Neuroprotective Effect of Artichoke-Based Nanoformulation in Sporadic Alzheimer’s Disease Mouse Model: Focus on Antioxidant, Anti-Inflammatory, and Amyloidogenic Pathways
Abstract
:1. Introduction
2. Results and Discussion
2.1. Assessment of Total Phenolic Content (TPC) and Total Flavonoids Content (TFC)
2.2. Metabolite Profiling via UPLC-ESI-MS/MS
2.3. Determination of ART Antioxidant Potential
2.4. Preparation of Artichoke Loaded SLNs
2.5. Particle Size, Zeta Potential and Entrapment Efficiency
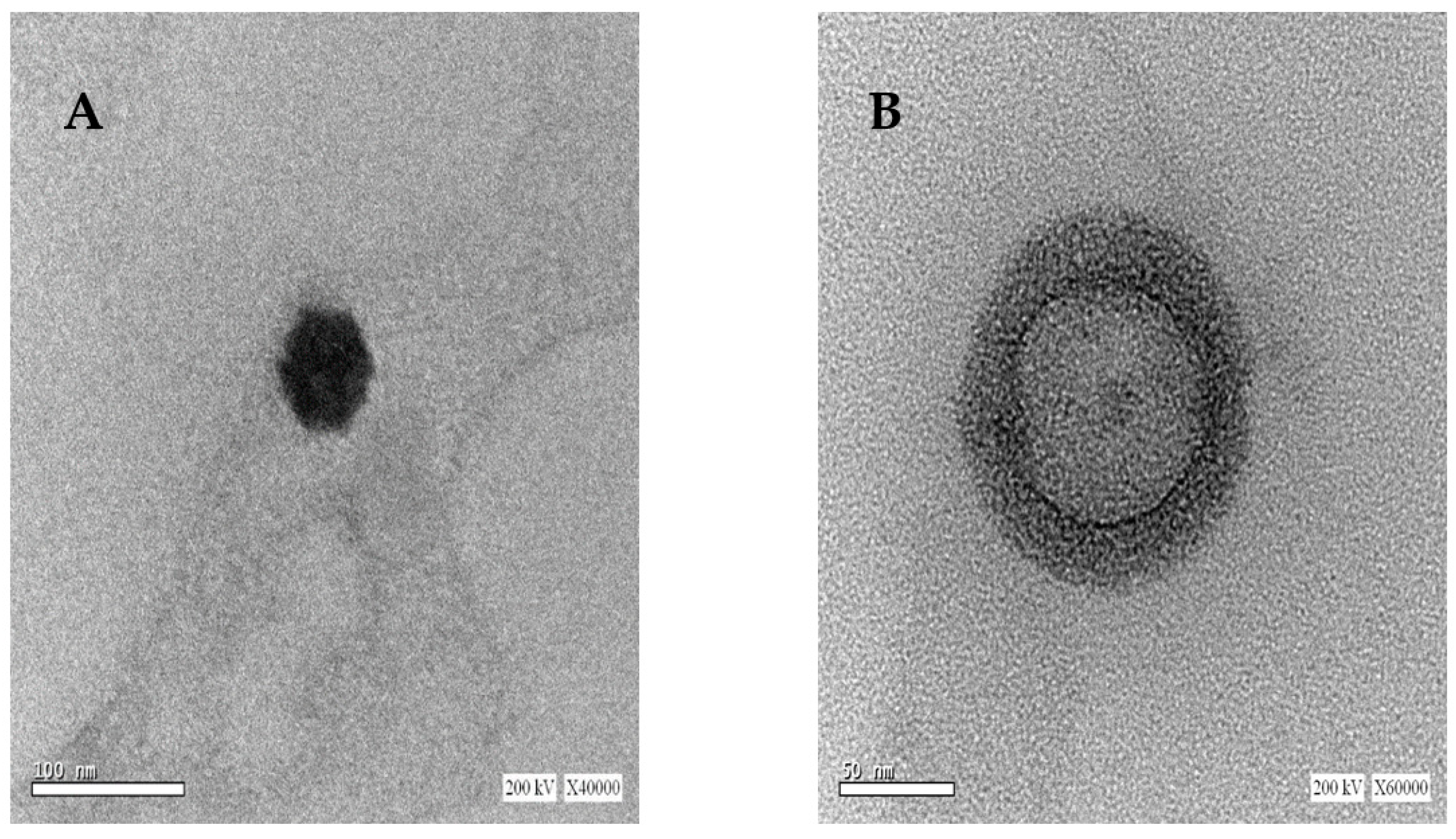
2.6. Morphology of Uncoated and Coated SLNs
2.7. In Vitro Release Study
2.8. Ex Vivo Permeation Studies using Goat Intestinal Mucosa
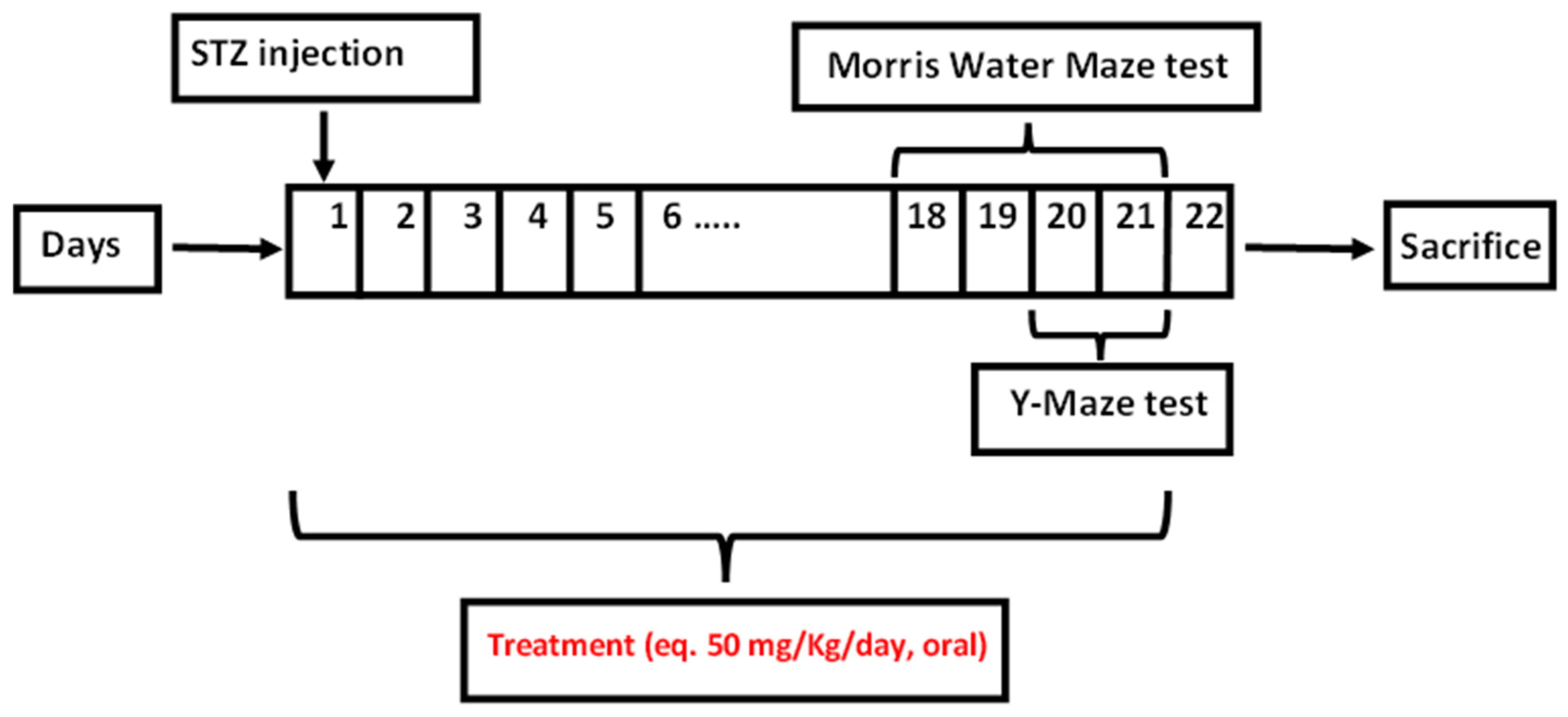
2.9. In Vivo Studies
2.9.1. Y-Maze Test
2.9.2. Morris Water Maze
2.9.3. Enzyme-Linked Immunosorbent Assay (ELISA)
2.9.4. Histological Examination
3. Material and Methods
3.1. Plant Material and Extraction
3.2. Assessment of Total Phenolic Content (TPC) and Total Flavonoids Content (TFC)
3.3. UPLC-ESI-MS/MS Analysis
3.4. Assessment of Antioxidant Properties
3.4.1. DPPH Radical Scavenging Capacity
3.4.2. Iron Metal Chelation Assay
3.4.3. ABTS Decolorization Assay
3.4.4. Oxygen Radical Absorbance Capacity (ORAC) Assay
3.5. Preparation of Uncoated and Chitosan-Coated Artichoke-Loaded Solid Lipid Nanoparticles (SLNs)
3.6. Measurement of Particle Size and Zeta Potential
3.7. Measurement of Entrapment Efficiency (EE%)
3.8. Morphological Examination by Transmission Electron Microscopy (TEM)
3.9. In Vitro Release Study
3.10. Ex Vivo Permeation Study Using Goat Intestinal Mucosa
3.11. In Vivo Study
3.11.1. Animals
3.11.2. Induction of AD and Treatment Modalities
3.11.3. Behavioral Assessment of the Effects of ART
Y-Maze
Morris Water Maze (MWM)
3.11.4. Enzyme-Linked Immunosorbent Assay (ELISA)
3.11.5. Histopathology
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. Fact-Sheets. Dementia. WHO. 2022. Available online: https://www.who.int/news-room/fact-sheets/detail/dementia (accessed on 10 September 2022).
- Habtemariam, S. Natural products in Alzheimer’s disease therapy: Would old therapeutic approaches fix the broken promise of modern medicines? Molecules 2019, 24, 1519. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.Y.; Gao, Y.; Sun, J.Y.; Meng, X.L.; Yang, D.; Fan, L.H.; Xiang, L.; Wang, P. Traditional Chinese medicine: Role in reducing β-amyloid, apoptosis, autophagy, neuroinflammation, oxidative stress, and mitochondrial dysfunction of Alzheimer’s disease. Front. Pharmacol. 2020, 11, 497. [Google Scholar] [CrossRef] [PubMed]
- The Plant List. Version 1.1. Available online: http://www.theplantlist.org/ (accessed on 7 July 2022).
- Zayed, A.; Farag, M.A. Valorization, extraction optimization and technology advancements of artichoke biowastes: Food and non-food applications. LWT 2020, 132, 109883. [Google Scholar] [CrossRef]
- FAOSTAT. Food and Agriculture Organization of the United Nations Statistical Database 2021. Available online: https://www.fao.org/faostat/en/#data/QCL (accessed on 9 May 2022).
- Ibrahim, N.; Moussa, A.Y. A comparative volatilomic characterization of Florence fennel from different locations: Antiviral prospects. Food Funct. 2021, 12, 1498–1515. [Google Scholar] [CrossRef]
- Sakr, M.; Ibrahim, N.; Ali, S.; Alzahaby, N.; Omar, A.; Khairy, W.; Zohdy, B.; Qassem, O.; Saleh, S. Identification of potential quorum quenching compounds in Brassica oleracea var. capitata against MDR Pseudomonas aeruginosa and Escherichia coli clinical isolates. Arch. Pharm. Sci. Ain Shams Univ. 2021, 5, 128–142. [Google Scholar] [CrossRef]
- Gostin, A.-I.; Waisundara, V.Y. Edible flowers as functional food: A review on artichoke (Cynara cardunculus L.). Trends Food Sci. Technol. 2019, 86, 381–391. [Google Scholar] [CrossRef]
- Yang, M.; Ma, Y.; Wang, Z.; Khan, A.; Zhou, W.; Zhao, T.; Cao, J.; Cheng, G.; Cai, S. Phenolic constituents, antioxidant and cytoprotective activities of crude extract and fractions from cultivated artichoke inflorescence. Ind. Crops Prod. 2020, 143, 111433. [Google Scholar] [CrossRef]
- Liao, G.-C.; Jhuang, J.-H.; Yao, H.-T. Artichoke leaf extract supplementation lowers hepatic oxidative stress and inflammation and increases multidrug resistance-associated protein 2 in mice fed a high-fat and high-cholesterol diet. Food Funct. 2021, 12, 7239–7249. [Google Scholar] [CrossRef]
- Abd El-Aziz, N.M.; Awad, O.M.E.; Shehata, M.G.; El-Sohaimy, S.A. Antioxidant and anti-acetylcholinesterase potential of artichoke phenolic compounds. Food Biosci. 2021, 41, 101006. [Google Scholar] [CrossRef]
- Yasukawa, K.; Matsubara, H.; Sano, Y. Inhibitory effect of the flowers of artichoke (Cynara cardunculus) on TPA-induced inflammation and tumor promotion in two-stage carcinogenesis in mouse skin. J. Nat. Med. 2010, 64, 388–391. [Google Scholar] [CrossRef]
- Ibrahim, N.; Ibrahim, H.; Sabater, A.M.; Mazier, D.; Valentin, A.; Nepveu, F. Artemisinin nanoformulation suitable for intravenous injection: Preparation, characterization and antimalarial activities. Int. J. Pharm. 2015, 495, 671–679. [Google Scholar] [CrossRef]
- Teja, P.K.; Mithiya, J.; Kate, A.S.; Bairwa, K.; Chauthe, S.K. Herbal nanomedicines: Recent advancements, challenges, opportunities and regulatory overview. Phytomedicine 2021, 96, 153890. [Google Scholar] [CrossRef]
- Tabassum, S.; Zia, M.; Carcahe de Blanco, E.J.; Batool, R.; Aslam, R.; Hussain, S.; Wali, Q.; Gulzar, M.M. Phytochemical, in-vitro biological and chemo-preventive profiling of Arisaema jacquemontii Blume tuber extracts. BMC Complement Altern. Med. 2019, 19, 256. [Google Scholar] [CrossRef]
- Lavecchia, R.; Maffei, G.; Paccassoni, F.; Piga, L.; Zuorro, A. Artichoke waste as a source of phenolic antioxidants and bioenergy. Waste Biomass Valorization 2019, 10, 2975–2984. [Google Scholar] [CrossRef]
- Balez, R.; Steiner, N.; Engel, M.; Muñoz, S.S.; Lum, J.S.; Wu, Y.; Wang, D.; Vallotton, P.; Sachdev, P.; O’Connor, M.; et al. Neuroprotective effects of apigenin against inflammation, neuronal excitability and apoptosis in an induced pluripotent stem cell model of Alzheimer’s disease. Sci. Rep. 2016, 6, 31450. [Google Scholar] [CrossRef]
- Silva dos Santos, J.; Goncalves Cirino, J.P.; de Oliveira Carvalho, P.; Ortega, M.M. The Pharmacological Action of Kaempferol in Central Nervous System Diseases: A Review. Front. Pharmacol. 2021, 11, 2143. [Google Scholar] [CrossRef]
- Daily, J.W.; Kang, S.; Park, S. Protection against Alzheimer’s disease by luteolin: Role of brain glucose regulation, anti-inflammatory activity, and the gut microbiota-liver-brain axis. Biofactors 2021, 47, 218–231. [Google Scholar] [CrossRef]
- Khan, H.; Ullah, H.; Aschner, M.; Cheang, W.S.; Akkol, E.K. Neuroprotective effects of quercetin in Alzheimer’s disease. Biomolecules 2020, 10, 59. [Google Scholar] [CrossRef]
- Kwon, S.H.; Lee, H.K.; Kim, J.A.; Hong, S.I.; Kim, H.C.; Jo, T.H.; Park, Y.I.; Lee, C.K.; Kim, Y.B.; Lee, S.Y.; et al. Neuroprotective effects of chlorogenic acid on scopolamine-induced amnesia via anti-acetylcholinesterase and anti-oxidative activities in mice. Eur. J. Pharmacol. 2010, 649, 210–217. [Google Scholar] [CrossRef]
- Pagano, I.; Piccinelli, A.L.; Celano, R.; Campone, L.; Gazzerro, P.; De Falco, E.; Rastrelli, L. Chemical profile and cellular antioxidant activity of artichoke by-products. Food Funct. 2016, 7, 4841–4850. [Google Scholar] [CrossRef]
- Lee, C.L.; Liao, K.C.; Chen, C.C.; Lin, Y.A.; Wu, T.Y.; Jhan, Y.L.; Chen, C.J.; Yang, J.C.; Wu, Y.C. Characterization Of Secondary Metabolites From The Rhizome Of Cynara Scolymus And Their Antioxidant Properties. Nat. Prod. Res. 2021, 35, 2051–2055. [Google Scholar] [CrossRef]
- Turkiewicz, I.P.; Wojdyło, A.; Tkacz, K.; Nowicka, P.; Hernández, F. Antidiabetic, anticholinesterase and antioxidant activity vs. terpenoids and phenolic compounds in selected new cultivars and hybrids of artichoke Cynara scolymus L. Molecules 2019, 24, 1222. [Google Scholar] [CrossRef]
- Gouveia, S.C.; Castilho, P.C. Phenolic composition and antioxidant capacity of cultivated artichoke, Madeira cardoon and artichoke-based dietary supplements. Food Res. Int. 2012, 48, 712–724. [Google Scholar] [CrossRef]
- D’Antuono, I.; Carola, A.; Sena, L.M.; Linsalata, V.; Cardinali, A.; Logrieco, A.F.; Colucci, M.G.; Apone, F. Artichoke Polyphenols Produce Skin Anti-Age Effects by Improving Endothelial Cell Integrity and Functionality. Molecules 2018, 23, 2729. [Google Scholar] [CrossRef] [PubMed]
- Alarcón-Flores, M.I.; Romero-González, R.; Martínez Vidal, J.L.; Garrido Frenich, A. Determination of phenolic compounds in artichoke, garlic and spinach by ultra-high-performance liquid chromatography coupled to tandem mass spectrometry. Food Anal. Methods 2014, 7, 2095–2106. [Google Scholar] [CrossRef]
- Lattanzio, V.; van Sumere, C.F. Changes in phenolic compounds during the development and cold storage of artichoke (Cynara scolymus L.) heads. Food Chem. 1987, 24, 37–50. [Google Scholar] [CrossRef]
- Ivanova, A.; Gerasimova, E.; Gazizullina, E. Study of antioxidant properties of agents from the perspective of their action mechanisms. Molecules 2020, 25, 4251. [Google Scholar] [CrossRef]
- Wong, J.Y.; Matanjun, P.; Ooi, Y.B.H.; Chia, K.F. Evaluation of antioxidant activities in relation to total phenolics and flavonoids content of selected Malaysian wild edible plants by multivariate analysis. Int. J. Food Prop. 2014, 17, 1763–1778. [Google Scholar] [CrossRef]
- Nagulendran, K.R.; Velavan, S.; Mahesh, R.; Begum, V.H. In vitro antioxidant activity and total polyphenolic content of Cyperus rotundus rhizomes. E-J. Chem. 2007, 4, 440–449. [Google Scholar] [CrossRef]
- Adedapo, A.A.; Jimoh, F.O.; Koduru, S.; Masika, P.J.; Afolayan, A.J. Evaluation of the medicinal potentials of the methanol extracts of the leaves and stems of Halleria lucida. Bioresour. Technol. 2008, 99, 4158–4163. [Google Scholar] [CrossRef] [PubMed]
- Jiménez-Moreno, N.; Cimminelli, M.J.; Volpe, F.; Ansó, R.; Esparza, I.; Mármol, I.; Rodríguez-Yoldi, M.J.; Ancín-Azpilicueta, C. Phenolic composition of artichoke waste and its antioxidant capacity on differentiated Caco-2 cells. Nutrients 2019, 11, 1723. [Google Scholar] [CrossRef]
- Oktay, M.; Gülçin, İ.; Küfrevioğlu, Ö.İ. Determination of in vitro antioxidant activity of fennel (Foeniculum vulgare) seed extracts. LWT-Food Sci. Technol. 2003, 36, 263–271. [Google Scholar] [CrossRef]
- Zhou, M.; Hou, J.; Zhong, Z.; Hao, N.; Lin, Y.; Li, C. Targeted delivery of hyaluronic acid-coated solid lipid nanoparticles for rheumatoid arthritis therapy. Drug Deliv. 2018, 25, 716–722. [Google Scholar] [CrossRef]
- Zewail, M. Folic acid decorated chitosan-coated solid lipid nanoparticles for the oral treatment of rheumatoid arthritis. Ther. Deliv. 2021, 12, 297–310. [Google Scholar] [CrossRef]
- Ganesan, P.; Ramalingam, P.; Karthivashan, G.; Ko, Y.T.; Choi, D.K. Recent developments in solid lipid nanoparticle and surface-modified solid lipid nanoparticle delivery systems for oral delivery of phyto-bioactive compounds in various chronic diseases. Int. J. Nanomed. 2018, 13, 1569. [Google Scholar] [CrossRef]
- Anchan, R.B.; Koland, M. Oral Insulin Delivery by Chitosan Coated Solid Lipid Nanoparticles: Ex vivo and in vivo Studies. J. Young Pharm. 2021, 13, 43. [Google Scholar] [CrossRef]
- Zewail, M.; Nafee, N.; Helmy, M.W.; Boraie, N. Coated nanostructured lipid carriers targeting the joints–An effective and safe approach for the oral management of rheumatoid arthritis. Int. J. Pharm. 2019, 567, 118447. [Google Scholar] [CrossRef]
- Patchornik, S.; Ram, E.; Ben Shalom, N.; Nevo, Z.; Robinson, D. Chitosan-hyaluronate hybrid gel intraarticular injection delays osteoarthritis progression and reduces pain in a rat meniscectomy model as compared to saline and hyaluronate treatment. Adv. Orthop. 2012, 2012, 979152. [Google Scholar] [CrossRef]
- Shin, G.H.; Kim, J.T. Observation of chitosan coated lipid nanoparticles with different lipid compositions under simulated in vitro digestion system. Food Hydrocoll. 2018, 84, 146–153. [Google Scholar] [CrossRef]
- Vieira, A.C.; Chaves, L.L.; Pinheiro, S.; Pinto, S.; Pinheiro, M.; Lima, S.C.; Ferreira, D.; Sarmento, B.; Reis, S. Mucoadhesive chitosan-coated solid lipid nanoparticles for better management of tuberculosis. Int. J. Pharm. 2018, 536, 478–485. [Google Scholar] [CrossRef]
- Luo, Q.; Zhao, J.; Zhang, X.; Pan, W. Nanostructured lipid carrier (NLC) coated with Chitosan Oligosaccharides and its potential use in ocular drug delivery system. Int. J. Pharm. 2011, 403, 185–191. [Google Scholar] [CrossRef] [PubMed]
- Hu, L.; Sun, Y.; Wu, Y. Advances in chitosan-based drug delivery vehicles. Nanoscale 2013, 5, 3103–3111. [Google Scholar] [CrossRef] [PubMed]
- Abbas, H.; Gad, H.A.; El Sayed, N.S.; Rashed, L.A.; Khattab, M.A.; Noor, A.O.; Zewail, M. Treatment of lung cancer via telomerase inhibition: Self-assembled nanoplexes versus polymeric nanoparticles as vectors for 2′-O-Methyl-RNA. Eu. J. Pharm. Biopharm. 2012, 80, 478–489. [Google Scholar]
- Nasr, M.; Nafee, N.; Saad, H.; Kazem, A. Improved antitumor activity and reduced cardiotoxicity of epirubicin using hepatocyte-targeted nanoparticles combined with tocotrienols against hepatocellular carcinoma in mice. Eur. J. Pharm. Biopharm. 2014, 88, 216–225. [Google Scholar] [CrossRef]
- Thilakarathna, S.H.; Rupasinghe, H.P. Flavonoid bioavailability and attempts for bioavailability enhancement. Nutrients 2013, 5, 3367–3387. [Google Scholar] [CrossRef]
- Sharma, M.; Gupta, Y. Intracerebroventricular injection of streptozotocin in rats produces both oxidative stress in the brain and cognitive impairment. Life Sci. 2001, 68, 1021–1029. [Google Scholar] [CrossRef]
- Sorial, M.E.; El Sayed, N.S.E.D. Protective effect of valproic acid in streptozotocin-induced sporadic Alzheimer’s disease mouse model: Possible involvement of the cholinergic system. Naunyn-Schmiedeberg’s Arch. Pharmacol. 2017, 390, 581–593. [Google Scholar] [CrossRef]
- Khalili, M.; Hamzeh, F. Effects of active constituents of Crocus sativus L., crocin on streptozocin-induced model of sporadic Alzheimer’s disease in male rats. Iran. Biomed. J. 2010, 14, 59. [Google Scholar]
- Abbas, H.; Refai, H.; El Sayed, N.; Rashed, L.A.; Mousa, M.R.; Zewail, M. Superparamagnetic Iron Oxide Loaded Chitosan Coated Bilosomes for Magnetic Nose to Brain Targeting of Resveratrol. Int. J. Pharm. 2021, 610, 121244. [Google Scholar] [CrossRef]
- Wang, P.; Guan, P.P.; Wang, T.; Yu, X.; Guo, J.J.; Wang, Z.Y. Aggravation of Alzheimer’s disease due to the COX-2-mediated reciprocal regulation of IL-1β and A β between glial and neuron cells. Aging Cell 2014, 13, 605–615. [Google Scholar] [CrossRef]
- Manek, E.; Darvas, F.; Petroianu, G.A. Use of Biodegradable, Chitosan-Based Nanoparticles in the Treatment of Alzheimer’s Disease. Molecules 2020, 25, 4866. [Google Scholar] [CrossRef]
- Wang, G.; Hu, Z.; Fu, Q.; Song, X.; Cui, Q.; Jia, R.; Zou, Y.; He, C.; Li, L.; Yin, Z. Resveratrol mitigates lipopolysaccharide-mediated acute inflammation in rats by inhibiting the TLR4/NF-κBp65/MAPKs signaling cascade. Sci. Rep. 2017, 7, 45006. [Google Scholar] [CrossRef]
- Kandimalla, R.J.; Prabhakar, S.; Wani, W.Y.; Kaushal, A.; Gupta, N.; Sharma, D.R.; Grover, V.K.; Bhardwaj, N.; Jain, K.; Gill, K.D. CSF p-Tau levels in the prediction of Alzheimer’s disease. Biol. Open 2013, 2, 1119–1124. [Google Scholar] [CrossRef]
- Duits, F.H.; Wesenhagen, K.E.; Ekblad, L.; Wolters, E.; Willemse, E.A.; Scheltens, P.; van der Flier, W.M.; Teunissen, C.E.; Visser, P.J.; Tijms, B.M. Four subgroups based on tau levels in Alzheimer’s disease observed in two independent cohorts. Alzheimer’s Res. Ther. 2021, 13, 2. [Google Scholar] [CrossRef]
- Baptista, F.I.; Henriques, A.G.; Silva, A.M.; Wiltfang, J.; da Cruz e Silva, O.A. Flavonoids as therapeutic compounds targeting key proteins involved in Alzheimer’s disease. ACS Chem. Neurosci. 2014, 5, 83–92. [Google Scholar] [CrossRef]
- Decourt, B.; K Lahiri, D.; N Sabbagh, M. Targeting tumor necrosis factor alpha for Alzheimer’s disease. Curr. Alzheimer Res. 2017, 14, 412–425. [Google Scholar] [CrossRef]
- Standridge, J.B. Vicious cycles within the neuropathophysiologic mechanisms of Alzheimer’s disease. Curr. Alzheimer Res. 2006, 3, 95–107. [Google Scholar] [CrossRef]
- Ayaz, M.; Sadiq, A.; Junaid, M.; Ullah, F.; Ovais, M.; Ullah, I.; Ahmed, J.; Shahid, M. Flavonoids as prospective neuroprotectants and their therapeutic propensity in aging associated neurological disorders. Front. Aging Neurosci. 2019, 11, 155. [Google Scholar] [CrossRef]
- Guzzi, C.; Colombo, L.; Luigi, A.D.; Salmona, M.; Nicotra, F.; Airoldi, C. Flavonoids and Their Glycosides as Anti-amyloidogenic Compounds: Aβ1–42 Interaction Studies to Gain New Insights into Their Potential for Alzheimer’s Disease Prevention and Therapy. Chem.—Asian J. 2017, 12, 67–75. [Google Scholar] [CrossRef]
- El-Nashar, H.A.; Eldehna, W.M.; Al-Rashood, S.T.; Alharbi, A.; Eskandrani, R.O.; Aly, S.H. GC/MS Analysis of Essential Oil and Enzyme Inhibitory Activities of Syzygium cumini (Pamposia) Grown in Egypt: Chemical Characterization and Molecular Docking Studies. Molecules 2021, 26, 6984. [Google Scholar] [CrossRef]
- Zhao, L.; Wang, J.L.; Wang, Y.R.; Fa, X.Z. Apigenin attenuates copper-mediated β-amyloid neurotoxicity through antioxidation, mitochondrion protection and MAPK signal inactivation in an AD cell model. Brain Res. 2013, 1492, 33–45. [Google Scholar] [CrossRef] [PubMed]
- Alsadat, A.M.; Nikbakht, F.; Nia, H.H.; Golab, F.; Khadem, Y.; Barati, M.; Vazifekhah, S. GSK-3β as a target for apigenin-induced neuroprotection against Aβ 25-35 in a rat model of Alzheimer’s disease. Neuropeptides 2021, 90, 102200. [Google Scholar] [CrossRef] [PubMed]
- Dourado, N.S.; Souza, C.D.S.; De Almeida, M.M.A.; Bispo da Silva, A.; Dos Santos, B.L.; Silva, V.D.A.; De Assis, A.M.; da Silva, J.S.; Souza, D.O.; Costa, M.D.F.D.; et al. Neuroimmunomodulatory and Neuroprotective Effects of the Flavonoid Apigenin in in vitro Models of Neuroinflammation Associated With Alzheimer’s Disease. Front. Aging Neurosci. 2020, 12, 119. [Google Scholar] [CrossRef] [PubMed]
- Jeong, C.H.; Jeong, H.R.; Choi, G.N.; Kim, D.O.; Lee, U.K.; Heo, H.J. Neuroprotective and anti-oxidant effects of caffeic acid isolated from Erigeron annuus leaf. Chin. Med. 2011, 6, 25. [Google Scholar] [CrossRef]
- Colonnello, A.; Aguilera-Portillo, G.; Rubio-López, L.C.; Robles-Bañuelos, B.; Rangel-López, E.; Cortez-Núñez, S.; Evaristo-Priego, Y.; Silva-Palacios, A.; Galván-Arzate, S.; García-Contreras, R.; et al. Comparing the Neuroprotective Effects of Caffeic Acid in Rat Cortical Slices and Caenorhabditis elegans: Involvement of Nrf2 and SKN-1 Signaling Pathways. Neurotox. Res. 2020, 37, 326–337. [Google Scholar] [CrossRef]
- Kumar, G.; Mukherjee, S.; Paliwal, P.; Singh, S.S.; Birla, H.; Singh, S.P.; Krishnamurthy, S.; Patnaik, R. Neuroprotective effect of chlorogenic acid in global cerebral ischemia-reperfusion rat model. Naunyn. Schmiedeberg’s Arch. Pharmacol. 2019, 392, 1293–1309. [Google Scholar] [CrossRef]
- Metwally, D.M.; Alajmi, R.A.; El-Khadragy, M.F.; Yehia, H.M.; AL-Megrin, W.A.; Akabawy, A.M.; Amin, H.K.; Moneim, A.E.A. Chlorogenic acid confers robust neuroprotection against arsenite toxicity in mice by reversing oxidative stress, inflammation, and apoptosis. J. Funct. Foods 2020, 75, 104202. [Google Scholar] [CrossRef]
- Rebai, O.; Belkhir, M.; Sanchez-Gomez, M.V.; Matute, C.; Fattouch, S.; Amri, M. Differential Molecular Targets for Neuroprotective Effect of Chlorogenic Acid and its Related Compounds Against Glutamate Induced Excitotoxicity and Oxidative Stress in Rat Cortical Neurons. Neurochem. Res. 2017, 42, 3559–3572. [Google Scholar] [CrossRef]
- Xu, P.X.; Wang, S.W.; Yu, X.L.; Su, Y.J.; Wang, T.; Zhou, W.W.; Zhang, H.; Wang, Y.J.; Liu, R.T. Rutin improves spatial memory in Alzheimer’s disease transgenic mice by reducing Aβ oligomer level and attenuating oxidative stress and neuroinflammation. Behav. Brain Res. 2014, 264, 173–180. [Google Scholar] [CrossRef]
- Abdelghffar, E.A.; El-Nashar, H.A.; Al-Mohammadi, A.G.; Eldahshan, O.A. Orange fruit (Citrus sinensis) peel extract attenuates chemotherapy-induced toxicity in male rats. Food Funct. 2021, 12, 9443–9455. [Google Scholar] [CrossRef]
- Attard, E. A rapid microtitre plate Folin-Ciocalteu method for the assessment of polyphenols. Open Life Sci. 2013, 8, 48–53. [Google Scholar] [CrossRef]
- Kiranmai, M.; Kumar, C.M.; Mohammed, I. Comparison of total flavanoid content of Azadirachta indica root bark extracts prepared by different methods of extraction. Res. J. Pharm. Biol. Chem. Sci. 2011, 2, 254–261. [Google Scholar]
- Lalitha, T.; Jayanthi, P. Study of antioxidant activity of ethanolic extract of fresh Eichhornia crassipes (Mart.) Solms. Der Pharm. Sin. J. 2012, 3, 271–277. [Google Scholar]
- Santos, J.S.; Alvarenga Brizola, V.R.; Granato, D. High-throughput assay comparison and standardization for metal chelating capacity screening: A proposal and application. Food Chem. 2017, 214, 515–522. [Google Scholar] [CrossRef]
- Arnao, M.B.; Cano, A.; Acosta, M. The hydrophilic and lipophilic contribution to total antioxidant activity. Food Chem. 2001, 73, 239–244. [Google Scholar] [CrossRef]
- Liang, Z.; Cheng, L.; Zhong, G.Y.; Liu, R.H. Antioxidant and antiproliferative activities of twenty-four Vitis vinifera grapes. PLoS ONE 2014, 9, e105146. [Google Scholar] [CrossRef]
- Mehla, J.; Pahuja, M.; Gupta, Y.K. Streptozotocin-induced sporadic Alzheimer’s disease: Selection of appropriate dose. J. Alzheimer’s Dis. 2013, 33, 17–21. [Google Scholar] [CrossRef]
- Abbas, H.; Gad, H.A.; Khattab, M.A.; Mansour, M. The Tragedy of Alzheimer’s Disease: Towards Better Management via Resveratrol-Loaded Oral Bilosomes. Pharmaceutics 2021, 13, 1635. [Google Scholar] [CrossRef]
- Culling, C.F.A. Handbook of Histopathological and Histochemical Techniques: Including Museum Techniques; Butterworth-Heinemann: Oxford, UK, 2013. [Google Scholar]
- Abbas, H.; Gad, H.A.; El Sayed, N.S.; Rashed, L.A.; Khattab, M.A.; Noor, A.O.; Zewail, M. Development and Evaluation of Novel Leflunomide SPION Bioemulsomes for the Intra-Articular Treatment of Arthritis. Pharmaceutics 2022, 14, 2005. [Google Scholar] [CrossRef]





| No | tR (min) | [M − H]− m/z | Molecular Weight | MS(n) m/z | Molecular Formula | Tentative Identification | Class | Reference(s) |
|---|---|---|---|---|---|---|---|---|
| 1. | 0.75 | 178 | 179 | 135 | C9H8O4 | Caffeic acid | Phenolic acid | [23] |
| 2. | 0.98 | 181 | 182 | 155, 140 | C9H10O4 | Syringaldehyde | Aldehyde | [24] |
| 3. | 1.15 | 353 | 354 | 191, 179, 135 | C16H18O9 | Chlorogenic acid | Phenolic acid | [24] |
| 4. | 13.72 | 515 | 516 | 353, 179, 191 | C25H24O12 | 1,3 di-O-caffeoylquinic acid | Phenolic acid | [24] |
| 5. | 13.90 | 515 | 516 | 335, 317, 203, 179, 191 | C25H24O12 | 3,4 di-O-caffeoylquinic acid | Phenolic acid | [25] |
| 6. | 18.31 | 521 | 522 | 359, 223, 161 | C24H26O13 | Rosmarinic acid-O-hexoside | Phenolic acid glycoside | [26] |
| 7. | 19.09 | 415 | 416 | 269 | C21H20O9 | Apigenin-O-deoxyhexoside | Flavonoid glycoside | [27] |
| 8. | 19.47 | 577 | 578 | 269, 225, 151 | C27H30O14 | Apigenin-O-rutinoside | Flavonoid glycoside | [23] |
| 9. | 20.02 | 445 | 446 | 269, 151, 117 | C21H18O11 | Apigenin-O-hexouronide | Flavonoid glycoside | [25] |
| 10. | 20.98 | 447 | 448 | 285, 241, 151 | C21H20O11 | Luteolin-O-hexoside | Flavonoid glycoside | [28,29] |
| 11. | 22.12 | 593 | 594 | 285, 227, 151 | C27H30O15 | Kaempferol-O-rutinoside | Flavonoid glycoside | [28,29] |
| 12. | 22.35 | 283 | 284 | 270, 229, 225 | C16H12O5 | Glycitein | Flavonoid glycoside | [28,29] |
| 13. | 23.39 | 609 | 610 | 301, 300, 271, 243, 227 | C27H30O16 | Quercetin-3-O-hexoside-3-deoxyhexoside (Rutin) | Flavonoid glycoside | [12] |
| 14. | 24.54 | 431 | 432 | 269, 225, 151, 117 | C21H20O10 | Apigenin-O-hexoside | Flavonoid glycoside | [27] |
| 15. | 31.02 | 533 | 534 | 490, 489, 285 | C25H25O12 | Luteolin-O-diacetylhexoside | Flavonoid glycoside | [26] |
| 16. | 31.72 | 683 | 684 | 341, 179, 143, 131 | C15H18O9 | Caffeic acid-O-hexoside dimer | Phenolic acid glycoside | [26] |
| Formulation Code | F1 | F2 | F3 | F4 |
|---|---|---|---|---|
| Internal aqueous phase | ART (1 mg) in 0.2 mL 0.1 M HCl | |||
| Lipid phase | GMS | |||
| External aqueous phase | Poloxamer 407 | Tween 80 | Poloxamer 407 | Tween 80 |
| CS coating solution (%w/v) | ------- | 0.50% | ||
| Particle size (nm) | 165.3 ± 1.69 | 320.4 ± 1.03 | 198.3 ± 1.98 | 448.3 ± 1.23 |
| PDI | 0.235 ± 0.006 | 0.312 ± 0.004 | 0.203 ± 0.003 | 0.504 ± 0.0031 |
| Zeta potential (mV) | −26.3 ± 2.04 | −32.5 ±1.45 | 19.25 ±1.89 | 22.4 ±0.87 |
| EE % | 74 ± 1.56 | 57 ± 2.06 | 79.2 ± 1.12 | 54 ± 1.09 |
| Release fitting (R2) | ||||
| Zero order | 0.947 | 0.941 | 0.945 | 0.959 |
| First order | 0.982 | 0.987 | 0.908 | 0.9344 |
| Higuchi | 0.988 | 0.984 | 0.964 | 0.975 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
El-Nashar, H.A.S.; Abbas, H.; Zewail, M.; Noureldin, M.H.; Ali, M.M.; Shamaa, M.M.; Khattab, M.A.; Ibrahim, N. Neuroprotective Effect of Artichoke-Based Nanoformulation in Sporadic Alzheimer’s Disease Mouse Model: Focus on Antioxidant, Anti-Inflammatory, and Amyloidogenic Pathways. Pharmaceuticals 2022, 15, 1202. https://doi.org/10.3390/ph15101202
El-Nashar HAS, Abbas H, Zewail M, Noureldin MH, Ali MM, Shamaa MM, Khattab MA, Ibrahim N. Neuroprotective Effect of Artichoke-Based Nanoformulation in Sporadic Alzheimer’s Disease Mouse Model: Focus on Antioxidant, Anti-Inflammatory, and Amyloidogenic Pathways. Pharmaceuticals. 2022; 15(10):1202. https://doi.org/10.3390/ph15101202
Chicago/Turabian StyleEl-Nashar, Heba A. S., Haidy Abbas, Mariam Zewail, Mohamed H. Noureldin, Mai M. Ali, Marium M. Shamaa, Mohamed A. Khattab, and Nehal Ibrahim. 2022. "Neuroprotective Effect of Artichoke-Based Nanoformulation in Sporadic Alzheimer’s Disease Mouse Model: Focus on Antioxidant, Anti-Inflammatory, and Amyloidogenic Pathways" Pharmaceuticals 15, no. 10: 1202. https://doi.org/10.3390/ph15101202
APA StyleEl-Nashar, H. A. S., Abbas, H., Zewail, M., Noureldin, M. H., Ali, M. M., Shamaa, M. M., Khattab, M. A., & Ibrahim, N. (2022). Neuroprotective Effect of Artichoke-Based Nanoformulation in Sporadic Alzheimer’s Disease Mouse Model: Focus on Antioxidant, Anti-Inflammatory, and Amyloidogenic Pathways. Pharmaceuticals, 15(10), 1202. https://doi.org/10.3390/ph15101202






