Potential Therapeutic Benefits of Metformin Alone and in Combination with Sitagliptin in the Management of Type 2 Diabetes Patients with COVID-19
Abstract
1. Introduction
2. Results
2.1. Anthropometric and Biochemical Variables at Admission Time
2.1.1. Effects of Metformin
2.1.2. Effects of Metformin plus Sitagliptin
2.1.3. Effects of Metformin versus Metformin plus Sitagliptin
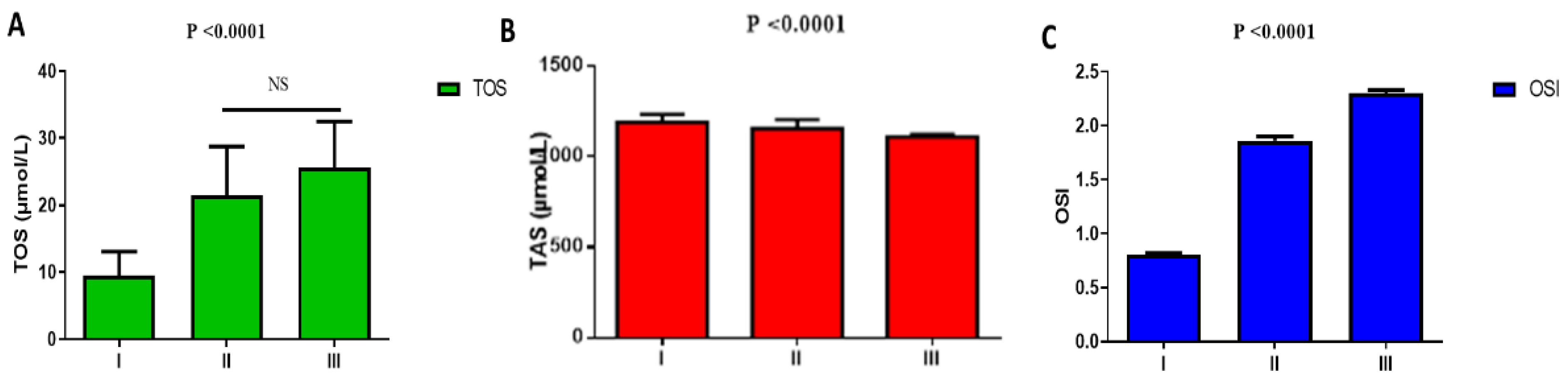
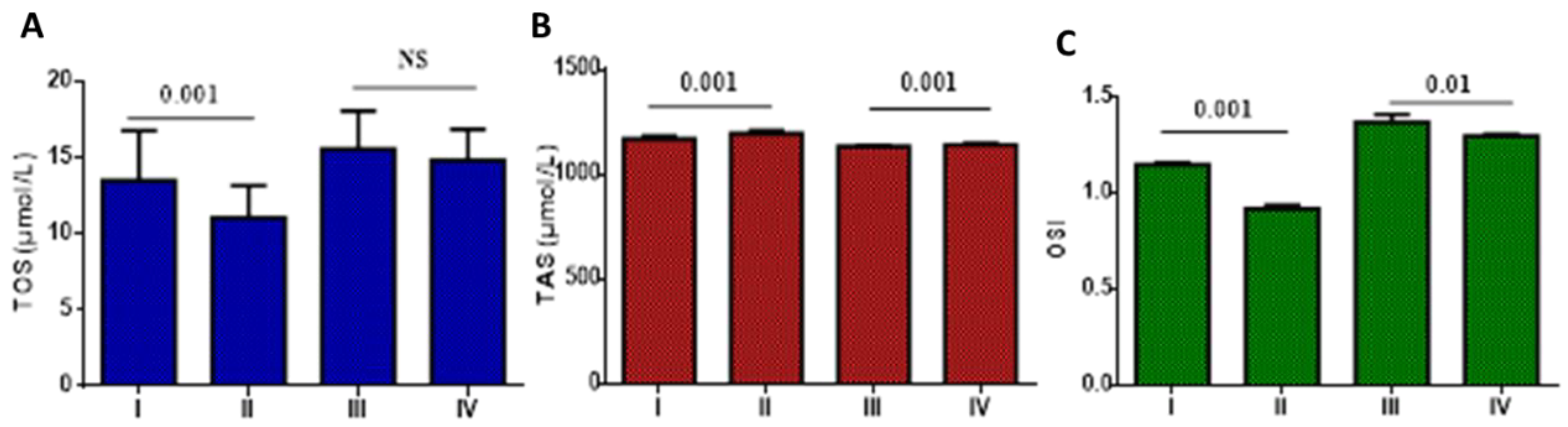
2.2. Oxidative Stress at Admission Time
2.2.1. Impacts of Metformin on Oxidative Stress
2.2.2. Effect of Metformin plus Sitagliptin
2.2.3. Effect of Metformin versus Metformin plus Sitagliptin
2.3. Gender Assessment at Admission Time
2.4. Assessment of COVID-19 Patients at the Time of Discharge
2.4.1. Effects of Metformin versus Metformin plus Sitagliptin on the Anthropometric and Biochemical Variables at the Discharge Time
2.4.2. Gender Assessment at the Time of Discharge
3. Discussion
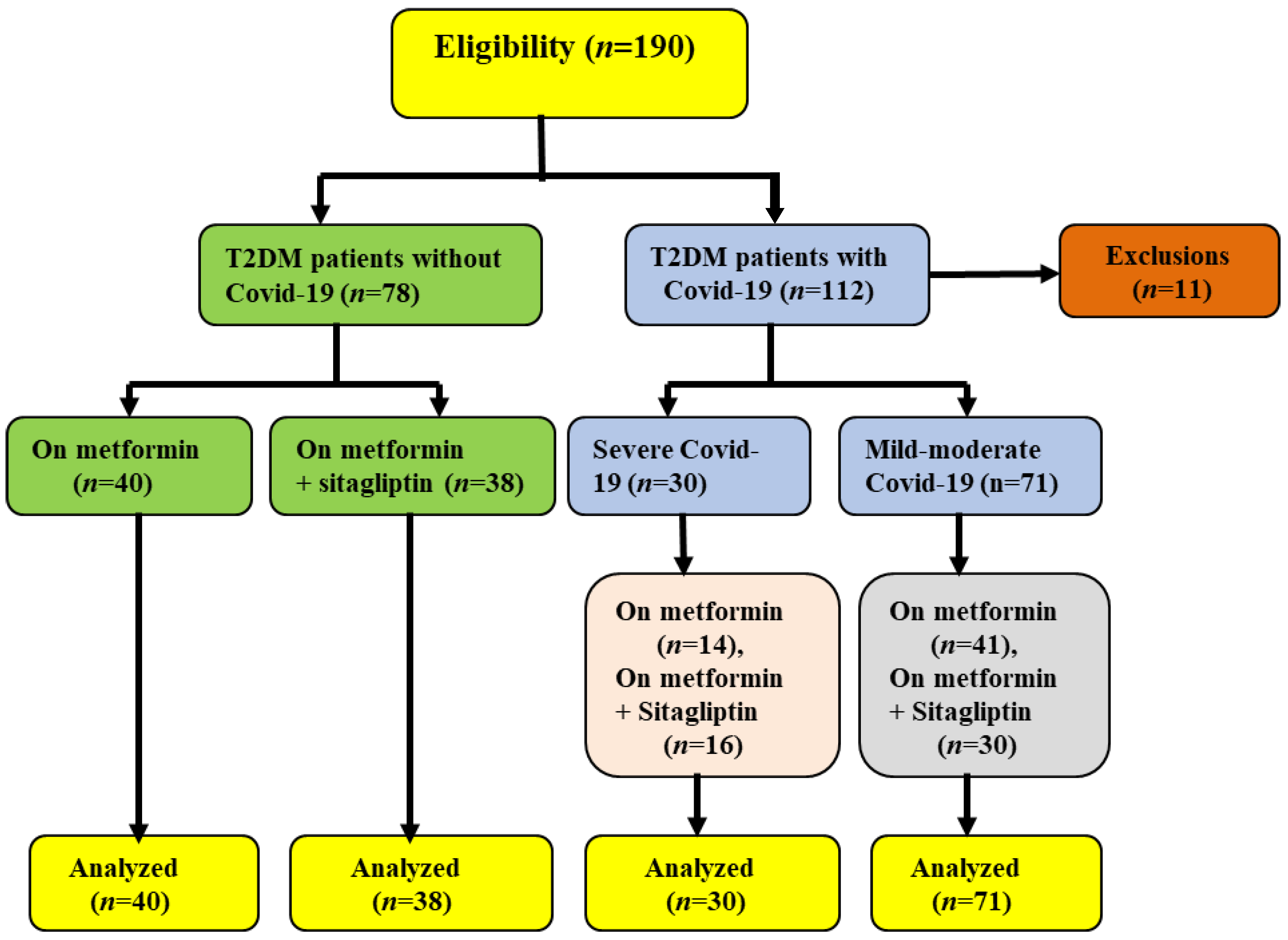
4. Materials and Methods
4.1. Materials and Chemicals
4.2. Patients
4.3. Experimental Protocol
- Group A: T2DM patients with COVID-19 (10 women + 50 men) on metformin treatments 850 mg twice daily plus standard therapy (n = 60).
- Group B: T2DM patients with COVID-19 (12 women + 40 men) on metformin (1000 mg/daily) plus sitagliptin (50 mg/ daily) plus standard therapy (n = 52).
- Group C: T2DM patients without COVID-19 (15 women + 25 men) on metformin treatments 850 mg twice (n = 40).
- Group D: T2DM patients without COVID-19 (13 women + 25 men) on metformin (1000 mg/ daily) plus sitagliptin (50 mg/ daily) (n = 38).
4.4. Inclusion Criteria
4.5. Exclusion Criteria
4.6. Anthropometric Measurements
4.7. Serological and Biochemical Investigations
4.8. Assessment of Pulmonary Radiological Findings
4.9. Assessment of Clinical Outcomes
4.10. Data Analysis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ciotti, M.; Ciccozzi, M.; Terrinoni, A.; Jiang, W.-C.; Wang, C.-B.; Bernardini, S. The COVID-19 pandemic. Crit. Rev. Clin. Lab. Sci. 2020, 57, 365–388. [Google Scholar] [CrossRef] [PubMed]
- Al-Kuraishy, H.M.; Al-Gareeb, A.I.; Alzahrani, K.J.; Cruz-Martins, N.; Batiha, G.E.-S. The potential role of neopterin in Covid-19: A new perspective. Mol. Cell. Biochem. 2021, 476, 4161–4166. [Google Scholar] [CrossRef] [PubMed]
- Al-Kuraishy, H.M.; Al-Gareeb, A.I.; Al-Niemi, M.S.; Al-Buhadily, A.K.; Al-Harchan, N.A.; Lugnier, C. COVID-19 and phosphodiesterase enzyme type 5 inhibitors. J. Microsc. Ultrastruct. 2020, 8, 141. [Google Scholar] [CrossRef]
- Li, Y.; Zhang, Z.; Yang, L.; Lian, X.; Xie, Y.; Li, S.; Xin, S.; Cao, P.; Lu, J. The MERS-CoV receptor DPP4 as a candidate binding target of the SARS-CoV-2 spike. Iscience 2020, 23, 101160. [Google Scholar] [CrossRef] [PubMed]
- Singh, A.K.; Gupta, R.; Ghosh, A.; Misra, A. Diabetes in COVID-19: Prevalence, pathophysiology, prognosis and practical considerations. Diabetes Metab. Syndr. Clin. Res. Rev. 2020, 14, 303–310. [Google Scholar] [CrossRef] [PubMed]
- Pinchera, B.; Scotto, R.; Buonomo, A.; Zappulo, E.; Stagnaro, F.; Gallicchio, A.; Viceconte, G.; Sardanelli, A.; Mercinelli, S.; Villari, R. Diabetes and COVID-19: The potential role of mTOR. Diabetes Res. Clin. Pract. 2022, 186, 109813. [Google Scholar] [CrossRef]
- Al-Kuraishy, H.M.; Sami, O.M.; Hussain, N.R.; Al-Gareeb, A.I. Metformin and/or vildagliptin mitigate type II diabetes mellitus induced-oxidative stress: The intriguing effect. J. Adv. Pharm. Technol. Res. 2020, 11, 142. [Google Scholar] [CrossRef]
- Abdul-Hadi, M.H.; Naji, M.T.; Shams, H.A.; Sami, O.M.; Al-Harchan, N.A.-A.; Al-Kuraishy, H.M.; Al-Gareeb, A.I. Oxidative stress injury and glucolipotoxicity in type 2 diabetes mellitus: The potential role of metformin and sitagliptin. Biomed. Biotechnol. Res. J. (BBRJ) 2020, 4, 166. [Google Scholar]
- Deacon, C.F. Physiology and pharmacology of DPP-4 in glucose homeostasis and the treatment of type 2 diabetes. Front. Endocrinol. 2019, 10, 80. [Google Scholar] [CrossRef]
- Konradi, A.; Villevalde, S.; Duplyakov, D.; Kozlenok, A.; Melnik, O.; Mikhailov, E.; Moiseeva, O.; Nedoshivin, A.; Soloveva, A.; Fokin, V. An open-label multicenter observational study (registry) of patients recovered from coronavirus disease 2019 (COVID-19) with involvement of the cardiovascular system or with baseline severe cardiovascular diseases: Rationale, design, and implications for clinical practice. Russ. J. Cardiol. 2021, 26, 4287. [Google Scholar]
- Mao, L.; Jin, H.; Wang, M.; Hu, Y.; Chen, S.; He, Q.; Chang, J.; Hong, C.; Zhou, Y.; Wang, D. Neurologic manifestations of hospitalized patients with coronavirus disease 2019 in Wuhan, China. JAMA Neurol. 2020, 77, 683–690. [Google Scholar] [CrossRef] [PubMed]
- Al-Kuraishy, H.M.; Al-Gareeb, A.I. COVID-19 and acute kidney injury: A new perspective. Age 2021, 30, 42. [Google Scholar]
- Al-Kuraishy, H.M.; Al-Gareeb, A.I.; Al-Niemi, M.S.; Alexiou, A.; Batiha, G.E. Calprotectin: The link between acute lung injury and gastrointestinal injury in Covid-19: Ban or boon. Curr. Protein Pept. Sci. 2022, 23, 310–320. [Google Scholar]
- Al-Kuraishy, H.M.; Hussien, N.R.; Al-Niemi, M.S.; Al-Gareeb, A.I. Colchicine in the management of Covid-19: With or lieu of evidence. JPMA J. Pak. Med. Assoc. 2021, 71, S127–S132. [Google Scholar]
- Asgary, A.; Blue, H.; Solis, A.O.; McCarthy, Z.; Najafabadi, M.; Tofighi, M.A.; Wu, J. Modeling COVID-19 Outbreaks in Long-Term Care Facilities Using an Agent-Based Modeling and Simulation Approach. Int. J. Environ. Res. Public Health 2022, 19, 2635. [Google Scholar] [CrossRef]
- Dhillon, S. Sitagliptin. Drugs 2010, 70, 489–512. [Google Scholar] [CrossRef] [PubMed]
- Al-Kuraishy, H.M.; Al-Gareeb, A.I.; Faidah, H.; Alexiou, A.; Batiha, G.E.-S. Testosterone in COVID-19: An Adversary Bane or Comrade Boon. Front. Cell. Infect. Microbiol. 2021, 11, 666987. [Google Scholar] [CrossRef]
- Al-Kuraishy, H.M.; Al-Gareeb, A.I.; Alblihed, M.; Guerreiro, S.G.; Cruz-Martins, N.; Batiha, G.E.-S. COVID-19 in relation to hyperglycemia and diabetes mellitus. Front. Cardiovasc. Med. 2021, 8, 644095. [Google Scholar] [CrossRef]
- Liu, B.M.; Martins, T.B.; Peterson, L.K.; Hill, H.R. Clinical significance of measuring serum cytokine levels as inflammatory biomarkers in adult and pediatric COVID-19 cases: A review. Cytokine 2021, 142, 155478. [Google Scholar] [CrossRef]
- Alnima, T.; Mulder, M.M.; van Bussel, B.C.; Ten Cate, H. COVID-19 coagulopathy: From pathogenesis to treatment. Acta Haematol. 2022, 145, 282–296. [Google Scholar] [CrossRef]
- Oguntibeju, O.O. Type 2 diabetes mellitus, oxidative stress and inflammation: Examining the links. Int. J. Physiol. Pathophysiol. Pharmacol. 2019, 11, 45. [Google Scholar] [PubMed]
- Paul, A.K.; Hossain, M.K.; Mahboob, T.; Nissapatorn, V.; Wilairatana, P.; Jahan, R.; Jannat, K.; Bondhon, T.A.; Hasan, A.; de Lourdes Pereira, M. Does oxidative stress management help alleviation of COVID-19 symptoms in patients experiencing diabetes? Nutrients 2022, 14, 321. [Google Scholar] [CrossRef] [PubMed]
- Somasundaram, N.P.; Ranathunga, I.; Ratnasamy, V.; Wijewickrama, P.S.A.; Dissanayake, H.A.; Yogendranathan, N.; Gamage, K.K.K.; de Silva, N.L.; Sumanatilleke, M.; Katulanda, P. The impact of SARS-Cov-2 virus infection on the endocrine system. J. Endocr. Soc. 2020, 4, bvaa082. [Google Scholar] [CrossRef] [PubMed]
- Wang, A.; Zhao, W.; Xu, Z.; Gu, J. Timely blood glucose management for the outbreak of 2019 novel coronavirus disease (COVID-19) is urgently needed. Diabetes Res. Clin. Pract. 2020, 162, 108118. [Google Scholar] [CrossRef]
- Michalakis, K.; Ilias, I. SARS-CoV-2 infection and obesity: Common inflammatory and metabolic aspects. Diabetes Metab. Syndr. Clin. Res. Rev. 2020, 14, 469–471. [Google Scholar] [CrossRef]
- Mehta, P.; McAuley, D.F.; Brown, M.; Sanchez, E.; Tattersall, R.S.; Manson, J.J. COVID-19: Consider cytokine storm syndromes and immunosuppression. Lancet 2020, 395, 1033–1034. [Google Scholar] [CrossRef]
- Babalghith, A.O.; Al-Kuraishy, H.M.; Al-Gareeb, A.I.; De Waard, M.; Al-Hamash, S.M.; Jean-Marc, S.; Negm, W.A.; Batiha, G.E.-S. The role of berberine in COVID-19: Potential adjunct therapy. Inflammopharmacology 2022, 1–14. [Google Scholar] [CrossRef]
- Chhabra, M.; Sharma, S. Potential role of peroxisome proliferator activated receptor gamma analogues in regulation of endothelial progenitor cells in diabetes mellitus: An overview. Diabetes Metab. Syndr. Clin. Res. Rev. 2019, 13, 1123–1129. [Google Scholar] [CrossRef]
- Lu, Y.; Lu, P.; Wang, Y.; Fang, X.; Wu, J.; Wang, X. A novel dipeptidyl peptidase IV inhibitory tea peptide improves pancreatic β-cell function and reduces α-cell proliferation in streptozotocin-induced diabetic mice. Int. J. Mol. Sci. 2019, 20, 322. [Google Scholar] [CrossRef]
- Subir, R. Use of pioglitazone in people with type 2 diabetes mellitus with coronavirus disease 2019 (COVID-19): Boon or bane? Diabetes Metab. Syndr. Clin. Res. Rev. 2020, 14, 829–831. [Google Scholar]
- Zayed, E.A.; AinShoka, A.A.; El Shazly, K.A.; El-Mosallamy, A.; Zayed, A.A.; Abd El Latif, H.A. Fenugreek oil and metformin improve insulin resistance via increase of GLUT4 and PPARγ in metabolic syndrome-induced rats. Asian J. Res. Rep. Endocrinol. 2021, 4, 29–39. [Google Scholar]
- Al-Kuraishy, H.M.; Al-Gareeb, A.I.; Negm, W.A.; Alexiou, A.; Batiha, G.E.-S. Ursolic acid and SARS-CoV-2 infection: A new horizon and perspective. Inflammopharmacology 2022, 30, 1493–1501. [Google Scholar] [CrossRef] [PubMed]
- Kamyshnyi, O.; Matskevych, V.; Lenchuk, T.; Strilbytska, O.; Storey, K.; Lushchak, O. Metformin to decrease COVID-19 severity and mortality: Molecular mechanisms and therapeutic potential. Biomed. Pharmacother. 2021, 144, 112230. [Google Scholar] [CrossRef] [PubMed]
- Samuel, S.M.; Varghese, E.; Büsselberg, D. Therapeutic potential of metformin in COVID-19: Reasoning for its protective role. Trends Microbiol. 2021, 29, 894–907. [Google Scholar] [CrossRef]
- Lukito, A.A.; Pranata, R.; Henrina, J.; Lim, M.A.; Lawrensia, S.; Suastika, K. The effect of metformin consumption on mortality in hospitalized COVID-19 patients: A systematic review and meta-analysis. Diabetes Metab. Syndr. Clin. Res. Rev. 2020, 14, 2177–2183. [Google Scholar] [CrossRef]
- Hasanpour, D.A.; Abbaszadeh, A.; Mir, S.; Hasanvand, A. Metformin and its anti-inflammatory and anti-oxidative effects; new concepts. J. Ren. Inj. Prev. 2019, 8, 54–61. [Google Scholar]
- Wu, L.; Cen, Y.; Feng, M.; Zhou, Y.; Tang, H.; Liao, X.; Wang, Y.; Wang, M.; Zhou, M. Metformin activates the protective effects of the AMPK pathway in acute lung injury caused by paraquat poisoning. Oxidative Med. Cell. Longev. 2019, 2019, 1709718. [Google Scholar] [CrossRef]
- Usman, A.; Bliden, K.P.; Cho, A.; Walia, N.; Jerjian, C.; Singh, A.; Kundan, P.; Duhan, S.; Tantry, U.S.; Gurbel, P.A. Metformin use in patients hospitalized with COVID-19: Lower inflammation, oxidative stress, and thrombotic risk markers and better clinical outcomes. J. Thromb. Thrombolysis 2022, 53, 363–371. [Google Scholar] [CrossRef]
- Xin, G.; Wei, Z.; Ji, C.; Zheng, H.; Gu, J.; Ma, L.; Huang, W.; Morris-Natschke, S.L.; Yeh, J.-L.; Zhang, R. Metformin uniquely prevents thrombosis by inhibiting platelet activation and mtDNA release. Sci. Rep. 2016, 6, 36222. [Google Scholar] [CrossRef]
- Katsiki, N.; Ferrannini, E. Anti-inflammatory properties of antidiabetic drugs: A “promised land” in the COVID-19 era? J. Diabetes Its Complicat. 2020, 34, 107723. [Google Scholar] [CrossRef]
- Goodman, B.P.; Khoury, J.A.; Blair, J.E.; Grill, M.F. COVID-19 dysautonomia. Front. Neurol. 2021, 12, 624968. [Google Scholar] [CrossRef] [PubMed]
- Bardaweel, S.K.; Hajjo, R.; SABBAH, A. Sitagliptin: A potential drug for the treatment of COVID-19? Acta Pharm. 2021, 71, 175–184. [Google Scholar] [CrossRef] [PubMed]
- Abbasi, F.; Adatorwovor, R.; Davarpanah, M.A.; Mansoori, Y.; Hajiani, M.; Azodi, F.; Sefidbakht, S.; Davoudi, S.; Rezaei, F.; Mohammadmoradi, S. A Randomized Trial of Combination Therapy, Sitagliptin and Spironolactone, in Hospitalized Adult Patients with COVID-19. J. Endocr. Soc. 2022, 6, bvac017. [Google Scholar] [CrossRef] [PubMed]
- Mozafari, I. A Bridge Between Diabetes and COVID-19, and Possible Management With Sitagliptin. Med. Hypotheses 2020, 143, 110111. [Google Scholar] [CrossRef] [PubMed]
- Hasan, S.S.; Kow, C.S.; Bain, A.; Kavanagh, S.; Merchant, H.A.; Hadi, M.A. Pharmacotherapeutic considerations for the management of diabetes mellitus among hospitalized COVID-19 patients. Expert Opin. Pharmacother. 2021, 22, 229–240. [Google Scholar] [CrossRef]
- ÇAKINA, S.; Öztürk, Ş. Oxidative stress markers in liver in streptozocin-induced diabetic rats: Effects of metformin and sitagliptin. Cukurova Med. J. 2021, 45, 1733–1741. [Google Scholar] [CrossRef]
- Kawasaki, T.; Chen, W.; Htwe, Y.M.; Tatsumi, K.; Dudek, S.M. DPP4 inhibition by sitagliptin attenuates LPS-induced lung injury in mice. Am. J. Physiol.-Lung Cell. Mol. Physiol. 2018, 315, L834–L845. [Google Scholar] [CrossRef]
- Coll, A.P.; Chen, M.; Taskar, P.; Rimmington, D.; Patel, S.; Tadross, J.A.; Cimino, I.; Yang, M.; Welsh, P.; Virtue, S. GDF15 mediates the effects of metformin on body weight and energy balance. Nature 2020, 578, 444–448. [Google Scholar] [CrossRef]
- Chiang, S.-M.; Ueng, K.-C.; Yang, Y.-S. Gender differences in variables associated with dipeptidyl peptidase 4 genetic polymorphisms in coronary artery disease. Adv. Clin. Exp. Med. 2020, 29, 1181–1186. [Google Scholar] [CrossRef]
- Chung, W.K.; Erion, K.; Florez, J.C.; Hattersley, A.T.; Hivert, M.-F.; Lee, C.G.; McCarthy, M.I.; Nolan, J.J.; Norris, J.M.; Pearson, E.R. Precision medicine in diabetes: A consensus report from the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care 2020, 43, 1617–1635. [Google Scholar] [CrossRef]
- Carod-Artal, F.J. Post-COVID-19 syndrome: Epidemiology, diagnostic criteria and pathogenic mechanisms involved. Rev. De Neurol. 2021, 72, 384–396. [Google Scholar]
- Hemming, K.; Kasza, J.; Hooper, R.; Forbes, A.; Taljaard, M. A tutorial on sample size calculation for multiple-period cluster randomized parallel, crossover and stepped-wedge trials using the Shiny CRT Calculator. Int. J. Epidemiol. 2020, 49, 979–995. [Google Scholar] [CrossRef] [PubMed]
- Moscou, S. Getting the word out: Advocacy, social marketing, and policy development and enforcement. In Public Health Nursing: Practicing Population-Based Care; Truglio-Londrigan, M., Ed.; Jones & Bartlett Publishers: Burlington, MA, USA, 2010; p. 285. [Google Scholar]
- Francone, M.; Iafrate, F.; Masci, G.M.; Coco, S.; Cilia, F.; Manganaro, L.; Panebianco, V.; Andreoli, C.; Colaiacomo, M.C.; Zingaropoli, M.A. Chest CT score in COVID-19 patients: Correlation with disease severity and short-term prognosis. Eur. Radiol. 2020, 30, 6808–6817. [Google Scholar] [CrossRef] [PubMed]


| Variables | Group I | Group II | Group III | A | B | C | ANOVA |
|---|---|---|---|---|---|---|---|
| (n = 40) | (n = 41) | (n = 14) | |||||
| SBP (mmHg) | 143.67 ±11.56 | 140.41 ± 10.93 | 140.78 ± 9.53 | NS | NS | NS | 0.38 |
| DBP (mmHg) | 89.85 ±7.33 | 82.56 ± 5.85 | 73.91 ± 6.61 | 0.0001 | 0.0001 | 0.0001 | 0.0001 |
| MAP (mmHg) | 107.80 ± 4.12 | 101.80 ± 3.99 | 96.2 ± 4.41 | 0.01 | 0.0001 | 0.0001 | 0.0001 |
| PP (mmHg) | 53.81 ± 3.07 | 57.84 ± 4.67 | 66.87 ± 3.94 | 0.01 | 0.0001 | 0.0001 | 0.0001 |
| FBG (mg/dL) | 144.72 ± 6.92 | 159.62 ± 8.46 | 187.91 ± 9.54 | 0.01 | 0.0001 | 0.0001 | 0.0001 |
| HbA1c (%) | 7.23 ± 1.31 | 7.07 ± 1.55 | 7.51 ± 1.31 | NS | NS | NS | 0.59 |
| FSI (µIU/mL) | 19.85 ± 6.97 | 19.47 ± 8.38 | 27.08 ± 8.44 | NS | 0.01 | 0.006 | 0.006 |
| HOMA2-IR | 2.81 ± 1.04 | 2.82 ± 1.07 | 3.98 ± 1.06 | NS | 0.001 | 0.001 | 0.006 |
| β-cell function (%) | 75.00 ± 6.84 | 61.9 ± 5.90 | 56.9 ± 5.33 | 0.0001 | 0.0001 | 0.03 | 0.0001 |
| IS (%) | 35.60 ± 6.98 | 35.62 ± 4.07 | 25.13 ± 3.02 | NS | 0.0001 | 0.0001 | 0.0001 |
| TC (mg/dL) | 198.68 ± 12.81 | 141.64 ± 9.51 | 130.91 ± 5.82 | 0.0001 | 0.0001 | 0.0001 | 0.0001 |
| TG (mg/dL) | 223.95 ± 14.78 | 230.61 ± 13.20 | 274.12 ± 6.11 | NS | 0.0001 | 0.0001 | 0.0001 |
| HDL-c (mg/dL) | 43.61 ± 7.33 | 37.05 ± 6.04 | 31.63 ± 6.81 | 0.0001 | 0.0001 | 0.02 | 0.0001 |
| LDL (mg/dL) | 110.3 ± 6.39 | 58.5 ± 4.38 | 44.50 ± 4.05 | 0.0001 | 0.0001 | 0.01 | 0.0001 |
| VLDL (mg/dL) | 44.79 ± 4.33 | 46.12 ± 4.11 | 54.82 ± 3.61 | NS | 0.0001 | 0.0001 | 0.0001 |
| Non-HDL-c (mg/dL) | 155.07 ± 9.57 | 104.59 ± 9.39 | 99.28 ± 6.03 | NS | 0.0001 | NS | 0.0001 |
| AI | 0.71 ± 0.01 | 0.77 ± 0.02 | 0.93 ± 0.04 | 0.0001 | NS | 0.03 | 0.0001 |
| AC | 5.55 ± 1.02 | 2.82 ± 1.04 | 3.13 ± 1.02 | 0.0001 | 0.0001 | NS | 0.0001 |
| CRR | 4.55 ± 1.72 | 3.82 ± 1.02 | 4.13 ± 1.06 | NS | NS | NS | 0.06 |
| CVRI | 5.36 ± 2.29 | 6.22 ± 2.99 | 8.66 ± 3.06 | NS | 0.005 | 0.01 | 0.0009 |
| SaO2 (%) | 99.86 ± 1.23 | 98.89 ± 1.76 | 90.04 ± 3.15 | NS | 0.0001 | 0.0001 | 0.0001 |
| CT scan score (%) | ………….. | 3.82 ± 1.27 | 40.61 ± 3.85 | ……. | …….. | 0.0001 | …….. |
| WBC (103/µL) | 8.09 ± 2.41 | 10.90 ± 3.04 | 16.38 ± 4.57 | 0.03 | 0.0001 | 0.0001 | 0.0001 |
| Neutrophils (%) | 75.91 ± 6.80 | 79.31 ± 8.59 | 88.53 ± 7.18 | NS | 0.0001 | 0.0001 | 0.0001 |
| Lymphocytes (%) | 24.73 ± 3.05 | 20.82 ± 4.65 | 13.62 ± 5.71 | 0.002 | 0.0001 | 0.0001 | 0.0001 |
| NLR | 3.06 ± 1.09 | 3.80 ± 1.99 | 6.51 ± 2.04 | NS | 0.0001 | 0.0001 | 0.0001 |
| CRP (mg/L) | 7.02 ± 2.06 | 10.42 ± 3.11 | 21.72 ± 5.19 | 0.02 | 0.0001 | 0.0001 | 0.0001 |
| Ferritin (ng/mL) | 190.38 ± 13.97 | 257.31 ± 15.33 | 494.31 ± 11.39 | 0.0001 | 0.0001 | 0.0001 | 0.0001 |
| LDH (U/L) | 110.83 ± 9.92 | 267.68 ± 11.97 | 382.68 ± 12.11 | 0.0001 | 0.0001 | 0.04 | 0.0001 |
| D-dimer (ng/mL) | 200.16 ± 10.11 | 283.68 ± 13.01 | 463.82 ± 10.11 | 0.0001 | 0.0001 | 0.02 | 0.0001 |
| PCT (ng/mL) | 0.06 ± 0.01 | 0.18 ± 0.03 | 0.26 ± 0.05 | 0.0001 | 0.0001 | 0.003 | 0.0001 |
| Variables | Group I | Group II | Group III | A | B | C | ANOVA |
|---|---|---|---|---|---|---|---|
| (n = 38) | (n = 30) | (n = 16) | |||||
| BMI (kg/m2) | 30.66 ± 4.63 | 31.74 ± 3.99 | 32.82 ± 3.99 | NS | NS | NS | 0.22 |
| SBP (mmHg) | 145.85 ± 11.63 | 139.69 ± 11.81 | 137.06 ± 10.59 | NS | 0.03 | NS | 0.01 |
| DBP (mmHg) | 90.01 ± 6.89 | 81.75 ± 6.32 | 68.61 ± 8.64 | 0.0001 | 0.0001 | 0.0001 | 0.0001 |
| MAP (mmHg) | 108.60 ± 4.96 | 101.10 ± 4.03 | 91.40 ± 4.32 | 0.0001 | 0.0001 | 0.0001 | 0.0001 |
| PP (mmHg) | 55.83 ± 3.45 | 57.94 ± 4.69 | 68.45 ± 5.19 | NS | 0.0001 | 0.0001 | 0.0001 |
| FBG (mg/dL) | 133.06 ± 7.22 | 148.53 ± 6.85 | 157.91 ± 7.54 | 0.0001 | 0.0001 | 0.0002 | 0.0001 |
| HbA1c (%) | 7.01 ± 1.99 | 7.52 ± 1.21 | 7.02 ± 1.44 | NS | NS | NS | 0.4 |
| FSI (µIU/mL) | 17.04 ± 8.11 | 18.11 ± 6.94 | 22.03 ± 8.17 | NS | NS | NS | 0.09 |
| HOMA2-IR | 2.38 ± 1.03 | 2.58 ± 1.05 | 3.15 ± 1.08 | NS | 0.04 | NS | 0.05 |
| β-cell function (%) | 77.7 ± 8.93 | 66.7 ± 6.47 | 69.50 ± 7.05 | 0.0001 | 0.0001 | NS | 0.0001 |
| IS (%) | 42.0 ± 5.06 | 38.7 ± 6.33 | 31.70 ± 4.39 | 0.03 | 0.0001 | 0.0002 | 0.0001 |
| TC (mg/dL) | 183.07 ± 11.91 | 139.06 ± 9.61 | 133.21 ± 6.04 | 0.0001 | 0.0001 | NS | 0.0001 |
| TG (mg/dL) | 214.51 ± 12.79 | 231.93 ± 13.74 | 264.33 ± 9.33 | 0.0001 | 0.0001 | 0.0001 | 0.0001 |
| HDL-c (mg/dL) | 44.94 ± 7.08 | 38.05 ± 6.44 | 33.93 ± 6.51 | 0.0002 | 0.0001 | NS | 0.0001 |
| LDL (mg/dL) | 95.2 ± 4.99 | 54.2 ± 4.22 | 46.40 ± 3.22 | 0.0001 | 0.0001 | 0.03 | 0.0001 |
| VLDL (mg/dL) | 42.90 ± 4.99 | 46.38 ± 4.69 | 52.86 ± 5.31 | 0.01 | 0.0001 | 0.0001 | 0.0001 |
| Non-HDL-c (mg/dL) | 138.13 ± 8.19 | 101.01 ± 7.73 | 99.28 ± 5.81 | 0.0001 | 0.0001 | NS | 0.0001 |
| AI | 0.67 ± 0.02 | 0.78 ± 0.01 | 0.89 ± 0.02 | NS | NS | 0.0001 | 0.0001 |
| AC | 3.07 ± 2.66 | 2.65 ± 1.22 | 2.92 ± 1.04 | NS | NS | NS | 0.68 |
| CRR | 4.07 ± 1.09 | 3.65 ± 1.33 | 3.92 ± 1.19 | NS | NS | NS | 0.36 |
| CVRI | 4.77 ± 2.56 | 6.09 ± 2.58 | 7.79 ± 3.09 | NS | 0.008 | NS | 0.001 |
| SaO2 (%) | 99.31 ± 2.21 | 98.05 ± 2.29 | 94.04 ± 2.02 | NS | 0.0001 | 0.0001 | 0.0001 |
| CT scan (%) | ………….. | 3.01 ± 1.12 | 35.17 ± 2.36 | ……. | …….. | 0.0001 | ………. |
| WBC (103/µL) | 8.79 ± 2.81 | 10.57 ± 3.55 | 14.29 ± 3.24 | NS | 0.0001 | 0.0008 | 0.0001 |
| Neutrophils (%) | 73.31 ± 5.41 | 77.31 ± 8.04 | 78.91 ± 6.08 | 0.03 | 0.01 | NS | 0.006 |
| Lymphocytes (%) | 27.06 ± 3.63 | 19.03 ± 4.85 | 17.51 ± 4.61 | 0.0001 | 0.0001 | NS | 0.0001 |
| NLR | 2.70 ± 1.22 | 4.06 ± 1.84 | 4.50 ± 1.97 | 0.002 | 0.001 | NS | 0.0001 |
| CRP (mg/L) | 6.45 ± 2.09 | 11.32 ± 3.04 | 20.41 ± 6.04 | 0.01 | 0.0001 | 0.0001 | 0.0001 |
| Ferritin (ng/mL) | 187.27 ± 14.97 | 249.36 ± 14.11 | 464.62 ± 12.78 | 0.0001 | 0.0001 | 0.0001 | 0.0001 |
| LDH (U/L) | 113.31 ± 10.03 | 272.41 ± 11.02 | 372.38 ± 13.81 | 0.0001 | 0.0001 | 0.0001 | 0.0001 |
| D-dimer (ng/mL) | 207.85 ± 11.61 | 294.83 ± 12.54 | 413.05 ± 14.73 | 0.0001 | 0.0001 | 0.0001 | 0.0001 |
| PCT (ng/mL) | 0.09 ± 0.02 | 0.16 ± 0.03 | 0.21 ± 0.02 | 0.0001 | 0.0001 | 0.0001 | 0.0001 |
| Variables | Mild-Moderate COVID-19 | p | Severe COVID-19 | p | ||
|---|---|---|---|---|---|---|
| Group I (n = 30) | Group II (n = 41) | Group III (n = 14) | Group IV (n = 16) | |||
| BMI (kg/m2) | 31.83 ± 4.22 | 31.74 ± 3.99 | NS | 35.09 ± 4.99 | 32.82 ± 3.99 | NS |
| SBP (mmHg) | 140.41 ± 10.93 | 139.69 ± 11.81 | NS | 140.78 ± 9.53 | 137.06 ± 10.59 | NS |
| DBP (mmHg) | 82.56 ± 5.85 | 81.75 ± 6.32 | NS | 73.91 ± 6.61 | 68.61 ± 8.64 | NS |
| MAP (mmHg) | 101.80 ± 3.99 | 101.10 ± 4.03 | NS | 96.20 ± 4.41 | 91.40 ± 4.32 | 0.005 |
| PP (mmHg) | 57.84 ± 4.67 | 57.94 ± 4.69 | NS | 66.87 ± 3.94 | 68.45 ± 5.19 | NS |
| FBG (mg/dL) | 159.62 ± 8.46 | 148.53 ± 6.85 | 0.001 | 187.91 ± 9.54 | 157.91 ± 7.54 | 0.001 |
| HbA1c (%) | 7.07 ± 1.55 | 7.52 ± 1.21 | NS | 7.51 ± 1.31 | 7.02 ± 1.44 | NS |
| FSI (µIU/mL) | 19.47 ± 8.38 | 18.11 ± 6.94 | NS | 27.08 ± 8.44 | 22.03 ± 8.17 | NS |
| HOMA2-IR | 2.82 ± 1.07 | 2.58 ± 1.05 | NS | 3.98 ± 1.06 | 3.15 ± 1.08 | NS |
| β-cell function (%) | 61.9 ± 5.90 | 66.7 ± 6.47 | 0.001 | 56.9 ± 5.33 | 69.50 ± 7.05 | 0.001 |
| IS (%) | 35.62 ± 4.07 | 38.7 ± 6.33 | 0.01 | 25.13 ± 3.02 | 31.70 ± 4.39 | 0.001 |
| TC (mg/dL) | 141.64 ± 9.51 | 139.06 ± 9.61 | NS | 130.91 ± 5.82 | 133.21 ± 6.04 | NS |
| TG (mg/dL) | 230.61 ± 13.20 | 231.93 ± 13.74 | NS | 274.12 ± 6.11 | 264.33 ± 9.33 | 0.002 |
| HDL-c (mg/dL) | 37.05 ± 6.04 | 38.05 ± 6.44 | NS | 31.63 ± 6.81 | 33.93 ± 6.51 | NS |
| LDL (mg/dL) | 58.5 ± 4.38 | 54.2 ± 4.22 | 0.001 | 44.50 ± 4.05 | 46.40 ± 3.22 | NS |
| VLDL (mg/dL) | 46.12 ± 4.11 | 46.38 ± 4.69 | NS | 54.82 ± 3.61 | 52.86 ± 5.31 | NS |
| Non-HDL-c (mg/dL) | 104.59 ± 9.39 | 101.01 ± 7.73 | NS | 99.28 ± 6.03 | 99.28 ± 5.81 | NS |
| AI | 0.77 ± 0.02 | 0.78 ± 0.01 | NS | 0.93 ± 0.04 | 0.89 ± 0.02 | 0.001 |
| AC | 2.82 ± 1.04 | 2.65 ± 1.22 | NS | 3.13 ± 1.02 | 2.92 ± 1.04 | NS |
| CRR | 3.82 ± 1.02 | 3.65 ± 1.33 | NS | 4.13 ± 1.06 | 3.92 ± 1.19 | NS |
| CVRI | 6.22 ± 2.99 | 6.09 ± 2.58 | NS | 8.66 ± 3.06 | 7.79 ± 3.09 | NS |
| SaO2 (%) | 98.89 ± 1.76 | 98.05 ± 2.29 | NS | 90.04 ± 3.15 | 94.04 ± 2.02 | 0.0002 |
| CT scan score (%) | 3.82 ± 1.27 | 3.01 ± 1.12 | NS | 40.61 ± 3.85 | 35.17 ± 2.36 | 0.001 |
| WBC (103/µL) | 10.90 ± 3.04 | 10.57 ± 3.55 | NS | 16.38 ± 4.57 | 14.29 ± 3.24 | NS |
| Neutrophils (%) | 79.31 ± 8.59 | 77.31 ± 8.04 | NS | 88.53 ± 7.18 | 78.91 ± 6.08 | 0.0004 |
| Lymphocytes (%) | 20.82 ± 4.65 | 19.03 ± 4.85 | NS | 13.62 ± 5.71 | 17.51 ± 4.61 | 0.04 |
| NLR | 3.80 ± 1.99 | 4.06 ± 1.84 | NS | 6.51 ± 2.04 | 4.50 ± 1.97 | 0.01 |
| CRP (mg/L) | 10.42 ± 3.11 | 11.32 ± 3.04 | NS | 21.72 ± 5.19 | 20.41 ± 6.04 | NS |
| Ferritin (ng/mL) | 257.31 ± 15.33 | 249.36 ± 14.11 | 0.02 | 494.31 ± 11.39 | 464.62 ± 12.78 | 0.001 |
| LDH (U/L) | 267.68 ± 11.97 | 272.41 ± 11.02 | NS | 382.68 ± 12.11 | 372.38 ± 13.81 | 0.03 |
| D-dimer (ng/mL) | 283.68 ± 13.01 | 294.83 ± 12.54 | 0.0006 | 463.82 ± 10.11 | 413.05 ± 14.73 | 0.001 |
| PCT (ng/mL) | 0.18 ± 0.03 | 0.16 ± 0.03 | NS | 0.26 ± 0.05 | 0.21 ± 0.02 | 0.001 |
| Variables | Total | Men | Women | p |
|---|---|---|---|---|
| n | 101 (100%) | 79 (78.21%) | 22 (21.78%) | 0.001 |
| On metformin only | 55 (54.45%) | 45 (56.96%) | 10 (45.45%) | 0.34 |
| Mild-moderate | 41 (74.54%) | 34 (75.56%) * | 7 (70.00%) ** | 0.59 |
| Severe | 14 (25.45%) | 11 (24.44%) | 3 (30.00%) | 0.59 |
| On metformin plus sitagliptin | 46 (45.54%) | 34 (43.03%) | 12 (54.54%) | 0.34 |
| Mild-moderate | 30 (65.21%) | 20 (58.82%) | 10 (83.33%) *** | 0.02 |
| Severe | 16 (34.78) | 14 (41.17%) | 2 (16.66%) | 0.03 |
| Variables | Mild-Moderate COVID-19 | p | Severe COVID-19 | p | ||
|---|---|---|---|---|---|---|
| Group I (n = 40) | Group II (n = 30) | Group III (n = 11) | Group IV (n = 15) | |||
| BMI (kg/m2) | 31.97 ± 4.95 | 31.33 ± 3.21 | NS | 35.11 ± 4.32 | 32.74 ± 3.98 | NS |
| SBP (mmHg) | 141.83 ± 10.07 | 140.69 ± 10.11 | NS | 142.05 ± 9.38 | 139.89 ± 9.36 | NS |
| DBP (mmHg) | 80.78 ± 5.31 | 80.94 ± 5.39 | NS | 75.04 ± 6.93 | 76.03 ± 6.91 * | NS |
| MAP (mmHg) | 101.13 ± 3.53 | 100.68 ± 4.72 | NS | 97.38 ± 4.91 | 91.40 ± 4.32 * | 0.002 |
| PP (mmHg) | 61.05 ± 4.84 * | 59.57 ± 4.22 | NS | 67.01 ± 3.41 * | 68.49 ± 5.19 | NS |
| FBG (mg/dL) | 112.92 ± 7.03 * | 103.99 ± 7.11 # | 0.001 | 127.03 ± 6.91 * | 117.56 ± 6.44 * | 0.001 |
| HbA1c (%) | 7.07 ± 1.55 | 7.52 ± 1.21 | NS | 7.51 ± 1.31 | 7.02 ± 1.44 | NS |
| FSI (µIU/mL) | 12.06 ± 2.66 * | 9.11 ± 2.61 # | 0.01 | 17.08 ± 4.18 * | 12.09 ± 5.36 * | 0.01 |
| HOMA2-IR | 1.64 ± 0.25 * | 1.22 ± 0.05 # | NS | 2.36 ± 1.05 * | 1.66 ± 1.08 * | NS |
| β-cell function (%) | 84.3 ± 7.04 * | 81. 8 ± 7.33 # | NS | 84.8 ± 5.11 * | 77.6 ± 5.09 * | 0.001 |
| IS (%) | 61.00 ± 8.31 * | 81.9 ± 8.91 # | 0.01 | 42.3 ± 3.02 * | 60.3 ± 4.05 # | 0.001 |
| TC (mg/dL) | 160.05 ± 8.21 * | 165.06 ± 8.99 # | 0.01 | 167.21 ± 5.82 * | 163.47 ± 5.94 # | NS |
| TG (mg/dL) | 168.03 ± 9.10 * | 161.73 ± 9.57 # | 0.01 | 178.19 ± 4.22 * | 174.64 ± 4.03 # | 0.03 |
| HDL-c (mg/dL) | 43.05 ± 5.22 * | 48.05 ± 5.92 # | 0.03 | 40.44 ± 5.03 * | 43.51 ± 5.81 # | NS |
| LDL (mg/dL) | 83.4 ± 6.06 * | 84.7 ± 4.73 # | NS | 91.05 ± 4.68 * | 85.00 ± 4.29 # | 0.02 |
| VLDL (mg/dL) | 33.66 ± 5.21 * | 32.34 ± 5.03 # | NS | 35.63 ± 3.93 * | 34.92 ± 5.31 # | NS |
| Non-HDL-c (mg/dL) | 117.00 ± 8.05 * | 117.01 ± 8.91 # | NS | 126.77 ± 5.11 * | 119.96 ± 5.06 # | 0.03 |
| AI | 0.59 ± 0.01 * | 0.52 ± 0.02 # | 0.01 | 0.64 ± 0.03 * | 0.60 ± 0.01 # | 0.01 |
| AC | 2.71 ± 1.48 * | 2.43 ± 1.29 # | NS | 3.17 ± 1.09 * | 2.79 ± 1.02 # | NS |
| CRR | 3.71 ± 1.09 * | 3.43 ± 1.33 # | NS | 4.17 ± 1.02 * | 3.79 ± 1.05 # | NS |
| CVRI | 3.90 ± 1.92 * | 3.35 ± 1.22 # | NS | 4.45 ± 1.01 * | 4.04 ± 1.22 # | NS |
| SaO2 (%) | 99.91 ± 1.01 | 99.05 ± 1.04 | NS | 96.04 ± 3.21 * | 97.09 ± 2.09 # | NS |
| CT scan score (%) | ………….. | …………. | ….. | 10.12 ± 2.01 * | 4.01 ± 1.99 # | 0.001 |
| Clinical score (0–7) | …………… | ………….. | …… | 2.31 ± 1.05 * | 1.03 ± 0.61 # | 0.01 |
| WBC (103/µL) | 8.39 ± 2.01 * | 10.57 ± 3.55 # | 0.001 | 11.38 ± 3.88 * | 14.29 ± 3.24 # | 0.04 |
| Neutrophils (%) | 75.91 ± 5.19 * | 74.31 ± 5.09 # | NS | 78.27 ± 3.19 * | 77.91 ± 5.09 # | NS |
| Lymphocytes (%) | 25.92 ± 3.65 * | 26.03 ± 3.04 # | NS | 20.69 ± 2.02 | 23.51 ± 3.65 # | 0.02 |
| NLR | 2.92 ± 1.99 * | 2.85 ± 1.84 # | NS | 3.78 ± 2.55 * | 3.31 ± 2.02 # | NS |
| CRP (mg/L) | 3.21 ± 1.57 * | 3.83 ± 1.51 # | NS | 7.53 ± 2.19 * | 8.25 ± 3.82 # | NS |
| Ferritin (ng/mL) | 159.61 ± 7.82 * | 149.36 ± 6.04 # | 0.001 | 286.31 ± 6.04 * | 260.62 ± 8.06 # | 0.001 |
| LDH (U/L) | 257.68 ± 9.97 * | 261.10 ± 10.33 # | NS | 350.23 ± 11.12 * | 359.22 ± 12.35 # | NS |
| D-dimer (ng/mL) | 144.93 ± 8.55 * | 131.02 ± 5.82 # | 0.01 | 211.02 ± 6.88 * | 201.05 ± 5.12 # | 0.0002 |
| PCT (ng/mL) | 0.10 ± 0.01* | 0.09 ± 0.01 # | NS | 0.14 ± 0.03 * | 0.11 ± 0.02 # | NS |
| Variables | Total | Men | Women | p |
|---|---|---|---|---|
| n | 96 (100%) | 74 (77.08%) | 22 (21.91%) | 0.001 |
| On metformin only | 51 (53.12%) | 41 (55.40%) | 10 (45.45% | 0.41 |
| Mild-moderate | 40 (78.43%) | 33 (80.48%) * | 7 (70.00%) ** | 0.29 |
| Severe | 11 (21.56%) | 8 (19.51%) | 3 (30.00%) | 0.29 |
| On metformin plus sitagliptin | 45 (46.87%) | 33 (44.59%) | 12 (54.54%) | 0.41 |
| Mild-moderate | 30 (66.67%) | 20 (60.60%) | 10 (83.33%) *** | 0.04 |
| Severe | 15 (33.30%) | 13 (39.39%) | 2 (16.66%) | 0.04 |
| Mortality rate | 5 (5.2%) | 5 (6.75%) | ………….. | |
| Mild-moderate | 1 (20.00%) # | 1 (1.35%) # | ………….. | |
| Severe | 4 (4.16%) | 4 (5.40%) | …………… |
| Scores | Interpretations |
|---|---|
| I | Patient has normal activity and does not need hospitalization. |
| II | Patient has sub-normal activity and does not need hospitalization. |
| III | Patient needs to be hospitalized without the need for oxygen therapy. |
| IV | Patient needs to be hospitalized and non-invasive oxygen therapy. |
| V | Patient needs to be hospitalized and invasive oxygen therapy. |
| VI | Patient needs to be hospitalized and mechanical ventilation. |
| VII | Death. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Al-Kuraishy, H.M.; Al-Gareeb, A.I.; Albogami, S.M.; Jean-Marc, S.; Nadwa, E.H.; Hafiz, A.A.; A. Negm, W.; Kamal, M.; Al-Jouboury, M.; Elekhnawy, E.; et al. Potential Therapeutic Benefits of Metformin Alone and in Combination with Sitagliptin in the Management of Type 2 Diabetes Patients with COVID-19. Pharmaceuticals 2022, 15, 1361. https://doi.org/10.3390/ph15111361
Al-Kuraishy HM, Al-Gareeb AI, Albogami SM, Jean-Marc S, Nadwa EH, Hafiz AA, A. Negm W, Kamal M, Al-Jouboury M, Elekhnawy E, et al. Potential Therapeutic Benefits of Metformin Alone and in Combination with Sitagliptin in the Management of Type 2 Diabetes Patients with COVID-19. Pharmaceuticals. 2022; 15(11):1361. https://doi.org/10.3390/ph15111361
Chicago/Turabian StyleAl-Kuraishy, Hayder M., Ali I. Al-Gareeb, Sarah M. Albogami, Sabatier Jean-Marc, Eman Hassan Nadwa, Amin A. Hafiz, Walaa A. Negm, Marwa Kamal, Mohammed Al-Jouboury, Engy Elekhnawy, and et al. 2022. "Potential Therapeutic Benefits of Metformin Alone and in Combination with Sitagliptin in the Management of Type 2 Diabetes Patients with COVID-19" Pharmaceuticals 15, no. 11: 1361. https://doi.org/10.3390/ph15111361
APA StyleAl-Kuraishy, H. M., Al-Gareeb, A. I., Albogami, S. M., Jean-Marc, S., Nadwa, E. H., Hafiz, A. A., A. Negm, W., Kamal, M., Al-Jouboury, M., Elekhnawy, E., Batiha, G. E.-S., & Waard, M. D. (2022). Potential Therapeutic Benefits of Metformin Alone and in Combination with Sitagliptin in the Management of Type 2 Diabetes Patients with COVID-19. Pharmaceuticals, 15(11), 1361. https://doi.org/10.3390/ph15111361











