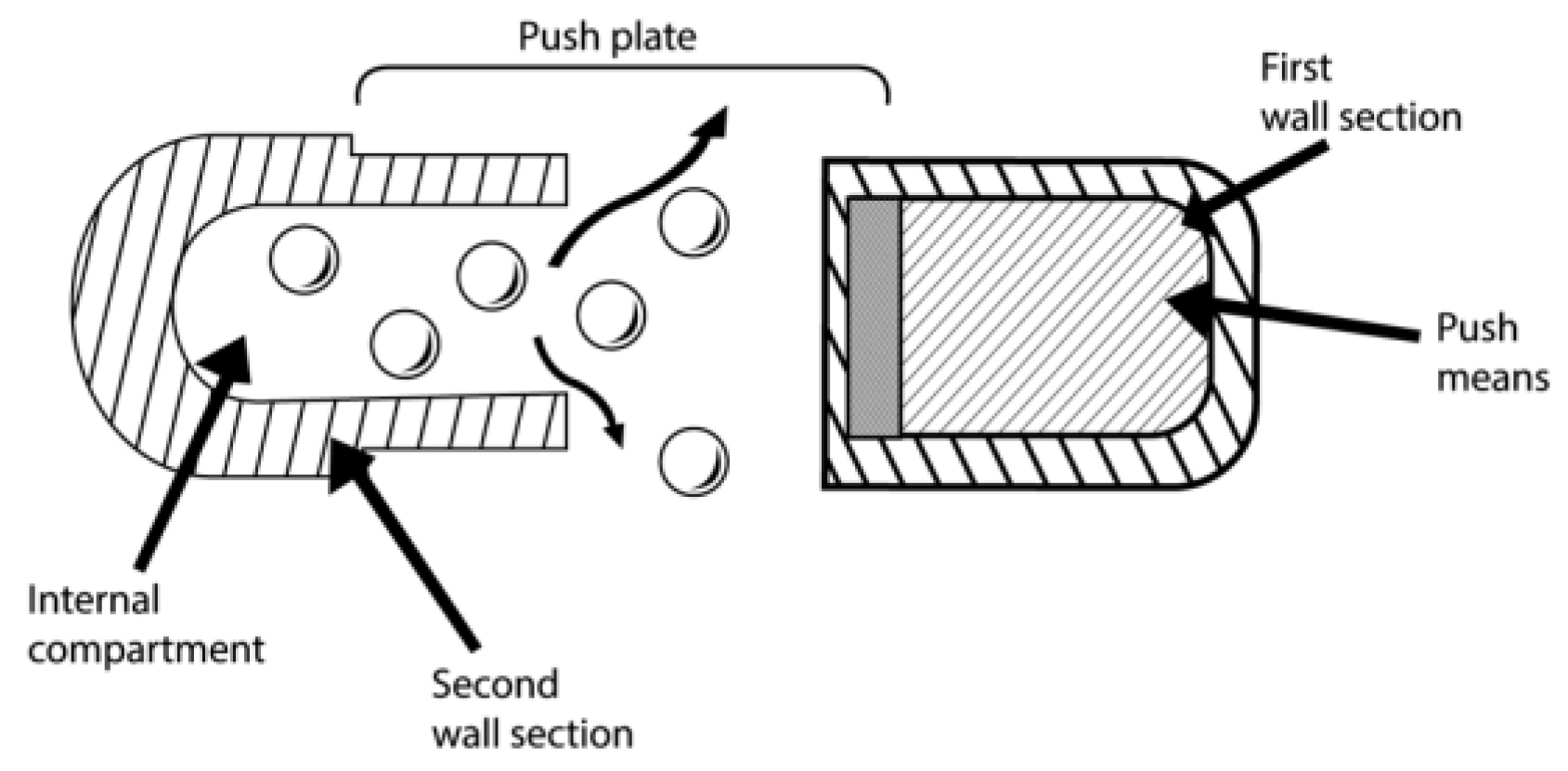
Telescopic Capsule for Delayed Release [77]
| Product Name | Active Pharmaceutical Ingredients | Osmotic System Type |
|---|---|---|
| Oral Products | ||
| UT-15C | Treprostinil Diethanolamine | EOP |
| LCP-Lerc | Lercanidipine | EOP |
| Ditropan XL | Oxybutynin Chloride | EOP |
| Altoprev | Lovastatin | EOP |
| Flexeril XL | Cyclobenzaprine | EOP |
| Elafax XR | Venlafaxine HCl | EOP |
| Tegretol XL | Carbamazepine | EOP |
| Osmosin | Indomethacin | EOP |
| Teosona Sol | Theophylline | EOP |
| Allegra D 24 h | Pseudoephedrine HCl Fexofenadine HCl | EOP |
| Loremex | Pseudoephedrine HCl Loratadin | EOP |
| Mildugen D | Pseudoephedrine HCl Astemizol | EOP |
| Efidac 24bromphenirmine | Pseudoephedrine HCl Brompheniramin | EOP |
| Volmax | Albuterol | EOP |
| Acutrim | Phenylpropanolamine | EOP |
| Osmoran | Ranitidine HCl | EOP |
| Teczem | Enalapril Diltiazem | Controlled Porosity Osmotic Pump |
| Tiamate | Diltiazem HCl | Controlled Porosity Osmotic Pump |
| ActoPlus XR | Metformin HCl Pioglitazone HCl | Controlled Porosity Osmotic Pump |
| Acu System C | Vitamine C | Controlled Porosity Osmotic Pump |
| Covera HS | Verapamil HCl | Push–pull Osmotic Pump |
| DynaCirc CR | Isradipine | Push–pull Osmotic Pump |
| Minipress XL | Prazosin | Push–pull Osmotic Pump |
| Procardia XL | Nifedipine | Push–pull Osmotic Pump |
| Glucotrol XL | Glipizide | Push–pull Osmotic Pump |
| Cardura CR | Doxazosin Mesylate | Push–pull Osmotic Pump |
| Oxycontin | Oxycodone | Push–pull Osmotic Pump |
| Jusnista | Hydromorphone | Push–pull Osmotic Pump |
| Invega | Paliperidone | Push–pull Osmotic Pump |
| Topamax | Topiramate | Push-Stick Osmotic Pump |
| Concerta | Methylphenidate HCl | Push-Stick Osmotic Pump |
| Implantable Products | ||
| ChronogesicTM | Sufentanil | Implantable osmotic system |
| Viadur | Leuprolide Acetate | Implantable osmotic system |
5. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Keraliya, R.A.; Patel, C.; Patel, P.; Keraliya, V.; Soni, T.G.; Patel, R.C.; Patel, M. Osmotic drug delivery system as a part of modified release dosage form. Int. Sch. Res. Not. 2012, 2012, 528079. [Google Scholar] [CrossRef] [PubMed]
- Kaparissides; Costas; Alexandridou, S.; Kotti, K.; Chaitidou, S. Recent advances in novel drug delivery systems. J. Nanotechnol. Online 2006, 2, 1–11. [Google Scholar]
- Patel, J.; Parikh, S.; Patel, S. Comprehensive review on osmotic drug delivery system. World J. Pharm. Res. 2021, 10, 29. [Google Scholar]
- Bruschi, M.L. Strategies to Modify the Drug Release from Pharmaceutical Systems; Woodhead Publishing: Sawston, UK, 2015. [Google Scholar]
- Cheng, L.; Gao, S.; Ouyang, D.; Wang, H.; Wang, Y.; Pan, W.; Yang, X. Release Mechanism Between Ion Osmotic Pressure and Drug Release in Ionic-Driven Osmotic Pump Tablets (I). AAPS PharmSciTech 2018, 19, 803–811. [Google Scholar] [CrossRef] [PubMed]
- Siddique, W.; Zaman, M.; Sarfraz, R.M.; Butt, M.H.; Rehman, A.U.; Fassih, N.; Albadrani, G.M.; Bayram, R.; Alfaifi, M.Y.; Abdel-Daim, M.M. The Development of Eletriptan Hydrobromide Immediate Release Buccal Films Using Central Composite Rotatable Design: An In Vivo and In Vitro Approach. Polymers 2022, 14, 3981. [Google Scholar] [CrossRef] [PubMed]
- Arafat, M. Approaches to achieve an oral controlled release drug delivery system using polymers: A recent review. Int. J. Pharm. Pharm. Sci. 2015, 7, 16–21. [Google Scholar]
- Ratnaparkhi, M.; Gupta Jyoti, P.J.T. Sustained release oral drug delivery system—An overview. Int. J. Pharm. Res. 2013, 3, 10–22270. [Google Scholar]
- Farooqi, S.; Yousuf, R.I.; Shoaib, M.H.; Ahmed, K.; Ansar, S.; Husain, T. Quality by Design (QbD)-Based Numerical and Graphical Optimization Technique for the Development of Osmotic Pump Controlled-Release Metoclopramide HCl Tablets. Drug Des. Dev. Ther. 2020, 14, 5217. [Google Scholar] [CrossRef]
- Swathi, B.; Manichandrika, K.P.; Niharika, R.; Pravalika, G.; Sahithya, D.; Meghana, M. Formulation and evaluation of quinidine osmotic drug delivery system. Int. J. Adv. Res. Med. Pharm. Sci. 2019, 4, 17–22. [Google Scholar]
- Hanif, M.; Zaman, M.; Chaurasiya, V. Polymers used in buccal film: A review. Des. Monomers Polym. 2015, 18, 105–111. [Google Scholar] [CrossRef]
- Flavia, L.; Keckeis, V. Advances in drug delivery systems: Work in progress still needed? Int. J. Pharm. 2020, 590, 119912. [Google Scholar]
- Shirole, P.U.; Patil, P.B.; Bachhav, R.S. Review on Osmotic Drug Delivery System. IJRAR-Int. J. Res. Anal. Rev. (IJRAR) 2020, 7, 160–167. [Google Scholar]
- Patel, H.; Parikh, V.P. An overview of osmotic drug delivery system: An update review. Int. J. Bioassays 2017, 6, 5426–5436. [Google Scholar] [CrossRef]
- Sahoo, C.K.; Rao, S.R.; Sudhakar, M. Evaluation of controlled porosity osmotic pump tablets: A Review. Res. J. Pharm. Technol. 2015, 8, 1340. [Google Scholar] [CrossRef]
- Sharma, A.; Kumar, D.; Painuly, N. A review on osmotically controlled drug delivery systems. Asian J. Pharm. Res. Dev. 2018, 6, 101–109. [Google Scholar] [CrossRef][Green Version]
- Gundu, R.; Pekamwar, S.; Shelke, S.; Kulkarni, D.; Gadade, D.; Shep, S. Development and pharmacokinetic evaluation of osmotically controlled drug delivery system of Valganciclovir HCl for potential application in the treatment of CMV retinitis. Drug Deliv. Transl. Res. 2022, 12, 2708–2729. [Google Scholar] [CrossRef]
- Zaman, M.; Siddique, W.; Waheed, S.; Sarfraz, R.; Mahmood, A.; Qureshi, J.; Iqbal, J.; Chughtai, F.; Rahman, M.U.; Khalid, U. Hydrogels, their applications and polymers used for hydrogels: A review. Int. J. Biol. Pharm. Allied Sci. 2015, 4, 6581–6603. [Google Scholar]
- Srikonda, S.; Kotamraj, P.; Barclay, B. Osmotic controlled drug delivery systems. In Design of Controlled Release Drug Delivery Systems; 2006. [Google Scholar]
- Santus, G.; Baker, R.W. Osmotic drug delivery: A review of the patent literature. J. Control. Release 1995, 35, 1–21. [Google Scholar] [CrossRef]
- Sareen, R.; Jain, N.; Kumar, D.J. An insight to osmotic drug delivery. Curr. Drug Deliv. 2012, 9, 285–296. [Google Scholar] [CrossRef]
- Harper, D.J.; Milo, C.F. Osmotic Pump Drug Delivery Systems and Methods. U.S. Patent no 6471688 B1, 29 October 2002. [Google Scholar]
- Patel, K.N.; Mehta, T.A. A review on oral osmotically driven systems. Int. J. Pharm. Pharm. Sci. 2013, 5, 1005–1013. [Google Scholar]
- Prajapati, H.M.; Prajapati, S.T.; Patel, C.N. A review on recent innovation in osmotically controlled drug delivery system. Int. J. Pharm. Res. Bio-Sci. 2012, 1, 158–194. [Google Scholar]
- Cortese, R.; Theeuwes, F. Osmotic Device with Hydrogel Driving Member. U.S. Patent no 4327725, 4 May 1982. [Google Scholar]
- Malaterre, V.; Ogorka, J.; Loggia, N.; Gurny, R.J.I. Approach to design push–pull osmotic pumps. Int. J. Pharm. 2009, 376, 56–62. [Google Scholar] [CrossRef] [PubMed]
- Gundu, R.; Pekamwar, S.; Shelke, S.; Kulkarni, D.; Shep, S. Development, optimization and pharmacokinetic evaluation of biphasic extended-release osmotic drug delivery system of trospium chloride for promising application in treatment of overactive bladder. Future J. Pharm. Sci. 2021, 7, 1–20. [Google Scholar] [CrossRef]
- Kumaravelrajan, R.; Narayanan, N.; Suba, V.J.L. Development and evaluation of controlled porosity osmotic pump for Nifedipine and Metoprolol combination. Lipids Health Dis. 2011, 10, 51. [Google Scholar] [CrossRef]
- Wong, P.S.; Theeuwes, F.; Barclay, B.L.; Dealey, M.H. Osmotic Dosage System for Liquid Drug Delivery. U.S. Patent no 5413572, 9 May 1995. [Google Scholar]
- Rastogi, S.; Vaya, N.; Mishra, B.J.E. Osmotic pump: A novel concept in rate controlled oral drug delivery. East. Pharm. 1995, 38, 79. [Google Scholar]
- Verma, R.; Mishra, B.; Garg, S. Osmotically controlled oral drug delivery. Drug Dev. Ind. Pharm. 2000, 26, 695–708. [Google Scholar] [CrossRef]
- Farheen, F.; Bharadwaj, S. A review on osmotically regulated systems. PharmaTutor 2014, 2, 51–64. [Google Scholar]
- Udawant, S.J.W. A review: Osmotic drug delivery system. World J. Pharm. Res. 2015, 4, 1787–1801. [Google Scholar]
- Malaterre, V.; Ogorka, J.; Loggia, N.; Gurny, R.J. Oral osmotically driven systems: 30 years of development and clinical use. Eur. J. Pharm. Biopharm. 2009, 73, 311–323. [Google Scholar] [CrossRef]
- Babu, A.; Ratna, P.R.V. Controlled-porosity osmotic pump tablets—An overview. Asian J. Pharm. Res. Health Care 2010, 2, 1. [Google Scholar]
- Verma, R.K.; Garg, S.J. Development and evaluation of osmotically controlled oral drug delivery system of glipizide. Eur. J. Pharm. Biopharm. 2004, 57, 513–525. [Google Scholar] [CrossRef] [PubMed]
- Rudnic, E.M.; Burnside, B.A.; Flanner, H.H.; Wassink, S.E.; Couch, R.A.; Pinkett, J.E. Osmotic Drug Delivery System. U.S. Patent no 6110498, 29 August 2000. [Google Scholar]
- Singla, D.; Hari Kumar, S.; Nirmala, G.J. Osmotic pump drug delivery: A novel approach. Int. J. Res. Pharm. Chem. 2012, 2, 661–670. [Google Scholar]
- Okimoto, K.; Rajewski, R.A.; Stella, V.J. Release of testosterone from an osmotic pump tablet utilizing (SBE) 7m-β-cyclodextrin as both a solubilizing and an osmotic pump agent. J. Control. Release 1999, 58, 29–38. [Google Scholar] [CrossRef]
- Herrlich, S.; Spieth, S.; Messner, S.; Zengerle, R. Osmotic micropumps for drug delivery. Adv. Drug Deliv. Rev. 2012, 64, 1617–1627. [Google Scholar] [CrossRef] [PubMed]
- Jerzewski, R.L.; Chien, Y.W. Osmotic drug delivery. In Treatise on Controlled Drug Delivery; CRC Press: Boca Raton, FL, USA, 2017; pp. 225–253. [Google Scholar]
- Banerjee, A.; Verma, P.R.P.; Gore, S. Controlled porosity solubility modulated osmotic pump tablets of Gliclazide. AAPS PharmSciTech 2015, 16, 554–568. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Siew, A. Controlling drug release through osmotic systems. Pharm. Technol. 2013, 37, 32–35. [Google Scholar]
- Lindstedt, B.; Ragnarsson, G.; Hjärtstam, J. Osmotic pumping as a release mechanism for membrane-coated drug formulations. J. Control. Release 1989, 56, 261–268. [Google Scholar] [CrossRef]
- Makhija, S.N.; Vavia, P.R. Controlled porosity osmotic pump-based controlled release systems of pseudoephedrine: I. Cellulose acetate as a semipermeable membrane. J. Control. Release 2003, 89, 5–18. [Google Scholar] [CrossRef]
- Seminoff, L.A.; Zentner, G.M. Cellulosic Coating. European Patent no 0425023A2, 23 October 1989. [Google Scholar]
- Ahmed, K.; Shoaib, M.H.; Yousuf, R.I.; Qazi, F.; Anwer, S.; Nasiri, M.I.; Mahmood, Z.A. Use of Opadry® CA—A cellulose acetate/polyethylene glycol system for rate-controlled osmotic drug delivery of highly soluble antispastic agent Eperisone HCl. Adv. Polym. Technol. 2018, 37, 2730–2742. [Google Scholar] [CrossRef]
- Sanap, S.L.; Savkare, A.D. Controlled porosity osmotic pump: A review. Int. J. Pharm. Res. Dev. 2014, 5, 70–80. [Google Scholar]
- Markovsky, E.; Baabur-Cohen, H.; Eldar-Boock, A.; Omer, L.; Tiram, G.; Ferber, S.; Ofek, P.; Polyak, D.; Scomparin, A.; Satchi-Fainaro, R. Administration, distribution, metabolism and elimination of polymer therapeutics. J. Control. Release 2012, 161, 446–460. [Google Scholar] [CrossRef] [PubMed]
- Ghosh, T.; Ghosh, A.J. Drug delivery through osmotic systems—An overview. J. Appl. Pharm. Sci. 2011, 1, 38–49. [Google Scholar]
- Mathur, M.; Mishra, R. A review on osmotic pump drug delivery system. Pharma Sci. Monit. 2016, 7, 453. [Google Scholar]
- Zentner, G.M.; Rork, G.S.; Himmelstein, K. The controlled porosity osmotic pump. J. Control. Release 1985, 1, 269–282. [Google Scholar] [CrossRef]
- Thulasiramaraju, T.; Reddy, S.R.; Patnaik, N.A.; Kumar, K.S. Osmotic drug delivery system: A promising drug delivery Technology. AJRC 2013, 1, 7–22. [Google Scholar]
- Verma, R.K.; Krishna, D.M.; Garg, S.J. Formulation aspects in the development of osmotically controlled oral drug delivery systems. J. Control. Release 2002, 79, 7–27. [Google Scholar] [CrossRef]
- Singh, K.; Walia, M.K.; Agarwal, G.; Harikumar, S.J. Osmotic pump drug delivery system: A noval approach. J. Drug Deliv. Ther. 2013, 3, 156–162. [Google Scholar] [CrossRef][Green Version]
- Asghar, F.; Ahmad, S.; Gul, M.; Malik, T. Mucoadhesive system to enhance drug activity containing Flurbiprofen as model drug. Mucoadhesive Syst. Enhanc. Drug Act. Contain. Flurbiprofen Model Drug 2020, 59, 9. [Google Scholar]
- Patel, P.M.; Yadav, J. Osmotic Controlled Drug Delivery System: A Review. Pharma Sci. Monit. 2018, 9, 695–708. [Google Scholar]
- Venkateswarlu, B.S.; Pasupathi, C.; Pasupathi, A.; Jaykar, B.; Chandira, R.M.; Palanisamy, P. Osmotic drug delivery system: A review. J. Drug Deliv. Ther. 2019, 9, 759–764. [Google Scholar]
- Sharma, D.; Kumar, D.; Singh, M.; Singh, G.; Rathore, M.S. A review on novel osmotically controlled drug delivery system. Indian J. Pharm. 2012, 3, 97–105. [Google Scholar]
- Verma, R.; Mishra, B.J.P. Studies on formulation and evaluation of oral osmotic pumps of nimesulide. Pharmazie 1999, 54, 74–75. [Google Scholar]
- Theeuwes, F.; Saunders, R.J.; Mefford, W.S. Process for Forming Outlet Passageways In pills Using a Laser. U.S. Patents no 4088864, 9 May 1978. [Google Scholar]
- Li, N.; Fan, L.; Wu, B.; Dai, G.; Jiang, C.; Guo, Y.; Wang, D. Preparation and in vitro/in vivo evaluation of azilsartan osmotic pump tablets based on the preformulation investigation. Drug Dev. Ind. Pharm. 2019, 45, 1079–1088. [Google Scholar] [CrossRef]
- Chen, C.-M.; Lee, D.-Y.; Xie, J. Controlled Release Formulation for Water Insoluble Drugs in Which a Passageway is Formed In Situ. U.S. Patents no 5736159, 7 April 1998. [Google Scholar]
- Gawai, N.M.; Aher, S.S.; B, R. Saudagar. A Review on Drug Category Suitable for Monolithic Osmotic Tablet. Res. J. Pharm. Dos. Technol. 2016, 8, 24–30. [Google Scholar]
- Rose, S.; Nelson, J. A continuous long-term injector. Aust. J. Exp. Biol. Med. Sci. 1955, 33, 415–419. [Google Scholar] [CrossRef]
- Gohel, M.; Parikh, R.; Shah, N. Osmotic Drug Delivery: An Update. World J. Pharm. Res. 2009, 7, 1–7. [Google Scholar]
- Higuchi, T.; Leeper, H. Osmotic Dispenser. U.S. Patent no 3995631, 7 December 1976. [Google Scholar]
- Higuchi, T. Osmotic Dispenser with Collapsible Supply Container. U.S. Patent no 3732865, 15 May 1973. [Google Scholar]
- Umamaheswari, A. Formulation and Evaluation of Controlled Porosity Osmotic Tablets of Lornoxicam. Ph.D. Thesis, College of Pharmacy, Madras Medical College, Chennai, India, 2012. [Google Scholar]
- Theeuwes, F.; Yum, S. Principles of the design and operation of generic osmotic pumps for the delivery of semisolid or liquid drug formulations. Ann. Biomed. Eng. 1976, 4, 343–353. [Google Scholar] [CrossRef]
- Theeuwes, F. Osmotic System for Delivering Selected Beneficial agents Having Varying Degrees of Solubility. U.S. Patnet no 4111201, 5 September 1978. [Google Scholar]
- Capozza, R.; Eckenhoff, B.; Yum, S. Design and performance of the implantable osmotic minipump. J. Med. Eng. Technol. 1977, 1, 281–283. [Google Scholar] [CrossRef]
- Kerenyi, S.Z.; Hartgraves, S.L. Premature excess release from the Alzet osmotic pump. Pharmacol. Biochem. Behav. 1987, 27, 199–201. [Google Scholar] [CrossRef]
- Ouyang, D.; Nie, S.; Li, W.; Guo, H.; Liu, H.; Pan, W. Design and evaluation of compound metformin/glipizide elementary osmotic pump tablets. J. Pharm. Pharmacol. 2005, 57, 817–820. [Google Scholar] [CrossRef]
- Lieberman, H.A.; Lachman, L.; Schwartz, J.B. Pharmaceutical Dosage Forms: Tablets; Dekker, M., Ed.; CRC Press: Boca Raton, FL, USA, 1980; Volume 1. [Google Scholar]
- Theeuwes, F. Elementary osmotic pump. J. Pharm. Sci. 1975, 64, 1987–1991. [Google Scholar] [CrossRef] [PubMed]
- Murkute, R.S.; Wanare, R.S.; Dongre, K.J. A Review: Recent Scenario on Osmotic Controlled Drug Delivery System. Res. J. Pharm. Technol. 2012, 5, 580–591. [Google Scholar]
- Prabakaran, D.; Singh, P.; Kanaujia, P.; Jaganathan, K.; Rawat, A.; Vyas, S.P. Modified push–pull osmotic system for simultaneous delivery of theophylline and salbutamol: Development and in vitro characterization. Int. J. Pharm. 2004, 284, 95–108. [Google Scholar] [CrossRef] [PubMed]
- Wong, P.S.; Barclay, B.; Deters, J.C.; Theeuwes, F. Osmotic Device with Dual Thermodynamic Activity. US Patent 4612008, 16 September 1986. [Google Scholar]
- Wakode, R.; Bhanushali, R.; Bajaj, A. Development and evaluation of push–pull based osmotic delivery system for pramipexole. PDA J. Pharm. Sci. Technol. 2008, 62, 22–31. [Google Scholar] [PubMed]
- Kumaravelrajan, R.; Narayanan, N.; Suba, V.; Bhaskar, K. Simultaneous delivery of Nifedipine and Metoprolol tartarate using sandwiched osmotic pump tablet system. Int. J. Pharm. 2010, 399, 60–70. [Google Scholar] [CrossRef]
- Mohanty, S.; Sahu, M.; Sirisha, A. Osmotic pump: A novel approach to control drug delivery. Indo Am. J. Pharm. Res. 2014, 4, 2367–2373. [Google Scholar]
- Pujara, N.; Thacker, A.P.; Dudhat, K.R.; Patel, N.V.; Parmar, R.B. Osmotically Controlled Oral Drug Delivery Systems: A Novel Approach. Inventi Rapid NDDS 2012, 4, 1–8. [Google Scholar]
- Parashar, B.; Maurya, B.; Yadav, V.; Sharma, L. A review on osmotically regulated devices. Pharma Innov. 2012, 1, 48–56. [Google Scholar]
- Syed, S.M. Osmotic Drug Delivery System: An Overview. Drug Deliv. Syst. 2015, 4, 1–50. [Google Scholar]
- Gupta, N.R.; Mishal, A.; Bhosle, Y.; Shetty, S. A review on recent innovation in osmotically controlled drug delivery system. Indian J. Pharm. Biol. Res. 2014, 2, 117–129. [Google Scholar] [CrossRef]
- Haslam, J.L.; Rork, G.S. Controlled Porosity Osmotic Pump. U.S. Patent no 4880631, 14 November 1989. [Google Scholar]
- Sahoo, C.K.; Sahoo, N.K.; Rao, S.R.M.; Sudhakar, M.; Satyanarayana, K. A review on controlled porosity osmotic pump tablets and its evaluation. Bull. Fac. Pharm. Cairo Univ. 2015, 53, 195–205. [Google Scholar] [CrossRef]
- Oakley, J.A.; Shaw, K.J.; Docker, P.T.; Dyer, C.E.; Greenman, J.; Greenway, G.M.; Haswell, S.J. Development of a bi-functional silica monolith for electro-osmotic pumping and DNA clean-up/extraction using gel-supported reagents in a microfluidic device. Lab Chip 2009, 9, 1596–1600. [Google Scholar] [CrossRef]
- Liu, L.; Khang, G.; Rhee, J.M.; Lee, H.B. Monolithic osmotic tablet system for nifedipine delivery. J. Control. Release 2000, 67, 309–322. [Google Scholar] [CrossRef]
- Liu, L.; Che, B. Preparation of monolithic osmotic pump system by coating the indented core tablet. Eur. J. Pharm. Biopharm. 2006, 64, 180–184. [Google Scholar] [CrossRef]
- Patra, C.N.; Swain, S.; Sruti, J.; Patro, A.P.; Panigrahi, K.C.; Beg, S.; Rao, M.E. Osmotic drug delivery systems: Basics and design approaches. Pat. Drug Deliv. Formul. 2013, 7, 150–161. [Google Scholar] [CrossRef]
- Shah, N.; Patel, N.; Patel, K.; Patel, D. A review on osmotically controlled oral drug delivery systems. J. Pharm. Sci. Bio Res. 2012, 2, 230–237. [Google Scholar]
- Liu, H.; Yang, X.-G.; Nie, S.-F.; Wei, L.-L.; Zhou, L.-L.; Liu, H.; Tang, R.; Pan, W.-S. Chitosan-based controlled porosity osmotic pump for colon-specific delivery system: Screening of formulation variables and in vitro investigation. Int. J. Pharm. 2007, 332, 115–124. [Google Scholar] [CrossRef] [PubMed]
- Nie, X.; Wang, B.; Hu, R.; Lu, W.; Chen, J.; Liu, S.; Jin, D.; Sun, C.; Gao, S.; Guo, Y.J.A.P. Development and Evaluation of Controlled and Simultaneous Release of Compound Danshen Based on a Novel Colon-Specific Osmotic Pump Capsule. AAPS PharmsciTech 2020, 21, 38. [Google Scholar] [CrossRef]
- Li, M.; Shen, Q.; Lu, W.; Chen, J.; Yu, L.; Liu, S.; Nie, X.; Shao, L.; Liu, Y.; Gao, S.; et al. Development and evaluation of controlled release of metformin hydrochloride for improving the oral bioavailability based on a novel enteric osmotic pump capsule. J. Drug Deliv. Sci. Technol. 2020, 60, 102054. [Google Scholar] [CrossRef]
- Amidon, S.; Brown, J.E.; Dave, V.S. Colon-targeted oral drug delivery systems: Design trends and approaches. AAPS Pharmscitech 2015, 16, 731–741. [Google Scholar] [CrossRef]
- Mene, H.R.; Mene, N.R.; Parakh, D.R.; Ingale, T.B.; Magar, D.R.; Mangale, M.R. Formulation aspects in development of controlled porosity osmotic pump tablet. Pharm. Biol. Eval. 2016, 3, 1–8. [Google Scholar]
- Siddique, W.; Zaman, M.; Khan, R.; Butt, M.H.; Muhammad, K.; Salawi, A.; Safhi, A.Y.; Sabei, F.Y. Formulation and Evaluation of Hydroxypropyl Methylcellulose Based Topical Gel Loaded with Ganciclovir. Lat. Am. J. Pharm. 2022, 41, 2096–2108. [Google Scholar]
- Gupta, B.P.; Thakur, N.; Jain, N.P.; Banweer, J.; Jain, S. Osmotically controlled drug delivery system with associated drugs. JPPS 2010, 13, 571–588. [Google Scholar] [CrossRef] [PubMed]
- Piyush, G.; Pankaj, R.; Dabeer, A.; Ayaj, A. A review on osmotically regulated devices. Int. J. Pharm. Life Sci. 2010, 1, 302–312. [Google Scholar]
- Thombre, A.; DeNoto, A.; Gibbes, D. Delivery of glipizide from asymmetric membrane capsules using encapsulated excipients. J. Control. Release 1999, 60, 333–341. [Google Scholar] [CrossRef]
- Suman, S.; Chauhan, M. Asymmetric Membrane Capsule: New Prospects in Osmotic Delivery. Int. J. Drug Deliv. 2011, 3, 185. [Google Scholar]
- Kolli, P.; Kancharla, S.; Gopaiah, K.V. Osmotic release tablets formulation and evaluationof ace inhibitor molecule. Int. J. Pharm. Drug Anal. 2021, 9, 24–35. [Google Scholar] [CrossRef]
- Kushner, J., IV; Lamba, M.; Stock, T.; Wang, R.; Nemeth, M.A.; Alvey, C.; Chen, R.; DeMatteo, V.; Blanchard, A. Development and validation of a Level A in-vitro in-vivo correlation for tofacitinib modified-release tablets using extrudable core system osmotic delivery technology. Eur. J. Pharm. Sci. 2020, 147, 105200. [Google Scholar] [CrossRef]
- Dong, L.; Shafi, K.; Wan, J.; Wong, P. A novel osmotic delivery system: L-OROS Soft cap. In Proceedings of the International Symposium on Controlled Release of Bioactive Materials, Basel, Switzerland, 15–19 August 1988. [Google Scholar]
- Zentner, G.M.; Rork, G.S.; Himmelstein, K.J. Controlled porosity Osmotic Pump. U.S. Patent no 4968507, 6 November 1990. [Google Scholar]
- Li, X.-D.; Nie, S.-F.; Wu, L. Studies on controlled release effervescent osmotic pump tablets from Traditional Chinese Medicine Compound Recipe. J. Control. Release 2004, 96, 359–367. [Google Scholar] [CrossRef]
- Raja, R.K.; Vasu, N.V.; Anka, R.A. Osmotic controlled drug delivery system: A review. Int. J. Pharm. Sci. 2015, 1, 31–37. [Google Scholar]
- Haslam, J.L.; Rork, G.S. Multiparticulate Controlled Porosity Osmotic Pump. U.S. Patent no 4886668, 12 December 1989. [Google Scholar]
- Schultz, P.; Kleinebudde, P. A new multiparticulate delayed release system.: Part I: Dissolution properties and release mechanism. J. Control. Release 1997, 47, 181–189. [Google Scholar] [CrossRef]
- Roy, P.; Shahiwala, A. Multiparticulate formulation approach to pulsatile drug delivery: Current perspectives. J. Control. Release 2009, 134, 74–80. [Google Scholar] [CrossRef] [PubMed]
- Kommana, N.; Bharti, K.; Surekha, D.B.; Thokala, S.; Mishra, B. Development, optimization and evaluation of losartan potassium loaded Self Emulsifying Drug Delivery System. J. Drug Deliv. Sci. Technol. 2020, 60, 102026 1-9. [Google Scholar] [CrossRef]
- Wei, L.; Li, J.; Guo, L.; Nie, S.; Pan, W.; Sun, P.; Liu, H. Investigations of a novel self-emulsifying osmotic pump tablet containing carvedilol. Drug Dev. Ind. Pharm. 2007, 33, 990–998. [Google Scholar] [CrossRef]
- Khandagale, P.M.; Bhairav, B.; Saudagar, R. Osmotically Controlled Drug Delivery System-A Novel Approach. Asian J. Res. Pharm. Sci. 2017, 7, 68–76. [Google Scholar] [CrossRef]
- Xue, Y.; Yu, S.; Wang, H.; Liang, J.; Peng, J.; Li, J.; Yang, X.; Pan, W. Design of a timed and controlled release osmotic pump system of atenolol. Drug Dev. Ind. Pharm. 2015, 41, 906–915. [Google Scholar] [CrossRef]
- Patil, P.; Uphade, K.; Saudagar, R. A Review: Osmotic Drug Delivery System. Pharma Sci. Monit. 2018, 9, 283–300. [Google Scholar]
- Qiu, Y.; Lee, P. Rational design of oral modified-release drug delivery systems. In Developing Solid Oral Dosage Forms; Elsevier: Amsterdam, The Netherlands, 2017; pp. 519–554. [Google Scholar]
- Khatri, N.; Nikam, S.; Bilandi, A. Oral osmotic drug delivery system: A review. Int. J. Pharm. Sci. Res. 2016, 7, 2302. [Google Scholar]

| Advantages | Disadvantages |
|---|---|
| After the administration of the system as intended, first comes a phase known as the lag phase, which occurs in the initial phase, and then a zero-order rate of drug release is achieved [30]. | There might be a risk of dose dumping, resulting in a greater concentration of the drug in the blood than required with potential for toxicity [31]. |
| Side effects are reduced when using this technique. | With implantable pumps, there is a chance of rapidly developing tolerance. |
| By using this technique, a modified form as a delayed or pulsed-type system for introducing drugs into the body can be formulated when required [32]. | If the patient’s immune system is hypersensitive, it may cause a hypersensitivity reaction. |
| In an osmotic system, the release of drugs is driven by osmotic pressure, so it is not dependent on physiological factors of the gastric region, such as pH, and is also independent of hydrodynamic factors [20]. | The integrity of this system and its required consistency are difficult to achieve [33]. |
| The release rate is independent of the drug. | There might be a risk of film defects when there is a problem or poor performance in the coating process. The critical step is the size of the orifice through which the drug is delivered, and this has a direct impact on the drug delivery system’s performance [6,14]. |
| The correlation between in vitro dissolution and in vivo bioavailability is high when this system is employed [34]. | If any toxicity or poisoning occurs, it is impossible to withdraw or to retrieve it from the body system [35]. |
| This system is easily formulated and is also simple to handle. | |
| When implanted or given orally, these systems provide the prolonged or sustained release of drugs, thereby reducing the frequency of drug doses to be taken by patient and improving patient compliance [36,37]. | |
| These systems provide sustained drug release and achieve a steady-state and uniform drug concentration in the blood to provide a therapeutic effect for a prolonged period [35]. |
| Osmotic System | Similarity | Differences/Drawbacks |
|---|---|---|
| EOP | All the osmotic drug delivery systems have a semi-permeable membrane that controls the flow of water and has an osmotic core. | It consists of only one orifice and the drug is released only in solution form. Suitable only for water-soluble drugs. Drug release follows only zero-order kinetics. |
| Rose-Nelson Pump | One of the major drawbacks of this pump is that whenever the pump comes into contact with water, its osmotic action begins due to the presence of a semi-permeable membrane. For this reason, the pump is stored empty and in air-tight containers and must be loaded with water before use. | |
| Push–pull | A push–pull system is better than an EOP system as this system can release drugs both in suspension and solution form. Thus, this system is preferred for highly soluble drugs such as oxybutynin hydrochloride and for very poorly soluble drugs such as glipizide and nifedipine. Meanwhile, the system has a drawback in that a complicated drilling technique is involved in drilling the orifice in the pump. | |
| Push-stick | A push-stick is a longitudinally compressed bilayer tablet system. It consists of a single large orifice and osmotic agents in the push layer. Drug is released from the system as it comes in contact with water and gets moistened, followed by disintegration and then dissolution. | |
| Controlled Porosity and Single Composition Osmotic Tablet (SCOT) | This system consists of a single-layer tablet with no drilled holes; hence, the drug is released from the system through cracks in the form of a wet mass or solution. Compared to other systems, this system significantly reduces gastric irritation. The drug is released from the whole surface of the device (not only from a single orifice). Furthermore, no complex laser drilling, such as that required in a push–pull system, is required since the orifices are formed in situ. | |
| L-OROS | These are soft-gel capsules consisting of only one orifice, and the drug is released in liquid form. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Almoshari, Y. Osmotic Pump Drug Delivery Systems—A Comprehensive Review. Pharmaceuticals 2022, 15, 1430. https://doi.org/10.3390/ph15111430
Almoshari Y. Osmotic Pump Drug Delivery Systems—A Comprehensive Review. Pharmaceuticals. 2022; 15(11):1430. https://doi.org/10.3390/ph15111430
Chicago/Turabian StyleAlmoshari, Yosif. 2022. "Osmotic Pump Drug Delivery Systems—A Comprehensive Review" Pharmaceuticals 15, no. 11: 1430. https://doi.org/10.3390/ph15111430
APA StyleAlmoshari, Y. (2022). Osmotic Pump Drug Delivery Systems—A Comprehensive Review. Pharmaceuticals, 15(11), 1430. https://doi.org/10.3390/ph15111430






